Abstract
Background:
The treatment outcome “default” under Revised National Tuberculosis Control Program (RNTCP) is a patient who after treatment initiation has interrupted treatment consecutively for more than 2 months.
Aims:
To assess the timing, characteristics and distribution of the reasons for default with relation to some sociodemographic variables among new sputum-positive (NSP) tuberculosis (TB) patients in Darjeeling District, West Bengal.
Settings and Design:
A case-control study was conducted in three tuberculosis units (TUs) of Darjeeling from August’2011 to December’2011 among NSP TB patients enrolled for treatment in the TB register from 1st Qtr’09 to 2nd Qtr’10. Patients defaulted from treatment were considered as “cases” and those completed treatment as “controls” (79 cases and 79 controls).
Materials and Methods:
The enrolled cases and controls were interviewed by the health workers using a predesigned structured pro-forma.
Statistical Analysis Used:
Logistic regression analysis, odds ratios (OR), adjusted odds ratios (AOR).
Results:
75% of the default occurred in the intensive phase (IP); 54.24% retrieval action was done within 1 day during IP and 75% within 1 week during continuation phase (CP); cent percent of the documented retrieval actions were undertaken by the contractual TB program staffs. Most commonly cited reasons for default were alcohol consumption (29.11%), adverse effects of drugs (25.32%), and long distance of DOT center (21.52%). In the logistic regression analysis, the factors independently associated were consumption of alcohol, inadequate knowledge about TB, inadequate patient provider interaction, instances of missed doses, adverse reactions of anti-TB drugs, Government Directly Observed Treatment (DOT) provider and smoking.
Conclusions:
Most defaults occurred in the intensive phase; pre-treatment counseling and initial home visit play very important role in this regard. Proper counseling by health care workers in patient provider meeting is needed.
Keywords: Alcohol drinking, case-control study, smoking, treatment outcome, tuberculosis
Introduction
In 2013, total population of India covered under Revised National Tuberculosis Control Program (RNTCP) were 1247 millions; 81,21,514 TB suspects were examined; 9,28,190 smear-positive TB patients were diagnosed; 7,98,414 smear-positive cases were notified; and 14,10,880 patients were registered for treatment. The treatment success rate has been more than 85% since the year 2001; default rates have decreased from 9% in 1999 to 6% in 2012 among NSP cases. High default rates among smear-positive retreatment cases (more than 15%) have been an area of concern.[1] The treatment outcome “default” under RNTCP is a patient who after treatment initiation has interrupted treatment consecutively for more than 2 months.[2] The public health and clinical consequences of TB treatment default are severe. Defaulted patients perpetuate TB transmission and have high mortality rate and rate of recurrent disease than those who have completed treatment.[3,4]
In 2013, in West Bengal, total population covered by RNTCP was 932 lakhs; 5,62,619 TB suspects were examined; 61658 smear-positive TB patients were diagnosed; 90423 TB patients were registered for treatment; default rates were 6% among NSP cases; 7% among new smear negative (NSN) cases; 4% among new extra pulmonary cases; 11% among relapse cases; 15% among treatment failure cases; and 23% among treatment after default cases, respectively.[5]
Darjeeling is epidemiologically important district regarding tuberculosis (TB). It has the highest case finding rate (326/Lac)[6] and highest death rate in West Bengal suggesting high rates of transmission and late case recognition. Geographically it has diverse terrain with lots of difficulty to reach the target areas. It is the last district to implement RNTCP in West Bengal (December 2004) but one of the first districts to start DOTS Plus (2009) due to high multi-drug-resistant (MDR) TB.[6] Population covered under RNTCP in 2013 was 18.8 lakhs; 14,771 TB suspects were examined; 2143 smear-positive TB patients were diagnosed; total patients registered for treatment were 3236; treatment success rate among new smear positive cases was 84%; received DOT through a community volunteer were 1755 (54%); default rates of NSP were 11% and default rates of retreatment cases were 26–28%.[5] Treatment in this district is related to default and it should be unfolded. This will help the program managers to take required steps to place the defaulters into treatment in right time to reduce transmission, morbidity and mortality due to TB.
Risk factors for default among NSP patients have been reported in several studies from India and abroad.[7,8,9,10,11,12] However, such studies in West Bengal are very few and probably no such study carried out in Darjeeling district.
With this background, the present study was conducted to assess the timing, characteristics, and distribution of the reasons for default with relation to some sociodemographic variables among new sputum–positive (NSP) TB patients at Darjeeling district.
Materials and Methods
An observational analytical case-control study was conducted in three randomly selected tuberculosis units (TUs) of Darjeeling district, West Bengal namely Siliguri, Kurseong, and Khoribari for 5 months; from August 2011 to December 2011. The study population was NSP pulmonary TB patients enrolled for treatment in the TB register from 1st Qtr’09 to 2nd Qtr’10 in those three TUs of Darjeeling district. Study tools were a pre-designed pre tested structured pro-forma and different registers of RNTCP (OPD Register, Laboratory register, Treatment cards, Tuberculosis Register). Study variables were some sociodemographic characteristics (age, gender, marital status, education, occupation, residence, per capita monthly income, smoking habit, alcohol consumption) and some treatment-related variables (time of default, main cause of default, retrieval action, distance of DOT center, type of DOT provider, pre-treatment counseling, adverse reaction of anti TB drugs, number of missed doses, knowledge about TB, initial home visit, migration, patient provider interaction, overlapping working hours). Study technique was face-to-face interview of the study population. The inclusion criteria were NSP TB patients, not seriously ill, and gave informed written consent whereas the exclusion criteria were new extra-pulmonary TB patients (CAT I), NSN pulmonary TB patients (CAT I), previously treated TB patients (CAT II), MDR-TB patients, seriously ill patients and who did not gave informed written consent.
For case control study of 5% level of significance,[12] Power 80%,[13] two-sided test with anticipated adjusted odds ratio of 2.5[14] and exposure of non-defaulted of 20%,[14] which means patients with at least five missed dosages, a sample size of 79 cases and 79 controls were estimated.[15] Six TUs of Darjeeling district report on an average 25 defaulted NSP TB cases annually. So, three to four randomly selected TUs were required.
Selection of cases and controls were done as follows: NSP Patients registered from 1st Qtr’09 to 2nd Qtr’10 as treatment category I with a recorded treatment outcome of default from the TB register were the cases. Patients registered as a NSP case, who completed the treatment irrespective of final sputum result, were the controls. They included cured and treatment completed groups. For every case of default identified, the next patient who completed the treatment was selected as a control. Case and control ratio was 1:1 and age and sex matching were done.
Data collection technique was as follows: After obtaining ethical clearance from the Ethical Committee of All India Institute of Hygiene and Public Health (AIIH and PH), Kolkata, Peripheral Health Workers (PHWs)/Multipurpose Workers (MPWs)/Public Health Nurse (PHN)/Senior Treatment Supervisors (STS)/Senior TB Laboratory Supervisors (STLS) were trained in data collection at the office of the District Tuberculosis Officer (DTO) by a primary investigator (PI) with prior permission from Chief Medical Officer of Health (CMOH), Darjeeling district. Relevant information were collected from the TB registers/laboratory the registers/treatment cards. Patients’ addresses were retrieved and patients were interviewed at their residence. They were explained about the purpose of the study; assured about confidentiality and anonymity; informed written consent was obtained from them, then enrolled cases and controls were interviewed. In case of absence at residence, an attempt was made to contact the cases and controls at least thrice. To maintain the quality of data, 20% of the study population was re-interviewed by primary investigator as a method of cross check.
Data analysis was done using following methods: The data were scrutinized for completeness; all records were keyed twice. Finally, the collected data were tabulated, analyzed and interpreted by proper statistical methods (proportions, univariate and multivariate analysis). Mantel-Haenszel Crude Odds Ratios (OR) and 95% confidence Intervals (CI) were calculated for the interpretation of univariate analysis. P values of <0.05 were considered statistically significant. To identify the independent risk factors for default, adjusted odds ratios (AOR) and 95% CIs were calculated. The statistical analyses were performed using Microsoft Excel 2010 (Microsoft Corp, Redmond, WA, USA), Epi-info 6.04d (Centers for Disease Control and Prevention, Atlanta, GA, USA, 2001) and SPSS 15 (Chicago, IL, 2006).
Operational definitions
Smear-positive pulmonary TB; cured; treatment completed; defaulted; DOT provider; Initial home visit; retrieval action: As per standard definition of RNTCP.[2]
Pretest and pretreatment counseling: For TB diagnosis, treatment initiation and treatment continuation – counseling done when the client comes for the test results and before TB treatment initiation for those who test positive.[16]
DOT center: The place of consumption of anti-TB drugs under supervision by a designated provider.
Literate: A person can be considered literate if he/she can read and write with understanding in any language and he/she should be 7 years and above.[17]
Smoker: Smoking at least 100 cigarettes in their lifetime and who, at the time of survey, smoked either every day or some days.[18]
Alcohol consumption: Patients who said they habitually drunk alcohol every day during the study period were considered to be alcoholic for the purpose of this study.
Knowledge about TB: The overall knowledge was assessed based on the response to twelve (12) TB-related questions. Correct answers were given a value of one (1) and incorrect answers were given a value of zero (0). Knowledge was categorized as satisfactory or unsatisfactory based on the cumulative result and the related mean value of responses.
Results
Sociodemographic factors of the study population
About 63.29% of the study population consisted of males; 27.84% were within 25-35 years of age group; followed by 45-55 years and 55-65 years (18.99% each); mean age was 38.22 years; median age was 40.08 years; 29.11% were from hilly area and 70.89% were from plain area. As per the educational status concerned; 42.41% were illiterate; 9.49% read up to primary level; 28.48% secondary passed; 14.57% higher secondary passed; graduate and post graduate were 3.79% and 1.26%, respectively. Occupational distribution showed that 3.67% were unemployed; 11.39% were unskilled laborers; 29.12% were skilled laborers; 6.96% were housewives; 7.59% had business; and 1.26% had service. About 81.64% had Per Capita Monthly Income (PCMI) below Rs. 3000/; followed by 12.03% (between Rs. 3000/and 5000/); 4.43% (between Rs. 5000/and 10000/); 1.27% (between Rs. 10,000/and 15,000/); and 0.63% (more than Rs. 15,000/), respectively.
Time of default
About 75% of the default occurred in the intensive phase i.e., within 0–2 months (34% between 0 and 1 month and 41% between 1 and 2 months, respectively); rest 25% default occurred within 2–4 months (20% between 2 and 3 months and 5% between 3 and 4 months, respectively).
Causes of default
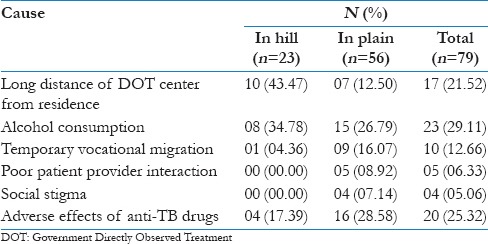
Most commonly cited reasons for default were alcohol consumption, adverse effects of anti-TB drugs, long distance of DOT center from residence, temporary vocational migration, poor patient provider interaction, and social stigma [Table 1].
Table 1.
Distribution of cases according to main cause of default (n=79)
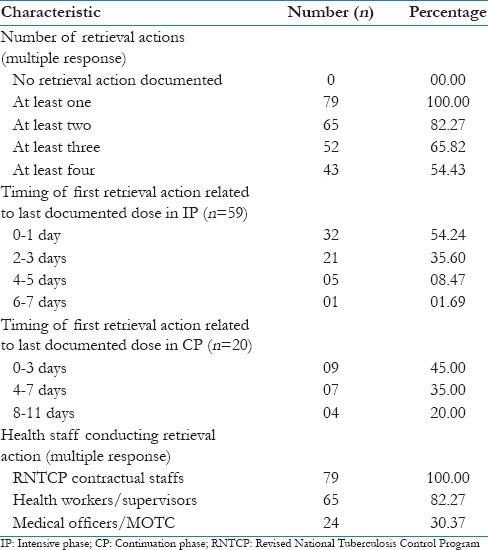
Retrieval action by the program
Zero retrieval action was not documented, retrieval was not delayed by more than 1 week in IP and 11 days in CP. Almost one third of the documented retrieval actions were undertaken by medical officers and cent per cent by the contractual TB program staffs [Table 2].
Table 2.
Retrieval actions by the program after treatment interruptions (n=79)
Univariate analysis
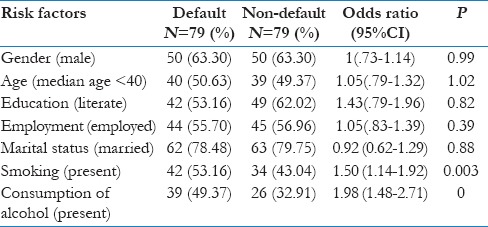
Patient-related risk factors for default
Univariate analysis of these factors revealed significant association of default with smoking and alcoholism and no significant differences between defaulted and non-defaulted groups for any other sociodemographic factors were found [Table 3].
Table 3.
Univariate analysis of sociodemographic risk factors among defaulted and treatment completed patients (N=157)
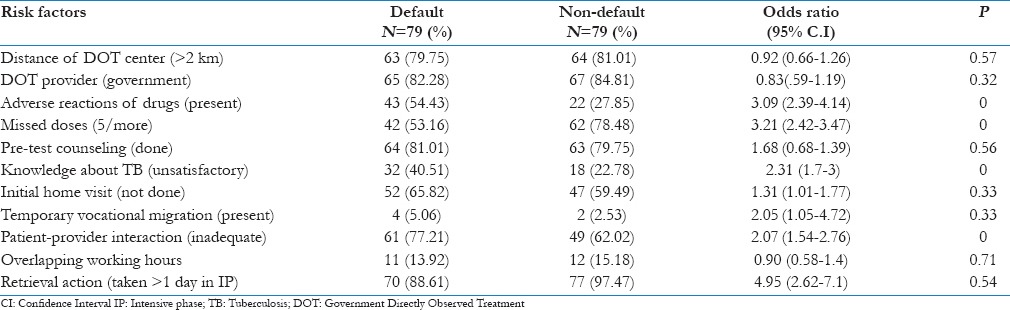
Treatment related risk factors for default
In the overall univariate analysis, factors significantly associated with default were poor knowledge regarding TB, inadequate patient provider interaction, patients with 5 or more missed doses, and side effects of anti-TB drugs. For factors like distance of DOT center >2 km, type of DOT provider, and overlapping working hours were showing OR less than one. Pre-treatment counseling, no initial home visit, temporary vocational migration, and retrieval action >1 day in IP were showing OR more than 1, but P values were more than 0.05 [Table 4].
Table 4.
Univariate analysis of treatment-related risk factors among defaulted and treatment completed patients (N=157)
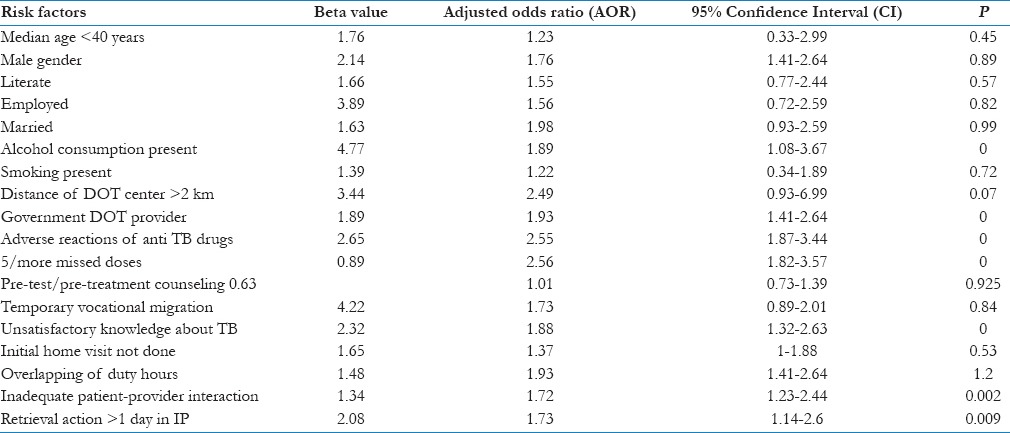
Multivariate analysis
Poor knowledge was more in defaulted patients than in patients who were not defaulted. Poor patient provider interaction was a potential risk factor for default. Proportion of patients with five or more missed doses during the treatment was significantly higher among the defaulted group. Adverse effects to anti-TB drugs were reported by higher proportion of patients in defaulted than in completed group. Although no significant association was found in univariate analysis for type of DOT provider and retrieval action in IP; multivariate analysis showed positive association, more in case of Government DOT providers and patients who were not retrieved in IP within 24 hours. Some other factors like distance of DOT center, overlapping working hours of the patient, no initial home visit, and pre-treatment counseling were showing A.O.R more than 1 with a P value more than 0.05 [Table 5].
Table 5.
Multivariate analysis of risk factors for default
Discussion
The question often arises why some patients complete treatment successfully while others don’t under comparable conditions.[7] Seeking answer in this direction, a comparison was made between the defaulted and completed group of TB patients regarding the sociodemographic and treatment-related risk factors, using a case control study with a logistic risk model.
In this study, most defaults occurred early; 75% in the IP and 25% in the CP which was corroborative with the findings of some previous studies.[9,12,19,20,21] However, these findings differ from other settings, which showed the tendency of default at the later phase of treatment.[22,23,24,25,26]
In the present study, retrieval was not delayed by more than 1 week in IP. However, in some studies, efforts to retrieve treatment interrupters were found to be weak and far below program guidelines.[20]
As per the RNTCP guidelines, staff of the general health system maximally participates in default retrieval efforts. In our study, 30.37% of the documented retrieval actions were undertaken by medical officers and 100% by the contractual TB program staffs, which was far above than other previous studies.[20]
Most commonly cited reasons for default were migration, adverse effects of anti-TB drugs, consumption of alcohol, long distance of DOT center from residence, social stigma, similar in the present study and other studies.[9,20,21,24,26]
In the overall logistic regression analysis, the patient related and treatment-related factors independently associated with default were consumption of alcohol, inadequate knowledge about TB, inadequate patient provider interaction, instances of missed doses, adverse reactions of anti-TB drugs, Government DOT provider, retrieval action more than 1 day, and smoking.
Alcoholism has been identified as an important predictor of non-compliance in several studies in India and abroad.[7,8,9,10,11,12] Recurring use of alcohol leads to forgetting taking of anti-TB drugs and eventual default. Besides, alcohol is injurious to liver, potentiating the hepatic effects of anti-TB drugs.[12] Elicitation of history of alcoholism prior to treatment initiation will help in identifying potential defaulters needing special attention during treatment.[12] However, some studies didn’t find significant association between default and alcoholism.[19]
It was observed that more than one fourth of defaulted patients stopped treatment because of toxicity of drugs, which was also strongly supported by logistic analysis. Some previous studies in India and different parts of world also supported this view.[7,12,19,20,21,22,23,24,25,26,27,28,29] One of the reasons for higher incidence of perceived side effects perhaps could be the continued practice of giving medication on empty stomach.[7] Frequently reported minor side effects can be successfully dealt with proper instructions on drug consumption, reassurance to patients and prompt symptomatic treatment before it leads to default.[7]
We found a significant association between smoking and defaulter, which has also been reported previously.[9,10,11,19,26]
Effective patient provider interaction is a means of providing treatment-related information: Importance of DOT and clearing the doubts regarding disease and treatment. This plays an important role in enhancing treatment compliance.[7] Poor patient provider interaction has also been reported as a risk factor in studies elsewhere.[7,12,24,25,26,27,28,29,30]
It is encouraging to note that in the present study, more than two third of patients who underwent treatment, had satisfactory knowledge about various aspects of TB. This study also revealed that the compliance of DOT was significantly high among those who had good knowledge about the disease which was in tune with other studies.[7,12,19,23,25,27,30]
Type of DOT provider play an important role; patients who were observed by Government DOT providers, defaulted more than that of observed by volunteers; because community DOT providers get their honorarium only after completion of treatment. Moreover, the problems like overlapping of duty hours and distance of the DOT center can be well tackled by social workers.[19,21,27,28,29,30]
Instances of missed doses was also a significant factor in the present study and other studies.[7]
Our study revealed that other sociodemographic factors (age, gender, education, occupation and marital status) were not associated significantly with default, similar to few other studies in India.[7,19,27,29] However, in some studies[9,10,11,12,20,21,23,24,30] young adult and elderly, male gender, unmarried, education lower than secondary level, and unemployment were the predictors of default.
Like other studies, our study also had some limitations. These are: To some extent, recall bias might occur which is the limitation of any retrospective study. This study was done in a hilly district of West Bengal. Out of six TUs, only three TUs were taken for this study considering feasibility. Thus, the results obtained can’t be extrapolated in general/wider sense. Moreover, though the interviewers were trained before data collection, the questions about reasons for default were a multifactor issue that is difficult to explore in depth. Decision was made to ask the main reason for default, which on the one hand over-simplifies the question, but on the other hand, is likely to improve reliability. Lastly only the patients attended for treatment at public health system were included in the study. As many TB patients go to the private practitioners, these data were missing in this study; so the problem of default was under-estimated.
Conclusions
In this study most defaults occurred in the IP. So pre-treatment counseling and initial home visit play an important role in this regard. Zero retrieval action was not documented; retrieval was not delayed by more than 1 week in IP; cent per cent of the documented retrieval actions were undertaken by the contractual TB program staffs. The most commonly cited reason for default was migration. In the overall logistic regression analysis, the factors independently associated with default were consumption of alcohol, unsatisfactory knowledge about TB, inadequate patient provider interaction, instances of missed doses, adverse reactions of anti-TB drugs, Government DOT provider, retrieval action more than 1 day, and smoking. During pre-treatment counseling, following aspects need to be emphasized: Duration of treatment, importance of completion of treatment, adverse effect of drugs etc. Also, patients using alcohol need to be kept under strict monitoring and should be given repeated counseling.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare, Nirman Bhavan, New Delhi. TB India 2014. Revised National TB Control Programme. Annual Status Report. Reach the Unreached. Find, Treat, Cure TB, Save Lives. 2014. [Last accessed on 2014 Dec 26]. pp. 7–59. Available from: http://www.tbcindia.nic.in .
- 2.New Delhi: Training Module for Medical Practitioners. Administaring Treatment; 2010. Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare, Nirman Bhavan; pp. 26–56. [Google Scholar]
- 3.Kolappan C, Subramani R, Kumaraswami V, Santha T, Narayanan PR. Excess mortality and risk factors for mortality among a cohort of TB patients from rural South India. Int J Tuberc Lung Dis. 2008;12:81–6. [PubMed] [Google Scholar]
- 4.Chandrasekaran V, Gopi PG, Santha T, Subramani R, Narayanan PR. Status of re-registered patients for tuberculosis treatment under DOTS programme. Indian J Tuberc. 2007;54:12–6. [PubMed] [Google Scholar]
- 5.Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare, Nirman Bhavan, New Delhi. TB India 2014. Revised National TB Control Programme. Annual Status Report 2014. State and District Wise Annualized Performance. 2013:68–170. [Google Scholar]
- 6.Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India, New Delhi. TB India 2011. Revised National TB Control Programme. Annual Status Report. 2011:113. [Google Scholar]
- 7.Vijay S, Kumar P, Chauhan LS, Vollepore BH, Kizhakkethil UP, Rao SG. Risk Factors Associated with Default among New Smear Positive TB Patients Treated Under DOTS in India. PLoS One. 2010;5:e10043. doi: 10.1371/journal.pone.0010043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vijay S, Balasangameshwara VH, Jagannatha PS, Saroja VN, Kumar P. Defaults among Tuberculosis Patients treated under DOTS in Bangalore City – A search for solution. Indian J Tub. 2003;50:185–95. [Google Scholar]
- 9.Santh AT, Garg R, Frieden TR, Chandrasekaran V, Subramani R, Gopi PG, et al. Risk factors associated with default, failure and death among tuberculosis patients treated in a DOTS programme in Tiruvallur District, South India, 2000. Int J Tuberc Lung Dis. 2002;6:780–8. [PubMed] [Google Scholar]
- 10.Jakubowiak WM, Bogorodskaya EM, Borisov ES, Danilova DI, Kourbatova EK. Risk factors associated with default among new pulmonary TB patients and social support in six Russian regions. IntJ Tuberc Lung Dis. 2007;11:46–53. [PubMed] [Google Scholar]
- 11.PinidiyaPathirage J, Senaratne W, Wickremasinghe R. Prevalence and predictors of default with tuberculosis treatment in Sri Lanka. Southeast Asian J Trop Med Public Health. 2008;39:1076–82. [PubMed] [Google Scholar]
- 12.Muture BN, Keraka MN, Kimuu PK, Kabiru EW, Ombeka VO, Oguya F. Factors associated with default from treatment among tuberculosis patients in Nairobi province, Kenya: A case control study. BMC Public Health. 2011;11:696–700. doi: 10.1186/1471-2458-11-696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lemeshow S, Hosmer DW, Klar J, Lwanga SK. WHO/HST/ESM/86. United States: John Wiley and Sons; 1990. Adequacy of sample size in health studies; p. 1. [Google Scholar]
- 14.Suresh KP, Chandrashekara S. Sample size estimation and power analysis for clinical research studies. J Hum Reprod Sci. 2012;5:7–13. doi: 10.4103/0974-1208.97779. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Dupont WD, Plummer WD., Jr Power and Sample Size Calculations: A Review and Computer Program. Control Clin Trials. 1990;11:116–28. doi: 10.1016/0197-2456(90)90005-m. [DOI] [PubMed] [Google Scholar]
- 16.PATH. Interpersonal Communication and Counselling for Clients on TB. Part III. Counseling on TB. [Last accessed on 2015 Jun 11]. p. 73. Available from: http://www.path.org/publications/files/CP_ukraine_tb_hiv_ipcc_3.pdf .
- 17.Park K. Demography and Family Planning. 22nd ed. Jabalpur: Banarsidas Bhanot Publishers; 2013. Park's Textbook of Preventive and Social Medicine; p. 447. [Google Scholar]
- 18.Centers for Disease Control and Prevention. State-specific second hand smoke exposure and current cigarette smoking among adults–United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:1232–5. [PubMed] [Google Scholar]
- 19.Chang KC, Leung CC, Tamrisk CM. Risk factors for defaulting from anti-tuberculosis treatment under directly observed treatment in Hong Kong. Int J Tuberc Lung Dis. 2009;8:1492–8. [PubMed] [Google Scholar]
- 20.Jha UM, Satyanarayana S, Dewan PK, Chadha S, Wares F, Sahu S, et al. Risk Factors for Treatment Default among Re-Treatment Tuberculosis Patients in India, 2006. PLoS One. 2010;5:e8873. doi: 10.1371/journal.pone.0008873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jain S, Bhagyalaxmi A, Kadri AM. Defaulter rate and associated factors among the tuberculosis patients treated under DOTS in Ahmedabad city. Indian J Prev Soc Med. 2012;43:158–64. [Google Scholar]
- 22.Kruk ME, Schwalbe NR, Aguiar CA. Timing of default from tuberculosis treatment: A systematic review. Trop Med Int Health. 2008;13:703–12. doi: 10.1111/j.1365-3156.2008.02042.x. [DOI] [PubMed] [Google Scholar]
- 23.Tekle B, Mariam DH, Ali A. Defaulting from DOTs and its determinants in three district of Arsi Zone in Ethiopia. Int J Tuberc Lung Dis. 2007;6:573–6. [PubMed] [Google Scholar]
- 24.Gopi PG, Vasantha M, Muniyandi M, Chandrasekaran V, Balasubramanian R, Narayanan PR. Risk factors for non-adherence to directly observed treatment (DOT) in a rural tuberculosis unit, South India. Indian J Tuberc. 2007;54:66–70. [PubMed] [Google Scholar]
- 25.Shargie EB, Lindtjørn B. Determinants of Treatment adherence among Smear-Positive Pulmonary Tuberculosis Patients in Southern Ethiopia. PLoS Med. 2007;4:e37. doi: 10.1371/journal.pmed.0040037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahmad SR, Velhal GD. Study of treatment interruption of new sputum smear positive TB cases under DOTS strategy. Int J Med Sci Public Health. 2014;3:977–81. [Google Scholar]
- 27.Pandit N, Choudhary SK. A Study of Treatment Compliance in Directly Observed Therapy for Tuberculosis. Indian J Community Med. 2006;31:241–3. [Google Scholar]
- 28.Jaiswal A, Singh V, Ogden JA, Porter JD, Sharma PP, Sarin R, et al. Adherence to tuberculosis treatment: Lessons from the urban setting of Delhi, India. Trop Med Int Health. 2003;8:625–33. doi: 10.1046/j.1365-3156.2003.01061.x. [DOI] [PubMed] [Google Scholar]
- 29.Liam CK, Lim KH, Wong CM, Tang BG. Attitude and knowledge of newly diagnosed tuberculosis patients regarding the disease, and factors affecting treatment compliance. Int J Tuberc Lung Dis. 1999;3:300–9. [PubMed] [Google Scholar]
- 30.Dandona R, Dandona L, Mishra A, Dhingra S, Venkatagopalakrishna K, Chauhan LS. Utilization of and barriers to public sector tuberculosis services in India. Natl Med J India. 2004;17:292–9. [PubMed] [Google Scholar]


