Abstract
Background:
The prevalence of gestational diabetes is on the rise. Understanding the various outcomes of it is necessary to face this challenge.
Objectives:
To study the frequency of occurrence of various maternal and fetal outcomes among gestational diabetes patients.
Methods:
This is a retrospective cohort study conducted in rural Kerala, a southern state of India. The study participants were followed up for a period of 4 years, from 2007 to 2011. The participants included 60 women with gestational diabetes and 120 women without gestational diabetes. Gestational diabetes was the major exposure variable. The frequencies of various outcomes were computed. Multivariable logistic regression was done to compute the risk for various outcomes in gestational diabetes.
Results:
The major outcomes included termination of pregnancy by caesarean section, long-term progression to type 2 diabetes, in-born nursery (IBN) admissions and increased neonatal birth weight. The maximum adjusted RR [13.2 (1.5-116.03)] was for the development of type 2 DM later.
Conclusion:
Gestational diabetes can result in significant feto-maternal outcomes; so better facilities are needed to manage gestational diabetes.
Keywords: Gestational diabetes, pregnancy outcome, retrospective cohorts
Background
Gestational diabetes is a condition characterized by glucose intolerance that particularly develops during pregnancy. There has always been a dilemma among the clinicians to diagnose gestational diabetes. Several criteria have been proposed by various societies across the world. To bring in uniformity the WHO brought out the guidelines in 1999 that was updated in 2006 and this was being followed largely. In 2013, the WHO has revised and formulated the new set of diagnostic criteria for gestational diabetes.[1] These new range of values were devised based on the risk of adverse feto-maternal outcomes.
Irrespective of the ambiguity in the diagnostic values, there is ample evidence to suggest the increasing prevalence of gestational diabetes.[2,3] There is wide region to region variation in prevalence ranging from 2.5% to 21%.[4,5,6,7] The prevalence has also been noted to be different across the sociodemographic and economic strata. Various studies point out the ethnic differences in the prevalence of gestational diabetes. Asian women, especially those having Indian ethnicity, have been undoubtedly proved to be more at risk for this condition.[2,8]
In India the prevalence of gestational diabetes varies widely geographically. Studies conducted in southern part of the country reveal a bigger burden of gestational diabetes than the northern states.[7,9,10] The regional differences in the prevalence of gestational diabetes is in correlation with that of type 2 diabetes. The risk of developing type 2 diabetes mellitus is high for the patients with gestational diabetes.[11]
Kerala is a state which is currently facing a huge burden of diabetes mellitus. Increasing prevalence of gestational diabetes will make a major contribution to the diabetic pool of this state. Moreover, a significant proportion of the women belonging to the reproductive age group in Kerala are overweight and obese.[12] High BMI is a proven risk factor to develop gestational diabetes.[13,14,15] In the setting of high prevalence of type 2 diabetes, these women also are prone to have a positive family history which also adds to the risk of gestational diabetes.[13] It is inevitable for the state's health system to be equipped to face the consequences of the burgeoning burden of gestational diabetes in the near future. Understanding the various outcomes of gestational diabetes would be the key to initiate the cascade of preparatory steps to tackle them. Studies are available from various parts of the country signifying the adverse maternal and neonatal outcomes of gestational diabetes. However, similar studies from Kerala setting are scarce. This study therefore aims to study the frequency of the occurrence of various maternal and fetal outcomes among gestational diabetes patients.
Materials and Methods
This retrospective cohort study included a total of 180 individuals. These participants were taken from the database of INDADE (Indo Danish Collaboration on Diabetes Epidemiology) study, a community prospective cohort study conducted in rural Kerala. This study is a collaborative research program between Health Action by People (HAP), a non-profit research organization in Kerala and University of southern Denmark. The INDADE study included 25,000 subjects and it was aimed to understand the epidemiology of diabetes mellitus. The residents of a Local Self Government Unit (Ottoor Panchayath) in southern Kerala were the study participants. They were followed up for a period of 4 years, from 2007 to 2011. Ottoor Local Self Government unit belongs to the rural area of Thiruvananthapuram district in Kerala. After recording their baseline anthropometric measurements and fasting blood sugar levels, individuals aged above 20 years were being followed up. Annual medical examination and biochemical investigations were performed among the diabetic individuals. The current analysis was conducted in 2010, for which the baseline data collected in 2007 were retrieved from the records of INDADE study. These included their personal identification details, educational qualification, occupation, anthropometric measurements like weight, height, waist and hip circumference, and FBS values. The participants included 60 women with gestational diabetes and 120 women who were pregnant but without gestational diabetes. The details of their antenatal period and the pregnancy outcomes were collected through telephonic interview using a semi-structured questionnaire. Interviewers were trained to conduct interviews in a uniform manner. The questionnaire included their glycemic status, details of the treatment, mode of delivery, delivery complications, pre-mature births, still births, abortions, birth weight of the child, neonatal ICU admissions and persistence of hyperglycemia after delivery.
Gestational diabetes was the major exposure variable. All quantitative variables have been summarized using mean (SD) and qualitative variables in proportions. We analyzed the feto-maternal outcomes of the patients with gestational diabetes. Bivariate analysis was done using the Chi-square test. A P value less than 0.05 was considered to be statistically significant. Multivariable logistic regression was done to compute the risk for various outcomes in gestational diabetes as compared to those without gestational diabetes. Analysis was done using SPSS software, version 16.
Results
A total of 180 individuals were included in the study of which 60 had gestational diabetes and 120 did not. The mean (SD) age of the study group was 32 (7.8) years. Majority of them [160 (89.8%)] had an educational qualification above the high school level. Most of the participants [157 (87.2%)] were home makers. The baseline characteristics which were measured in 2007, of those with gestational diabetes have been compared with those without gestational diabetes in Table 1.
Table 1.
Baseline characteristics of gestational diabetic individuals as compared to those without gestational diabetes
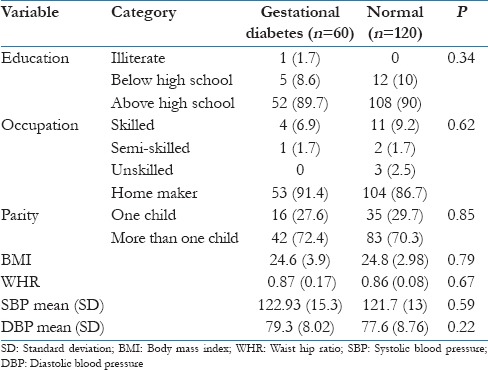
The baseline fasting blood sugar value done at the start of the study was on the higher side for gestational diabetes patients with a mean (SD) of 91 (37.6) mg/dl as compared to 84 (16.4) mg/dl for those without gestational diabetes. However, this difference was not statistically significant. The mean BMI of this study group was 24.7 (3.5) kg/m2. More than one fourth of these individuals [50 (27.8%)] had BMI above 25 kg/m2. The mean (SD) waist-hip ratio of the diabetic individuals was higher [0.87 (0.16)] than that of the non-diabetic individuals [0.86 (0.08)], but the difference was not statistically significant.
Nearly half [28 (48.3%)] of 60 individuals who had gestational diabetes had a positive family history for type 2 diabetes. Most of the gestational diabetic patients [42 (70%)] were multi-gravida. Majority of them [41 (68.3%)] had developed gestational diabetes during the first pregnancy itself. Insulin therapy had to be initiated for 26 (43.3%) patients. A few of the patients with gestational diabetes [12 (21.1%)] also had associated hypertension during pregnancy. Mode of delivery was by caesarean section for 19 (32.8%) individuals. It was noted that more than half of those who underwent caesarean section [10 (52.6%)] were on insulin therapy.
The outcome of the pregnancy ended in abortion for 11 (19%) of individuals. Birth weight of the newborns was above 3 kg in more than half [31 (51.7%)] of these individuals. In-born nursery (IBN) admission was warranted for neonates of seven (12.1%) patients. The various feto-maternal outcomes of the 60 individuals with gestational diabetes are given in Table 2. The adjusted risk for progression to overt diabetes after delivery, babies with birth weight more than 3 kg and IBN admissions of the neonates, was significantly more for those with gestational diabetes [Table 3].
Table 2.
Feto-maternal complications among patients with gestational diabetes (n=60)
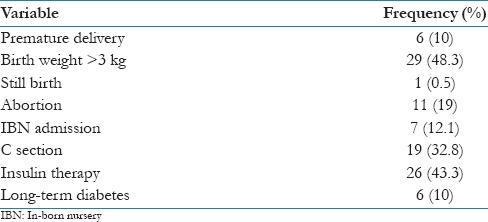
Table 3.
Adjusted relative risk for developing complications among GDM patients as compared to non GDM individuals
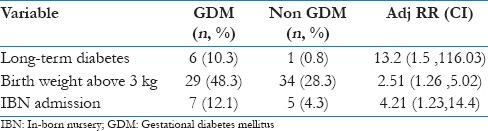
The progression to type 2 diabetes was observed in six (10%) of the gestational diabetes patients. They were significantly older than the rest of the gestational diabetic with the mean (SD) age being 37 (7.2) years (P = 0.006). The mean (SD) baseline fasting blood glucose value for them was 130 (92.3) mg/dl which was much higher than the rest of the group (P = 0.001). Out of these six individuals who progressed to type 2 DM, four (66.7%) had given birth to babies with birth weight more than 3 kilograms. The mode of delivery was through caesarean section for 5 (83.3%) out of 6 of these patients. This association was found to be statistically significant (P = 0.005).
Discussion
This study brings into light the various maternal and neonatal outcomes of gestational diabetes. Delivering the child through surgical intervention and progression to type 2 diabetes mellitus were the major maternal outcomes. Major neonatal outcomes included increased birth weight, IBN admissions, premature deliveries and abortions. Evidence generated from other parts of the country supports the results in this study.[10,11]
Long-term progression to type 2 diabetes has far reaching implication in this study setting. The prevalence of type 2 diabetes is as high as 20% in Kerala.[16] It is a known fact that the intrauterine hyperglycemic status in gestational diabetes increases the risk for type 2 diabetes in future.[11,17,18] Even the molecular aspects of progression to type 2 diabetes has been studied in detail among gestational diabetes patients. The endothelial irregularities found in diabetic vasculopthic patients was detected in the fetal placenta of gestational diabetic individuals.[19] This suggests that the origin of diabetic complication is seen right from the fetus of gestational diabetic women. The population of Kerala is highly vulnerable for the development of type 2 diabetes with the alarming prevalence of other risk factors such as obesity, unhealthy dietary habits, sedentary lifestyle and a positive family history.[20] Hence, the early detection and control of gestational diabetes become a mandate in controlling the unprecedented increase in the type 2 diabetes burden of the state.
The rate of caesarean section in the state is considerably high than the rest of the country.[21,22] This study highlights that more than 32% of the gestational diabetes patients had to undergo caesarean section to terminate their pregnancy. Big baby which is an outcome of gestational diabetes is an indication for caesarean section. Similar studies done in other parts of the world also concludes that women with gestational diabetes are more at risk for caesarean sections.[23] More than half of those who underwent caesarean section were on insulin therapy for uncontrolled glycemic status. Regular monitoring of blood glucose and its strict control reduces the risk of surgical interventions and can facilitate normal deliveries. Simple interventions like this could reduce the rate of caesarean section in the state.
Health indicators in Kerala are the best in the country and are at par with the developed nations. The most important health indicator suggestive of the system of health care of a region is the infant mortality rate (IMR). It reflects the development of the region as a whole. According to Sample Registration System (SRS) 2011 data, the IMR in Kerala is 12 which is much lower than the national average of 44.[24] Neonatal deaths takes up the major share of infant mortality. A study done in central Kerala reveals that neonatal mortality accounts for 58% of childhood mortality in that area. Preterm births are an important cause of neonatal mortality. This study reveals the prevalence of preterm delivery to be 10% among gestational diabetes patients. IBN admissions were required for 12% of the neonates of these patients. The need for improving the neonatal care facilities in the states health care infrastructure is being brought into light here. The development of neonatal health care facilities is inevitable to further bring down the state's IMR from the static figure of 12.
Conclusion
This study concludes that the major feto-maternal outcomes of gestational diabetes are long-term progression to type 2 diabetes, increased birth weight and increased IBN admissions for neonates. In the present health milieu of the state these findings are of utmost importance. The burden of gestational diabetes is only going to increase in the near future. Cautious attention therefore must be given to devise measures to tackle the challenges of gestational diabetes. Awareness to achieve good glycemic control and to prevent progression to type 2 diabetes must be given to these women. The Government should largely take up the responsibility of improving the neonatal care facilities of the state to handle the neonatal outcomes of gestational diabetes.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Geneva: World Health Organization; 2013. [Last Accessed on 2014 Sep 18]. World Health Organization. Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy. Published 2013. Available from: http://www.who.int/iris/handle/10665/85975 . [PubMed] [Google Scholar]
- 2.Ferrara A. Increasing prevalence of gestational diabetes mellitus. A public health perspective. Diabetes Care. 2007;30:141–6S. doi: 10.2337/dc07-s206. [DOI] [PubMed] [Google Scholar]
- 3.Anna V, Van Der Ploeg HP, Cheung NW, Huxley RR, Bauman AE. Sociodemographic correlates of the increasing trend in prevalence of gestational diabetes mellitus in a large population of women between 1995 and 2005. Diabetes Care. 2008;31:2288–93. doi: 10.2337/dc08-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmidt MI, Duncan BB, Reichelt AJ, Branchtein L, Matos MC, Costa e Forti A, et al. For the Brazilian Gestational Diabetes Study Group. Gestational diabetes mellitus diagnosed with a 2-h 75 gm oral glucose tolerance test and adverse pregnancy outcomes. Diabetes Care. 2001;24:1151–5. doi: 10.2337/diacare.24.7.1151. [DOI] [PubMed] [Google Scholar]
- 5.Seshiah V, Balaji V, Balaji MS, Sanjeevi CB, Green A. Gestational diabetes mellitus in India. J Assoc Physicians India. 2004;52:707–11. [PubMed] [Google Scholar]
- 6.Zargar AH, Sheikh MI, Bashir MI, Masoodi SR, Laway BA, Wani AI, et al. Prevalence of gestational diabetes mellitus in Kashmiri women from the Indian Subcontinent. Diabetes Res Clin Pract. 2004;66:139–45. doi: 10.1016/j.diabres.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 7.Seshiah V, Balaji V, Balaji MS, Paneerselvam A, Arthi T, Thamizharasi M, et al. Prevalence of gestational diabetes mellitus in South India (Tamil Nadu) - a community based study. J Assoc Physicians India. 2008;56:329–3. [PubMed] [Google Scholar]
- 8.Harrison C, Bayram C, Britt H. Gestational diabetes. Aust Fam Physician. 2013;42:523. [PubMed] [Google Scholar]
- 9.Rajput R, Yadav Y, Nanda S, Rajput M. Prevalence of gestational diabetes mellitus and associated risk factors at a tertiary care hospital in Haryana. Indian J Med Res. 2013;137:728–33. [PMC free article] [PubMed] [Google Scholar]
- 10.Nayak PK, Mitra S, Sahoo JP, Daniel M, Mathew A, Padma A. Feto-maternal outcomes in women with and without gestational diabetes mellitus according to the International Association of Diabetes and Pregnancy Study Groups (IADPSG) diagnostic criteria. Diabetes Metab Syndr. 2013;7:206–9. doi: 10.1016/j.dsx.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 11.Mahalakshmi MM, Bhavadharini B, Kumar M, Anjana RM, Shah SS, Bridgette A, et al. Clinical profile, outcomes, and progression to type 2 diabetes among Indian women with gestational diabetes mellitus seen at a diabetes center in south India. Indian J Endocrinol Metab. 2014;18:400–6. doi: 10.4103/2230-8210.131205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.India: National Family Health Survey; [Last accessed on 2014 Sep 18]. Key indicators of Kerala from NFHS-3. NFHS-3 fact sheets for key indicators based on final data. Available from: http://www.rchiips.org . [Google Scholar]
- 13.Bhat M, K N R, Sarma SP, Menon S, C V S, S GK. Determinants of gestational diabetes mellitus: A case control study in a district tertiary care hospital in south India. Int J Diabetes Dev Ctries. 2010;30:91–6. doi: 10.4103/0973-3930.62599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kale SD, Kulkarni SR, Lubree HG, Meenakumari K, Deshpande VU, Rege SS, et al. Characteristics of gestational diabetic mothers and their babies in an Indian diabetes clinic. J Assoc Physicians India. 2005;53:857–63. [PubMed] [Google Scholar]
- 15.Albareda M, Caballero A, Badell G, Piquer S, Ortiz A, de Leiva A, et al. Diabetes and abnormal glucose tolerance in women with previous gestational diabetes. Diabetes Care. 2003;26:1199–205. doi: 10.2337/diacare.26.4.1199. [DOI] [PubMed] [Google Scholar]
- 16.Baruah MP, Pathak A, Kalra S, Das AK, Zargar AH, Bajaj S, et al. A revisit to prevailing care and challenges of managing diabetes in India: Focus on regional disparities. Indian J Endocrinol Metab. 2014;18:254–63. doi: 10.4103/2230-8210.131113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huopio H, Hakkarainen H, Pääkkönen M, Kuulasmaa T, Voutilainen R, Heinonen S, et al. Long-Term changes in glucose metabolism after gestational diabetes: A double cohort study. BMC Pregnancy Childbirth. 2014;14:296. doi: 10.1186/1471-2393-14-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hayes C. Long-term prognostic factors in the diagnosis of gestational diabetes. Br J Nurs. 2009;18:523–4. doi: 10.12968/bjon.2009.18.9.42253. 526. [DOI] [PubMed] [Google Scholar]
- 19.Samuel R, Ramanathan K, Mathews JE, Seshadri MS. Back to the future: Examining type 2 diabetic vasculature using the gestational diabetic placenta. Diab Vasc Dis Res. 2014;11:363–5. doi: 10.1177/1479164114537509. [DOI] [PubMed] [Google Scholar]
- 20.Daivadanam M, Absetz P, Sathish T, Thankappan KR, Fisher EB, Philip NE, et al. Lifestyle change in Kerala, India: Needs assessment and planning for a community-baseddiabetes prevention trial. BMC Public Health. 2013;13:95. doi: 10.1186/1471-2458-13-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar GA. Antenatal history and caesarean section in the southern part of Kerala, India. World Health Popul. 2006;8:41–6. doi: 10.12927/whp.2006.17895. [DOI] [PubMed] [Google Scholar]
- 22.Mishra US, Ramanathan M. Delivery-related complications and determinants of caesarean section rates in India. Health Policy Plan. 2002;17:90–8. doi: 10.1093/heapol/17.1.90. [DOI] [PubMed] [Google Scholar]
- 23.Ovesen P, Jensen D, Damm P, Rasmussen S, Kesmodel US. Maternal and neonatal outcomes in pregnancies complicated by gestational diabetes. A nation-wide study. J Matern Fetal Neonatal Med. 2014;1:14. doi: 10.3109/14767058.2014.966677. [DOI] [PubMed] [Google Scholar]
- 24.Maternal and child mortality rates and total fertility rates. [Last accessed on 2014 Sep 20]. Available from: http://www.censusindia.gov.in .


