Abstract
Background:
The main purpose of this study was to investigate the effect of the PRECEDE model and health locus of control (HLC) on postpartum depression. This study used the path analysis to test the pattern of causal relations through the correlation coefficients.
Materials and Method:
The participants included 230 pregnant women in the north-east of Iran who were selected by convenience sampling. To analyze data, Pearson correlation and path analysis were applied to examine the relationships between variables using SPSS 20 and LISREL 8.50software.
Results:
The result of path analysis showed that a positive correlation exists between predisposing (knowledge, internal HLC, powerful others HLC, chance HLC) enabling and reinforcing factors with postpartum depression by GHQ score (GFI = 1, RSMEA = 000).
Conclusion:
The current study supported the application of the PRECEDE model and HLC in understanding the promoting behaviors in mental health and demonstrated their relationships with postpartum depression.
Keywords: Health locus of control, mental health promotion, postpartum depression-PRECEDE
Introduction
The maternal role is very important to ensure the infant's safety, survival, and well-being, but it does not come without costs.[1] In this period as much as the physical aspects, social and psychological aspect are important.[2] In fact, postpartum is a transitional period when mother faces new roles, patterns, and relationships, and has to adjust herself with all of them.[3] The World Health Organization (WHO) states that maternal mental health problems may lead to impose huge social, and economic burden on women, their infants, their families, and society, and create a major public health challenge. The peak prevalence of major depressive disorders in women occurs during the childbearing period and the first postpartum year.[4] Some symptoms of postpartum depression include depressed mood and/or loss of pleasure, changes in weight or sleep, fatigue or loss of energy, feeling of worthlessness or guilt, concentration difficulties, and suicidal ideation.[5] Although the overall prevalence of mental disorders is similar for both men and women, it seems that the effect of depression and anxiety disorders on women’ mental health is more excessive, especially during childbearing.[6] In addition to the considerable negative personal impact of postpartum depression (PPD) on women, PPD also negatively impacts marital relationships.[7] PPD may also detrimentally affect mother–infant attachment, and infant social-cognitive development. Depressed mothers are less emotionally sensitive and have less attention to their infant's emotional state. These serious implications make PPD an important mental illness. For this reason, the study of PPD tremendous impacts on mothers, supporting systems, child's development and familial relationships is essential.[7] The disability of a woman in adjusting herself with these changes affects herself, her infant, other children she may have, and her partner.[5] Healthy People 2010 has listed the improvement of the health and well-being of women, infants, children, and families as its goals.[5] An important problem among people with depression is the low rate of diagnosis and treatment of these patients. Only less than half of the women suffering from major depression disorder are identified and treated due to the complexity of the depression diagnosis as a clinical and health issue.[8]
In the field of health education, certain models help us to explain the occurrence of behaviors and to conduct health education program in order to consider its effect on an especial behavior.[9] Therefore, the selection of a model for comprehension knowledge about postpartum depression is necessary. The selected model should be able to know the predictor factors of the behavioral changes and their effects on postpartum depression. One of the most frequently used models in health education and promotion is the PRECEDE model (Predisposing, Reinforcing, Enabling, Causes in, Educational Diagnosis and Evaluation).
The PRECEDE portion of the model (Phases 1–4) includes social, epidemiological, behavioral, environmental, educational, administrative, and policy assessments. The PRECEDE model has been developed by Green and Kreuter as a theoretical model to identify the needs for educational programs and health promotion.[10]
In the view of PERCED model, health and its risk factors have different dimensions.[11] In this model, all the background factors and dependent factors are classified based on their importance and effects.[12]
According to this model, people's perceived ability to control their health is an important issue.[13] For example, Health Locus of Control (HLC) can be regarded as an individual's belief about the determiners of health and its outcomes. In HLC field, researches have mostly focused on internal control (i.e. personal behaviors), chance control (i.e., fate/luck), and control by powerful others (i.e., health professionals and other people).[14]
People with a strong IHLC believe that their behaviors determine their health status. They are more likely to seek information about health-threatening conditions and follow healthier behaviors, such as disease prevention to maintain their health.[13] In contrast, an external HLC (EHLC) is marked by the belief of fate influence, powerful others, or effective supernatural occurrences upon one's health.[15] The importance of these attitudes is due to their potential negative consequences on affected individuals, their families, economic affairs, and public health. Based on previous reports, mental disorders are the second disease forced on economic affairs.[12] It is estimated that by 2020, major depression will be the single leading cause of disease burden in the world.[12] Although the perinatal phase is considered as a pleasure period, many women frequently experience adjustment difficulties and depressive symptoms during their pregnancy and the postpartum period.[16] A study which examined the factors associated with promoting behaviors of mental health using PRECEDE framework among Hong Kong adults showed that predisposing, enabling, and reinforcing factors are important to understand promoting behavioral practices for mental health. The knowledge of these factors contributed to the promotion of mental well-being and life quality.[12] In spite of unclear relationship between HLC and PPD,[17] HLC role in the prediction of prenatal depression has been significant.[17,18] The study of predisposing variables (related to IHLC, EHLC), dependent and independent variables (related to general health questionnaire or GHQ) and the prediction of postpartum depression based on PERCED model is a suitable and integrated assessment.
The purpose of this study was to apply the PRECEDE model and HLC on Iranian pregnant women for preventing PPD. It was hypothesized that predisposing, enabling and reinforcing factors would serve as antecedents to general health, which in turn affect postpartum depression.
Materials and Methods
Ethical considerations
This study protocol was approved by ethical and research committees at Gonabad University of Medical Sciences (N. 296/A).
The authors respected to the Helsinki Declaration concerning human rights. They followed the correct research procedures concerning to the human and animal treatment. Also, brochure and verbal information about the study contents were provided to the participants. The respondents were anonymous and participated willingly and voluntarily in this study.
Procedures and participants
The correlative path analysis design was used to investigate direct and indirect structural relationships among variables. Convenience sampling method was applied to select study subjects including 230 pregnant women who were attended in three urban healthcare centers for their routine pregnancy examinations in the north-east of Iran. Inclusion criteria consisted of residing in the north-east of Iran, gestational age between 28 and 30 weeks, literacy (ability to read and write), healthy fetus on ultrasound, history loss of mental disease or depression, and subject's consent for participation in the study. Exclusion criteria were as follows: Having the history of hospitalization or stillbirth, serious physical and mental problems such as death of a first degree relative during intervention, and subject's disinclination to continue. The postpartum depression of pregnant women was measured from the beginning of the study until 15–20 days after birth. Because of researchers’ serious tracking, all 230 subjects who participated in the study filled out the questionnaires.
Questionnaire
Researcher-made questionnaire
This questionnaire was based on the constructs of the PRECEDE model to identify and examine predisposing, enabling, and reinforcing factors and designed through literature review and examined by an expert panel comprising the specialists of health education, psychology, biostatistics, and obstetrics. After receiving comments and resolving and modifying the problems, the questioner was made available to 15 pregnant women for assessing its content. After completion of the questionnaire by pregnant women, the challengeable and vague questions were modified or removed. To determine reliability, the questionnaire was made available to 30 pregnant women, and after completion, Cronbach's alpha was found to be 83%. To assess credibility, the questionnaires were again returned to the first subjects to be completed after 3 weeks using retest method. This questionnaire comprised of predisposing factors (35 items), enabling factors (10 items), and 2 items on reinforcing factors (these questions assessed pregnant women's understandings of perceived support from their relatives).
General health questionnaire-28
The General Health Questionnaire is widely used as screening instrument for assessing the presence of distress, psychopathology, and overall well-being. Also, this questionnaire has showed high reliability and validity.[19] The 28-item version (GHQ-28) was derived from the GHQ-60 version in the 1970s to distinguish four correlated concepts as subscales A, B, C and D. Each subscale includes seven items, for example the presence of somatic symptoms (subscale A, items 1–7), anxiety and insomnia (subscale B, items 22–28), social dysfunction (subscale C, items 15–21) and severe depression (subscale D, items 22–28).[20]
The psychometric properties of the Persian version of GHQ-28 have been found acceptable. The test–retest, split-half, Cronbach alpha, the sensitivity and specificity of this questionnaire were calculated as 0.70, 0.93, 0.89, 0.88 and 0.79, respectively.[21]
Edinburgh postnatal depression scale
This tool contains 10 short statements, with 4 answers for each statement and is used to identify postnatal depression. Scores less than 12 are considered as depressed and 12 and over as non-depressed. The validity and reliability of the questionnaire have been confirmed in Iran. Cronbach's alpha coefficient and test-rest reliability were found to be 0.86 and 0.80, respectively.[22]
Multidimensional HLC scale
This scale predicts health behaviors according to participants’ beliefs. In this study, Form B was used comprising three components (6 items for each; totally 18 items), namely Internal Health Locus of Control (IHLC), Powerful Others Health Locus of Control (PHLC) and Chance Health Locus of Control (CHLC). All items contained 6-point Likert style, scoring from 1 to 6. So a person's score could vary from 6 to 36 for each component, and they would not be summed together, but were calculated independently. There was no cut-off point in this tool, and the mean score was used for final evaluation.[23] After translating this scale, face, content, concurrent and construct validity, test-retest reliability, parallel tests, and internal consistency were confirmed in Iran.[24]
Analysis
The data was analyzed by using SPSS 20 software. In addition to descriptive analysis, several statistical tests were used to evaluate different demographic, dependent and independent variables of the study including mean age, mean marriage age and Pearson correlation matrix. Also, path analysis of relationship, direct, indirect and total effects as well as fitness indexes were calculated using LISREL 8.5 software.
Results
Demographic data results showed that subjects’ mean age was 27.909 ± 5.812 years and mean marriage age was 75.56 ± 67.79 months. According to the PRECEDE model framework, the predisposing (knowledge and attitude), enabling, and reinforcing factors were expected to be indirectly associated with postpartum depression disorder through moderating score of GHQ. In fact, these factors were predicted to have a direct effect on the GHQ score and an indirect effect on postpartum depression. The relationship between the mentioned components using Pearson correlation coefficient is reported in Table 1.
Table 1.
Bivariate relations between study variables
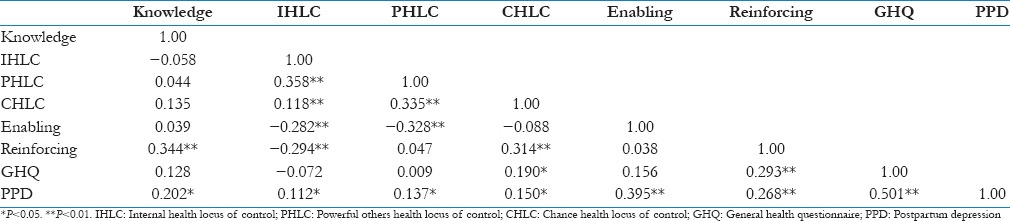
Table 1
The Bivariate relations of the study variables are presented in Table 2. As it is demonstrated, all three components of HLC (IHLC, PHLC and CHLC) had significant correlations with PPD. Also, it was observed that IHLC was correlated significantly with PHLC and CHLC. Besides, CHLC was significantly associated with PHLC. Also enabling factor had a negatively significant correlation with IHLC and PHLC. Furthermore, reinforcing factor was significantly associated with knowledge and CHLC, while the others had a negatively significant relationship with IHLC.
Table 2.
Direct, indirect and total effects
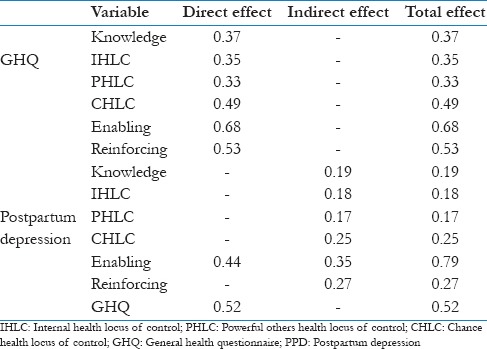
Moreover, GHQ was significantly associated with PPD (β=0.501, standard error [SE] =0.044, P < 0.001). In terms of the background variables, CHLC and reinforcing factor were significantly related to GHQ. As compared with CHLC, GHQ was primarily driven by reinforcing factor, respectively (β=0.247, SE = 0.447, P < 0.001).
Path analysis of relationship based on the PRECEDE model has been summarized in Figure 1. The arrows indicate the direction of the path, from exogenous variables (knowledge, IHLC, PHLC, and CHLC, as well as enabling and reinforcing factors) toward endogenous variables (general health and postpartum depression). Although the PRECEDE model assumes that the effects of the background variables on postpartum depression are mediated by GHQ score, the relatively poor fitness of the model suggested that the examination of the direct paths from the background variables to postpartum depression was warranted. Therefore, we added the direct effect of enabling factor on the postpartum depression.
Figure 1.
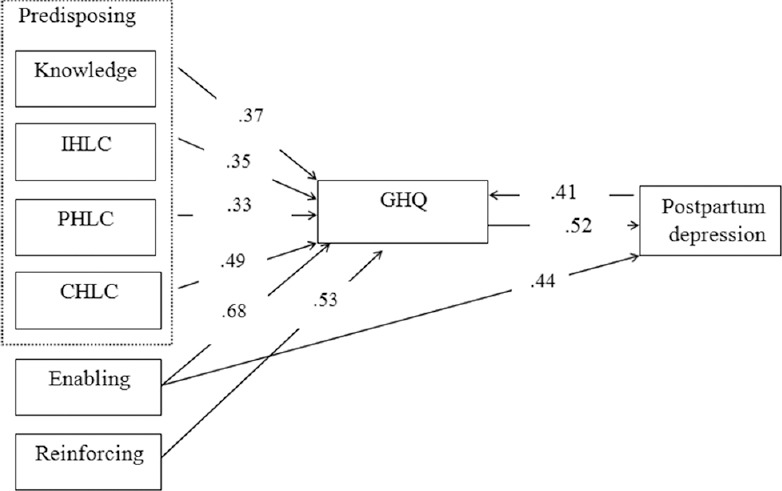
PRECEDE model and HLC to understanding postpartum depression
Figure 1
The general purpose of the model was to investigate the effects of predisposing (knowledge, IHLC, PHLC, and CHLC), enabling, and reinforcing factors as well as the general health on postpartum depression using a path analysis model.
Coefficients of direct, indirect, and overall effects as well as the explained variance between the variables are presented on the model [Table 2].
Table 2
The fitness of the proposed model was assessed through Chi-square (χ2), the goodness of fit index (GFI), the index of ratio of χ2 to the degree of freedom, the comparative fit index (CFI), the normed fit index (NFI), the relative fit index (RFI), Akaike's information criterion (AIC), the root mean square error of approximation (RMSEA) and the standardized root mean square residual (SRMR) [Table 3]. Since each of the indices indicates only a specific aspect of the model fitness, usually several indices are used to assess the adequacy of model fitness.[25]
Table 3.
Path analysis model fitness indices
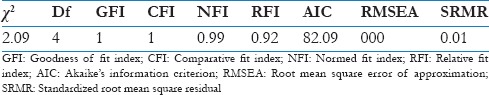
Table 3
When the values of CFI, NFI, RFI, and GFI approach to 1, the model fitness is favorable. Although the Chi-square index is usually used to assess the goodness of fit, it is increased when the sample size and the degree of freedom increase. Therefore, using SRMR and RMSEA has been recommended.[26] According to Schermelleh-Engel et al.,[27] a value between 0 and 0.05 for SRMR indicates a good fitness, while a value between 0.05 and 0.1 indicates an acceptable fitness. Also, a value between 0 and 0.08 for RMSEA indicates a good fit. Thus, according to the figures in table 3, it can be argued that the path analysis model has followed a good fitness.
Discussion
The prevalence of PPD in both developed and developing countries has led to consider this disorder as a major problem of general health in these countries.[22] PPD is a preventable and curable disorder, and most depressed mothers will be fully recovered and returned to their normal life through early diagnosis and treatment.[28] Therefore, the recognition of preventive factors is considered as an important step in the treatment of PPD. Predisposing factors like knowledge, IHLC, PHLC and CHLC as well as enabling and reinforcing factors are presented as the underlying factors of the PRECEDE model. Considering each of these factors by individuals and the society plays an important role in the prevention of this disorder.
All three factors of predisposing, enabling, and reinforcing were considered as the exogenous variables, and as demonstrated in the path analysis model no hypothesis was assumed about the effect of other variables on them. Moreover, the general health is assumed as an intermediate variable in the relationship between these three factors and PPD. Additionally, among the background variables, enabling factor was directly associated with PPD.
Knowledge, IHLC, PHLC and CHLC were considered as predisposing factors. Predisposing factors like knowledge, attitude, beliefs, values and perception of the needs and abilities are pre-behaviors that provide people basic reasons and motivate them to do certain behaviors., These factors motivate a person or a group to adopt a behavior and belong to the realm of psychology including cognitive and effective aspects like feeling, beliefs, values and a sense of trust. HLC refers to someone's’ belief to have the ability to control his own health. So this can be a part of predisposing factors in the PRECEDE model which guides a person to control his diseases/sickness such as postpartum depression. The results of path analysis modeling showed that knowledge had a significant relationship with GHQ score among pregnant women. Health education programs are perquisites of behavior change. They increase the level of knowledge and create positive attitude. It is clear that effort in promoting women's knowledge to reinforce their self-care improves their quality of life during pregnancy.[29] Our findings are similar to those of Sabzmakan et al.[30] They studied the effectiveness of an educational program based on the PRECEDE model (predisposing factors, enabling factors, reinforcing factors) on the reduction of depression level as well as GHQ score. They reported significant correlations between IHLC, PHLC, and CHLC with pregnant women's GHQ score. They stated that women with more IHLC toward this phenomenon enjoyed better mental health and observed a significant relationship between IHLC and PPD. Although Abraham[17] and Lamanna[31] showed a negatively significant relationship between IHLC and postpartum depression, the results of a study by Springer et al.[32] showed that pregnant women with higher IHLC enjoyed healthier nutrition. IHLC was associated with knowledge, positive attitude, psychological status, health behaviors and health. In contrast, most external beliefs of HLC were associated with negative health behaviors and poor psychological status.[23] In the present study, no relationship was found between PHLC and PPD. Researchers did not find any similar studies in this regard. Results revealed a significant relationship between CHLC and PPD. Richardson et al.[18] showed that CHLC is an important predictor of depression, especially among pregnant women. Benassi et al.[33] found that belief control is associated with PPD.[33] Their results showed a positively significant relationship between PHLC and CHLC. However, the results of a study conducted by Moshki et al.[34] on the investigation of the relationship between the health control beliefs and lifestyle in pregnant women showed an insignificant relationship between two external beliefs.
The results revealed a significant relationship between GHQ score and reinforcing factors. Reinforcing factors generally included perceived social support that affects pregnant women's GHQ score. These results are consistent with most results of the previous studies such as Logsdon et al.,[1] Reid and Meadows-Oliver[35] and Masoudnia.[36] Also, there was a negatively significant correlation between the mothers’ perceived social support and the incidence of PPD. Thus, mothers with high scores of perceived social support showed fewer symptoms of postpartum depression than others. Explaining the mechanisms that relate social support to the incidence of depression is complex. Researchers have identified a range of paths which show that the lack of social support leads to depression.
Generally, the results of path analysis modeling showed that the proposed model had a very good fitness with the data in the current study. Accordingly, GHQ score has played its mediating role very well. This means that the relationship between background factors (predisposing, enabling, and reinforcing) and depression disorder is affected by GHQ score. Since in the PRECEDE model, predisposing factors provide necessary motivation to do health behaviors, knowledge and attitude (HLC) of the study subjects can be considered as facilitating causes of adopting preventive health behaviors against depression.
Mothers are fully active in their role. When they feel healthy the society considers them healthy. However, PPD can be explained through clinical criteria, physical symptoms and social recognition. General health is considered as an indicator including all physical symptoms and personal and social functions. Therefore, paying attention to pregnant women mental health is a significant point in predicting PPD.
A limitation of this study was selecting subjects only from urban pregnant women. Urban women may have different feelings toward pregnancy and childbirth due to their superior enabling factors, and perhaps, reinforcing and predisposing factors compared to rural women. Hence, it is likely to obtain different results in different studies. Lack of resources and local studies on the subject of this study are also other limitations of the present study.
Further studies are needed to be conducted in other populations with different social factors, cultural factors, beliefs, and customs to reveal the relationship between PPD and the components of HLC, and other demographic factors. Therefore, appropriate educational interventions on the culture and custom of each region can be adopted to prevent people from postpartum depression. It seems that further extensive studies on PPD and the contributing risk factors lead to the improvement of mental health among mothers, children and families.
Implications for practitioners
The results of the current study showed that the proposed model had a very good fit with the study data. Accordingly, GHQ score has played its mediating role well. In terms of application, the present study also contains positive results that can be a part of the agenda of: Health, medical, and research and education deputies of universities. The findings of this study make mental health professionals familiar with PPD, and help them to recognize the role of biological, psychological, social and cultural factors in the incidence of PPD that is implicit in the PRECEDE model. Development of implementing educational programs for mothers and their first-degree families especially their spouses during pregnancy, to increase their awareness of the symptoms and outcomes about postpartum mood disorders especially PPD and the way to deal with them, and reinforcing the sense of cooperation are the effective reinforcing factors. Accordingly, holding classes and meetings during pregnancy in the health clinics (public and private) and the offices of doctors and midwives is recommended.
Acknowledgements
The authors would like to thank the officials at Social Development and Health Promotion Research Center, Gonabad University of Medical Sciences for supporting the research. We are indebted to all pregnant women who were voluntarily attended in the healthcare centers of Gonabad city.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Logsdon MC, Wisner KL, Pinto-Foltz MD. The impact of postpartum depression on mothering. J Obstet Gynecol Neonatal Nurs. 2006;35:652–8. doi: 10.1111/j.1552-6909.2006.00087.x. [DOI] [PubMed] [Google Scholar]
- 2.Tabrizi M, Lorestani K. Effectiveness of the eclectic counseling in decreasing depression during pregnancy and preventing postnatal depression. Thought Behav Clin Psychol. 2011;17:19–26. [Google Scholar]
- 3.Stocky A, Lynch J. Acute psychiatric disturbance in pregnancy and the puerperium. Baillieres Best Pract Res Clin Obstet Gynaecol. 2000;14:73–87. doi: 10.1053/beog.1999.0064. [DOI] [PubMed] [Google Scholar]
- 4.Davey HL, Tough SC, Adair CE, Benzies KM. Risk factors for sub-clinical and major postpartum depression among a community cohort of Canadian women. Matern Child Health J. 2011;15:866–75. doi: 10.1007/s10995-008-0314-8. [DOI] [PubMed] [Google Scholar]
- 5.Veisani Y, Delpisheh A, Sayehmiri K, Rezaeian S. Trends of Postpartum Depression in Iran: A systematic review and meta-analysis. Depress Res Treat. 2013 doi: 10.1155/2013/291029. 291029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Markhus MW, Skotheim S, Graff IE, Frøyland L, Braarud HC, Stormark KM, et al. Low omega-3 Index in pregnancy is a possible biological risk factor for postpartum depression. PLoS One. 2013;8:e67617. doi: 10.1371/journal.pone.0067617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christian S. United States of America: ProQuest LLC; 2013. Meta-Analysis of the effectiveness of biological and non-biological treatments for postpartum depression. [Google Scholar]
- 8.Chen TH, Lan TH, Yang CY, Juang KD. Postpartum mood disorders may be related to a decreased insulin level after delivery. Med Hypotheses. 2006;66:820–3. doi: 10.1016/j.mehy.2005.09.032. [DOI] [PubMed] [Google Scholar]
- 9.Glanz K, Rimer BK, Viswanath K. 4th ed. San Francisco: Jossey-bass Publisher; 2008. Health Behavior and Health Education: Theory, Research, and Practice. [Google Scholar]
- 10.Green LW, Kreuter MW. 4th ed. New York: McGraw-Hill; 2005. Health promotion planning: An educational and ecological approach. [Google Scholar]
- 11.Butler TH. United States: Wads Words Co; 2000. Principle of health education and health promotion. [Google Scholar]
- 12.Mo PK, Mak WW. Application of the PRECEDE model to understanding mental health promoting behaviors in Hong Kong. Health Educ Behav. 2008;35:574–87. doi: 10.1177/1090198108317409. [DOI] [PubMed] [Google Scholar]
- 13.Wang R, Aldridge AA, Malcarne VL, Choe S, Branz P, Sadler GR. Health locus of control and assimilation of cervical cancer information in deaf women. J Cancer Educ. 2010;25:354–9. doi: 10.1007/s13187-010-0053-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis DP, Jandrisevits MD, Iles S, Weber TR, Gallo LC. Demographic, socioeconomic, and psychological factors related to medication non-adherence among emergency department patients. J Emerg Med. 2012;43:773–85. doi: 10.1016/j.jemermed.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Brincks AM, Feaster DJ, Burns MJ. The influence of health locus of control on the patient-provider relationship. Psychol Health Med. 2010;15:720–8. doi: 10.1080/13548506.2010.498921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ikeda M, Kamibeppu K. Measuring the risk factors for postpartum depression: Development of the Japanese version of the Postpartum Depression Predictors Inventory-Revised (PDPI-R-J) BMC Pregnancy Childbirth. 2013;13:112. doi: 10.1186/1471-2393-13-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abraham AJ. Master's thesis. Available from: ProQuest dissertations and thesis database; 2008. [Last accessed on 2013 Jul 15]. Correlating health locus of control and risk for postpartum depression. UMI no. 1454982. [Google Scholar]
- 18.Richardson A, Field T, Newton R, Bendell D. Locus of control and prenatal depression. Infant Behav Dev. 2012;35:662–8. doi: 10.1016/j.infbeh.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldberg D, Williams P. London: Nfer-Nelson; 1991. A User's Guide to the general health questionnaire. [Google Scholar]
- 20.Prady SL, Miles JN, Pickett KE, Fairley L, Bloor K, Gilbody S, et al. The psychometric properties of the subscales of the GHQ-28 in a multi-ethnic maternal sample: Results from the Born in Bradford cohort. BMC Psychiatry. 2013;13:55. doi: 10.1186/1471-244X-13-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taghavi MR. General health questionnaire: A validity and reliability study. J Psychol. 2002;5:380–97. [Google Scholar]
- 22.Montazeri A, Torkan B, Omidvari S. The edinburgh postnatal depression scale (EPDS): Translation and validation study of the Iranian version. BMC Psychiatry. 2007;7:11. doi: 10.1186/1471-244X-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wallston KA. The validity of the multidimensional health locus of control scales. J Health Psychol. 2005;10:623–31. doi: 10.1177/1359105305055304. [DOI] [PubMed] [Google Scholar]
- 24.Moshki M, Ghofranipour F. Iranian version of Form B of the multidimensional health locus of control scales among the Youth. J Clin Nurs. 2011;20:419–24. doi: 10.1111/j.1365-2702.2010.03479.x. [DOI] [PubMed] [Google Scholar]
- 25.Kline P. 2nd ed. New York: The Guilford Press; 2005. Principles and practice of structural equation modeling. [Google Scholar]
- 26.Hooper D, Couglan J, Mullen MR. Structural equation modeling: Guidelines for determining model fit. Electron J Bus Res Methods. 2008;6:53–60. [Google Scholar]
- 27.Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res Online. 2003;8:23–74. [Google Scholar]
- 28.Lee DT, Yip AS, Leung TY, Chung TK. Identifying women at risk of postnatal depression: Prospective longitudinal study. Hong Kong Med J. 2000;6:349–54. [PubMed] [Google Scholar]
- 29.Yang QM, Lin W, Du M. Strategy and analysis health education and health promotion in community of Shanghai city. Tianjin J Nurs. 2008;16:251–2. [Google Scholar]
- 30.Sabzmakan L, Hazavehei S, Morowatisharifabad M, Hasanzadeh A, Rabiee K, Sadeqi M. The effects of a PRECEDE-based educational program on depression, general health, and quality of life of coronary artery bypass grafting patients. Asian J Psychiatr. 2010;3:79–83. doi: 10.1016/j.ajp.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 31.Lamanna M. Doctoral dissertation. Available from ProQuest Dissertation and Thesis Database; 2000. [Last accessed on 2013 Feb 16]. The relationships among emotional intelligence, locus of control and depression in selected cohorts of women. UMI no. 9990330. [Google Scholar]
- 32.Springer NS, Bogue EL, Arnold M, Yankou D, Oakley D. Nutrition locus of control and dietary behaviors of pregnant women. Appl Nurs Res. 1994;7:28–31. doi: 10.1016/0897-1897(94)90017-5. [DOI] [PubMed] [Google Scholar]
- 33.Benassi VA, Sweeny PD, Dufour CL. Is there a relation between locus of control orientation and depression.? J Abnorm Psychol. 1988;97:3597–67. doi: 10.1037//0021-843x.97.3.357. [DOI] [PubMed] [Google Scholar]
- 34.Moshki M, Tavakolizadeh J, Bahri N. The relationship between health locus of control and life style in pregnant women. Armaghane-danesh. 2010;15:161–70. [Google Scholar]
- 35.Reid V, Meadows-Oliver M. Postpartum depression in adolescent mothers: An integrative review of the literature. J Pediatr Health Care. 2007;21:289–98. doi: 10.1016/j.pedhc.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 36.Masoudnia E. Relationship between perceived social support and risk of postpartum depression disorder. Iran J Nurs. 2011;24:8–18. [Google Scholar]


