Abstract
Background
Many internal medicine programs have reorganized their resident continuity clinics to improve the ambulatory care experience for residents. The effect of this redesign on patient satisfaction is largely unknown.
Methods
Our multi-institutional, cross-sectional study included 569 internal medicine residents from 11 programs participating in the Educational Innovations Project Ambulatory Collaborative. An 11-item patient satisfaction survey from the Consumer Assessment of Healthcare Providers and Systems was used to assess patient satisfaction, comparing patient satisfaction in traditional models of weekly continuity clinic with 2 new clinic models. We then examined the relationship between patient satisfaction and other practice variables.
Results
Patient satisfaction responses related to resident listening and communication skills, knowledge of medical history, perception of adequate visit time, overall rating, and willingness to refer to family and friends were significantly better in the traditional and block continuity models than the combination model. Higher ambulatory workload was associated with reduced patient perception of respect shown by the physician. The percentage of diabetic patients with glycated hemoglobin < 8% was positively correlated with number of visits, knowledge of medical history, perception of respect, and higher scores for recommending the physician to others. The percentage of diabetic patients with low density lipoprotein < 100 mg/dL was positively correlated with the physician showing respect.
Conclusions
Patient satisfaction was similar in programs using block design and traditional models for continuity clinic, and both outperformed the combination model programs. There was a delicate balance between workload and patient perception of the physician showing respect. Care outcome measures for diabetic patients were associated with aspects of patient satisfaction.
What was known
Internal medicine programs reorganized their resident continuity clinics to improve residents' and patients' experience.
What is new
Patient satisfaction was significantly higher in traditional and block continuity models than a combination model with some weekly experiences and some ambulatory block rotations.
Limitations
Lack of randomization of clinics to the models; inability to control for some patient- and resident-related factors.
Bottom line
Two internal medicine resident continuity clinic models resulted in higher patient satisfaction, which also was associated with improved outcomes of care.
Introduction
Patients' satisfaction with their health care has been associated with increased adherence to medical regimens1,2 and improved clinical outcomes,3 and the Medicare program plans to link a portion of its value-based purchasing bonuses to patients' perceptions of quality of care.4 Factors that have been shown to affect patient satisfaction include patient age, functional status, and socioeconomic status.5 Other factors associated with higher patient satisfaction in ambulatory settings include improved provider-specific continuity,6,7 increased patient-perceived encounter time,8 use of health information technology,9 better patient-physician communication,5,10 and overall fulfillment of expectations.5,11,12 Single-site studies have found that a heavy inpatient workload is associated with decreased patient satisfaction in resident continuity clinics13 and that changes in residency practice continuity are associated with improved satisfaction and clinical outcomes.14,15
The continuity clinic experience differs significantly across internal medicine (IM) programs, and there have been multiple calls for reorganization of ambulatory training practices.16–18 A number of programs have developed block models seeking to separate inpatient from outpatient care during residency training.14,19,20 We compare patient satisfaction results of the traditional ambulatory model with 2 new clinic models within multiple residencies participating in the Accreditation Council for Graduate Medical Education's Educational Innovations Project (EIP)21 and discuss elements associated with higher patient satisfaction. We also examined the relationship between patient satisfaction and other practice variables, such as continuity, ambulatory workload, utilization, resident satisfaction, and quality of care across participating programs.
Methods
Study Population and Setting
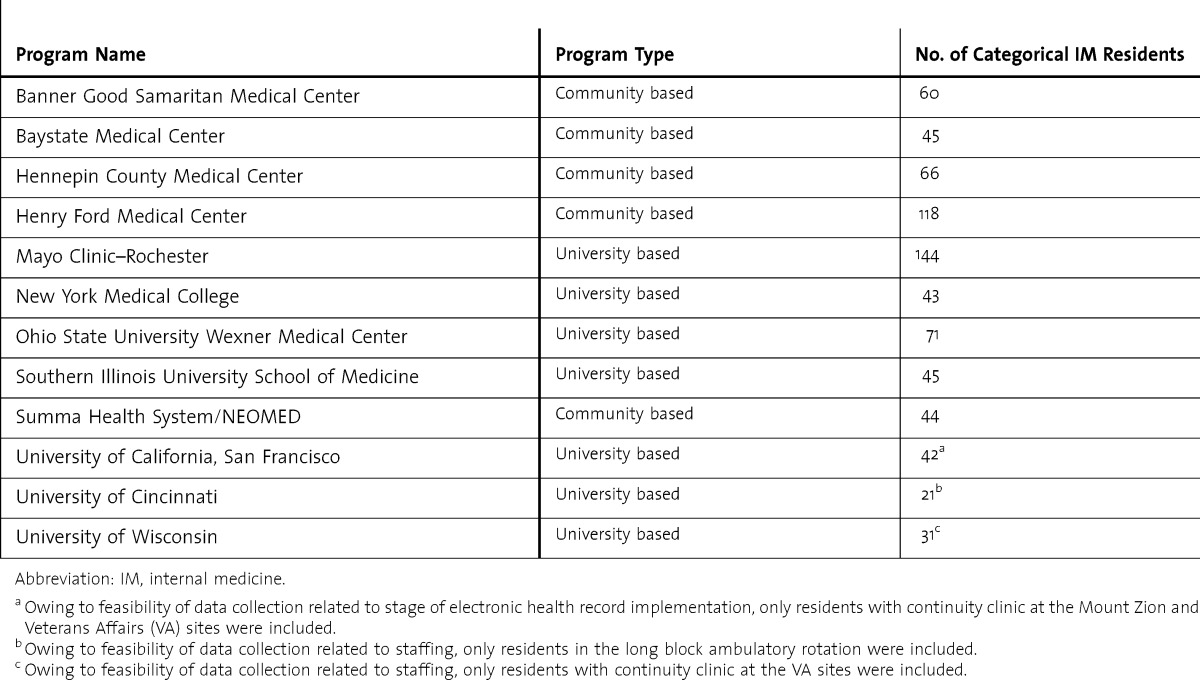
Twelve programs participated in the EIP Ambulatory Collaborative (EPAC; table 1)22; patient satisfaction data were available from 11 (the 12th program used a different survey for institution historical comparison). For the 11 programs, consent to participate was obtained from 97% (569 of 586) of residents. Texas Tech University Health Sciences Center El Paso provided oversight of the project.
TABLE 1.
Educational Innovations Project Ambulatory Collaborative Participating Programs
All participating sites received approval from their local Institutional Review Board.
Study Design
We used a multi-institutional, cross-sectional study design to assess the effect of clinic structure and key practice metrics on patient satisfaction in IM residency continuity clinics. Data collection occurred between September 1, 2010, and May 31, 2011, for visit and practice data. Patient satisfaction data were collected during the latter half of this period. One institution implemented a long block ambulatory experience that was off cycle from the academic year, and the study time frame at this institution was adjusted accordingly.
Measures
Patient Satisfaction
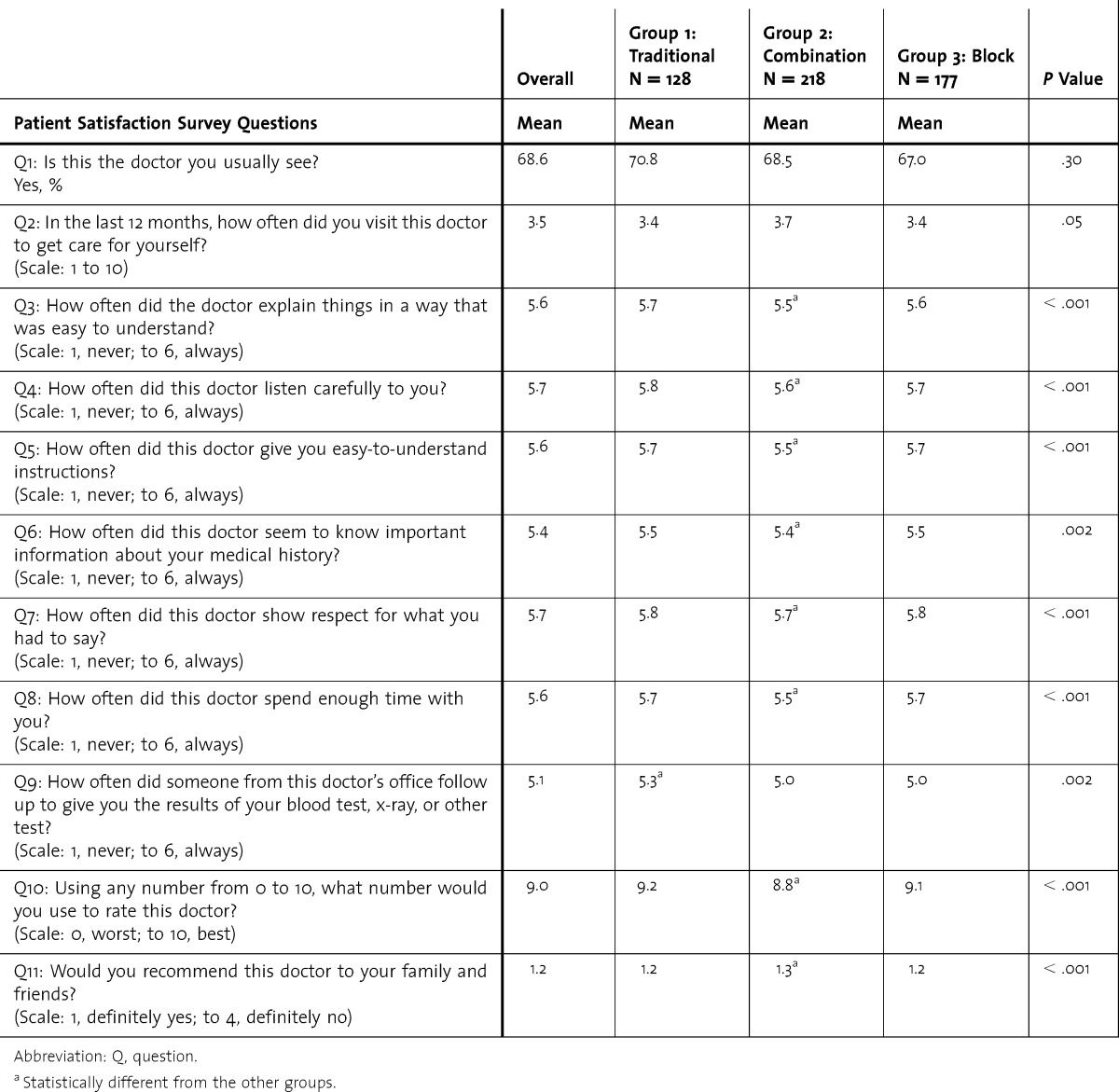
To assess patient satisfaction, we used an 11-question survey from the Consumer Assessment of Healthcare Providers and Systems.23 Surveys were collected at the time of patient visits, with only 1 survey completed by each patient for a given resident. Survey questions and corresponding scales are displayed in the first column of table 2.
TABLE 2.
Continuity Clinic Model and Patient Satisfaction
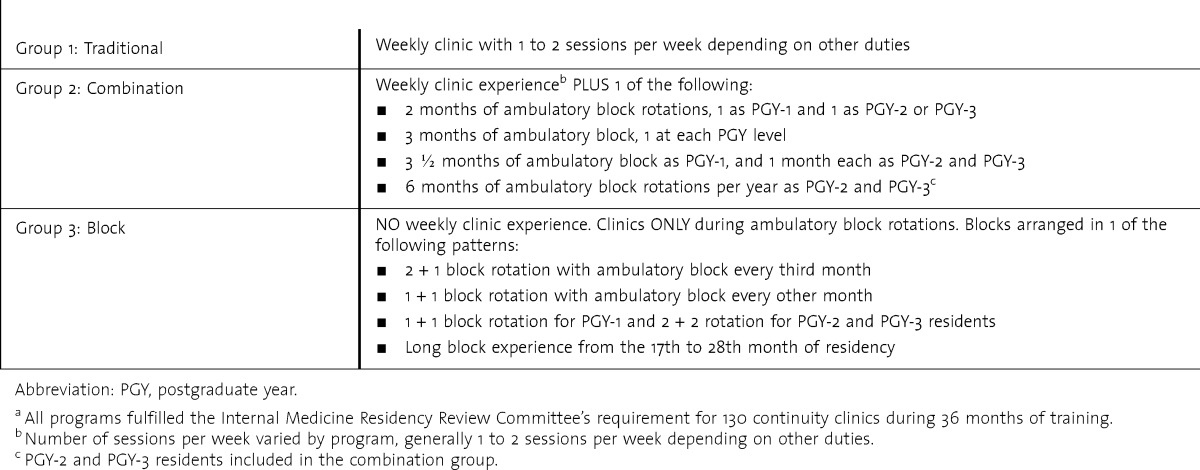
Clinic Model
Program leadership from each institution described their continuity clinic model as falling into 3 groups: (1) traditional weekly experience, (2) combination with some weekly experiences plus additional ambulatory block rotations, and (3) block structure with discrete inpatient and ambulatory rotations (table 3).22 We assessed associations between these models and patient satisfaction.
TABLE 3.
Description of Clinic Models Based on Curriculum Description Questionnaire22,a
Workload, Utilization, and Continuity
Ambulatory workload was defined by volume as the total number of patient visits seen by each resident during the study period divided by the number of clinics attended. Utilization was defined as the average number of visits by each patient during the study period. Continuity was measured by using the usual provider-of-care method (UPC),24,25 defined as percentage of visits in which patients were seen by their primary resident.
Quality Measures for Patients With Diabetes Mellitus
Three outcome and 2 process measures were reported for diabetic patients. Outcome measures were in keeping with standards of care at the time of data collection,26 and included percentage of patients with glycated hemoglobin (HbA1c) < 8%, percentage of patients with blood pressure < 130/80 mm Hg, and percentage of patients with low density lipoprotein (LDL) < 100 mg/dL. Process measures reported were percentage of patients with recorded measurement of HbA1c and LDL within the last 12 months.
Resident Satisfaction
Resident satisfaction was measured by using the Veterans Affairs Learners' Perception Survey,27 with additional questions related to conflict in duties across care settings.22
Statistical Analysis
Scores on the patient satisfaction survey were dependent variables. The percentage of “yes” responses to the first question was calculated for each resident. For the remainder of the questions, means were calculated. Independent variables included in the analysis were clinic model, postgraduate year (PGY) level, UPC, ambulatory workload, utilization, and resident satisfaction as well as quality measures for patients with diabetes mellitus described above. We compared the 3 clinic models by using analysis of covariance with a subsequent least significant difference test for those means found to be statistically significant. A P value of < .05 was considered statistically significant. The Tukey studentized range (HSD) test was used to assess significance among groups. The same analysis was conducted in the comparison of PGY levels. Pearson correlation coefficients were calculated to evaluate potential relationships between patient satisfaction and other independent variables using the calculated mean responses. We used SAS Version 9.3 (SAS Institute Inc) for statistical analysis. Missing values and responses marked “not applicable” were eliminated.
Results
Patient satisfaction data were available for 523 of 569 eligible residents (92%) with a median of 17 surveys completed per resident. Our primary analysis examined the relationship between clinic model and patient satisfaction. Data were available for 128 residents in group 1 (traditional model), 218 residents in group 2 (combination model), and 177 residents in group 3 (block model). Results comparing the models, along with overall mean values, are displayed in table 2. The percentage of patients seeing their usual physician and the number of visits reported in the last 12 months did not differ across groups. The responses related to how well the physician provided explanations, listened carefully, gave easy-to-understand instructions, seemed to know important medical information, showed respect, and spent enough time were significantly better in the traditional and block model programs than the combination model programs. However, there were no significant differences between traditional and block models. The overall rating of the physician and willingness to refer to family and friends were also significantly better in the traditional and block models than the combination model, but again there was no significant difference between traditional and block models. Patients rated follow-up of test results better in traditional programs than the other groups. Differences in patient satisfaction found between clinic models remained statistically significant after controlling for utilization.
Patients completing the survey for PGY-1 residents, compared to PGY-2 and PGY-3 residents, were less likely to report that this physician was their usual physician (P = .004). Number of visits with this physician reported in the last 12 months was significantly higher for PGY-3 than for PGY-1 and PGY-2 residents (P = .009). The PGY-3 residents received significantly higher ratings for listening carefully and giving easy-to-understand instructions than PGY-2 residents (P = .03 and .005, respectfully), as well as for knowing important historical information compared to the other groups (P = .003). When asked if the patient would recommend this physician, PGY-3 residents received better ratings than PGY-2 residents, but neither was statistically different from PGY-1 residents (P = .01).
In the secondary analysis, we found utilization positively correlated with all questions on the patient satisfaction survey (table 4), including a higher overall rating of the physician and a higher likelihood of referral to family and friends. Higher ambulatory workload was associated with increased likelihood that patients saw their usual physician, but also reduced the perception of respect shown by the physician (table 4). The UPC, representing continuity of care for each resident's panel of patients, was not related to overall physician rating or likelihood to recommend the physician when controlled for utilization (data not shown). However, patients who answered “yes” to the question, “Is this the doctor you usually see?” rated the physician more favorably on the 10-point scale (P = .004). Resident satisfaction was not significantly related to patient satisfaction (data not shown).
TABLE 4.
Correlation Between Utilization, Workload, Patient Outcome Measures, and Patient Satisfaction
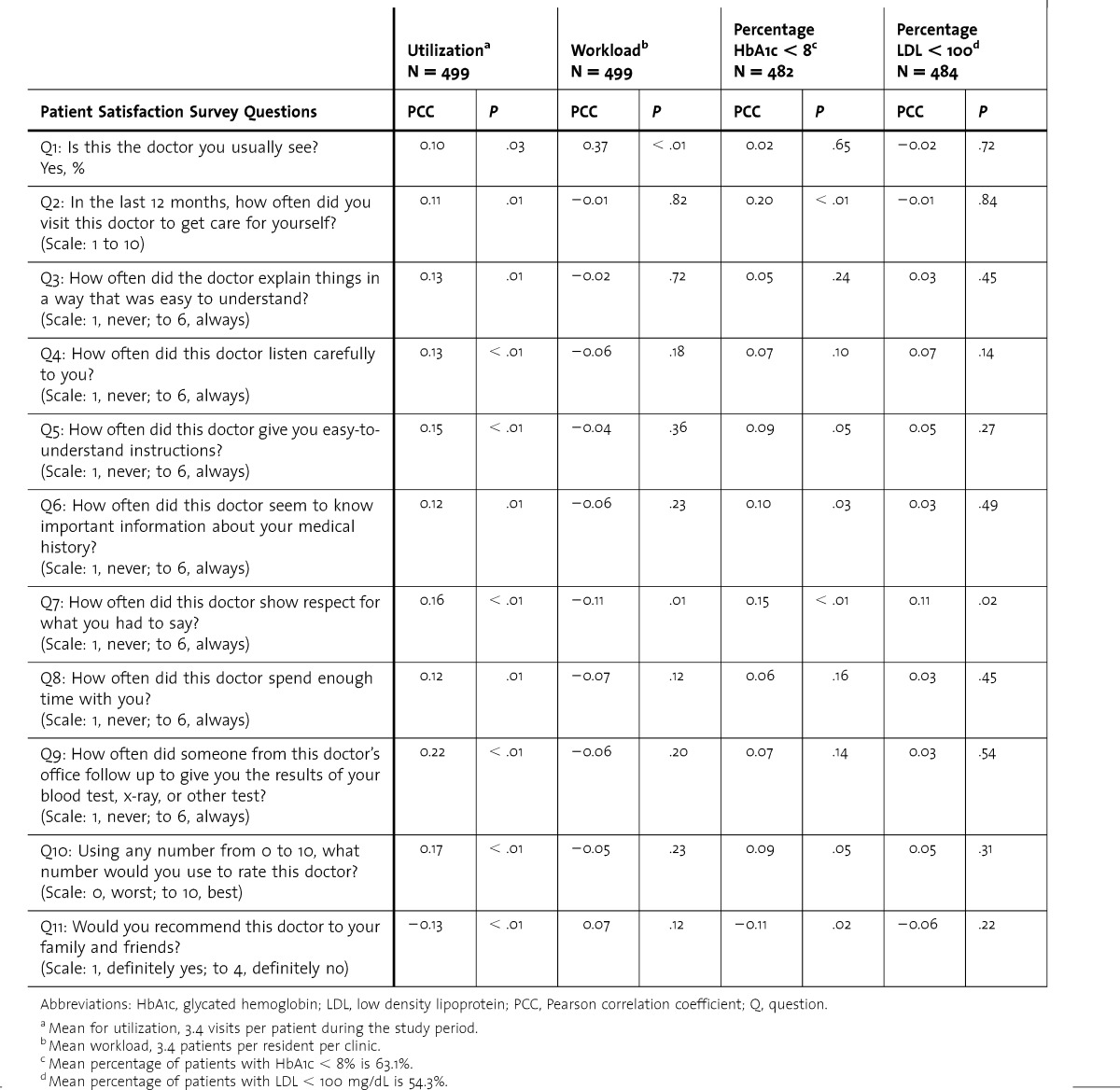
Quality measures for empanelled patients with diabetes were evaluated in relation to patient satisfaction. Measurements of HbA1c and LDL within the last 12 months were positively associated with patients reporting seeing their usual physician and the number of visits that patients reported with their physician in the prior 12 months (P < .01). These process measures were not significantly associated with any of the other questions on the patient satisfaction survey. The outcome measures evaluated were percentage of patients with HbA1c < 8%, percentage of patients with an LDL < 100 mg/dL, and blood pressure < 130/80 mm Hg. The percentage of patients with HbA1c < 8% was positively correlated with the number of visits reported by patients in the last 12 months, the physician knowing your medical history, the physician showing respect, as well as better scores for recommending the physician to family and friends (table 4). The percentage of patients with an LDL < 100 mg/dL was positively correlated with the physician showing respect (table 4). The percentage of patients with blood pressure < 130/80 mm Hg was not significantly associated with any of the items on the patient satisfaction survey (data not shown).
Discussion
To our knowledge, this is the first multi-institutional report describing associations between IM resident clinic structure and patient satisfaction. Combined with results from a companion study,22 resident and patient satisfaction are comparable in programs using the block model design and the traditional structure, allaying initial fears that block model designs would reduce satisfaction. However, patient satisfaction was found to be lower in programs that attempted to combine features of a weekly clinic with more intensive ambulatory rotations. The reasons for this are unclear, especially since the number of patients who reported seeing their usual physician was similar across all groups.
There are many factors that potentially affect patient satisfaction in addition to clinic model. Level of training was associated with some differences in patient satisfaction. The PGY-3 residents have likely followed up their patients for a longer period of time and therefore received higher ratings on knowing important historical information. The PGY-1 residents are new to the system so it is not surprising that their patients were less likely to report seeing their usual physician. Patients were less satisfied with residents in PGY-2 than PGY-3. This is based on lower ratings for PGY-2 residents on listening carefully, giving easy-to-understand instructions, and willingness to refer to family and friends. This may be explained by a typical shift toward busier sessions with less supervision during PGY-2.
Our data also suggest that increased use of the system and patient satisfaction are tightly linked. However, we cannot differentiate whether utilization is driving satisfaction or vice versa. Familiarity and knowledge of the system may affect patient expectations. It is also possible that additional visits help patients build a healing relationship with their resident physician.
Prior reports in the literature have found a correlation between continuity and patient satisfaction.6,7 We did not find this in our study using UPC as the measure of continuity. However, patient-perceived continuity as reflected in the question, “Is this the doctor you usually see?” was associated with a more favorable rating of the physician in keeping with prior reports. We recognize that newer models of care create continuity at levels beyond the primary provider, such as team-based care in a patient-centered medical home.28 Level of training was associated with differences in patient satisfaction, with lower scores for PGY-2 residents. This and other findings suggest there is a delicate balance between workload and patient satisfaction, and workload in resident continuity clinics requires balancing. Higher workload creates more access but appears to result in lower ratings on respect for patients. Residents may benefit from additional training in teamwork as well as effective, respectful communication focusing on areas such as agenda setting for time-pressured situations. This is an important skill in this era of high-volume practices and underscores the need for teamwork to balance access and workload.
In keeping with prior literature,3 better patient outcomes were associated with aspects of patient satisfaction in our study. In particular, HbA1c < 8% and LDL < 100 mg/dL were both positively correlated with the physician showing respect. Contact with the physician, as reflected in number of visits in the last 12 months, was also associated with higher percentage of patients with HbA1c < 8% as well as with higher percentages on process measures, such as measurement of HbA1c and LDL. Improving outcomes is complex, but respect for the patient as a partner in their care and appropriate access are basic tenets of the chronic care model29 and the patient-centered medical home.30
Limitations of our study include a lack of randomization; individual programs chose the structure and scheduling of their resident clinics. There are inherent variations within the general categories that we called block and combination models.22 Inpatient workload, which can distract residents from clinic duties,31 was not measured. Ambulatory workload was not adjusted for case mix or severity of illness, and we were not able to control for differences in patient factors, such as age and socioeconomic status,5 or physician factors, such as language concordance,32 which may affect patient satisfaction. Finally, in the ambulatory environment, there are many challenges that could not be controlled that may affect the patient's experience, such as institutional culture, level of staffing, staff training, clinic procedures, and stage of implementation of electronic health records.
Conclusion
Patient satisfaction is similar between block clinic designs and traditional models, and both had better patient satisfaction than combination model programs. The reasons for lower satisfaction in combination model programs are not well understood. Quality measures in diabetic patients, including outcome measures such as HbA1c < 8% and LDL < 100 mg/dL, appear to relate to aspects of patient satisfaction in IM resident continuity clinics. Future research is needed to explore the reasons for lower satisfaction in the combination model, and to look at the alignment of the patient experience and educational design with population health and value. Exploration of patient satisfaction with team continuity also merits future study.
Supplementary Material
Footnotes
Maureen D. Francis, MD, FACP, is College Master and Associate Professor, Medical Education, Texas Tech University Health Sciences Center at El Paso; Eric Warm, MD, FACP, is Professor of Medicine and Program Director, Internal Medicine Residency, University of Cincinnati Academic Health Center; Katherine A. Julian, MD, is Professor of Clinical Medicine and Track Director, UC Primary Care General Internal Medicine Residency Program, University of California, San Francisco; Michael Rosenblum, MD, FACP, is Director, Baystate Internal Medicine Residency Programs, and Assistant Clinical Professor, Tufts University School of Medicine; Kris Thomas, MD, is Associate Professor of Medicine, Consultant, Division of Primary Care Internal Medicine, and Associate Program Director, Internal Medicine Residency, Mayo Clinic; Sean Drake, MD, FACP, is Program Director, Internal Medicine Residency, Henry Ford Hospital, and Clinical Assistant Professor, Wayne State University; Keri Lyn Gwisdalla, MD, is Associate Program Director, Internal Medicine Residency, Banner Good Samaritan Medical Center/Phoenix VAHCS, and Assistant Professor of Clinical Medicine, University of Arizona College of Medicine-Phoenix; Michael Langan, MD, FACP, is Assistant Professor and Associate Program Director, Internal Medicine Residency, The Ohio State University Wexner Medical Center; Christopher Nabors, MD, is Assistant Professor and Associate Program Director, Internal Medicine Residency, New York Medical College at Westchester Medical Center; Anne Pereira, MD, MPH, FACP, is Program Director, Internal Medicine Residency, and Assistant Chief of Medicine for Faculty Development and Education, Hennepin County Medical Center, and Associate Professor of Medicine, University of Minnesota; Amy Smith, MS, is Instructor, School of Medicine and Public Health, University of Wisconsin-Madison; David Sweet, MD, FACP, is Program Director, Internal Medicine Residency, Summa Health System, and Professor, Internal Medicine, Northeast Ohio Medical University; Andrew Varney, MD, is Professor of Clinical Medicine and Program Director, Internal Medicine Residency, Southern Illinois University School of Medicine; and Mark L. Francis, MD, MS, is Professor, Medical Education, Texas Tech University Health Sciences Center at El Paso.
Funding: The authors report no external funding source for this study.
Conflict of Interest: The authors declare they have no competing interests.
The authors would like to thank the following for their contributions to the design of the study and data management at the participating institutions: Jayne Peterson, MD, Banner Good Samaritan Medical Center; Reva Kleppel, MSW, MPH, Baystate Medical Center; Mark Wieland, MD, Mayo Clinic–Rochester; David Wininger, MD, The Ohio State University Wexner Medical Center; Lynn Clough, PhD, Summa Health System/NEOMED; Rebecca Shunk, MD, Maya Dulay, MD, and Pat O'Sullivan, PhD, University of California, San Francisco; Bennett Vogelman, MD, and Robert Holland, MD, University of Wisconsin. We would also like to thank Melchor Ortiz, PhD, Texas Tech University Health Sciences Center El Paso, for his assistance in the initial management of the data. Lastly, we extend our gratitude to the Alliance for Academic Internal Medicine for providing administrative support for the project and meeting space for the EIP Ambulatory Collaborative.
References
- 1.Hulka BS, Cassel JC, Kupper LL, Burdette JA. Communication, compliance, and concordance between physicians and patients with prescribed medications. Am J Public Health. 1976;66(9):847–853. doi: 10.2105/ajph.66.9.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Uhlmann RF, Inui TS, Carter WB. Patient requests and expectations: definitions and clinical applications. Med Care. 1984;22(7):681–685. doi: 10.1097/00005650-198407000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Alazri MH, Neal RD. The association between satisfaction with services provided in primary care and outcomes in type 2 diabetes mellitus. Diabet Med. 2003;20(6):486–490. doi: 10.1046/j.1464-5491.2003.00957.x. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare & Medicaid Services. Hospital value-based purchasing. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/hospital-value-based-purchasing/index.html?redirect=/hospital-value-based-purchasing. Accessed June 10, 2013. [Google Scholar]
- 5.Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52(4):609–620. doi: 10.1016/s0277-9536(00)00164-7. [DOI] [PubMed] [Google Scholar]
- 6.Fan VS, Burman M, McDonell MB, Fihn SD. Continuity of care and other determinants of patient satisfaction with primary care. J Gen Intern Med. 2005;20(3):226–233. doi: 10.1111/j.1525-1497.2005.40135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nutting PA, Goodwin MA, Flocke SA, Zyzanski SJ, Stange KC. Continuity of primary care: to whom does it matter and when. Ann Fam Med. 2003;1(3):149–155. doi: 10.1370/afm.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin CT, Albertson GA, Schilling LM, Cyran EM, Anderson SN, Ware L, et al. Is patients' perception of time spent with the physician a determinant of ambulatory patient satisfaction. Arch Intern Med. 2001;161(11):1437–1442. doi: 10.1001/archinte.161.11.1437. [DOI] [PubMed] [Google Scholar]
- 9.Rozenblum R, Donze J, Hockey PM, Guzdar E, Labuzetta MA, Zimlichman E, et al. The impact of medical informatics on patient satisfaction: a USA-based literature review. Int J Med Inform. 2013;82(3):141–158. doi: 10.1016/j.ijmedinf.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 10.Smith RC, Lyles JS, Mettler JA, Marshall AA, Van Egeren LF, Stoffelmayr BE, et al. A strategy for improving patient satisfaction by the intensive training of residents in psychosocial medicine: a controlled, randomized study. Acad Med. 1995;70(8):729–732. doi: 10.1097/00001888-199508000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Lewis CL, Wickstrom GC, Kolar MM, Keyserling TC, Bognar BA, Dupre CT, et al. Patient preferences for care by general internists and specialists in the ambulatory setting. J Gen Intern Med. 2000;15(2):75–83. doi: 10.1046/j.1525-1497.2000.05089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kravitz RL, Cope DW, Bhrany V, Leake B. Internal medicine patients' expectations for care during office visits. J Gen Intern Med. 1994;9(2):75–81. doi: 10.1007/BF02600205. [DOI] [PubMed] [Google Scholar]
- 13.Feddock CA, Hoellein AR, Griffith CH, Wilson JF, Becker NS, Bowerman JL, et al. Are continuity clinic patients less satisfied when residents have a heavy inpatient workload. Eval Health Prof. 2005;28(4):390–399. doi: 10.1177/0163278705281070. [DOI] [PubMed] [Google Scholar]
- 14.Warm EJ, Schauer DP, Diers T, Mathis BR, Neirouz Y, Boex JR, et al. The ambulatory long-block: an accreditation council for graduate medical education (ACGME) educational innovations project (EIP) J Gen Intern Med. 2008;23(7):921–926. doi: 10.1007/s11606-008-0588-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dearinger AT, Wilson JF, Griffith CH, Scutchfield FD. The effect of physician continuity on diabetic outcomes in a resident continuity clinic. J Gen Intern Med. 2008;23(7):937–941. doi: 10.1007/s11606-008-0654-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nadkarni M, Reddy S, Bates CK, Fosburgh B, Babbott S, Holmboe E. Ambulatory-based education in internal medicine: current organization and implications for transformation: results of a national survey of resident continuity clinic directors. J Gen Intern Med. 2011;26(1):16–20. doi: 10.1007/s11606-010-1437-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fitzgibbons JP, Bordley DR, Berkowitz LR, Miller BW, Henderson MC. Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine. Ann Intern Med. 2006;144(12):920–926. doi: 10.7326/0003-4819-144-12-200606200-00010. [DOI] [PubMed] [Google Scholar]
- 18.Stevens DP, Wagner EH. Transform residency training in chronic illness care—now. Acad Med. 2006;81(8):685–687. doi: 10.1097/00001888-200608000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Wieland ML, Halvorsen AJ, Chaudhry R, Reed DA, McDonald FS, Thomas KG. An evaluation of internal medicine residency continuity clinic redesign to a 50/50 outpatient-inpatient model. Gen Intern Med. 2013;28(8):1014–1019. doi: 10.1007/s11606-012-2312-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaudhry SI, Balwan S, Friedman KA, Sunday S, Chaudhry B, Dimisa D, et al. Moving forward in GME reform: a 4 + 1 model of resident ambulatory training. Gen Intern Med. 2013;28(8):1100–1104. doi: 10.1007/s11606-013-2387-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mladenovic J, Bush R, Frohna J. Internal medicine's Educational Innovations Project: improving health care and learning. Am J Med. 2009;122(4):398–404. doi: 10.1016/j.amjmed.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 22.Francis MD, Thomas K, Langan M, Smith A, Drake S, Gwisdalla KL, et al. Clinic design, key practice metrics, and resident satisfaction in internal medicine continuity clinics: findings of the Educational Innovations Project Ambulatory Collaborative. J Grad Med Educ. 2014;6(2):249–255. doi: 10.4300/JGME-D-13-00159.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.CAHPS Clinician & Group Surveys: Version: Adult Primary Care Questionnaire 1.0. https://cahps.ahrq.gov/surveys-guidance/docs/351a6-AdultPrim-Eng-6pt-V1.pdf. Accessed October 28, 2013. [Google Scholar]
- 24.Breslau N, Reeb KG. Continuity of care in a university-based practice. J Med Educ. 1975;50(10):965–969. doi: 10.1097/00001888-197510000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Steinwachs DM. Measuring provider continuity in ambulatory care: an assessment of alternative approaches. Med Care. 1979;17(6):551–565. doi: 10.1097/00005650-197906000-00001. [DOI] [PubMed] [Google Scholar]
- 26.NCQA. HEDIS 2009 Volume 2 Technical Update. http://www.ncqa.org/portals/0/PolicyUpdates/HEDIS%20Technical%20Updates/09_CDC_Spec.pdf. Accessed October 28, 2013. [Google Scholar]
- 27.Keitz SA, Holland GJ, Melander EH, Bosworth HB, Pincus SH. The Veterans Affairs Learners' Perceptions Survey: the foundation for educational quality improvement. Acad Med. 2003;78(9):910–917. doi: 10.1097/00001888-200309000-00016. [DOI] [PubMed] [Google Scholar]
- 28.Hochman ME, Asch S, Jibilian A, Chaudry B, Ben-Ari R, Hsieh E, et al. Patient-centered medical home intervention at an internal medicine resident safety-net clinic. JAMA Intern Med. 2013;173(18):1694–1701. doi: 10.1001/jamainternmed.2013.9241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness. Eff Clin Pract. 1998;1(1):2–4. [PubMed] [Google Scholar]
- 30.Rosenthal TC. The medical home: growing evidence to support a new approach to primary care. J Am Board Fam Med. 2008;21(5):427–440. doi: 10.3122/jabfm.2008.05.070287. [DOI] [PubMed] [Google Scholar]
- 31.Salerno SM, Faestel PM, Mulligan T, Rosenblum MJ. Disruptions and satisfaction in internal medicine resident continuity clinic differ between inpatient and outpatient rotations. Teach Learn Med. 2007;19(1):30–34. doi: 10.1080/10401330709336620. [DOI] [PubMed] [Google Scholar]
- 32.Gonzalez HM, Vega WA, Tarraf W. Health care quality perceptions among foreign-born Latinos and the importance of speaking the same language. J Am Board Fam Med. 2010;23(6):745–752. doi: 10.3122/jabfm.2010.06.090264. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


