Abstract
Background:
To determine the prevalence of diabetes and pre-diabetes and to assess the risk factors associated with diabetes and pre-diabetes in the urban slums of Bangalore.
Materials and Methods:
A cross-sectional study was conducted in four slums of Bangalore in the age group of 35 years and above comprising of total 2013 subjects. Risk factors like age, sex, family history, behavior, physical activity, BMI, waist hip ration, diet habits were assessed to find their association with diabetes.
Results:
Prevalence of diabetes was 12.33% and of pre-diabetes was 11.57%. Prevalence was more among the females compared to males. Increasing age, over weight and obesity, sedentary life style, tobacco consumption, diet habits showed statistically significant association with prevalence of diabetes and pre-diabetes.
Conclusion:
Physical activity like regular exercises both at the office and at home, fibers-rich diet, blood sugar estimation after 35 years are some of the recommendations which can control diabetes.
Keywords: Diabetes, pre-diabetes, prevalence, risk factors
Introduction
Diabetes is fast becoming the epidemic of the 21st century.[1] Over the past 30 years, the status of diabetes has changed from being considered as a mild disorder of the elderly to one of the major causes of morbidity and mortality affecting the youth and middle-aged people.[2] It is estimated that 20% of global burden of diabetes is in South East Asian Region (SEAR), which will triple to 228 million by the year 2025 from the current 84 million.[3] World Health Organization (WHO) has projected the maximum increase in diabetes would occur in India.[4] The International Diabetes Federation (IDF) estimates the total number of diabetic subjects to be around 40.9 million in India and this is further set to rise to 69.9 million by the year 2025.[1] According to the National Urban Diabetes Survey, the prevalence of diabetes and pre-diabetes were 12.1% and 14%, respectively.[5] The Bangalore Urban Diabetes Study revealed that direct and indirect costs of diabetes care for patients undergoing treatment that involved hospitalization were approximately US$ 850 per patient per year. The cost of care is high and comparable to costs in other countries, especially if one keeps in mind the purchasing power parity.[6]
The present study was conducted with the objective of determining the prevalence of diabetes and pre-diabetes in the urban slum of Bangalore and also to assess the risk factors associated with the two conditions.
Material and Methods
This was a cross-sectional, community-based study among adults aged 35 years and above in four urban slums located in the central part of Bangalore. Screening was conducted by trained community health workers who conducted house to house visits for this purpose. Written informed consent was taken from the participants in the local language and the study was approved by ethics committee of the Art of Living Foundation.
House to house survey of people above 35 years in all the four slums yielded 2075 persons (total population 6127). People were eligible if they had been residing the study area for at least 2 years. Survey was conducted from 2012 November to March 2013. Three house visits were made in case the eligible participants were not available on the first visit. Participants who refused to participate or those who could not be contacted despite three house visits were taken as non-responders.
The information collection proforma contained details about the socio demographic factors, morbidity profile and anthropometric measurements. Social class was defined using standard of living index score described by Parasuraman et al. Participants were considered as tobacco user if they consumed any form of tobacco daily and as alcoholics if they consumed any form of alcoholic drink one or more times per day. Psychosocial stress was coded as “yes” if the study subjects reported that feeling sad, blue, or depressed for 2 weeks or more in a row during the past 12 months. Physical activity was categorized as sedentary, moderate and heavy depending on activity at the work place or at home and during leisure time. Blood sugar was measured using a free style Optium Glucometer (Glucometer was standardized cross checking laboratory result) and blood pressure measurement was conducted using a OMRON digital machine in the sitting position. Height and weight measurement, hip circumference, waist circumference were measured using standard techniques.
The prevalence of diabetes was defined to include all individuals with known diabetes and those in whom GRBS (Glucometer random blood sugar) was ≥ 200 mg/dL and fasting glucose ≥ 126 mg/dL. Pre-diabetics included those with GRBS between 140 and 199 mg/dL and fasting glucose between 100 and 125 mg/dL (ADA recommendation[7]). Hypertensive subjects were defined as those with known hypertension or with two average systolic BP readings > 140 mmHg and/or diastolic BP >90 mmHg (two readings measured 15 min duration apart) (JNC[8]). Body mass index (BMI) of all the participants was calculated using Quetlet's index (weight in kilograms/height2 in meters). Based on BMI participants were categorized into undernourished (BMI < 18.5 kg/m2); Normal (BMI =18.5 to 24.99 kg/m2); overweight (BMI =25 to 29.99 kg/m2); and Obese (BMI > 30 kg/m2). A waist circumference of >80 cm in females and 90 cm for males was considered as abnormal.
Participants who were diagnosed with diabetes and hypertension were referred to the project clinic which was conducted in the project area once in a month. After the interview participants were educated on symptoms, complications, treatment and prevention of diabetes using the flip chart.
The collected data were alphabetically and numerically coded and entered in Microsoft Excel 2007 and statistical analysis was done in SSPS version 19.0. Socio-demographic variables, morbidity profile and risk factor data were analyzed using descriptive statistics like frequencies, mean and standard deviation. Chi-square test of association or Fishers exact probability test was used as applicable to assess the association between diabetes/pre-diabetes and associated variables. Variables which exhibited a statistically significant association on univariate analysis were entered into a multiple logistic regression model with the presence of diabetes/pre-diabetes as the dependent variable and the associated variables as the independent variables. A P value of <0.05 was considered to be significant for all analyses.
Results
The total population of the four slums was 6127 out of which 2075 individuals were over the age of 35 years. A total of 13 individuals did not consent to participate in the study and 49 people could not be contacted despite three home visits. So a total of 2013 subjects above 35 years of age were interviewed and examined.
Out of a total of 2013 participants 1023 (50.8%) were females. Table 1 describes age and gender distribution of the study population. Majority belonged to the age group 35–44 years (44.70%) followed by 45–54 years (28.41%), with a mean age 47.82 years (S.D. 11.32061). About 64.48% of them belonged to the low socio-economic class (SLI score 0-15). Around one-third (30.6%) had BPL cards, whereas 31% of the participants (638) had no ration card. A vast majority (92.84%) of the study subjects did not have any form of health insurance and only 111 (5.51%) had ESI facility and 33 (1.63%) had availed private health insurance. Majority of the people worked as daily wage earners (51.16%) and most of the women were house wives (17.63%). Around half (51.31%) had no formal education and 21.85% people had completed high school.
Table 1.
Age and gender distribution of the study population
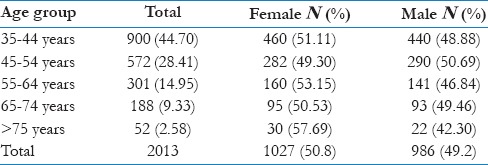
Table 2 describes the prevalence of diabetes and pre-diabetes in the study population. Out of the total of 2013 individuals above the age of 35 years, 197 (9.78%) were known diabetics among whom 95 (48.2%) had their blood sugars in the control range (<200 mg/dL RBS or <126 mg/dL FBS). A total of 59 (2.93%) participants were newly diagnosed to have diabetes. The overall prevalence of diabetes among those over the age of 35 years in our study was 12.33%. Among the 256 individuals with diabetes, 155 were females (60.54%) and 101 (39.45%) were males. The prevalence of pre-diabetes in our study was 11.57% (233 individuals) with female contributing to 62.23% of the burden.
Table 2.
Prevalence of diabetes mellitus and pre diabetes in the study population
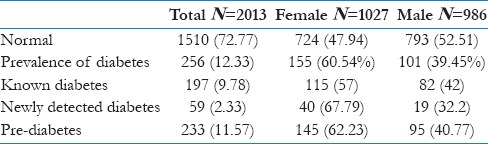
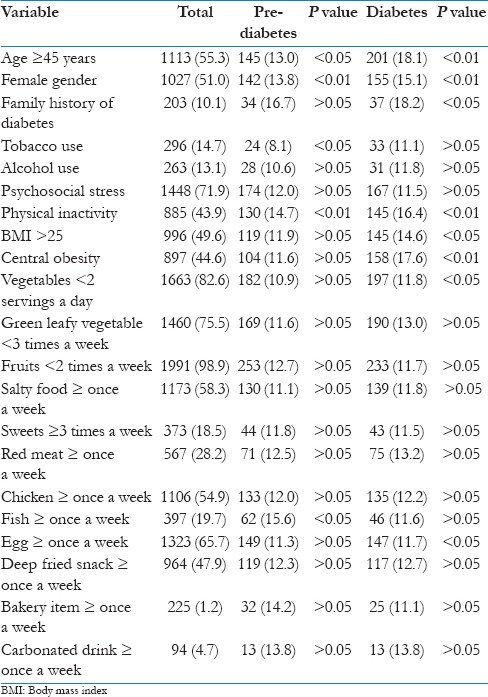
Table 3 describes association of various risk factors with pre-diabetes and diabetes. Individuals with age more than 45 years showed a statistically significant association with both diabetes and pre-diabetes. In addition, our study showed an increasing trend of prevalence of diabetes and pre-diabetes with increasing age (χ2 for trend = 18.03, P<0.01). Prevalence of both pre-diabetes and diabetes was more among females and this association was found to be statistically significant (χ2 =10.389, P<0.01 in pre-diabetes and χ2 =10.656, P<0.01 in diabetes). Family history of diabetics showed a statistically significant association with diabetes (χ2 =6.173, P<0.05). We found that pre-diabetes was more commonly seen among tobacco users (χ2 =4.075, P<0.05), whereas alcohol use and psychosocial stress did not show any significant association with pre-diabetes. Physical inactivity showed a statistically significant association with both diabetes (χ2 =32.835, P<0.01) and pre-diabetes (χ2 =17.430, P<0.01). Prevalence of both diabetes (χ2 =37.378, P<0.01) and pre-diabetes (χ2 =7.554, P<0.01) was more among the people with central obesity. Diabetes was more commonly seen among people who were overweight with a BMI >25 (χ2 =5.971, P<0.05). Hypertension was the most common co-morbidity and was seen in 44.9% (155 subjects) of the diabetics. People who consumed < 2 serving of vegetable per day had higher prevalence of diabetes (χ2 =6.541, P<0.05) and its association was statistically significant. People who consumed fish more than once a week had higher prevalence of pre-diabetes (χ2 =7.895, P<0.05) and people who consumed egg more than once a week had higher prevalence of diabetes (χ2 =8.971, P<0.05). Consumption of other food items like green leafy vegetable, fruits, salty food, sweets, red meat, chicken, deep fried food, bakery items and carbonated drink was not associated with prevalence of diabetes and pre-diabetes.
Table 3.
Association of various risk factors pre diabetes and diabetes (N=2013)
We did a multivariate analysis to compute the adjusted odd ratios for the different risk factors. Results of this analysis are depicted in Table 4. Our analysis revealed the odds of developing pre-diabetes were 1.4 times more among those who were above the age of 45 years and 1.5 times more in those who were physically inactive.
Table 4.
Unadjusted and adjusted odd ratios for risk factors of diabetes and pre-diabetes
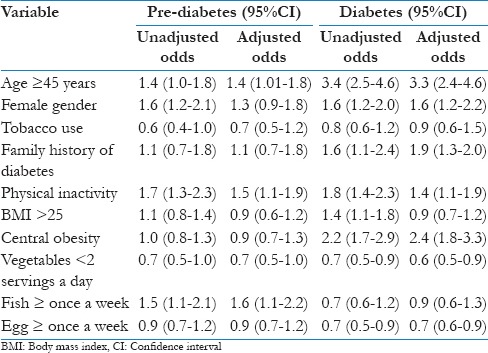
Multivariate analysis for the risk factors of diabetes reveled age greater than 45 years [OR 3.3 (2.4-4.6)] and the presence of central obesity [OR 2.4 (1.8-3.3)] to be the prominent risk factors for diabetes. Other risk factors that showed significant odds ratio were female gender [OR 1.6 (1.2-2.2)], family history of diabetes [OR 1.9 (1.3-2.0)] and physical inactivity [OR 1.4 (1.1-1.9)].
Discussion
Our study found the prevalence of diabetes and pre-diabetes among adults aged 35 years and above in the slums of Bangalore to be 12.33% and 11.57%, respectively. Studies from India have reported a prevalence of diabetes to be 13% to 16% and prevalence of pre-diabetes to be between 2-29%, which is similar to the findings in our study.[5,9,10] The results of our study show a higher prevalence of diabetes and pre-diabetes among females. This is probably explained by the fact that females were more sedentary in their habits and the prevalence of obesity including central obesity was more in females. Earlier reports from Chennai had shown a male preponderance in the prevalence of diabetes which in subsequent years had shifted slightly toward a female excess.[5]
In the present study, prevalence of diabetes and pre-diabetes increased with the increasing age. Similar findings were reported by the Chandigarh Urban Diabetes Study.[11] Family history was present in 14.06% of diabetes subjects and 12.01% of pre-diabetes subjects and its association with diabetes was significant and not with pre-diabetes. In a study conducted in slums of Mumbai, 18.2% subjects had a family history of diabetes. Studies have shown that the genetic factor plays an important role in the causation of diabetes.[12,13]
In our study, hypertension was seen as co-morbidity in 155 diabetics (44.9%) and co-prevalence of both diabetes and hypertension was 7.7%. Several studies have shown a close association between diabetes and hypertension. In a study conducted in Manipur[13] about 13.8% had both diabetes and hypertension which was much high than our study. In a study in France, Marre et al. reported hypertension in almost one third of diabetic cases.[14] Among adult Afro-Americans, elevation of blood pressure is significantly higher in individuals with impaired glucose tolerance and diabetics than in non-diabetics. The occurrence of hypertension in diabetic patients significantly increases the risk of coronary artery disease, mortality and nephropathy.[15]
Tobacco consumption was found to have a significant association with pre-diabetes. Prevalence of tobacco use was 14.7% and alcohol use 13.1% in the present study which is low compared to earlier reports. The reason for this could be that subjects denied tobacco and alcohol use in the presence of other family members. An association between alcohol and diabetes has been documented by many authors with a non-linear relationship between alcohol intake and the risk of type 2 diabetes.[16] Alcohol was found to be positively associated with diabetes in a study in Manipur.[13] Levitt et al., on the other hand, reported that alcohol intake was not a significant risk factor for DM in South Africa.[17] Vashitha et al. in a study of rural population of Haryana[18] reported that smoking and alcohol use were not found to be a risk predictor of diabetes mellitus.
Chida et al. in a study reported association of psychosocial factor with the prognosis of diabetes and as etiological effect was inclusive.[19] Another study on working women reported psychosocial work stress as independent predictor of type 2 diabetes among women after a 15-year follow-up.[20] The present study shows no significant association of psychosocial stress with diabetes and pre-diabetes.
Our study showed a significant association of physical inactivity with diabetes and pre-diabetes which is in line with the several other studies.[11,21]
In our study prevalence of overweight and obesity was 66.81 (overweight 17.23 and obese 49.57%), which was higher than in previous studies[22,23] with prevalence of diabetes and pre- diabetes among these subjects being 23.34% and 12.49%. Subjects with increased BMI showed increase prevalence of diabetes and the association was statistically significant. This was comparable with other studies.[5,11]
Overall prevalence of central obesity in our study was 73.02% (male 72.42% and female 73.60%). Prevalence of pre-diabetes in male and female was 9.48% and 6.37%, respectively. Diabetes was 11.85% in males and 15.40% in females. Prevalence of diabetes was much more than pre-diabetes. Higher prevalence of pre-diabetes was seen in male and diabetes was seen in females. Association of central obesity with diabetes and pre-diabetes was statistically significant. A study conducted in Punjab showed prevalence of 14.6% diabetes with central obesity.[24]
In our study larger proportion of the subjects had higher waist hip ratio (73.02%) compared to increased BMI (66.8%). Ramachandran et al. had shown susceptibility of urban Indians to central obesity in National urban diabetes survey.[6] Studies in India had shown that central obesity was more strongly associated with pre-diabetes than general obesity.[10,25,26] Lean Asian Indians had WHR values similar to the Mexicans with higher rates of BMI.[27] This could indicate that Asian Indians have a predisposition to deposit abdominal fat which could be one of the risk factor s contributing to the high prevalence of diabetes. Studies in UK and in the USA have shown that Asian Indians were insulin resistant despite having BMIs in the non-obese range, an observation which could probably be related to a high percentage of visceral fat.[28,29] The higher prevalence of diabetes in Asian Indians than in the white population might be partly related to the above feature.[5]
In our study consumption of vegetables and egg had a significant association with diabetes and fish with pre-diabetes. People who consumed >2 serving of vegetable had lesser prevalence of diabetes. Many studies have shown and discussed the uses of consuming high water soluble fiber (vegetable and fruits) and polyunsaturated fat (fish) in the control of diabetes and prevention of diabetes.[30,31,32] Viscous and gel-forming properties of soluble dietary fiber inhibit macronutrient absorption, reduce postprandial glucose response, and beneficially influence certain blood lipids. Dietary fibers consumption contributes to a number of unexpected metabolic effects independent of changes in body weight, which include improvement of insulin sensitivity, modulation of the secretion of certain gut hormones, and effects on various metabolic and inflammatory markers that are associated with the metabolic syndrome.[30] People who consumed egg more than once a week had higher prevalence of diabetes. This could be due to the high cholesterol and saturated fat in the yolk. People who consumed fried fish more than once a week had higher prevalence of pre-diabetes. This could be due to the excess oil they used for frying the fish. Polyunsaturated fatty acids (omega-3fats found in fish and flaxseed, pumpkin seed, canola, soy, and walnuts) appear to reduce the risk of diabetes while trans-fatty acids were responsible for the increase in incidence. Increased prevalence of diabetes in India has a lot to do with a switch from a traditional to a Western diet. Eating fiber-rich foods gives a sense of fullness. Eating a lot of refined carbohydrates such as soft drinks and candy bars–or or even pretzels and crackers–leads to feeding a vicious circle in body that never really satisfies hunger because one gets only short-term relief.[31]
Diabetes was diagnosed using single reading of blood sugar. Only few readings were taken in the fasting and all the others were random blood sugar.
Conclusion
Prevalence of diabetes and pre-diabetes was comparable to data from other part of the country and the association of risk factors was also similar to the previous studies. Increasing age, female gender, family history of diabetes, physical inactivity and central obesity emerged as the major risk factors for diabetes in our study.
Acknowledgment
We are very thankful to Becton, Dickinson and Company for their financial support and also for the guiding the team at every step. We thank the community medicine department of St John's hospital for helping us prepare the survey forms, IEC material, training the community health works and in analyzing the data. We are grateful to the staff of PMU, Art of living foundation and community health worker for their sincere work.
Footnotes
Source of Support: Financial support: Becton, Dickinson and Company, Technical support: St John Medical College.
Conflict of Interest: None declared.
References
- 1.Sicree R, Shaw J, Zimmet P. Diabetes and impaired glucose tolerance. In: Gan D, editor. Diabetes Atlas. International Diabetes Federation. 3rd ed. Belgium: International Diabetes Federation; 2006. pp. 15–103. [Google Scholar]
- 2.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 3.Park K. 19th ed. Jabalpur: M/s Banarasidas Bhanot; 2007. Park's Textbook of Preventive and Social Medicine. [Google Scholar]
- 4.King H, Aubert RE, Herman WH. Global Burden of diabetes 1995-2025 Prevalence, numerical estimates and projection. Diabetes Care. 1998;21:1414–31. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 5.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al. High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44:1094–101. doi: 10.1007/s001250100627. [DOI] [PubMed] [Google Scholar]
- 6.Rayappa PH, Raju KNM, Kapur A. Economic cost of diabetes care: The Bangalore Urban District Diabetes Study. Int J Diab Dev Countries. 1999;19:87–97. [Google Scholar]
- 7.American diabetes association. Standards of medical care in diabetes–2013. Diabetes care. 2013;36:S11–66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chobanian AV, Bakris GL. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. 2003 Nov 5; doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 9.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabtes and Prediabetes in urban and rural India: Phase 1 results of the Indian Council OF MEDICAL Research-India DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 10.Ramachandran A, Snehalatha C, Dharmaraj, Vishwanathan M. Prevalence of glucose intolerance in Asian Indians: Urban and rural differences and significance of upper body adiposity. Diabetes care. 1992;15:1348–55. doi: 10.2337/diacare.15.10.1348. [DOI] [PubMed] [Google Scholar]
- 11.Walia R, Bhansali A, Ravikiran M, Ravikumar P, Bhadada SK, Shanmugasundar G, et al. High prevalence of cardiovascular risk factors in Asian Indians: A Community survey- Chandigarh Urban Diabetes Study (CUDS) Indian J Med Res. 2014;139:252–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Ahuja MMS. Epidemiological studies on diabetes mellitus in India. In: Ahuja MMS, editor. Epidemiology of diabetes in developing countries. New Delhi: Interprint; 1979. pp. 29–38. [Google Scholar]
- 13.Jali MV, Kambar S. Prevalence of diabetes amongst the family members of known diabetics. Int J Diab Dev Ctries. 2006;26:81–5. [Google Scholar]
- 14.Marre M, Berrut G, Bouhanick B. Hypertension and diabetes mellitus. Biomed Pharmacother. 1993;12:61–6. doi: 10.1016/0753-3322(93)90292-s. [DOI] [PubMed] [Google Scholar]
- 15.El-Hazmi MA, Warsy AS. Association of hypertension and non- insulin dependent diabetes mellitus in the Saudi population. Ann Saudi Med. 2001;12:5–8. doi: 10.5144/0256-4947.2001.5. [DOI] [PubMed] [Google Scholar]
- 16.Wei M, Gibbons LW, Mitchell TL, Kampert JB, Blair SN. Alcohol intake and incidence of type 2 diabetes in men. Diabetes Care. 2000;12:18–22. doi: 10.2337/diacare.23.1.18. [DOI] [PubMed] [Google Scholar]
- 17.Levitt NS, Katzenellenbogen JM, Bradshaw D, Hoffman MN, Bonnici F. The prevalence and identification of risk factors for NIDDM in urban Africans in Cape Town, South Africa. Diabetes Care. 1993;12:601–7. doi: 10.2337/diacare.16.4.601. [DOI] [PubMed] [Google Scholar]
- 18.Vashitha A, Agarwal BK, Gupta S. Hospital based study: Prevalence and predictors of type 2 diabetes mellitus in rural population of Haryana. Asian Pac J Trop Dis. 2012;12:9. [Google Scholar]
- 19.Chida Y, Hamer M. An association of adverse psychosocial factors with diabetes mellitus: A meta-analytic review of longitudinal cohort studies. Diabetologia. 2008;51:2168–78. doi: 10.1007/s00125-008-1154-1. [DOI] [PubMed] [Google Scholar]
- 20.Heraclides A, Chandola T, Witte DR, Brunner EJ. Psychosocial Stress at Work Doubles the Risk of Type 2 Diabetes in Middle-Aged Women, 2009 by the American Diabetes Association. Diabetes Care. 2009;32:2230–5. doi: 10.2337/dc09-0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia. 2013;56:942–3. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 22.Tiwari R, Srivastava D, Gour N. A cross-sectional study to determine prevalence of obesity in high income group colonies of Gwalior city. Indian J Community Med. 2009;34:218–22. doi: 10.4103/0970-0218.55287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sidhu S, Tatla HK. Prevalence of Overweight and Obesity Among Adult Urban Females of Punjab: A Cross-Sectional Study. Anthropologist. 2002;1:101–3. [Google Scholar]
- 24.Goyal P, Sachar RK, Soni RK. Is Central Obesity A Predictor Of Lifestyle Diseases- A Cross Sectional Study In Adult Punjabis. Indian J Prev Soc Med. 2011;42:44–47. [Google Scholar]
- 25.Ramachandran A, Snehalatha C, Latha E, Vijay V, Vishwanathan M. Rising prevalence of NIDDM in urban population in India. Diabetologia. 1997;40:232–7. doi: 10.1007/s001250050668. [DOI] [PubMed] [Google Scholar]
- 26.Shelgikar KM, Jockaday TD, Yajnik CS. Central rather than generalized obesity is related to hyperglycemia in Asian Indian subjects. Diabet Med. 1997;8:712–7. doi: 10.1111/j.1464-5491.1991.tb01689.x. [DOI] [PubMed] [Google Scholar]
- 27.Ramachandran A, Snehalatha C, Vijay V, Vishwanathan M, Haffner SM. Risk of NIDDM conferred by obesity and central adiposity I different ethnic groups- A comparative analysis between Asian Indians, Mexican Americans and Whites. Diabetes Res Clin Prat. 1997;36:121–5. doi: 10.1016/s0168-8227(97)00040-5. [DOI] [PubMed] [Google Scholar]
- 28.McKeigue PM, Shah B, Marmot MG. Relation of central obesity and insulin resistance with higher diabetes prevalence and cardiovascular risk in South Asians. Lancet. 1991;337:382–6. doi: 10.1016/0140-6736(91)91164-p. [DOI] [PubMed] [Google Scholar]
- 29.Banerji MA, Faridi N, Atluri R, Chaiken RL, Lebovitz HE. Body composition, Visceral fat, leptin and insulin reisitance in Asian Indians men. J Clin Endocrinol Metab. 1999;84:137–44. doi: 10.1210/jcem.84.1.5371. [DOI] [PubMed] [Google Scholar]
- 30.Weickert MO, Pfeiffer AF. Metabolic effects of dietary fiber consumption and prevention of diabetes. J Nutr. 2008;138:439–42. doi: 10.1093/jn/138.3.439. [DOI] [PubMed] [Google Scholar]
- 31.Mitra A. Some salient points in Dietary and Life- Style survey of rural Bengal particularly tribal populace in relation to Rural Diabetes Prevalence. Ethno Med. 2008;2:51–6. [Google Scholar]
- 32.Riccardi G, Rivellese AA. Effects of Dietary Fiber and Carbohydrate on Glucose and Lipoprotein metabolism in diabetic patients. Diabetes Care. 1991;14:1115–25. doi: 10.2337/diacare.14.12.1115. [DOI] [PubMed] [Google Scholar]


