Abstract
Background:
Stigma associated with mental illnesses is one of the principal causes for mentally ill people not receiving adequate mental health care and treatment. The study was conducted to assess the extent of stigma associated with mental illness and knowledge of mental illness among the community.
Materials and Methods:
Community-based, cross-sectional study was conducted among 445 respondents from Udupi district; the community attitude toward the mentally ill (CAMI) scale was used to assess stigma. The probability proportional to sampling size technique was adopted to select the wards/blocks. Household from blocks/wards were selected using convenience sampling. Self- administered semi-structured questionnaire was used to collect the information. Data was analyzed using the software SPSS version 15.
Results:
Of the total 445 respondents, the prevalence of stigma toward mentally ill people was 74.61% (95% confidence interval, 0.7057, 0.7866). The prevalence of stigma was high under all the four domains of CAMI scale. High prevalence of stigma was seen among females and people with higher income.
Conclusions:
The overall prevalence of stigma toward PWMI was found to be high. The stigma toward PWMI was associated with gender with respect to AU, BE and CMHI. Hence, the study suggests that there is a strong need to eliminate stigma associated with mental illness to improve the mental health status of the region.
Keywords: Community attitude, discrimination, mental illness, stigma
Introduction
According to the World Health Organization (WHO), “it is estimated that globally 450 million people suffer from mental disorders.”[1] Around 80% of the people with mental disabilities live in low- and middle-income countries (LMICs),[2] four out of five people with serious mental disorders living in LMICs do not receive the needed mental health services.[1] Mental illness accounts for 14% of all disability adjusted life years (DALYs) lost worldwide,[3,4] and is one of the major contributors to the global burden of disease.[3]
Among Indian population, the estimated prevalence of mental disorders is found to be 5.8%.[5] A study from Pune suggests that the prevalence of mental health disorders was 5%;[6] a study from Bangalore reports the prevalence of mental health disorders ranged from 9.5 to 102 per 1000 population.[7] A study among elderly population of South India estimated the prevalence of depression to be 12.7%.[5]
Despite the existing programs for the control of non-communicable disease, including mental illness, mental health disorders remains as one of the hidden disease burdens in India due to stigma and discrimination.[8,9]
“Stigma can be divided into public and self-stigma.” Public stigma occurs when the general public supports a prejudice about a stigmatized group. Self-stigma occurs when a member of a stigmatized group internalize the negative views held by the general public.[10] Given its negative impact on treatment seeking, adherence and effectiveness, the stigma associated with mental illness can be considered as a major public health problem. The main determinants and sources of stigma, nature and forms of stigma are of interest hence, understanding the stigma faced by people with mental illness (PWMI) is necessary. In this study, we aim to assess the association of stigma with mental health problems. The study may contribute in bringing up the evidences for stigma against PWMI.
Materials and Methods
A community-based cross-sectional study was carried out from February to July 2014 Udupi district, Karnataka. The sample size estimated was 430, with prevalence as 50% (as no previous data on stigma was available). Relative precision was taken as 10% of the prevalence, cluster effect as 1.5 and 10% non-response rate. Overall, 500 participants were included in the study.
Data was collected through cluster sampling technique, wards from rural and blocks from urban areas were treated as clusters. Probability proportional to sampling size technique was used to select 10 wards/blocks of Udupi district, and proportional allocation was used to select sample size from each ward/block based on the population size of the ward/block. Convenience sampling was used to select households from each ward/block, data was collected by conducting house-to-house interviews, and one participant from each household was selected for the interview.
The approval to carry out the study was taken by Institutional Ethical Committee, Kasturba Medical College, Manipal (ECR/146/Inst/KA/2014). Written informed consent from all the participants was taken before data collection. The data was collected anonymously and confidentiality maintained.
Questionnaire design and analysis
The questionnaire consisted of two parts; first part included the open-ended questions and were interviewer administered which consisted of basic demographics, knowledge on mental health, previous and present contact with mentally ill people and if they personally had experienced any mental health problem. The second part was used to assess stigma through the community attitudes toward the mentally ill (CAMI) scale and it was self–administered. CAMI scale was a 5-point Likert scale, the responses ranged from strongly agree to strongly disagree.[10] CAMI Scale has four subscales: Authoritarianism (AU), benevolence (BE), social restrictiveness (SR), and community mental health ideology (CMHI). AU is a “view of the mentally ill person as someone who is inferior and requires supervision and coercion.” This implies an authoritative, strict, or oppressive personality toward subordinates. BE corresponds to “a humanistic and sympathetic view of mentally ill persons,” a higher BE score corresponds to a less humanistic and less sympathetic (malevolent) view of PWMI. SR means “the belief that mentally ill patients are a threat to society and should be avoided.” CMHI is “the acceptance of mental health services and the integration of mentally ill patients in the community.”[11] The subscale has 10 questions corresponding to AU, BE, SR and CMH. This measures the behavior toward mentally ill patients by an individual with respect to the questions of each subscale. Overall stigma scores against PWMI were calculated by adding the scores of subscales. Reverse recoding was done for negatively stated items for analysis. Higher scores indicated high stigma against PWMI.
A pilot study was conducted priory among 40 people and minor changes without altering the meaning of the questions were done according to the Indian scenario. The tool was validated by experts before conducting the study.
The data collected was tabulated and analyzed by using the software, Statistical Package for Social Sciences (SPSS) version 15. The quantitative variables were illustrated with frequencies and percentages. The Chi-square test was performed to find out the association between stigma and other factors. A probability (P value) level of less than 0.05 was considered significant. For analysis purpose the five categories of socio-economic status have been clubbed into three categories namely low, medium and high.
Results
Socio demographic characteristics
A total of 500 participants were included in the study, 55 participants’ data were excluded from the analysis due to missing data. The results of 445 participants are presented under various domains as frequencies and percentages followed by their interpretation.
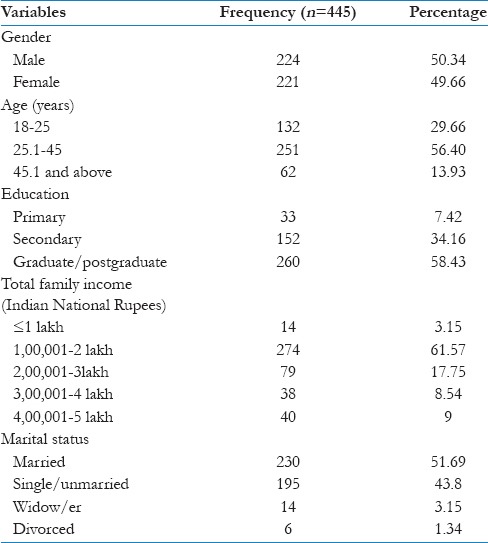
Of the total 445 study participants, 224 were males and 221 were females. The mean age of the participants was 32.37 years (SD 10.62). The maximum age was 62 years and the minimum 18 years. Around 68.17% were urban residents and 31.83% rural. The socio-demographic variables are shown in Table 1.
Table 1.
Socio-demographic variables
Mental health knowledge and perceptions
Variables to assess knowledge and perceptions on mental health with frequencies and percentages are described in Table 2. Majority of the participants were not aware of the names of mental illness. Those who knew among them only half of the participants could name only one of the mental illnesses.
Table 2.
Mental health knowledge and perception
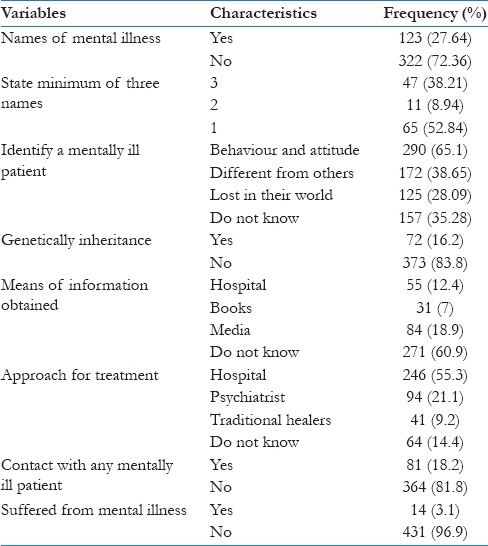
Majority of the participants reported that, they would identify a mentally ill person by his behavior and attitude. Significant number of participants believed that mental illness had no genetic inheritance. The self-reported prevalence of mental illness among the participants was 3.1%. Around 18% had at least one family member, relative or a friend having mental illness either currently or in the past with or known to them. Among all the participants, 14.59% had worked with PWMI some time in their lives.
Around three fifth of the participants had no information on mental illness. Of those who had information, 18.9% obtained from media, 12.4% from hospitals and health programs and 7.9% through books and other sources. A significant number of participants (76.4%) would approach hospital for the treatment; approximately 1 in 10 reported they would go to traditional healers, whereas 14.4% had no idea on the treatment for mental health when asked about facility preference.
Prevalence of stigma toward mental illness
CAMI scale was used to assess stigma, under four components: Authoritarianism, benevolence, social restrictiveness and community mental health ideology. Based on the total scores of stigma of CAMI scale, quartiles were considered as cut off points for low, medium and high stigma. Less than equal to Q1 were considered as low stigma, Q1 to Q2 was considered as medium stigma and more than Q2 was considered as high stigma. Figure 1 describes the prevalence of stigma. The overall prevalence of stigma toward mental illness was 74.61% (95% confidence interval: 0.7057, 0.7866)
Figure 1.
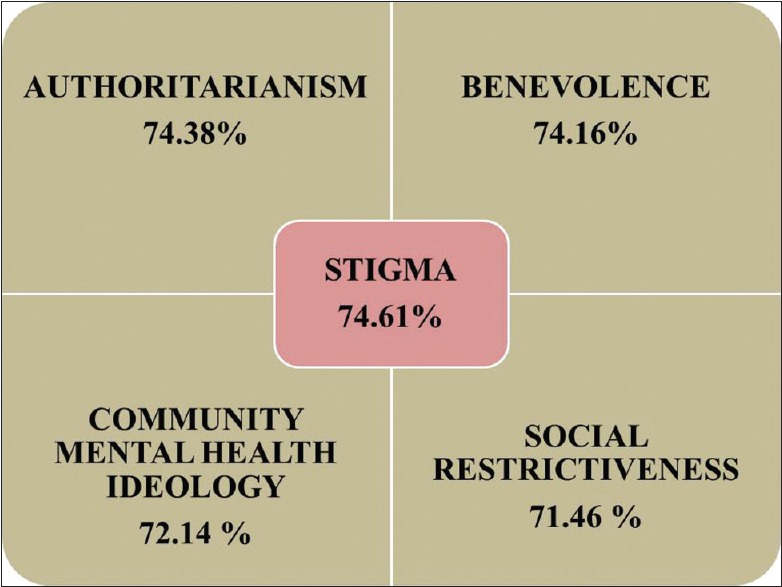
Prevalence of stigma (uploaded separately) the distribution of stigma toward mental illness in the community
Stigma scores for CAMI
Table 3 shows the stigma scores for the components of CAMI scale.
Table 3.
Stigma scores for the components of CAMI
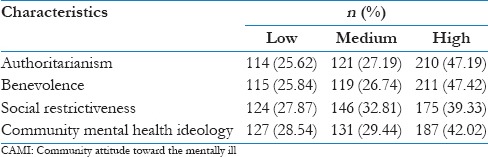
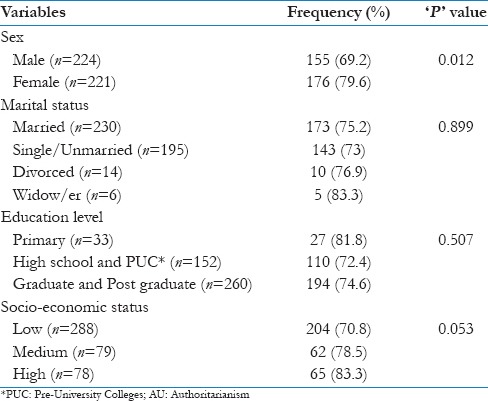
Authoritarianism (AU): Table 4 shows the distribution of high stigma scores for AU. High stigma among females (79.6%) is seen under AU. Stigma scores for AU remain almost the same for marital status. Stigma is high among primary education level participants (81.8%) and among high social class people (83.3%).
Table 4.
Distribution of high stigma according to AU
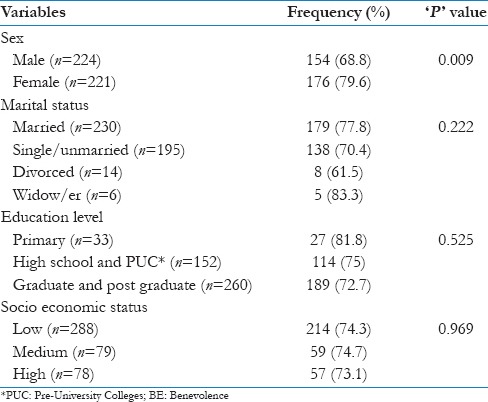
Benevolence (BE): Table 5 shows the distribution of high stigma scores for BE. High stigma among females (79.6%) was seen under BE. Stigma scores for BE remains high among married (77.8%) compared to unmarried, high among primary education level participants, (81.8%) and remains the same among all the social class people.
Table 5.
Distribution of high stigma according to BE
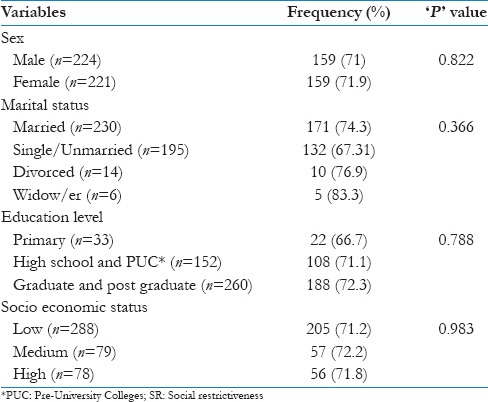
Social Restrictiveness (SR): Table 6 depicts the distribution of high stigma scores for SR. High stigma among females (79.6%). Stigma scores remain almost the same for marital status, education level and all the social class people.
Table 6.
Distribution of high stigma according to SR
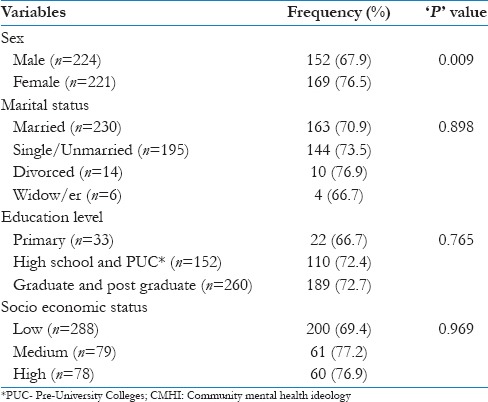
Community Mental Health Ideology (CMHI): Table 7 shows the distribution of high stigma scores for CMHI. Stigma was seen to be high among females (79.6%). Stigma scores remain high among married (77.8%), high among primary education level participants (81.8%) and remain the same among all the social class people.
Table 7.
Distribution of high stigma according to CMHI
Discussion
To the best of the author's knowledge, this is the first study in South Asia region addressing the issue of stigma faced by PWMI. Although mental illness is an important public health issue it has not been given much attention and very few studies have been conducted on stigma toward PWMI in the nation.
This study has provided a baseline to design and implement interventions to address the issue of stigma in the region. With the help of stakeholders who are involved in giving care to mentally ill people, we have come up with few interventions such as creating awareness and trying to bring about behavioral change in the community through mass media, local folk dances (e.g. Yakshagana) and healthcare workers. With the help of a non-governmental organization we have planned to conduct an intervention trial in one village as a pilot project.
Only literate participants were recruited in the present study which can be a potential source of bias. Another source of bias could result from the sampling technique employed since participants were recruited conveniently due to time constraints.
The aim of the present study was to assess the burden of stigma toward PWMI as well as the factors associated with it. The overall stigma scores against PWMI were high among females and high social class people. The stigma score was also high in all the four subscales of CAMI scale.
Studies conducted in Africa and Europe could not identify any association between gender and age with stigma toward PWMI.[12,13,14] However, in the present study gender was associated with the stigma toward PWMI. High stigma among females can be attributed to poor dissemination of information on mental illness among them. The present study informs that the people belonging to high social class tend to have higher stigma and education could be a significant factor for this association. The high stigma among people belonging to the high social class might be because they are more concerned with their status and reputation compared to low social class people.
Although some of the studies have found higher stigma among rural population, the current study does not provide evidence to this finding.[15]
The role of education on stigma against PWMI has been neutral in the present study; however some studies reported that education has negative effect on stigma.[16,17] On the contrary, few others stated it to have a positive effect.[18] The few studies exhibited that providing exposure to mental health information can reduce stigma levels toward PWMI.[19,20]
Conclusion
Stigma is one of the main barriers for quality mental health care and it takes diverse appearance in different forms. The present study was intended to assess the burden of stigma toward PWMI as well as the factors associated with it. The overall prevalence of stigma toward PWMI was found to be high. The stigma toward PWMI was associated with gender with respect to AU, BE and CMHI. Hence, the study suggests that there is a strong need to eliminate stigma associated with mental illness to improve the mental health status of the region. The results of this study can act as a baseline to design and implement integrated interventions at different levels to address the issue of stigma in the region.
Acknowledgement
We would like to acknowledge Dr. Anil Kumar Indira Krishna, Associate Professor, School of Public Health, SRM University Tamil Nadu; Dr. P. V. Bhandari, Psychiatrist, Dr. A.V. Baliga Hospital, Udupi; and Dr. PSVN Sharma, Professor and Head, Department of Psychiatry, Kasturba Medical College, Manipal for their support to carry out this research.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.World Health Organization. Risks to Mental Health: An overview of vulnerabilities and risk factors. Background paper by WHO secretariat for the development of a comprehensive mental health action plan. 2012. [Last accessed on 2014 May 12]. Available from: http://www.who.int/mental_health/mhgap/risks_to_mental_health_EN_27_08_12.pdf .
- 2.World Health Organization. Report of Global Health Observatory. 2010. [Last accessed on 2014 May 12]. Available from: http://www.who.int/gho/en .
- 3.Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370:859877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 4.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. Plos Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reddy VB, Gupta A, Lohiya A, Kharya P. Mental Health Issues and Challenges in India: A Review. Int J Sci Res Publ. 2013;3:2250–3153. [Google Scholar]
- 6.Deswal BS, Pawar A. An Epidemiological Study of Mental Disorders at Pune, Maharashtra. Indian J Community Med. 2012;37:116–21. doi: 10.4103/0970-0218.96097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Math SB, Srinivasaraju R. Indian Psychiatric epidemiological studies: Learning from the past. Indian J Psychiatry. 2010;52(Suppl 1):S95–103. doi: 10.4103/0019-5545.69220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for Mental Health: Scarcity, inequity, and inefficiency. Lancet. 2007;370:878–89. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- 9.Srinivasan TN, Thara R. Beliefs about causation of schizophrenia: Do Indian families believe in supernatural causes? Soc Psychiatry Psychiatr Epidemiol. 2001;36:134–40. doi: 10.1007/s001270050302. [DOI] [PubMed] [Google Scholar]
- 10.Thara R, Kamath S, Kumar S. Women with schizophrenia and broken marriages-doubly disadvantaged? Part I: Patient perspective. Int J Soc Psychiatry. 2003;49:225–32. doi: 10.1177/00207640030493008. [DOI] [PubMed] [Google Scholar]
- 11.Goffman E. Harmondsworth, Middlesex: Penguin Books; 1963. Stigma: Notes on the Management of Spoiled Identity. [Google Scholar]
- 12.Barney ST, Corser GC, White LH. Service-Learning with the Mentally Ill: Softening the Stigma. Michigan J Community Ser Learn Spring. 2010;3:66–77. [Google Scholar]
- 13.Girma E, Tesfaye M, Froeschl G, Moller-Leimkuhler AM, Muller N, Dehning S. Public Stigma against People with Mental Illness in the Gilgel Gibe Field Research Center (GGFRC) in Southwest Ethiopia. PLoS One. 2013;8:e82116. doi: 10.1371/journal.pone.0082116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilson C, Nairn R, Coverdale J, Panapa A Psychiatry and the media, mental illness depictions in prime-time drama: Identifying the discursive resources. Aust N Z J Psychiatry. 1999;33:232–9. doi: 10.1046/j.1440-1614.1999.00543.x. [DOI] [PubMed] [Google Scholar]
- 15.Barke A, Nyarko S, Klecha D. The stigma of mental illness in Southern Ghana: Attitudes of the urban population and patients’ views. Soc Psychiatry Psychiatr Epidemiol. 2011;46:1191–202. doi: 10.1007/s00127-010-0290-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deribew A, Tamirat Y. How are mental health problems perceived by a community in Agaro town? Ethiop J Health Dev. 2005;19:153–9. [Google Scholar]
- 17.Phelan JC, Bromet EJ, Link BG. Psychiatric illness and family stigma. Schizophr Bull. 1998;24:115–26. doi: 10.1093/oxfordjournals.schbul.a033304. [DOI] [PubMed] [Google Scholar]
- 18.Oestman M, Kjellin L. Stigma by association: Psychological factors in relatives of people with mental illness. Br J Psychiatry. 2002;181:494–8. doi: 10.1192/bjp.181.6.494. [DOI] [PubMed] [Google Scholar]
- 19.Corrigan PW, Edwards AB, Green A, Diwan SL, Penn DL. Prejudice, social distance, and familiarity with mental illness. Schizophr Bull. 2001;27:219–25. doi: 10.1093/oxfordjournals.schbul.a006868. [DOI] [PubMed] [Google Scholar]
- 20.Brockington IF, Hall P, Levings J, Murphy C. The community's tolerance of the mentally ill. Br J Psychiatry. 1993;162:93–9. doi: 10.1192/bjp.162.1.93. [DOI] [PubMed] [Google Scholar]


