Abstract
Background
Cardiopulmonary arrests are rare, high-stakes events that benefit from using crisis resource management (CRM). Simulation-based education with deliberate practice can promote skill acquisition.
Objective
We assessed whether using simulation-based education to teach CRM would lead to improved performance, compared to a lecture format.
Methods
We tested third-year internal medicine residents in simulated code scenarios. Participants were randomly assigned to simulation-based education with deliberate practice (SIM) group or lecture (LEC) group. We created a checklist of CRM critical actions (which includes announcing the diagnosis, asking for help/suggestions, and assigning tasks), and reviewed videotaped performances, using a checklist of skills and communications patterns to identify CRM skills and communication efforts. Subjects were tested in simulated code scenarios 6 months after the initial assessment.
Results
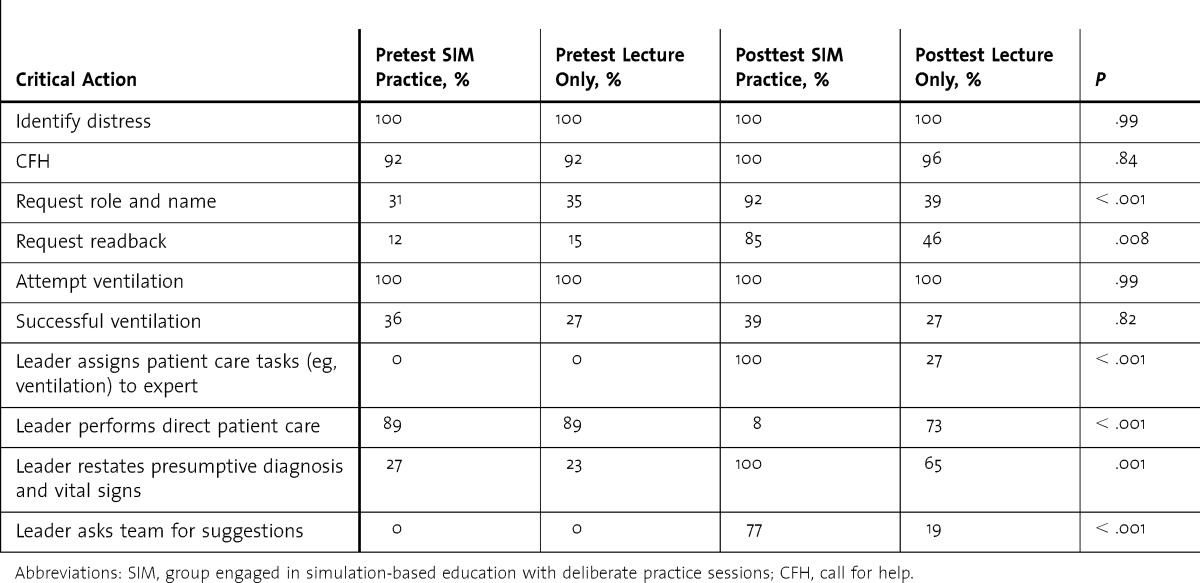
At baseline, all 52 subjects recognized distress, and 92% (48 of 52) called for help. Seventy-eight percent (41 of 52) did not succeed in resuscitating the simulated patient or demonstrate the CRM skills. After intervention, both groups (n = 26 per group) improved. All SIM subjects announced the diagnosis compared to 65% LEC subjects (17 of 26, P = .01); 77% (20 of 26) SIM and 19% (5 of 26) LEC subjects asked for suggestions (P < .001); and 100% (26 of 26) SIM and 27% (7 of 26) LEC subjects assigned tasks (P < .001).
Conclusions
The SIM intervention resulted in significantly improved team communication and cardiopulmonary arrest management. During debriefing, participants acknowledged the benefit of the SIM sessions.
What was known
Simulation-based education with deliberate practice can promote skill acquisition.
What is new
Study assesses internal medicine residents' skills after a simulation-based intervention compared to a traditional lecture format to learn team communication and crisis resource management (CRM).
Limitations
Single institution, and small sample size limit generalizability.
Bottom line
Residents exposed to simulation communicated and completed CRM skills more effectively than those taught in a lecture format.
Introduction
Effective communication and coordinated teamwork are critical to the successful management of complex events such as cardiac arrests or “codes.”1–5 Delays in resuscitation can result in poor outcomes.6–8 The essential “call for help” summons the emergency response personnel that the code leader must direct.1 While crisis resource management (CRM) skills have been adapted from industry to medicine to enhance team performance,3,9–15 these skills often are not explicitly taught during medical education.3,9,12,13,16–19
Simulation-based education improves learner knowledge and skills, and allows practice in controlled, safe environments.12,13,20 Deliberate practice, a feedback-based educational method, requires continued practice of challenging skills.21,22 Simulation-based education combined with deliberate practice8–26 promotes skill acquisition27–32 and adherence to Advanced Cardiac Life Support (ACLS) algorithms.25,26,32
Senior internal medicine residents at Cooper University Hospital routinely act as code leaders. All receive medical education about codes, but not CRM skills required to manage resuscitation efforts. We hypothesized that using simulation with deliberate practice to teach CRM skills to code leaders would improve performance of targeted measures when compared with a lecture format.
Methods
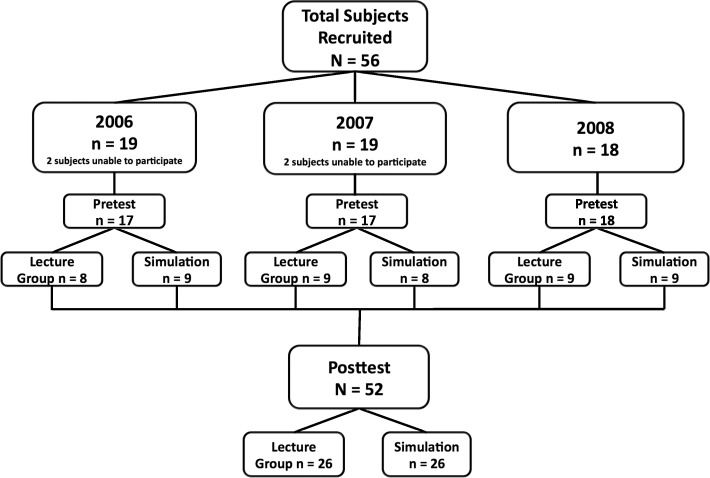
For academic years 2006–2007 through 2008–2009, all senior postgraduate year (PGY)–3 internal medicine residents were invited to participate in the study. Participants within each year were randomly assigned to 2 groups: the lecture (LEC) group attended 2 lectures about team management, and the simulation (SIM) group engaged in simulation-based education with deliberate practice sessions (figure).
FIGURE.
Study Design
All participants had 2 clinical months in the intensive care unit and had managed a minimum of 5 codes as leader. All participants were certified in Basic and Advanced Cardiac Life Support.
Scenario Development
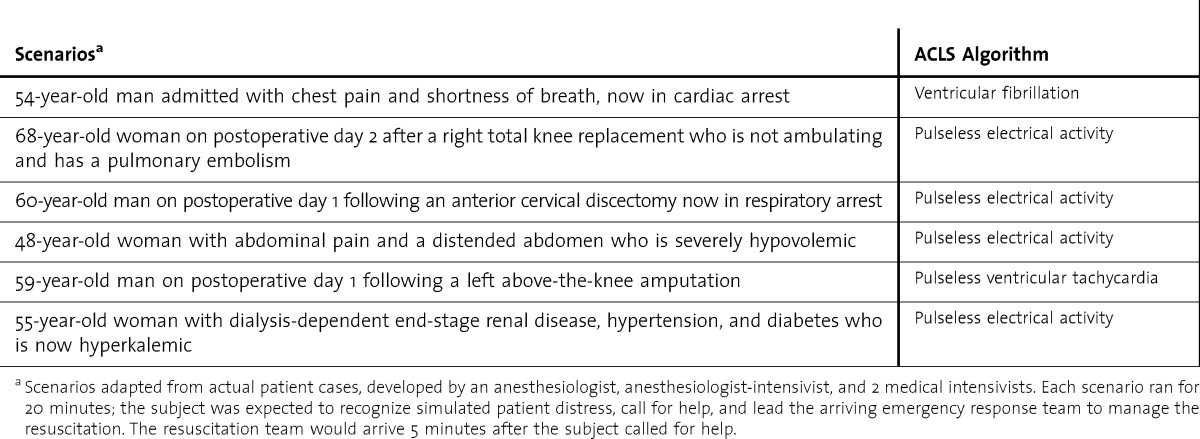
Six arrest scenarios (table 1) were created for testing purposes to assure that content was not shared among groups. Checklists of critical events that code leaders should perform were created and consensus was reached via a modified Delphi method.33
TABLE 1.
Scenario Events and Advanced Cardiac Life Support (ACLS) Algorithm
Preparing the Simulation Sessions and Briefing the Participants
Each resident was introduced to the functions and limitations of the high-fidelity simulator, SimMan (Laerdal Medical). A brief medical record outlining the simulated patient's history was placed in the room. Participants were required to recognize apnea and unresponsiveness, call for help, and lead the resuscitation team. This team consisted of 2 experienced anesthesiologists, 1 of whom was an intensivist, and a critical care nurse. Participants were told to verbalize all requests of the responding team. The team was instructed to provide requested information and assistance.
Debriefing and Intervention
Following the baseline simulation, each participant received an individual debriefing on his or her performance that identified areas for improvement. During debriefing, each participant's comfort during the scenario was assessed through questions. Participants were randomly assigned to 1 of 2 equal groups for teaching critical CRM skills (box 1). The SIM group engaged in 2 separate 2-hour simulation SIM sessions, the LEC group attended 2 separate 2-hour lectures. Both interventions taught the critical CRM skills (box 1). Lectures were taught by 2 anesthesiologists and a critical care nurse. All participants were individually tested 6 months after the educational interventions, 1 month before graduation.
box 1 Critical Crisis Resource Management Actions
Identify distress
Call for help
Request name and role of arriving code team personnel
Request readback of statements and requests (ie, the subject should ask the team to repeat all requests to administer medications, medication name, dose, route of administration, and completion of tasks)
Attempt ventilation
Successful ventilation
Leader does not perform direct patient care and assigns all tasks to the appropriate team member (eg, assigns ventilation to an expert)
Leader restates presumptive diagnosis and vital signs
Leader asks team for suggestions
Video Review of Scenarios
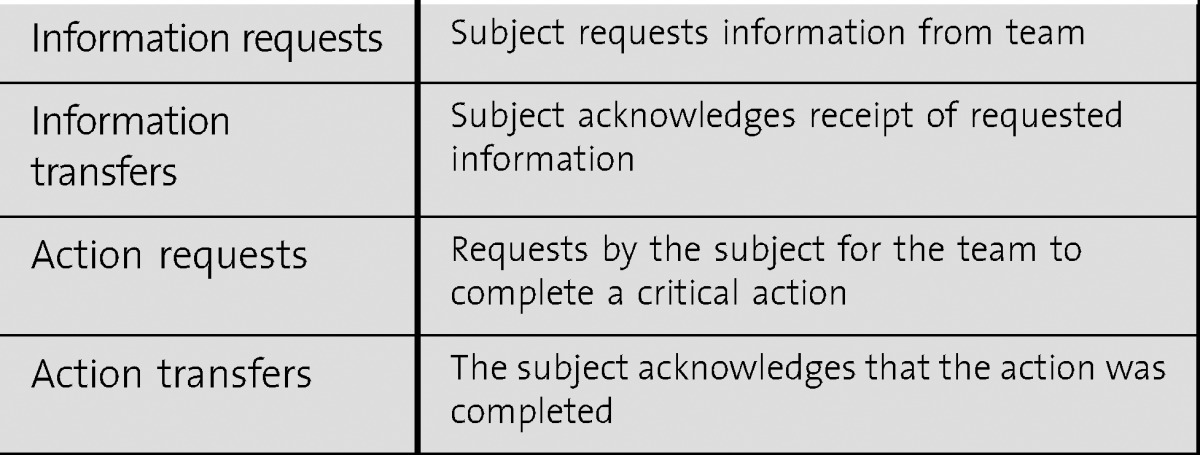
All scenarios were videotaped and reviewed to assess performance of critical actions (box 1) and communication patterns (box 2).
box 2 Critical Communication Matrix Elements
The study was approved by the Cooper Health System Institutional Review Board, and all participants gave consent.
Communication Pattern Review—Leader-Team Interaction Analysis of Preintervention and Postintervention Videos
To characterize and analyze team performance and decision-making processes between the participant and the team, we constructed a communication matrix and reviewed the simulation videos to evaluate the interaction between the code leaders and the team. The matrix, based on the military debriefing work of Entin et al,34–36 captured time-based elements and information participants were considering to assess their decision making and actions.23 While we evaluated medical technical skills (eg, successful ventilation), we were most interested in the performance of CRM skills (eg, calling for help, announcing the diagnosis, asking the team for suggestions; table 2). A rating criterion for video analysis assessed the communication of critical information or actions categorized as “information” requests or transfers and “action” requests or transfers (box 2). All requests and transfers were tracked and summed for each 1-minute interval for the 10-minute time periods in the preintervention and postintervention assessments. Video analysis was performed by the principal author and cross-checked by 2 other examiners familiar with the simulation scenarios. Questionable ratings were marked and reviewed by the 3 examiners before final scoring. There were 2 questionable ratings for 52 reviews, and both were resolved easily.
TABLE 2.
Critical Crisis Resource Management Actions Results
Data were analyzed by using univariate and multivariate analysis of variance with repeated measures for pretest and posttest evaluations. Nominal data were analyzed by using Pearson χ2 and Fisher exact tests. Statistical analyses were performed with SPSS version 20 (IBM Corp) with P < .05 considered statistically significant.
Results
Preintervention
Three groups of PGY-3 residents (19 in 2006, 19 in 2007, and 18 in 2008) were enrolled for a total of 56. Four participants (2 each in 2006 and 2007) were unavailable for the intervention, leaving 52 participants. The participants in each group were similar with respect to training level, age, and experience. All 52 attempted ventilation and 92% (48 of 52) did call for help. Seventy-eight percent (41 of 52) failed to successfully ventilate the patient, and all continued to attempt ventilation without asking for assistance from the arriving anesthesiologists. In all cases of failed ventilation, the simulated patient died (table 2). Debriefing revealed that the participants recognized their inability to manage available resources. Sixty-four percent (27 of 41) of those who could not ventilate the patient were aware of their ineffective ventilation, and none requested help.
Postsimulation-Based Education With Deliberate Practice Intervention Results (SIM)
All participants recognized distress, called for help, and attempted to ventilate the simulated patient; however, 73% (19 of 26) failed in the latter task. All SIM participants, including those who could ventilate, assigned ventilation to an anesthesiologist in the response team. All announced the patient's vital signs and presumptive diagnosis aloud, and 77% (20 of 26) asked the team for suggestions (table 2). The communication matrix revealed that these participants continued transfers of information and action requests with few gaps in communication.
Postlecture Intervention Results (LEC)
All participants recognized distress; 96% (25 of 26) did call for help. Sixty-one percent (16 of 26) of participants failed to successfully ventilate, and 73% (19 of 26) continued to attempt ventilation regardless of difficulty. All participants who could not ventilate the patient were aware of their inadequate ventilation. Seventy-three percent (19 of 26) of participants continued direct patient care while attempting to manage the team (table 2). Debriefing revealed that participants did not feel capable of managing resources effectively.
Communication Between Leader and Team
The communication matrix variables reflect the effectiveness of information exchange between the participants and team. These variables were measured across preintervention and postintervention periods between the SIM and LEC groups, and were quantified by summation of requests and transfers of information. All measures were significantly increased for each group during postintervention testing. The SIM participants demonstrated significantly higher (P < .001) communication skills, quantified as successful information and action transfers, than the LEC participants.
Debriefing Sessions
During the postscenario debriefing, participants reported difficulty in assessing the patient, communicating with the team, and prioritizing treatment steps. All participants said they behaved as if they were taking care of real patients and characterized the scenarios as realistic. The SIM participants reported that the opportunity to practice and debrief scenarios helped them learn to identify and treat the problem and manage the team. The SIM and LEC groups differed in their response to questions about performance, with a much higher percentage of the SIM group indicating comfort with CRM practices (eg, asking the team for help, asking for suggestions, assigning tasks to the team), comfort with managing the simulated emergency, and ability to manage the team. A higher percentage of SIM group participants also reported they incorporated lessons from the educational sessions, and the sessions made them more confident with real patients.
Discussion
Our study showed that simulation-based education with deliberate practice of CRM skills resulted in improved rare event and team management by senior internal medicine resident code leaders. While lecture format yielded some improvement in team and event management, the improvement was significantly greater for members of the simulation training group, especially for communication results. During debriefing sessions, participants disclosed difficulties they encountered while attempting to manage the event and team. While the LEC group demonstrated improved management, they reported that they did not feel comfortable asking the team for suggestions. In contrast, SIM participants reported that these sessions taught them to ask the team for help, resulting in greater comfort in both simulated and real code events.
Several studies suggest training deficits for residents functioning as leaders of code teams. Despite reporting that ACLS algorithm training seemed sufficient, many felt leadership training was insufficient.15,16,37–40 Significant numbers of residents reported feeling unprepared for (78%), overwhelmed by (73%), and incompetent at (22%) managing cardiac arrests.41 In the current study, the SIM participants reported increased comfort in managing real patient codes compared to the LEC group.
Simulation-based education with deliberate practice has been used to successfully teach procedural skills and adherence to algorithm steps.25,26,32 While several studies identified that team behaviors correlate with timing and quality of cardiopulmonary resuscitation,32,42 few studies have addressed leadership education and CRM skills.43–47 A retrospective analysis of simulated scenarios found that residents who demonstrated good or subpar performance in 1 domain (technical or nontechnical skills) showed performance at a similar level on the other domain.48 Yee et al49 demonstrated that residents exposed to simulated CRM training demonstrated improved nontechnical skills in a repeated simulated arrest. While this study offered an additional simulation session, it did not allow participants to review and deliberately practice poorly performed skills.49
Few educational programs or guidelines exist for teaching residents to become code leaders, and we sought to identify a successful approach to teach the nontechnical elements of resuscitation team management. While there was some improvement in the residents' scores after a lecture program in leadership skills, the improvement in the group exposed to simulation-based education was significantly greater.
Limitations of our study include the small number of participants and that the study was conducted at a single institution. The SIM group members may have become more familiar with the simulated environment during their education sessions. Another limitation is that while a growing body of work supports the use of simulation, we cannot predict whether participants' actions would be similar during a real patient emergency, nor can we infer the effect on patient outcomes as a result of suboptimal performance in code events.
Neither group in our study demonstrated improved ventilation skills. We did not teach airway management or ventilation in this study, but advised participants to identify technical skills they did not perform well, and assign those tasks to the appropriate professional. We stressed that code leaders should not perform patient care while leading the team. The SIM group assigned patient care and led the team with greater success, and reported comfort with asking the team for help, while the LEC group reported they remained uncomfortable assigning tasks to other members of the team.
Conclusion
We demonstrated that simulation with deliberate practice to teach senior resident code leaders CRM skills improved performance in communication and leadership skills. Residents exposed to simulation communicated and completed CRM skills more effectively than those taught in a lecture format.
Footnotes
Amanda R. Burden, MD, is Associate Professor of Anesthesiology, Director Simulation Program, Cooper Medical School of Rowan University, Department of Anesthesiology, Cooper University Hospital; Erin W. Pukenas, MD, is Assistant Professor of Anesthesiology, Cooper Medical School of Rowan University, Department of Anesthesiology, Cooper University Hospital; Edward R. Deal, DO, is Assistant Professor of Anesthesiology, Cooper Medical School of Rowan University, Department of Anesthesiology, Cooper University Hospital; Douglas B. Coursin, MD, is Professor of Anesthesiology and Internal Medicine, University of Wisconsin School of Medicine and Public Health; Gregory M. Dodson, DO, is Attending Anesthesiologist, Department of Anesthesiology, Cooper University Hospital; Gregory W. Staman, RN, is Director of Simulation Operations, Cooper Medical School of Rowan University and Cooper University Hospital; Irwin Gratz, DO, is Professor of Anesthesiology, Cooper Medical School of Rowan University, Department of Anesthesiology, Cooper University Hospital; and Marc C. Torjman, PhD, is Professor of Anesthesiology and Biomedical Sciences, Cooper Medical School of Rowan University, Department of Anesthesiology, Cooper University Hospital.
Funding: The authors report no external funding source for this study.
Conflict of Interest: The authors declare they have no competing interests.
The authors would like to thank Michael E. Goldberg, MD, Professor and Chairman, Department of Anesthesiology, Associate Dean for Medical Education, Cooper Medical School of Rowan University and Cooper University Hospital, for his contribution and support.
References
- 1.Eisenberg MS, Mengert TJ. Cardiac resuscitation. N Engl J Med. 2001;344(17):1304–1313. doi: 10.1056/NEJM200104263441707. [DOI] [PubMed] [Google Scholar]
- 2.Ali B, Zafari AM. Narrative review: cardiopulmonary resuscitation and emergency cardiovascular care: review of the current guidelines. Ann Intern Med. 2007;147(3):171–179. doi: 10.7326/0003-4819-147-3-200708070-00006. [DOI] [PubMed] [Google Scholar]
- 3.Gaba DM, Fish KJ, Howard SK. Crisis Management in Anesthesiology. Philadelphia, PA: Churchill Livingstone; 1994. pp. 5–47. [Google Scholar]
- 4.Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194. doi: 10.1097/00001888-200402000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Singh H, Thomas EJ, Petersen LA, Studdert DM. Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med. 2007;67(19):2030–2036. doi: 10.1001/archinte.167.19.2030. [DOI] [PubMed] [Google Scholar]
- 6.Larsen MP, Eisenberg MS, Cummins RO, Hallstrom AP. Predicting survival from out-of-hospital cardiac arrest: a graphic model. Ann Emerg Med. 1993;22(11):1652–1658. doi: 10.1016/s0196-0644(05)81302-2. [DOI] [PubMed] [Google Scholar]
- 7.Dane FC, Russell-Lindgren KS, Parish DC, Durham MD, Brown TD. In-hospital resuscitation: association between ACLS training and survival to discharge. Resuscitation. 2000;47(1):83–87. doi: 10.1016/s0300-9572(00)00210-0. [DOI] [PubMed] [Google Scholar]
- 8.Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295(1):50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 9.Gaba DM. Structural and organizational issues in patient safety: a comparison of health care to other high-hazard industries. Calif Manage Rev. 2001;43:83–102. [Google Scholar]
- 10.Gaba DM. The future vision of simulation in health care. Qual Saf Health Care. 2004;13(suppl 1):2–10. doi: 10.1136/qshc.2004.009878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper JB, Taqueti VR. A brief history of the development of mannequin simulators for clinical education and training. Qual Saf Health Care. 2004;13(suppl 1):11–18. doi: 10.1136/qshc.2004.009886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Issenberg SB, McGaghie WC, Hart IR, Mayer JW, Felner JM, Petrusa ER, et al. Simulation technology for health care professional skills training and assessment. JAMA. 1999;282(9):861–866. doi: 10.1001/jama.282.9.861. [DOI] [PubMed] [Google Scholar]
- 13.Dunn WF, editor. Simulators in Critical Care Education and Beyond. Des Plaines, IL: Society of Critical Care Medicine; 2004. pp. 1–6. [Google Scholar]
- 14.DeVita MA, Schaefer J, Lutz J, Dongilli T, Wang H. Improving medical crisis team performance. Crit Care Med. 2004;32(suppl 2):61–65. doi: 10.1097/01.ccm.0000110872.86812.1c. [DOI] [PubMed] [Google Scholar]
- 15.Stross JK. Maintaining competency in advanced cardiac life support skills. JAMA. 1983;249(24):3339–3341. [PubMed] [Google Scholar]
- 16.Brown TB, Dias JA, Saini D, Shah RC, Cofield SS, Terndrup TE, et al. Relationship between knowledge of cardiopulmonary resuscitation guidelines and performance. Resuscitation. 2006;69(2):253–261. doi: 10.1016/j.resuscitation.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 17.Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O'Hearn N, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293(3):305–310. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- 18.Howard SK, Gaba DM, Fish KJ, Yang G, Sarnquist FH. Anesthesia crisis resource management training: teaching anesthesiologists to handle critical incidents. Aviat Space Environ Med. 1992;63(9):763–770. [PubMed] [Google Scholar]
- 19.Bruppacher HR, Alam SK, LeBlanc VR, Latter D, Naik VN, Salvoldelli GL, et al. Simulation-based training improves physicians' performance in patient care in high-stakes clinical setting of cardiac surgery. Anesthesiology. 2010;112(4):985–992. doi: 10.1097/ALN.0b013e3181d3e31c. [DOI] [PubMed] [Google Scholar]
- 20.Tekian A, McGuire CH, McGaghie WC. Innovative Simulations for Assessing Professional Competence. Chicago, IL: University of Illinois at Chicago College of Medicine; 1999. pp. 7–22. [Google Scholar]
- 21.Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(suppl):70–81. doi: 10.1097/00001888-200410001-00022. [DOI] [PubMed] [Google Scholar]
- 22.Ericsson KA. Deliberate practice and acquisition of expert performance: a general overview. Acad Emerg Med. 2008;15(11):988–994. doi: 10.1111/j.1553-2712.2008.00227.x. [DOI] [PubMed] [Google Scholar]
- 23.Burden AR, Carr ZJ, Staman GW, Littman JJ, Torjman MC. Does every code need a “reader”: improvement of rare event management with a cognitive aid “reader” during a simulated emergency: a pilot study. Simul Healthc. 2012;7(1):1–9. doi: 10.1097/SIH.0b013e31822c0f20. [DOI] [PubMed] [Google Scholar]
- 24.Issenberg SB, McGaghie WC, Petrusa ER, Gordon DL, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- 25.Wayne DB, Didwania A, Feinglass J, Fudala MJ, Barsuk JH, McGaghie WC. Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: a case-control study. Chest. 2008;133(1):56–61. doi: 10.1378/chest.07-0131. [DOI] [PubMed] [Google Scholar]
- 26.Wayne DB, Butter J, Siddall VJ, Fudala MJ, Linquist LA, Feinglass J, et al. Simulation-based training of internal medicine residents in advanced cardiac life support protocols: a randomized trial. Teach Learn Med. 2005;17(3):210–216. doi: 10.1207/s15328015tlm1703_3. [DOI] [PubMed] [Google Scholar]
- 27.Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, et al. Proving the value of simulation in laparoscopic surgery. Ann Surg. 2004;240(3):518–525. doi: 10.1097/01.sla.0000136941.46529.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barsuk JH, McGaghie WC, Cohen ER, O'Leary KJ, Wayne DB. Simulation-based mastery learning reduces complications during central venous catheter insertions in a medical intensive care unit. Crit Care Med. 2009;32(10):2697–2701. [PubMed] [Google Scholar]
- 29.Gallagher AG, Cates CU. Virtual reality training for the operating room and cardiac catheterisation laboratory. Lancet. 2004;364(9444):1538–1540. doi: 10.1016/S0140-6736(04)17278-4. [DOI] [PubMed] [Google Scholar]
- 30.Andreatta PB, Woodrum DT, Birkmeyer JD, Yellamanchilli RK, Doherty GM, Gauger PG, et al. Laparoscopic skills are improved with LapMentor training: results of a randomized, double-blinded study. Ann Surg. 2006;243(6):854–863. doi: 10.1097/01.sla.0000219641.79092.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mayo PH, Hackney JE, Mueck JT, Ribaudo V, Schneider RF. Achieving house staff competence in emergency airway management: results of a teaching program using a computerized patient simulator. Crit Care Med. 2004;32(12):2422–2427. doi: 10.1097/01.ccm.0000147768.42813.a2. [DOI] [PubMed] [Google Scholar]
- 32.Wayne DB, Butter J, Siddall VJ, Fudala MJ, Wade LD, Feinglass J, et al. Mastery learning of advanced cardiac life support skills by internal medicine residents using simulation technology and deliberate practice. J Gen Intern Med. 2006;21(3):251–256. doi: 10.1111/j.1525-1497.2006.00341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stewart J, O'Halloran C, Harrigan P, Spencer JA, Barton JR, Singleton SJ. Identifying appropriate tasks for the preregistration year: modified Delphi technique. BMJ. 1999;319(7204):224–229. doi: 10.1136/bmj.319.7204.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Entin EE, Serfaty D. Adaptive team coordination. Hum Factors. 1999;41(2):312–325. [Google Scholar]
- 35.Entin EE. 1999. Optimized command and control architectures for improved process and performance. In: Proceedings: Command and Control Research and Technology Symposium: Department of Defense C41SR Cooperative Research Program. Washington, DC. [Google Scholar]
- 36.Entin EE, Serfaty D, Kerrigan C. 1998. Choice and performance under three command and control architectures. In: Proceedings: Command and Control Research and Technology Symbolist. Monterey, CA. [Google Scholar]
- 37.Joint Commission on Accreditation of Healthcare Organizations. Joint Commission International Center for Patient Safety. Communication: a critical component in delivering quality care. http://www.jointcommission.org/topics/patient_safety.aspx. Accessed March 10, 2013. [Google Scholar]
- 38.Holzman RS, Cooper JB, Gaba DM, Philip JH, Small SD, Feinstein D. Anesthesia crisis resource management: real-life simulation training in operating room crises. J Clin Anesth. 1995;7(8):675–687. doi: 10.1016/0952-8180(95)00146-8. [DOI] [PubMed] [Google Scholar]
- 39.Hayes CW, Rhee A, Detsky ME, Leblanc VR, Wax RS. Residents feel unprepared and unsupervised as leaders of cardiac arrest teams in teaching hospitals: a survey of internal medicine residents. Crit Care Med. 2007;35(7):1668–1672. doi: 10.1097/01.CCM.0000268059.42429.39. [DOI] [PubMed] [Google Scholar]
- 40.Healey A, Sherbino J, Fan J, Mensour M, Upadhye S, Wasi P. A low-fidelity simulation curriculum addresses needs identified by faculty and improves the comfort level of senior internal medicine resident physicians with in-hospital resuscitation. Crit Care Med. 2010;38(9):1899–1903. doi: 10.1097/CCM.0b013e3181eb3ca9. [DOI] [PubMed] [Google Scholar]
- 41.Morgan R, Westmoreland C. Survey of junior hospital doctors' attitudes to cardiopulmonary resuscitation. Postgrad Med J. 2002;78(921):413–415. doi: 10.1136/pmj.78.921.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jankouskas T, Bush MC, Murray B, Rudy S, Henry J, Dyer AM, et al. Crisis resource management: evaluating outcomes of a multidisciplinary team. Simul Healthc. 2007;2(2):96–101. doi: 10.1097/SIH.0b013e31805d8b0d. [DOI] [PubMed] [Google Scholar]
- 43.Thomas EJ, Sexton JB, Lasky RE, Helmreich RL, Crandell DS, Tyson J. Teamwork and quality during neonatal care in the delivery room. J Perinatol. 2006;26(3):163–169. doi: 10.1038/sj.jp.7211451. [DOI] [PubMed] [Google Scholar]
- 44.Thomas EJ, Taggart B, Crandell S, Lasky RE, Williams AL, Love LJ, et al. Teaching teamwork during the Neonatal Resuscitation Program: a randomized trial. J Perinatol. 2007;27(7):409–414. doi: 10.1038/sj.jp.7211771. [DOI] [PubMed] [Google Scholar]
- 45.Hunziker S, Tschan F, Semmer NK, Zobrist R, Spychiger M, Breuer M, et al. Hands-on time during cardiopulmonary resuscitation is affected by the process of teambuilding: a prospective randomised simulator-based trial. BMC Emerg Med. 2009;9:3. doi: 10.1186/1471-227X-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marsch SC, Müller C, Marquardt K, Conrad G, Tschan F, Hunziker PR. Human factors affect the quality of cardiopulmonary resuscitation in simulated cardiac arrests. Resuscitation. 2004;60(4):51–56. doi: 10.1016/j.resuscitation.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 47.Marsch SC, Tschan F, Semmer N, Spychiger M, Breuer M, Hunzkier PR. Performance of first responders in simulated cardiac arrests. Crit Care Med. 2005;33(5):963–967. doi: 10.1097/01.ccm.0000157750.43459.07. [DOI] [PubMed] [Google Scholar]
- 48.Riem N, Boet S, Bould MD, Tavares W, Naik VN. Do technical skills correlate with non-technical skills in crisis resource management: a simulation study. Br J Anaesth. 2012;109(5):723–728. doi: 10.1093/bja/aes256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yee B, Naik VN, Joo HS, Savoldelli GL, Chung DY, Houston PL, et al. Nontechnical skills in anesthesia crisis management with repeated exposure to simulation-based education. Anesthesiology. 2005;105(2):241–248. doi: 10.1097/00000542-200508000-00006. [DOI] [PubMed] [Google Scholar]