Abstract
Background:
Tooth brushing is most common method of maintaining oral hygiene. In removing plaque and other soft debris from the teeth, tooth brushes become contaminated with bacteria, blood, saliva and oral debris. These contaminated tooth brushes can be a source of infection.
Aims and objectives:
The aim of the present study was to evaluate the presence of microorganisms in the tooth brushes and to investigate the effect of disinfectants such as chlorhexidine gluconate, sodium hypochlorite and water to decontaminate them.
Materials and Methods:
Twenty-one children were asked to brush their teeth for 5 days with a tooth brush. The tooth brushes were put in Robertson's Cooked Meat broth and were observed for growth of Streptococcal microorganisms. These tooth brushes were then placed in disinfectants such as 0.2% chlorhexidine gluconate (Group I), 1% sodium hypochlorite (Group II) and water (Group III) for 24 hrs and then cultured again. Reduction of growth of microorganisms was seen in Group I, Group II and remnants of growth seen in Group III.
Conclusion:
We conclude that the use of disinfectant for a tooth brush is a must for every individual at least at regular intervals.
Keywords: Decontamination, disinfectants, tooth brush contamination
Introduction
The increased awareness of the need for good dental health and the emphasis on preventive procedures by dentists and dental educators have made the role of a tooth brush increasingly important. Tooth brush is most common oral hygiene aid to promote oral health and prevent dental diseases. These tooth brushes can get contaminated with microorganisms present in oral cavity. Retention and survival of micro-organisms on tooth brush after brushing represents a possible cause of re-contamination of the mouth.[1] Numerous studies[1,2,3] have shown that prolonged use of the tooth brush facilitates contamination by various micro-organisms such as Streptococcus, Staphylococcus, lactobacilli, Pseudomonas, Klebsiella, Escherichia coli and Candida.[2] These micro-organisms are implicated to cause dental caries, gingivitis, stomatitis, infective endocarditis in an individual. The possibility of these tooth brushes being associated with transmission of severe health problems such as heart disease (infective endocarditis), arthritis, bacteremia and stroke have also been well documented,[4,5] affecting both oral and general health. Often after brushing tooth brush is just rinsed in the plain water and stored in bathrooms or combined toilet/bathroom, which is an ideal place to harbor millions of microorganisms.[2] These microorganisms grow and flourish in warm and moist conditions.[3] Oral diseases as well as other systemic diseases can be greatly controlled by reducing the microbial load in the oral cavity and this can be achieved by maintaining proper oral hygiene, by using clean and decontaminated tooth brush daily. There is complete lack of awareness among public regarding tooth brush maintenance. So, it is of utmost importance to educate the public about proper storage, replacement and disinfection of tooth brushes. Considering this aspect, the present study was undertaken to evaluate the presence of Streptococcal microorganisms (cariogenic or cavity causing bacteria) in the tooth brushes and the effect of disinfectants such as chlorhexidine gluconate and sodium hypochlorite to decontaminate them.
Materials and Methods
Twenty-one children in the age group of 5 to 12 years were randomly selected for the present study. List of children from class 1st to 7th was obtained from the local school registry; children and parents were requested to be a part of the study. From this registry, children were picked by lottery method and randomly allotted into the three groups until the required sample size was reached. Written informed consent was taken prior to the commencement of study from all parents and ethical clearance from the institution was obtained for the same. Subjects with history of antibiotics usage 3 months prior to the study and subjects undergoing orthodontic treatment or with extensive intraoral prosthesis were excluded from the study. Dental hygiene instructions were explained to all the subjects after which each of them were given a tooth brush. Assuming the proportion of infected tooth brushes to be 95% or almost all[6] as proved by Bhat et al.,[6] all tooth brushes could get heavily infected by microorganisms originating not only from the oral cavity but also from the surroundings in which they are stored.[6] Relative precision chosen was 20% of p, sample size was calculated using the formula n = 4pq/d*d and found out to be 6 in each of the three group. Extra child was taken in each group and final sample consisted of 21 children.
The children were subjected to supervised brushing using Fone's tooth brushing technique, twice daily for five consecutive days. At the end of 5 days, tooth brushes were retrieved from them within 2 hours of usage. These tooth brushes were kept in separate sterile containers and were not allowed to come into contact with each other during the time of collection. They were then kept in test tubes containing Robertson's Cooked Meat Broth and incubated for about 4-5 hrs. This broth was cultured on Mitis Salivarius Agar plates (MSAB HIMEDIA REFM259) and incubated for 48 hrs. After incubation, different patterns of colonies of microorganisms were identified by observing their colony morphology on all the 21 agar plates. The microorganisms identified were Streptococcus mutans (S. mutans), Streptococcus salivaris (S. salivaris) [Figure 1] and Streptococcus mitis (S. mitis) [Figure 2]. Grams stain was done to isolate the microorganisms, which microscopically revealed the streptococcus microorganisms arranged in varying length of chains [Figure 3]. These brushes were then immersed in different disinfectants, 7 brushes in 0.2% chlorhexidine gluconate [Group I], 7 in 1% sodium hypochlorite [Group II] and 7 in water [Group III]. After 24 hrs, these brushes were again placed in Robertson Cooked Meat Broth and then cultured.
Figure 1.
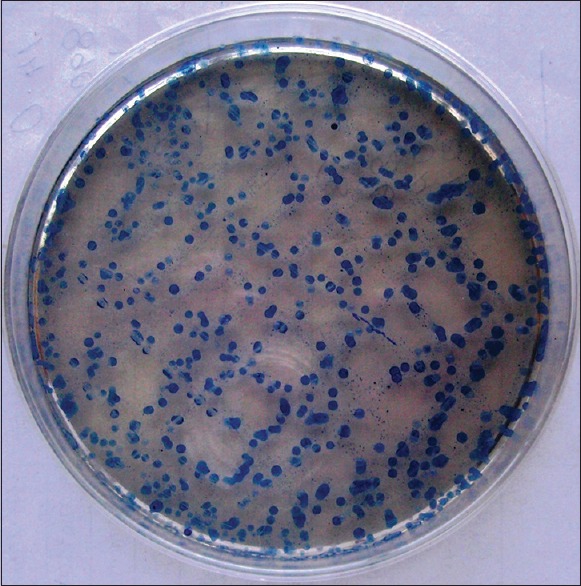
Growth of Streptococcus mitis seen as small, flat, hard colonies, blue in color with a domed center on Mitis Salivarius agar (original)
Figure 2.
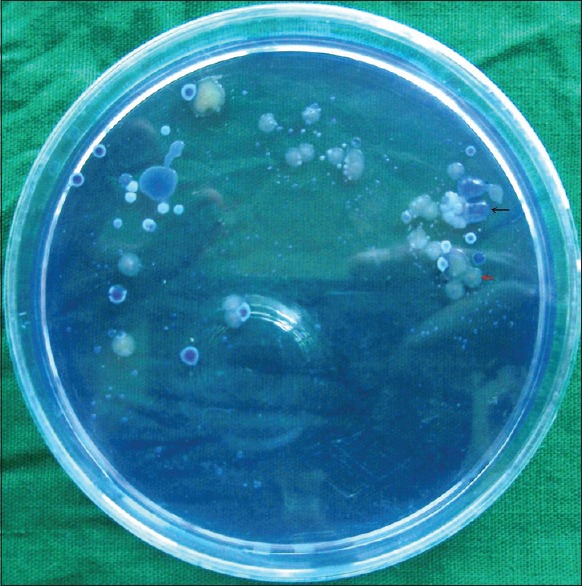
Growth of Streptococcus mutans (shown in black arrow) seen as raised, convex, opaque, pale-blue colonies that are granular (i.e., “frosted glass”) in appearance, exhibiting a glistening bubble on the surface due to excessive synthesis of glucan from sucrose and Streptococcus salivaris (shown in red arrow) seen as large, pale-blue, mucoid colonies that are glistening (i.e. “gum-drop”) in appearance on Mitis Salivarius agar (original)
Figure 3.
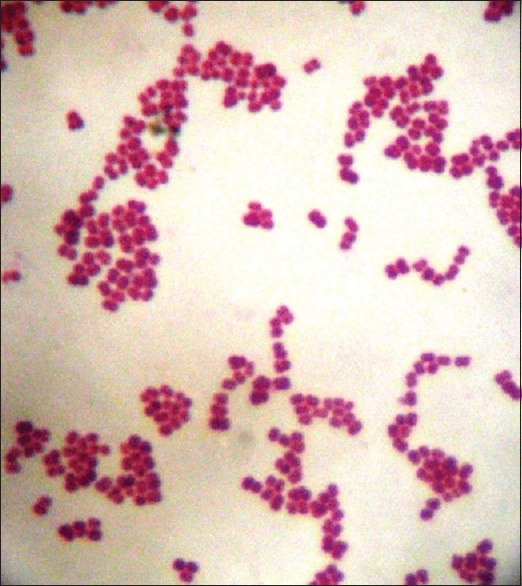
Grams stain showing Streptococcal microorganisms (original)
Results
Group I did not show any growth of Streptococcus colonies. Group II showed the growth in two of the agar plates and five agar plates did not show the growth. Group III showed colonies of Streptococci in six Mitis Salivarius agar plates and only one did not show the growth. Treatment of tooth brushes with chlorhexidine have shown 100% reduction of Streptococci colonies and treatment of tooth brushes with sodium hypochlorite resulted in 71% reduction of colonies, both the values are statistically highly significant. Tooth brushes stored in water gave 14% reduction in Streptococcal colonies, which was statistically not significant [Figure 4].
Figure 4.
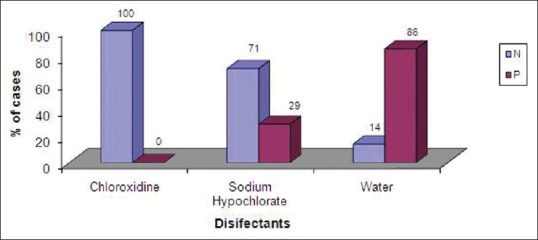
Bar graph showing in percentage the efficiency of different disinfectants in reducing the growth of streptococcal colonies (original)
Statistical analysis was carried out using Fisher's exact test.
The difference between chlorhexidine and sodium hypochlorite was not significant (P = 0.20, not significant). This suggests that both these chemicals are equally effective disinfectants. The difference between chlorhexidine and water is highly significant (P = 0.001, significant) suggesting that chlorhexidine is definitely regarded as effective disinfectant when compared to water. There was significant difference between sodium hypochlorite and water (P = 0.001, significant). Thus suggesting that sodium hypochlorite is effective in reducing the growth of organisms compared to water.
Discussion
Contaminated tooth brush has been characterized as a means of microbial transport, retention and growth. It can be the cause of reinfection of a person with pathogenic bacteria or can be the reservoir for environmental microorganisms.[7,8] Reinfection of the oral cavity is possible owing to injuries of the gingiva that can occur during tooth brushing.[7] Brushing with a contaminated brush introduces new microorganisms while simultaneously reducing the existing normal flora. The area of tooth brush in which the tufts are anchored is especially prone to heavy contamination. Fluids and food debris can be drawn into the spaces between tufts by capillary action; this may lead to bacterial growth. The conventional technique of fastening bristles with a metal anchor in the center creates small cavities between the tufts. There also is a great predrilled hole in the center of each bundle of filaments.[8] When the brush is trimmed, the end of the bristle has an irregular shaped lumen. Fluids can be drawn in this core by capillary action, allowing for bacterial growth. The bristles also split longitudinally, further increasing the bacterial contamination. Tooth brushes could be heavily infected with microorganisms especially Mutans Streptococci within 24 hrs of use.[9] In this study, children in a age group of 5-12 yrs were selected as in this age they fall into mixed dentition period that is the time for transitional changes in the oral microbial flora, also it is of utmost importance to educate the school children about oral health since they will carry these good habits throughout their life. The present study revealed the presence of Streptococcal species in the tooth brushes. Streptococci certainly originate from plaque trapped in tooth brush bristles. S. mutans is commonly found in oral cavity and is a principal etiologic agent in the development of dental caries due to its exceptional aciduric and acidogenic properties, and its ability to adhere and accumulate in large numbers on tooth surfaces in the presence of sucrose. Sucrose is used by S. mutans to produce a sticky, extracellular, dextran-based polysaccharide that allows them to cohere, forming plaque. The combination of plaque and acid leads to dental decay.[10] They cause initiation of dental caries.[8] S. mutans is also implicated in the pathogenesis of certain cardiovascular diseases and is the most prevalent bacterial species detected in extirpated heart valve tissues, as well as in atheromatous plaques, with an incidence of 68.6% and 74.1%, respectively.[11] S. mitis is a commensal organism present in the oral cavity. S. mitis is usually an etiologic agent in odontogenic infection and endocarditis and only in some cases have been acknowledged as respiratory pathogens. The most common host is humans. The major interaction in the pathogenesis of infective endocarditis is the direct binding of bacteria to platelets.[12] S. salivarius is the principal commensal bacterium of the oral cavity in humans. It may enter the blood stream by accident during dental work or when brushing the teeth. It is the first bacterium which colonizes the dental plaque, before being joined by numerous other species of various genera. It therefore seems to be the pioneer in colonizing dental plaque; it creates favorable conditions so other species can begin to colonize. It is also a bacterium that plays the role of moderator, permitting the implantation of bacteria which are harmful to the health of the oral cavity. Moreover, when this bacterium enters the bloodstream, it is found that it may cause septicemia in neutropenic patients.[13]
Tooth brushes that play a pivotal role in fighting against tooth decay can itself lead to dental diseases as well as many other systemic diseases, including septicemia and gastrointestinal, cardiovascular, respiratory, and renal problems,[14] if not properly stored and maintained. So, these tooth brushes should be disinfected or discarded at regular intervals for wellbeing of individual. The present study suggested that both chlorhexidine and sodium hypochlorite are effective chemical agents used in disinfection of tooth brushes. There was a significant increase in contamination of tooth brush in group III which implies that rinsing in water and air drying lead to tooth brush contamination. Hence, this suggests that rinsing with water and air drying is an incomplete procedure of tooth brush cleaning.
Chlorhexidine is a chemical antiseptic with bacteriostatic and bactericidal properties to both gram-positive and gram-negative microbes. It damages the cytoplasmic membrane of the microorganisms and disrupts the integrity of the cell membrane, causing leakage and precipitation of cytoplasmic protein and nucleic acids, thus destroying microorganisms.[15] Overnight immersion of a tooth brush in chlorhexidine gluconate was found to be highly effective in preventing microbial contamination; other studies had taken the immersion time into consideration and reported that immersing in chlorhexidine (0.12%) for 20 minutes[3], 2 hours[16] 12 hours[17] and in chlorhexidine (0.2%) for 24 hours[6] was adequate to decontaminate the tooth brushes.
Sodium hypochlorite has been reported to be an effective disinfectant.[18] Sodium hypochlorite is used worldwide for endodontic treatment due to its highly desirable properties as a bactericidal, deodorant and tissue solvent. When NaOCl is added to water, hypochlorous acid is formed, which contains active chlorine, a strong oxidizing agent. Substantial evidence suggests that chlorine exerts its antibacterial effect by the irreversible oxidation of –SH groups of essential enzymes, disrupting the metabolic functions of the bacterial cell. Chlorine may also combine with cytoplasmic components to form N-chloro compounds, toxic complexes which destroy the microorganism.[19] Studies done by Bhat et al. and Nelson et al. have also suggested that 0.12% chlorhexidine gluconate and 1% sodium hypochlorite are efficient chemicals for tooth brush disinfection.[17] Chamele et al. have stated chlorhexidine gluconate to be an ideal disinfectant.[20] Briseno has reported sodium hypochlorite to be an effective disinfectant.[21] Yokosuka et al. have reported the innovation of chlorhexidine-coated bristle tooth brushes to be an effective method of prevention of bacterial contamination.[22]
Limitations
Only Mitis Salivarius agar medium was used which is solid medium recommended for selective isolation of S. mitis, S. salivarius, and Enterococci from specimens of mixed bacterial flora. This investigation did not consider all the varieties of microorganisms present in the oral cavity. Further investigations should take into account survival of other microorganisms, such as other bacteria, fungi and viruses. Tooth brush contamination after 5 days was seen in the present study, contamination at time interval of 15 days, 1, 1.5, 2, 2.5 and 3 month duration to know the pathogenecity of microorganisms at different time interval was not taken into consideration. Anti-microbial solutions like 0.2% chlorhexidine and 1% sodium hypochlorite were used in the present study to disinfectant tooth brushes other anti-microbial solutions like neem, salt that are economical, nontoxic and easy to use can also be tested and, if proved efficient, could be recommended.
Conclusion
In spite of millions of tooth brushes sold throughout the world each year, there is very little public awareness that tooth brush can be contaminated with use. Millions of microorganisms thrive on infected tooth brush, being the root cause for many diseases which might have got undiscovered. A.D.A in 1996 has recommended the change of tooth brushes after every 3 months. Patients undergoing chemotherapy should change their tooth brushes after every 3 days.[23] Those subjected to major surgery are to change brushes everyday and those sick should change brushes at the beginning of illness, when they first feel better and when they are completely well.[17] Tooth brushes should not be kept in bathrooms especially those which have combined toilet which harbor potential pathogens, lot of brushes should not be kept in one container, they will rub against each other and spread germs, also tooth brushes should not be exchanged between individuals. Finally, we would like to emphasize that cleaning the oral cavity with contaminated tooth brush will do more harm than good. Thus, it is essential for every individual to disinfect his or her brush at regular intervals, thereby preventing reinfection and helping in maintaining a good oral hygiene and general wellbeing.
Acknowledgement
Our sincere thanks to Dr Rohit A, Assistant professor, Department of preventive and social medicine, Jaya Jagadguru Murugharajendra Medical College, Davangere, Karnataka for helping us in the statistical analysis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Wetzel WE, Schaumburg C, Ansari F, Kroeger T, Sziegoleit A. Microbial contamination of tooothbrushes with different principles of filament anchoring. J Am Dent Assoc. 2005;136:758–65. doi: 10.14219/jada.archive.2005.0259. [DOI] [PubMed] [Google Scholar]
- 2.Karibasappa GN, Nagesh L, Sujatha BK. Assessment of microbial contamination of toothbrush head: An in vitro study. Indian J Dent Res. 2011;22:2–5. doi: 10.4103/0970-9290.79965. [DOI] [PubMed] [Google Scholar]
- 3.Sogi SH, Subbareddy VV, Kiran SN. Contamination of tooth brushes at different time intervals and effectiveness of various disinfection solutions in reducing the contamination of tooth brush. J lndian Sot Pedo Prev Dent. 2002;20:81–5. [PubMed] [Google Scholar]
- 4.Warren DP, Goldschmidt MC, Thompson MB, Adler -Storthz K, Kenne HJ. The effects of toothpastes on the residual microbial contamination of toothbrushes. J Am Dent Assoc. 2001;132:1242–5. doi: 10.14219/jada.archive.2001.0366. [DOI] [PubMed] [Google Scholar]
- 5.Sammons Rl, Kaur D, Neal P. Bacterial survival and biofilm formation on conventional and antibacterial toothbrushes. Biofilms. 2004;1:123–30. [Google Scholar]
- 6.Bhat SS, Hegde KS, George RM. Microbial contamination of tooth brushes and their decontamination. J lndian Sot Pedo Prev Dent. 2003:21108–72. [PubMed] [Google Scholar]
- 7.Cobb CM. Toothbrushes as a cause of repeated infections of the mouth. Boston Med Surg J. 1920;183:263–4. [Google Scholar]
- 8.Glass RT, Lare MM. Toothbrush contamination: A potential health risk? Quintessence Int. 1986;17:39–42. [PubMed] [Google Scholar]
- 9.Svanberg M. Contamination of toothpaste and toothbrush by Streptococcus mutans. Scan J Dent Res. 1978;86:412–4. doi: 10.1111/j.1600-0722.1978.tb00646.x. [DOI] [PubMed] [Google Scholar]
- 10.Raghu AR, Sivapathasundharam B. Dental caries. In: Rajendran R, Sivapathasundharam B, editors. Shafer's Textbook of oral Pathology. 7th edn. New Delhi: Elsevier; 2012. pp. 424–5. [Google Scholar]
- 11.Nakano K, Inaba H, Nomura R, Nemoto H, Takeda M, Yoshioka H, et al. Detection of cariogenic Streptococcus mutans in extirpated heart valve and atheromatous plaque specimens. J Clin Microbiol. 2006;44:3313–7. doi: 10.1128/JCM.00377-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Streptococcus salivarius JIM8777, JIM8780: The principal inhabitant of the human oral cavity. Genoscope-Centre National de Sequencage. [Last accessed on 2014 Dec 15]. Available from: http://www.cns.fr/externe/English/Projets/Projet_MB/organisme_MB.html .
- 13.White JC, Niven CF., Jr Streptococcus S. B. E.: A Streptoccocus associated with subacute bacterial endocarditis. J Bacteriol. 1946;51:717–22. doi: 10.1128/jb.51.6.717-722.1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nascimento AP, Watanabe E, Ito IY. Toothbrush contamination by Candida spp and efficacy of mouthrinse spray for their disinfection. Mycopathologia. 2010;169:133–8. doi: 10.1007/s11046-009-9239-z. [DOI] [PubMed] [Google Scholar]
- 15.Russell AD. Chlorhexidine: Antibacterial action and bacterial resistance. Infection. 1986;14:212–5. doi: 10.1007/BF01644264. [DOI] [PubMed] [Google Scholar]
- 16.Aysegul O, Elgin IE, Gulcin A, Nedim S. The efficacy of chlorhexidine spray vs mouth wash in the microbial contamination of child toothbrushes. J Dent Child. 2007;74:177–81. [PubMed] [Google Scholar]
- 17.Mehta A, Sequeira PS, Bhat G. Bacterial contamination and decontamination of toothbrushes after use. N Y State Dent J. 2007;73:20–2. [PubMed] [Google Scholar]
- 18.Konidala U, Nuvvula S, Mohapatra A, Nirmala S. Efficacy of various disinfectants on microbially contaminated toothbrushes due to brushing. Contemp Clin Dent. 2011;2:302–7. doi: 10.4103/0976-237X.91793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Balappanavar AY, Nagesh L, Ankola AV. Antimicrobial efficacy of various disinfection solutions in reducing the contamination of toothbrushes. Oral Health Prev Dent. 2009;7:137–45. [PubMed] [Google Scholar]
- 20.Chamele J, Bhat C, Saraf T, Jadhav A, Beg A, Jagtap C, et al. Efficacy of microwaves and chlorhexidine for disinfection of pacifires and toothbrushes: An in vitro study. J Contemp Dent Pract. 2012;13:690–4. doi: 10.5005/jp-journals-10024-1210. [DOI] [PubMed] [Google Scholar]
- 21.Briseno BM, Writh R, Standhartinger W. Efficacy of different irrigation methods and concentration of R.C.T irrigation solution on bacteria in root canal. Endod Dent Traumatol. 1992;8:6–11. doi: 10.1111/j.1600-9657.1992.tb00218.x. [DOI] [PubMed] [Google Scholar]
- 22.Yokosuka N, Tanaka T, Ebisudani K, lwai T. Studies on bacterial contamination of chlorhexidine coated filaments of the toothbrush. Nihon Shishubyo Gakkai Kaishi. 1989;31:960–9. doi: 10.2329/perio.31.960. [DOI] [PubMed] [Google Scholar]
- 23.Denny FW. Risk of toothbrushes in the transmission of respiratory infections. Paed Infect Dis. 1991;10:710–1. [PubMed] [Google Scholar]


