Abstract
Objective
To examine the association between demographic and behavioral characteristics and sunburn among U.S. adults.
Method
We used 2010 National Health Interview Survey data (N = 24,970) to conduct multivariable logistic regressions examining associations with having 1 or more sunburns in the past year and having 4 or more sunburns in the past year.
Results
Overall, 37.1% of adults experienced sunburn in the past year. The adjusted prevalence of sunburn was particularly common among adults aged 18–29 years (52.0%), those who repeatedly burn or freckle after 2 weeks in the sun (45.9%), whites (44.3%), indoor tanners (44.1%), those with a family history of melanoma (43.9%), and those who are US-born (39.5%). Physical activity, alcohol consumption, and overweight/obesity were positively associated with sunburn (all P < 0.001); sun protection behaviors were not significantly associated with sunburn (P = 0.35). Among those who were sunburned in the past year, 12.1% experienced 4 or more sunburns.
Conclusion
Sunburn is common, particularly among younger adults, those with a more sun-sensitive skin type, whites, those with a family history of melanoma, the highly physically active, and indoor tanners. Efforts are needed to facilitate sun-safety during outdoor recreation, improve the consistency of sun protection practices, and prevent sunburn, particularly among these subgroups.
Keywords: Sunburn, Skin neoplasms, Primary prevention, Health behavior, Adult
Introduction
As the most common type of cancer in the United States, skin cancer is an urgent public health concern (Stern, 2010). Most of these skin cancers are non-melanoma skin cancers (NMSC) such as basal and squamous cell carcinomas which are treatable but can be disfiguring and costly to treat (Bickers et al., 2006; Guy and Ekwueme, 2011). Melanoma, one of the most common cancers among adults under the age of 40, can be deadly (Weir et al., 2011). In 2010 alone, more than 9000 people in the United States died from melanoma (U.S. Cancer Statistics Working Group, 2013). In addition to the health burden, skin cancer treatment costs were estimated to be $1.7 billion in 2004, with an additional $3.8 billion in costs due to lost productivity (Bickers et al., 2006). Although genetic factors contribute to skin cancer risk, exposure to ultraviolet (UV) radiation from the sun and from artificial sources (i.e., indoor tanning devices) is a well-recognized cause of skin cancer (Armstrong and Kricker, 2001; Boniol et al., 2012; El Ghissassi et al., 2009; IARC, 2007; Lazovich et al., 2010). Research shows that sunburn at any age is associated with an increased risk for melanoma and basal cell carcinoma (Armstrong and Kricker, 2001; Dennis et al., 2008; Veierod et al., 2003). Sunburn often occurs after intermittent UV exposure (e.g., recreational exposure) and indicates both the intensity of the exposure and the individual’s sensitivity to UV radiation.
Previous reports indicate that sunburn is common among adults and is associated with characteristics such as age, sex, race, ethnicity, and skin type (Buller et al., 2011; CDC, 2007; CDC, 2012; National Cancer Institute, 2012). Sunburn and behaviors that can lead to sunburn may also be associated with other health-related behaviors (e.g., smoking and alcohol consumption) (Coups et al., 2008; Heckman et al., 2012) and psychosocial factors (e.g., perceived benefits of tanning) (Heckman et al., 2012). The objective of this study is to examine the association between demographic and behavioral characteristics and sunburn among U.S. adults to inform future skin cancer prevention interventions.
Materials and methods
Study population
We analyzed the data from the 2010 National Health Interview Survey (NHIS), a nationally-representative cross-sectional survey of the civilian, non-institutionalized, U.S. population (CDC, 2013). The main objective of NHIS is to monitor the health of the U.S. population through collection and analysis of data on a broad range of health topics. NHIS data collection involves a complex, multistage sample design, including stratification, clustering, and oversampling of specific population subgroups. Interviews are conducted mainly in person with adults aged 18 years and older within each household, with follow-up by telephone when necessary. The Cancer Control Module and Sample Adult Core obtain additional information from one randomly selected adult in each family. In 2010, 27,157 adults were interviewed, with a final response rate of 60.8% (CDC, 2011). Our analysis included 24,970 respondents after excluding those with a personal history of melanoma (n = 171) and those with unknown or missing responses to the questions about melanoma (n = 37) or sunburn (n = 1979).
Sunburn
Respondents were asked, “During the past 12 months, how many times have you had a sunburn?” If necessary, the survey administrator read the following statement: “By ‘sunburn’ we mean even a small part of your skin turns red or hurts for 12 hours or more. Also include burns from sunlamps and other indoor tanning devices.”
Demographic and behavioral characteristics
Variables examined in relation to sunburn included demographic characteristics (sex, age group, race-ethnicity, marital status, education level, health insurance status, U.S. region, foreign-born status, skin’s reaction after two weeks in the sun, family history of melanoma, and history of a cancer diagnosis), health-related behaviors (sun protection, indoor tanning device use, receipt of a skin exam, physical activity, alcohol consumption, and smoking status), and body mass index (BMI).
Most variables examined in relation to sunburn were based on a single survey item. The exception was the variable for sun protection, which was computed from multiple survey items. Respondents were asked, “When you go outside on a warm sunny day for more than one hour, how often do you:
Stay in the shade?
Wear a hat that shades your face, ears, and neck such as a hat with a wide brim all around?
Wear a long sleeved shirt?
Wear long pants or other clothing that reaches your ankles?
Use sunscreen?”
Response options for each were always, most of the time, sometimes, rarely, and never. We created a dichotomous sun protection variable in which respondents were given a 1 if they reported engaging in at least 1 or more of the protective behaviors always or most of the time and a 0 if they did not. Respondents who reported using sunscreen were asked the SPF number of their sunscreen. Sunscreen use was only counted for respondents using a sunscreen with SPF ≥15. A small percentage of individuals responded to the sun protection questions by saying that they “don’t go out in the sun.” For these analyses, we considered not going out in the sun to be a protective behavior and gave participants a 1 for this response.
Statistical analyses
We examined the association between demographic and behavioral characteristics and having one or more sunburns (versus no sunburn) in the past year among all adults. Because melanoma rates are higher among non-Hispanic whites compared to other racial/ethnic groups (Wu et al., 2011), we repeated this analysis while stratifying by racial/ethnic group. To explore frequent sunburn, we examined the prevalence of having 4 or more sunburns among adults having any sunburn in the past year. We assessed these associations with unadjusted percentages using the Wald chi-square test and adjusted percentages (predictive margins) from multivariable logistic regression models using the Wald-F test (Graubard and Korn, 1999). Because rates of melanoma tend to be higher in young women (under the age of 40) compared with young men but higher among older men compared with older women (Jemal et al., 2011), we tested an interaction between sex and age. We assessed differences between categories within a variable using linear contrasts. The results regarding frequent sunburn were presented only for variables with a P-value of <0.05 in either the unadjusted or the adjusted model. We considered P-values < 0.05 statistically significant.
Because multiple risk behaviors often co-occur, we created a risk behavior index in which we summed the prevalence of 4 risk behaviors: heavy alcohol consumption, being a current smoker, being overweight or obese, and not meeting the 2008 Physical Activity Guidelines for strength or aerobic activity (U.S. Department of Health and Human Services, 2008). Potential scores ranged from 0 (lowest risk) to 4 (highest risk). We reran all analyses using this index in place of the 4 individual behavior variables.
We used SAS-callable SUDAAN to account for the complex sampling design. We calculated national estimates of the prevalence of sunburn, with weights provided with the NHIS data file to account for the probability of selection and non-response.
Results
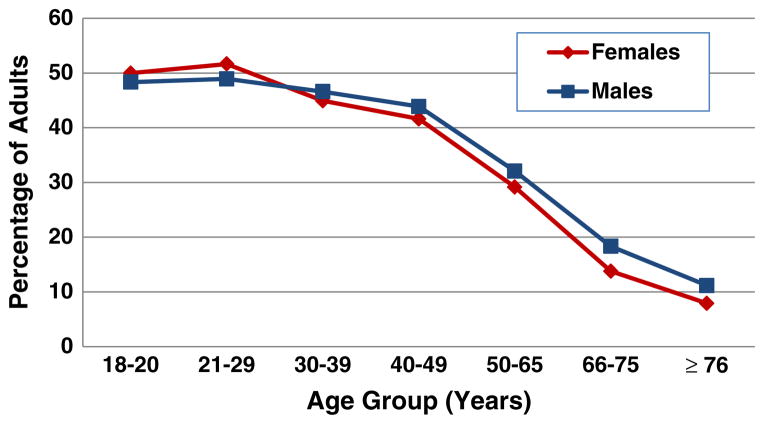
In 2010, an estimated 37.1% of adults aged 18 years and older experienced at least one sunburn in the past 12 months (Table 1). The highest prevalence of sunburn was observed among adults aged 18–29 (52.0%), and the prevalence decreased with age (P < 0.001) (Fig. 1). There was no significant difference in sunburn prevalence between males and females in the adjusted model. The interaction term between age and sex also was not significant (P = 0.273) and was excluded from the model. Sunburn was particularly common among those with skin that burns repeatedly and/or freckles after 2 weeks in the sun (45.9%), whites (44.3%), and those with a family history of melanoma (43.9%). Sunburn varied by U.S. region, ranging from 36.5% in the South to 40.4% in the Midwest (P = 0.001). Sunburn was less common among those who had lived in the U.S. for less than 10 years (22.4%) compared to those who were born in the U.S. (39.5%) or had lived in the U.S. for 10 or more years (33.4%; P < 0.001). Other demographic characteristics associated with sunburn included having at least some college education compared to having less education (P = 0.005) and having private/military insurance (39.2%) compared to other insurance types (35.8%; P = 0.001).
Table 1.
Unadjusted and adjusted percentages of U.S. adults who experienced ≥1 sunburns in the past 12 months, by demographic and behavioral characteristics, National Health Interview Survey, 2010.
| Overall
|
Non-Hispanic whites only
|
||||||
|---|---|---|---|---|---|---|---|
| Sample sizea,b | Unadjusted % (95% CI)c | Pd | Adjusted % (95% CI)c | Pe | Adjusted % (95% CI)c | Pe | |
| Total | 24,970 | 37.1 (36.3, 37.9) | |||||
| Demographic characteristics | |||||||
| Sex | <0.001 | 0.366 | 0.015 | ||||
| Male | 10,996 | 38.6 (37.5, 39.7) | 38.5 (37.4, 39.7) | 47.2 (45.7, 48.6) | |||
| Female | 13,974 | 35.8 (34.7, 36.8) | 37.8 (36.7, 39.0) | 44.6 (43.2, 46.0) | |||
| Age group | <0.001 | <0.001 | <0.001 | ||||
| 18–29 | 4941 | 50.0 (48.1, 51.9) | 52.0 (50.0, 54.1) | 64.6 (62.0, 67.2) | |||
| 30–39 | 4546 | 45.8 (44.0, 47.5) | 47.3 (45.5, 49.1) | 58.6 (56.1, 61.0) | |||
| 40–49 | 4436 | 42.7 (41.0, 44.5) | 42.4 (40.6, 44.2) | 51.8 (49.4, 54.2) | |||
| 50–65 | 6423 | 30.6 (29.2, 32.0) | 29.3 (27.9, 30.8) | 35.7 (33.9, 37.5) | |||
| ≥ 66 | 4624 | 13.0 (11.8, 14.3) | 15.4 (13.8, 17.3) | 18.3 (16.1, 20.7) | |||
| Race/ethnicityf | <0.001 | <0.001 | – | ||||
| White | 14,323 | 44.9 (44.0, 45.9) | 44.3 (43.1, 45.4) | – | |||
| Black | 4078 | 11.0 (9.8, 12.3) | 12.6 (11.1, 14.3) | – | |||
| Hispanic | 4774 | 27.0 (25.4, 28.7) | 31.1 (29.1, 33.2) | – | |||
| Other race | 1709 | 21.1 (18.8, 23.6) | 27.0 (24.0, 30.2) | – | |||
| Marital status | <0.001 | 0.019 | 0.008 | ||||
| Married/living with partner | 12,576 | 38.5 (37.5, 39.5) | 38.5 (37.6, 39.5) | 46.6 (45.4, 47.8) | |||
| Divorced/separated | 4140 | 31.2 (29.4, 33.0) | 37.3 (35.3, 39.3) | 44.2 (41.8, 46.7) | |||
| Widowed | 2278 | 12.3 (10.7, 14.1) | 32.4 (28.8, 36.3) | 38.7 (34.1, 43.5) | |||
| Never married | 5937 | 43.1 (41.3, 44.9) | 38.4 (36.6, 40.2) | 45.8 (43.4, 48.3) | |||
| Education level | <0.001 | 0.005 | 0.096 | ||||
| < High school | 4254 | 23.6 (21.9, 25.3) | 35.4 (33.1, 37.7) | 42.4 (39.1, 45.9) | |||
| High school/GED | 6563 | 33.5 (32.0, 35.1) | 36.6 (35.1, 38.2) | 44.6 (42.6, 46.6) | |||
| Some college | 7454 | 41.3 (40.0, 42.7) | 38.9 (37.6, 40.2) | 46.2 (44.6, 47.9) | |||
| College degree | 6606 | 43.2 (41.6, 44.7) | 39.8 (38.2, 41.5) | 47.4 (45.4, 49.4) | |||
| Insurance category | <0.001 | 0.002 | 0.010 | ||||
| Private/military | 15,338 | 41.3 (40.3, 42.4) | 39.2 (38.2, 40.2) | 46.8 (45.7, 48.0) | |||
| Public only | 4790 | 22.5 (21.0, 24.1) | 35.8 (33.6, 38.2) | 41.9 (38.7, 45.2) | |||
| None/single service | 4725 | 34.4 (32.6, 36.3) | 35.8 (34.0, 37.6) | 43.7 (41.0, 46.4) | |||
| U.S. region | <0.001 | 0.001 | 0.001 | ||||
| Northeast | 3951 | 36.4 (34.7, 38.2) | 37.7 (36.1, 39.4) | 45.3 (43.2, 47.5) | |||
| Midwest | 5493 | 43.6 (42.0, 45.3) | 40.4 (38.9, 41.9) | 48.8 (46.9, 50.6) | |||
| South | 9175 | 32.8 (31.4, 34.2) | 36.5 (35.1, 37.9) | 43.7 (42.0, 45.4) | |||
| West | 6351 | 37.8 (36.1, 39.5) | 38.7 (37.1, 40.3) | 46.0 (43.8, 48.1) | |||
| Foreign-born status | <0.001 | <0.001 | <0.001 | ||||
| Born in the US | 19,604 | 40.2 (39.4, 41.1) | 39.5 (38.6, 40.4) | 46.4 (45.4, 47.5) | |||
| <10 years | 1237 | 17.8 (12.3, 20.7) | 22.4 (19.1, 26.0) | 18.4 (13.0, 25.4) | |||
| 10+ years | 4068 | 23.1 (21.5, 24.8) | 33.4 (31.0, 35.8) | 42.1 (37.6, 46.7) | |||
| Skin’s reaction after 2 weeks in the sun | <0.001 | <0.001 | <0.001 | ||||
| Very dark tan | 3275 | 31.5 (29.6, 33.4) | 33.2 (31.2, 35.3) | 37.4 (34.5, 40.3) | |||
| Moderate tan | 7797 | 40.0 (38.7, 41.4) | 37.8 (36.5, 39.1) | 44.6 (42.9, 46.3) | |||
| Mild tan | 7434 | 38.0 (36.6, 39.4) | 38.6 (37.2, 40.0) | 47.7 (45.9, 49.5) | |||
| Burn repeatedly/freckle | 3609 | 49.2 (47.3, 51.1) | 45.9 (44.0, 47.7) | 53.6 (51.6, 55.6) | |||
| Do not go out in the sun | 2273 | 10.7 (9.0, 12.5) | 23.7 (20.8, 27.0) | 25.9 (21.4, 31.0) | |||
| Family history of melanoma | <0.001 | 0.011 | 0.008 | ||||
| Yes | 480 | 49.4 (44.2, 54.5) | 43.9 (39.4, 48.5) | 52.5 (47.5, 57.4) | |||
| No | 23,306 | 37.3 (36.5, 38.2) | 38.0 (37.2, 38.9) | 45.7 (44.6, 46.7) | |||
| Ever been told you had cancer | <0.001 | 0.969 | 0.506 | ||||
| Yes | 1994 | 28.1 (25.8, 30.6) | 38.1 (35.5, 40.8) | 46.9 (43.9, 50.0) | |||
| No | 22,976 | 37.9 (37.0, 38.7) | 38.2 (37.3, 39.1) | 45.8 (44.7, 46.9) | |||
| Behavioral characteristics | |||||||
| Sun protection | <0.001 | 0.499 | 0.056 | ||||
| Yes | 6792 | 42.1 (40.7, 43.7) | 38.0 (37.0, 39.0) | 45.2 (44.0, 46.5) | |||
| No | 9443 | 37.1 (35.8, 38.4) | 38.6 (37.2, 39.9) | 47.3 (45.6, 49.0) | |||
| Indoor tanning device use | <0.001 | <0.001 | 0.001 | ||||
| Yes | 1159 | 62.1 (58.7, 65.3) | 44.1 (40.9, 47.4) | 51.6 (48.1, 55.1) | |||
| No | 23,796 | 35.7 (34.9, 36.5) | 37.7 (36.9, 38.6) | 45.4 (44.3, 46.4) | |||
| Ever had a skin exam | 0.842 | 0.015 | 0.013 | ||||
| Yes | 4892 | 37.3 (35.7, 39.0) | 36.4 (34.9, 38.0) | 43.9 (42.0, 45.8) | |||
| No | 19,965 | 37.1 (36.2, 38.1) | 38.7 (37.7, 39.6) | 46.6 (45.5, 47.8) | |||
| Meets 2008 physical activity guidelines for Americans | <0.001 | <0.001 | <0.001 | ||||
| Meets neither criteria | 12,854 | 30.2 (29.1 31.2) | 35.9 (34.7, 37.1) | 43.1 (41.6, 44.7) | |||
| Meets strength only | 940 | 31.8 (27.9, 36.0) | 36.2 (32.2, 40.3) | 43.7 (38.4, 49.1) | |||
| Meets aerobic only | 6165 | 41.5 (40.0, 43.0) | 39.2 (37.8, 40.7) | 47.4 (45.7, 49.2) | |||
| Meets both aerobic and strength criteria | 4706 | 48.5 (46.8, 50.2) | 41.7 (40.0, 43.3) | 49.3 (47.3, 51.3) | |||
| Alcohol consumption | <0.001 | <0.001 | <0.001 | ||||
| Never drinker | 5528 | 24.8 (23.2, 26.5) | 33.2 (31.3, 35.1) | 40.5 (37.7, 43.4) | |||
| Former drinker | 3791 | 27.3 (25.5, 29.1) | 35.8 (33.7, 38.0) | 43.3 (40.7, 45.9) | |||
| Current drinker | 15,651 | 43.2 (42.2, 44.1) | 39.8 (38.9, 40.8) | 47.3 (46.2, 48.5) | |||
| Smoking status | 0.003 | 0.183 | 0.040 | ||||
| Current smoker | 4755 | 38.9 (37.1, 40.6) | 36.7 (34.9, 38.5) | 43.4 (41.2, 45.6) | |||
| Former smoker | 5294 | 35.0 (33.5, 36.7) | 38.7 (37.1, 40.4) | 46.7 (44.8, 48.7) | |||
| Never smoker | 14,896 | 37.3 (36.3, 38.4) | 38.5 (37.4, 39.6) | 46.5 (45.2, 47.9) | |||
| Overweight or obese | 0.678 | <0.001 | <0.001 | ||||
| Yes | 15,381 | 37.4 (35.8, 38.3) | 39.9 (38.9, 40.9) | 39.9 (38.9, 40.9) | |||
| No | 8978 | 37.1 (35.8, 38.3) | 35.3 (34.1, 36.6) | 37.1 (35.8, 38.3) | |||
Total sample size for each variable may not add to 24,970 because of missing.
Overall adjusted analysis is based on a sample of 22,082 adults. The adjusted analysis limited to non-Hispanic whites is based on 12,856 adults.
Percentages are weighted to the non-institutionalized population.
P values based on Wald χ2 test for association.
P values based on overall Wald F test for association from multivariable logistic regression models.
Persons identified as Hispanic might be of any race. Persons identified as white, black, or other race are all non-Hispanic.
Fig. 1.
Percentage of U.S. adults who experienced ≥1 sunburn in the past 12 months, by sex and age group, National Health Interview Survey, 2010.
The adjusted sunburn prevalence was also positively associated with indoor tanning device use, physical activity, alcohol consumption, and being overweight or obese (all P < 0.001) (Table 1). With regard to physical activity, adults who met the 2008 Physical Activity Guidelines for both strength and aerobic activity (U.S. Department of Health and Human Services, 2008) had the highest prevalence of sunburn (41.7%), followed by those who met the guidelines for aerobic activity only (39.2%; P < 0.001). With regard to alcohol consumption, sunburn was more common among current drinkers (39.8%) compared to both former (35.8%) and never drinkers (33.2%; P < 0.001). Sunburn was negatively associated with ever having had a skin exam (P = 0.015). Sunburn was not significantly associated with smoking status or sun protection. As a sensitivity analysis, we ran a separate model in which we did not count “do not go in the sun” in the sun protection variable; this model yielded very similar results. Findings were also very similar when the analysis was limited to non-Hispanic whites only (Table 1). The one notable difference was that among non-Hispanic whites, those who used sun protection were less likely to experience sunburn, an association that approached statistical significance (P = 0.056). This trend was not observed for the other racial/ethnic groups (data not shown).
Among adults who experienced sunburn in the past 12 months, 12.1% had 4 or more sunburns (Table 2). Experiencing 4 or more sunburns was negatively associated with age group (P < 0.001) and was common among ages 18–29 years (16.0%), blacks (18.5%), those with skin that burns or freckles repeatedly after 2 weeks in the sun (19.1%), and those who “do not go out in the sun” (23.4%). We found similar patterns for all analyses when we reran them using the risk behavior index in place of individual behavior variables; the index was positively associated with sunburn (results not shown).
Table 2.
Unadjusted and adjusted percentages of adults who experienced 4 or more sunburns in the past 12 months (among those experienced any sunburn), National Health Interview Survey, 2010.
| Unadjusted % (95% CI)a (n = 8146) | Pb | Adjusted % a,c (95% CI) | Pd | |
|---|---|---|---|---|
| Total | 12.1 (11.3, 12.9) | |||
| Demographic characteristics | ||||
| Sex | 0.298 | 0.236 | ||
| Male | 12.6 (11.3, 14.0) | 12.5 (11.2, 14.0) | ||
| Female | 11.6 (10.5, 12.8) | 11.3 (10.1, 12.6) | ||
| Age group | <0.001 | <0.001 | ||
| 18–29 | 15.4 (13.6, 17.3) | 16.0 (13.8, 18.5) | ||
| 30–39 | 12.7 (11.2, 14.4) | 12.0 (10.5, 13.7) | ||
| 40–49 | 10.1 (8.6, 11.9) | 10.5 (9.0, 12.3) | ||
| 50–65 | 9.3 (7.9, 11.0) | 8.4 (6.8, 10.2) | ||
| ≥ 66 | 10.2 (7.7, 13.4) | 9.1 (6.5, 12.7) | ||
| Race/ethnicitye | <0.001 | 0.011 | ||
| White | 12.1 (11.2, 13.1) | 11.9 (11.0, 13.0) | ||
| Black | 19.1 (15.1, 24.0) | 18.5 (13.9, 24.2) | ||
| Hispanic | 11.1 (9.2, 13.3) | 10.5 (8.5, 12.9) | ||
| Other race | 7.3 (4.6, 11.6) | 9.1 (5.6, 14.6) | ||
| Marital status | 0.010 | 0.536 | ||
| Married/living with partner | 11.0 (10.0, 12.1) | 11.4 (10.3, 12.6) | ||
| Divorced/separated | 12.0 (9.9, 14.5) | 13.2 (10.7, 16.3) | ||
| Widowed | 11.6 (7.7, 17.2) | 12.1 (7.3, 19.4) | ||
| Never married | 14.9 (13.1, 17) | 12.7 (10.9, 14.7) | ||
| U.S. region | 0.014 | 0.005 | ||
| Northeast | 9.8 (8.0, 11.8) | 8.9 (7.0, 11.3) | ||
| Midwest | 13.4 (11.8, 15.2) | 13.8 (12.2, 15.7) | ||
| South | 12.9 (11.5, 14.5) | 12.7 (11.2, 14.5) | ||
| West | 11.3 (9.8, 12.9) | 10.8 (9.3, 12.6) | ||
| Skin’s reaction after 2 weeks in the sun | <0.001 | <0.001 | ||
| Very dark tan | 9.7 (7.8, 12.0) | 9.8 (7.8, 12.1) | ||
| Moderate tan | 8.9 (7.7, 10.3) | 8.4 (7.2, 9.8) | ||
| Mild tan | 11.3 (9.9, 13.0) | 11.4 (9.9, 13.1) | ||
| Burn repeatedly/freckle | 18.6 (16.4, 21.0) | 19.1 (16.8, 21.6) | ||
| Do not go out in the sun | 23.5 (17.5, 30.6) | 23.4 (17.3, 30.8) | ||
| Behavioral characteristics | ||||
| Meets 2008 Physical Activity Guidelines for Americans | 0.021 | 0.032 | ||
| Meets neither criteria | 11.0 (9.8, 12.5) | 10.4 (9.1, 11.9) | ||
| Meets strength only | 9.0 (5.9, 13.6) | 10.0 (6.4, 15.2) | ||
| Meets aerobic only | 12.1 (10.6, 13.8) | 12.4 (10.9, 14.2) | ||
| Meets both aerobic and strength criteria | 13.9 (12.3, 15.6) | 13.8 (12.1, 15.7) | ||
| Overweight or obese | 0.276 | 0.012 | ||
| Yes | 12.5 (11.4, 13.6) | 12.9 (11.7, 14.1) | ||
| No | 11.5 (10.1, 13.0) | 10.5 (9.2, 11.9) | ||
Note: only variables with a significance level of <0.05 in the unadjusted or adjusted models are presented in this table except for sex. In addition to the variables shown in the table, the adjusted model includes the following variables: education level, insurance category, foreign-born status, family history of melanoma, ever been told of having cancer, sun protection behaviors, indoor tanning device use, ever had a skin exam, alcohol consumption, being overweight or obese, and smoking status.
Percentages are weighted to the non-institutionalized population.
P values based on Wald χ2 test for association.
The adjusted model is based on a sample of 7437 respondents.
P values based on overall Wald F test for association from multivariable logistic regression models.
Persons identified as Hispanic might be of any race. Persons identified as white, black, or other race are all non-Hispanic.
Discussion
Sunburn is common among U.S. adults, especially among younger adults and those who are most susceptible to skin cancer (i.e., whites, those with skin that burns repeatedly, and those with a family history of melanoma). Sunburn risk can be reduced by engaging in protective behaviors when outdoor in the sun. The lack of a strong association between sunburn and sun protection may suggest a need to further examine 1) the relative importance of different sun protective behaviors, 2) the clustering of sun protective behaviors, and 3) compliance with recommendations for sunburn avoidance.
The relationship observed between sunburn and foreign-born status is consistent with other research showing that more acculturated individuals demonstrate riskier skin cancer-related behaviors (Andreeva et al., 2009). The association between sunburn and other risky behaviors (i.e., alcohol use and overweight/obesity) indicates that some risky behaviors may cluster, suggesting a need for more comprehensive health promotion efforts that address multiple health behaviors. Previous research indicates that excess body weight is associated with a decreased risk for NMSC but not for melanoma (Pothiawala et al., 2012; Tang et al., 2013). Those who are overweight or obese may experience less chronic sun exposure compared to those who are of normal weight but may be more likely to experience intermittent sun exposure. This would explain the seemingly contradictory findings of a lower risk for NMSC and a higher risk for sunburn (Pothiawala et al., 2012). The association with indoor tanning suggests a link between sunburn and appearance-related behaviors. Although the data do not allow for conclusions regarding how the sunburns happened, some may have occurred while individuals were trying to get a tan. The association between sunburn and physical activity may reflect increased incidental sun exposure among the more physically active. Previous research suggests that more physically active individuals may engage in more skin cancer risk-related behaviors than those who are sedentary (Coups et al., 2008), or as a function of their recreational pursuits, may engage similarly to the physically inactive in overall sun protection, but use different strategies (i.e., use of clothing and chemical barriers rather than sun avoidance strategies) and require greater than average vigilance with sun protection (Lawler et al., 2007). Collectively, these findings suggest a need for more coordination across efforts to improve sun-safety and efforts to increase physical activity. One potential strategy would be to leverage shared partnerships with relevant organizations and stakeholders to create environments and incorporate practices that promote both sun-safety and physical activity (e.g., increasing shade availability in outdoor recreational spaces, including sunscreen use and reapplication prompts along with hydration recommendation messaging, encouraging use of sport specific clothing with an adequate SPF).
Having 4 or more sunburns in the past 12 months occurred among 12% of adults experiencing sunburn and was particularly common among those who do not go out in the sun. This is a novel finding that has not previously been discussed in the literature. Some of these results could be due in part to limitations of self-reported data and misunderstanding of the survey questions. It is also possible that those who report that they avoid going in the sun altogether may do so because of extreme skin sensitivity to the sun. This extreme sun-sensitivity might explain why some individuals are getting frequent burns in spite of efforts to avoid the sun. Those who do not often go outdoors for extended periods of time may also be less prepared to protect themselves when they do spend time outdoors. Frequent sunburn was also common among blacks. Skin type and sun-sensitivity vary greatly among blacks (Galindo et al., 2007; Pichon et al., 2010), and previous research indicates that blacks may be less likely to engage in certain protective behaviors, particularly sunscreen use, compared to other racial/ethnic groups (CDC 2012; Pinchon et al., 2010). Efforts to make sun protection the easy or default choice may help to reduce barriers to sunburn avoidance (Frieden 2010). Additionally, more nuanced public health messaging tailored to the various skin types may help to clarify misunderstandings about susceptibility.
These findings may inform future interventions to reduce skin cancer risk-related behaviors, particularly regarding target audiences and key intervention strategies. For example, the prevalence of frequent sunburn among all racial/ethnic groups indicates the importance of using photosensitivity to identify those at increased skin cancer risk, rather than relying solely on race/ethnicity. Furthermore, UV exposure can be either intentional (e.g., sunbathing and indoor tanning) or incidental (e.g., sun exposure during outdoor activities), and different strategies may be needed to address these different types of UV exposure. UV exposure is well-documented as causing premature skin aging, and consistent use of sun protection when outdoors and regular sunscreen use may help to prevent or delay photoaging (Fisher et al., 2002; Hughes et al., 2013; Wlaschek et al., 2001), in addition to reducing skin cancer risk (Green et al., 2011; van der Pols et al., 2006). The opportunity to prevent photoaging may be particularly motivating for those concerned about their appearance (e.g., tanners), and recent evidence suggests that appearance-related messages are effective in reducing UV exposure among young women (Lin et al., 2011). The US Preventive Services Task Force recommends counseling in a clinical setting for children, adolescents, and young adults aged 10 to 24 years who have fair skin about minimizing their exposure to ultraviolet radiation to reduce risk for skin cancer (USPSTF 2012). Such counseling could include cancer prevention or appearance-focused messages and could be done during a primary care visit (Lin et al., 2011; USPSTF 2012).
Different messages or intervention strategies may be needed for older adults, men, and individuals who do not necessarily seek out a tan but regularly engage in outdoor activities. For example, active individuals who spend much of their recreational time outdoors may benefit from environmental supports that facilitate sun-safety (e.g., shaded outdoor areas). Additionally, men are less likely to use sunscreen compared to women (CDC, 2012), so the use of other sun protection methods may be more appealing to men. More research is needed to determine the most effective approaches for increasing sun safety and preventing sunburn among these different subgroups.
Study limitations and strengths
This study has both strengths and limitations that should be considered. The use of a nationally-representative sample means that results are generalizable to the U.S. population, and ongoing collection of such data allows for continued monitoring of sunburn among U.S. adults. Furthermore, the large sample size and numerous demographic and behavioral variables allowed us to explore differences across many key subgroups. However, this study relied on the use of many single item indicators of health behaviors which introduces the potential for measurement error. The variable we used to measure sun protection is particularly limited because it does not take into account the use of multiple sun protective behaviors, the amount of exposed skin, or the time and intensity of participants’ UV exposure. There may also be residual confounding, as those who are the most sun-sensitive may also be most likely to engage in sun protective behaviors. Furthermore, the data are self-reported and subject to potential bias (e.g., recall bias and socially desirable responses), and the cross-sectional design limits the exploration of cohort effects and causal associations.
Conclusions
Sunburn is an important and preventable skin cancer risk factor. The results from this study indicate that sunburn is common among U.S. adults, especially among younger adults and those who are most susceptible to skin cancer. Given the high prevalence of skin cancer, sunburn prevention is critical. More public health efforts are needed, including environmental supports to facilitate sun safety during outdoor recreation and more targeted prevention efforts focusing on specific subgroups (i.e., intentional tanners, those who engage in frequent outdoor recreation, and those at an increased risk for skin cancer).
Footnotes
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official positions of the Centers for Disease Control and Prevention or the National Cancer Institute.
Conflict of interest
The authors declare that there are no conflicts of interest.
Contributor Information
Zahava Berkowitz, Email: zab3@cdc.gov.
Gery P. Guy, Jr., Email: irm2@cdc.gov.
Anne M. Hartman, Email: hartmana@mail.nih.gov.
References
- Andreeva VA, Unger JB, Yaroch AL, Cockburn MG, Baezconde-Garbanati L, Reynolds KD. Acculturation and sun-safe behaviors among US Latinos: findings from the 2005 Health Information National Trends Survey. Am J Public Health. 2009;99 (4):734–741. doi: 10.2105/AJPH.2007.122796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8–18. doi: 10.1016/s1011-1344(01)00198-1. [DOI] [PubMed] [Google Scholar]
- Bickers DR, Lim HW, Margolis D, et al. The burden of skin diseases: 2004. A joint project of the American Academy of Dermatology Association and the Society for Investigative Dermatology. J Am Acad Dermatol. 2006;55 (3):490–500. doi: 10.1016/j.jaad.2006.05.048. [DOI] [PubMed] [Google Scholar]
- Boniol M, Autier P, Boyle P, Gandini S. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis. BMJ. 2012;345:e4757. doi: 10.1136/bmj.e4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buller DB, Cokkinides V, Hall HI, et al. Prevalence of sunburn, sun protection, and indoor tanning behaviors among Americans: review from national surveys and case studies of 3 states. J Am Acad Dermatol. 2011;65 (5):S114–S123. doi: 10.1016/j.jaad.2011.05.033. [DOI] [PubMed] [Google Scholar]
- CDC. MMWR. Sunburn prevalence among adults — United States, 1999, 2003, and 2004. MMWR. 2007;56 (21):524–528. ( http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5621a2.htm) [PubMed] [Google Scholar]
- CDC. NHIS Survey Description. Hyattsville, MD: 2011. 2010 National Health Interview Survey (NHIS) Public Use Data Release. (Available online: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2010/srvydesc.pdf) [Google Scholar]
- CDC. MMWR. Sunburn and sun protective behaviors among adults aged 18–29 years — United States, 2000–2010. MMWR. 2012;61 (18):317–322. ( http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6118a1.htm?s_cid=mm6118a1_w) [PubMed] [Google Scholar]
- CDC. National Health Interview Survey. 2013 (Available online: http://www.cdc.gov/nchs/nhis.htm.)
- Coups EJ, Manne SL, Heckman CJ. Multiple skin cancer risk behaviors in the U.S. population. AJPM. 2008;34 (2):87–93. doi: 10.1016/j.amepre.2007.09.032. [DOI] [PubMed] [Google Scholar]
- Dennis LK, VanBeek MJ, Beane Freeman LE, Smith BJ, Dawson DV, Coughlin JA. Sunburns and risk of cutaneous melanoma, does age matter: a comprehensive meta-analysis. Ann Epidemiol. 2008;18 (8):614–627. doi: 10.1016/j.annepidem.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Ghissassi F, Baan R, Straif K, et al. A review of human carcinogens — part D: radiation. Lancet Oncol. 2009;10 (8):751–752. doi: 10.1016/s1470-2045(09)70213-x. [DOI] [PubMed] [Google Scholar]
- Fisher GJ, Kang S, Varani J, et al. Mechanisms of photoaging and chronological skin aging. Arch Dermatol. 2002;138 (11):1462–1470. doi: 10.1001/archderm.138.11.1462. [DOI] [PubMed] [Google Scholar]
- Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100 (4):590–595. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galindo GR, Mayer JA, Slymen D, et al. Sun sensitivity in 5 US ethnoracial groups. Cutis. 2007;80 (1):25–30. [PubMed] [Google Scholar]
- Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55 (2):652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol. 2011;29 (3):257–263. doi: 10.1200/JCO.2010.28.7078. [DOI] [PubMed] [Google Scholar]
- Guy GP, Jr, Ekwueme DU. Years of potential life lost and indirect costs of melanoma and non-melanoma skin cancer: a systematic review of the literature. Pharmacoeconomics. 2011;29 (10):863–874. doi: 10.2165/11589300-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Heckman CJ, Darlow S, Cohen-Filipic J, et al. Psychosocial correlates of sunburn among young adult women. Int J Environ Res Public Health. 2012;9:2241–2251. doi: 10.3390/ijerph9062241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes MCB, Williams GM, Baker P, Green AC. Sunscreen and prevention of aging: a randomized trial. Ann Intern Med. 2013;158:781–790. doi: 10.7326/0003-4819-158-11-201306040-00002. [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer. Working Group on artificial ultraviolet light, skin cancer. The association of use of sunbeds with cutaneous malignant melanoma and other skin cancers: a systematic review. Int J Cancer. 2007;120 (5):1116–1122. doi: 10.1002/ijc.22453. [DOI] [PubMed] [Google Scholar]
- Jemal A, Saraiya M, Patel P, et al. Recent trends in cutaneous melanoma incidence and death rates in the United States, 1992–2006. J Am Acad Dermatol. 2011;65:S17–S25. doi: 10.1016/j.jaad.2011.04.032. [DOI] [PubMed] [Google Scholar]
- Lawler S, Sugiyama T, Owen N. Sun exposure concern, sun protection behaviors and physical activity among Australian adults. Cancer Causes Control. 2007;18 (9):1009–1014. doi: 10.1007/s10552-007-9041-5. [DOI] [PubMed] [Google Scholar]
- Lazovich D, Vogel RI, Berwick M, Weinstock MA, Anderson KE, Warshaw EM. Indoor tanning and risk of melanoma: a case–control study in a highly exposed population. Cancer Epidemiol Biomarkers Prev. 2010;19 (6):1557–1568. doi: 10.1158/1055-9965.EPI-09-1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin JS, Eder M, Weinmann S. Behavioral counseling to prevent skin cancer: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;154 (3):190–201. doi: 10.7326/0003-4819-154-3-201102010-00009. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. Cancer trends progress report — 2011/2012 update. Bethesda, MD: 2012. National Institutes of Health, Department of Health and Human Services. http://progressreport.cancer.gov. [Google Scholar]
- Pichon LC, Landrine H, Corral I, Hao Y, Mayer JA, Hoerster KD. Measuring skin cancer risk in African Americans: is the Fitzpatrick Skin Type Classification Scale culturally sensitive? Ethn Dis. 2010;20:174–179. [PubMed] [Google Scholar]
- Pinchon LC, Corral I, Landrine H, Mayer JA, Norman GJ. Sun-protection behaviors among African Americans. Am J Prev Med. 2010;38 (3):288–295. doi: 10.1016/j.amepre.2009.10.041. [DOI] [PubMed] [Google Scholar]
- Pothiawala S, Qureshi AA, Li Y, Han J. Obesity and the incidence of skin cancer in US Caucasians. Cancer Causes Control. 2012;23 (5):717–726. doi: 10.1007/s10552-012-9941-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern RS. Prevalence of a history of skin cancer in 2007: results of an incidence-based model. Arch Dermatol. 2010;146 (3):279–282. doi: 10.1001/archdermatol.2010.4. [DOI] [PubMed] [Google Scholar]
- Tang JY, Henderson MT, Hernandez-Boussard T, et al. Lower skin cancer risk in women with higher body mass index: the women’s health initiative observational study. Cancer Epidemiol Biomarkers Prev. 2013;22:2412–2415. doi: 10.1158/1055-9965.EPI-13-0647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2010 Incidence and Mortality Web-based Report. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; Atlanta: 2013. (Available at: www.cdc.gov/uscs) [Google Scholar]
- U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. 2008 (Available at: http://www.health.gov/paguidelines/pdf/paguide.pdf.)
- U.S. Preventive Services Task Force. Behavioral counseling to prevent skin cancer. US Preventive Services Task Force recommendation statement. 2012 May; (Available at: http://www.uspreventiveservicestaskforce.org/uspstf11/skincancouns/skincancounsrs.htm.)
- van der Pols JC, Williams GM, Pandeya N, Logan V, Green AC. Prolonged prevention of squamous cell carcinoma of the skin by regular sunscreen use. Cancer Epidemiol Biomarkers Prev. 2006;15 (12):2546–2548. doi: 10.1158/1055-9965.EPI-06-0352. [DOI] [PubMed] [Google Scholar]
- Veierod MB, Weiderpass E, Thorn M, et al. A prospective study of pigmentation, sun exposure, and risk of cutaneous malignant melanoma in women. J Natl Cancer Inst. 2003;95 (20):1530–1538. doi: 10.1093/jnci/djg075. [DOI] [PubMed] [Google Scholar]
- Weir HK, Marrett LD, Cokkinides V, et al. Melanoma in adolescents and young adults (ages 15–39 years): United States, 1999–2006. JAAD. 2011;65 (5):S38–S49. doi: 10.1016/j.jaad.2011.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wlaschek M, Tantcheva-Poor I, Naderi L, et al. Solar UV irradiation and dermal photoaging. J Photochem Photobiol. 2001;63:45–51. doi: 10.1016/s1011-1344(01)00201-9. [DOI] [PubMed] [Google Scholar]
- Wu X, Eide MJ, King J, et al. Racial and ethnic variations in incidence and survival of cutaneous melanoma in the United States, 1999–2006. J Am Acad Dermatol. 2011;65 (5):S26–S37. doi: 10.1016/j.jaad.2011.05.034. [DOI] [PubMed] [Google Scholar]