Abstract
Background
Several national initiatives aim to teach high-value care to residents. While there is a growing body of literature on cost impact of physicians' therapeutic decisions, few studies have assessed factors that influence residents' prescribing practices.
Objective
We studied factors associated with intensive health care utilization among internal medicine residents, using brand name statin prescribing as a proxy for higher-cost care.
Methods
We conducted a retrospective, cross-sectional analysis of statin prescriptions by residents at an urban academic internal medicine program, using electronic health record data between July 1, 2010, and June 30, 2011.
Results
For 319 encounters by 90 residents, patients were given a brand name statin in 50% of cases. When categorized into quintiles, the bottom quintile of residents prescribed brand name statins in 2% of encounters, while the top quintile prescribed brand name statins in 98% of encounters. After adjusting for potential confounders, including patient characteristics and supervising attending, being in the primary care track was associated with lower odds (odds ratio [OR], 0.38; P = .02; 95% confidence interval [CI], 0.16–0.86), and graduating from a medical school with an above-average hospital care intensity index was associated with higher odds of prescribing brand name statins (OR, 1.70; P = .049; 95% CI, 1.003–2.88).
Conclusions
We found considerable variation in brand name statin prescribing by residents. Medical school attended and residency program type were associated with resident prescribing behavior. Future interventions should raise awareness of these patterns in an effort to teach high-value, cost-conscious care to all residents.
What was known
There are calls to enhance residents' awareness of the cost implications of their therapeutic decisions.
What is new
A study assessed factors at the resident and encounter level that resulted in residents prescribing generic rather than brand name statins for lipid-lowering therapy.
Limitations
Small sample, single institution study, and cross-sectional design reduce the ability to generalize.
Bottom line
Medical school graduation origin and being in the primary care versus categorical track had an impact on statin-prescribing practices.
Introduction
Health care costs in the United States were $2.6 trillion in 2010 and are predicted to rise to $4.6 trillion by 2020.1 As a result, there have been calls to incorporate cost awareness into graduate medical education.2,3 Past efforts to teach residents about costs focused mainly on the inpatient setting,4 and we know relatively little about factors driving resource utilization in residency.5,6 The limited information available about the drivers of resident ordering behavior may be 1 reason why educational interventions to improve cost-effective care among residents have not been successful.7,8
To better understand physician resource utilization patterns as they develop during medical training, we decided to focus on 1 of the “Top 5” practices that may be overused in internal medicine. The Top 5 list for internal medicine was developed in 2011 by the National Physician Alliance.9 This initiative later morphed into the American Board of Internal Medicine's Choosing Wisely campaign.10 The Top 5 list for internists included a recommendation to use generic statins rather than brand name statins when initiating lipid-lowering therapy.11,12 In 2009, brand name statin prescribing was estimated to account for $5.8 billion in annual costs.13
This study was designed to address 2 questions: (1) Was there variation in brand name versus generic statin prescribing when initiating cholesterol-lowering therapy by residents in an urban academic medical center? and (2) What resident characteristics were associated with higher rates of brand name statin prescribing?
Methods
We performed a retrospective, cross-sectional analysis of statin prescribing by internal medicine residents at Weill Cornell Internal Medicine Associates—the resident and attending practice of the New York Presbyterian/Weill Cornell internal medicine residency program. We obtained data from the practice's electronic health record for all patient encounters between July 1, 2010, and June 30, 2011 (including office visits, telephone encounters, and order-only encounters), where a statin was prescribed for a patient not previously receiving statin therapy. We selected this time interval because it predated generic availability of atorvastatin; therefore, all prescriptions for atorvastatin and rosuvastatin were for brand name Lipitor and Crestor, respectively. The study period also predated the US Food and Drug Administration's announcement about increased risk of muscle injury with high-dose simvastatin in June 2011.
Because we were interested in residents' initial choice of statin, we only included encounters in which the resident initiated statin therapy for a patient who was already established in the practice (for any indication). We excluded encounters in which the statin was refilled because this may not have reflected resident's choice of medication. We also excluded encounters for new patients because we were unable to distinguish whether the patient came to that visit already taking a statin (started by a previous doctor), with the resident just continuing the prior medication, or whether the resident initiated new statin therapy for the patient. Prescriptions that were later changed or discontinued (eg, if the patient or insurance company requested a change) were included in the analysis because our aim was to study initial prescribing behavior by the resident rather than the final statin obtained by the patient.
Our main outcome variable was percentage of brand name statin prescriptions (atorvastatin and rosuvastatin) for encounters with an established patient who received new statin therapy.
The independent variables were resident characteristics: postgraduate year (PGY), sex, program track (primary care or categorical), whether the resident was the patient's primary care provider, and the hospital care intensity (HCI) index. Residents in the primary care track rotated through the same inpatient rotations in PGY-1, but spent approximately 50% more time in the ambulatory practice in the last 2 years of training than categorical residents. In addition to increased ambulatory care time, primary care track residents were exposed to a comprehensive educational curriculum focusing on ambulatory medicine, including syllabus readings, case-based sessions, and clinical electives (eg, dermatology, musculoskeletal, women's health). No lectures during the study period focused specifically on generic prescribing or health care costs, and the clinic had no existing policy regarding generic medication prescribing.
The HCI is a measure of a health care utilization environment at an academic medical center and was used as a proxy of health care resource utilization intensity level in medical school. The HCI index was developed by the Dartmouth Atlas group14 as a composite of hospital days and inpatient physician visits in the last 2 years of life, using Medicare data. Across the United States, the HCI ranged from 0.6 (low intensity) to 2.1 (high intensity).14
We controlled for the following patient characteristics: age, sex, insurance (Medicare, Medicaid, and private/commercial insurance), and patient comorbidities (coronary artery disease, diabetes, cerebrovascular accident, and tobacco use).
The Weill Cornell Medical College Institutional Review Board reviewed and approved this study.
We performed 2 analyses: 1 at the resident level and 1 at the encounter level. For the resident-level analysis, the χ2 and Fisher exact tests were used to test for associations between resident characteristics and the quintile of proportion of brand name statin prescriptions. For the encounter-level analysis, multivariable logistic regression with clustering at the resident level was used to control for other potentially confounding variables, including the patient and resident characteristics listed above and a dummy variable for each attending to control for the effect of supervising attending. The dependent variable in the regression analysis was whether a brand name versus generic statin was prescribed for the patient.
A P value of < .05 was considered significant. All analyses were performed by using Stata version 11 (StataCorp LP).
Results
During the study interval, residents prescribed a statin for 1565 patient encounters. We excluded 1246 encounters because they were for a refill (81%), or the patient was new to the practice (19%), for a final sample of 319 unique patient encounters with 90 residents (70% of residents in the program) where statin therapy was initiated for an established patient.
Of the 90 residents in the sample, 37% (33 of 90) were PGY-1s; 33% (30 of 90) were PGY-2s; and 30% (27 of 90) were PGY-3s. Primary care track residents made up 11% (10 of 90) of the sample. Average HCI index for medical school residents had attended was 1.1, slightly higher than the national average (1.0).13 At the patient level, 64% (205 of 319) of patients in the sample were women, the mean age was 59.6 years (SD, 12.7 years), and most patients had publicly funded health insurance (40% [128 of 319] Medicare, 38% [122 of 319] Medicaid, and 22% [69 of 319] private/commercial insurance). Approximately a third of the patients had diabetes (34%, 109 of 319); 10% (32 of 319) had coronary artery disease; 2% (7 of 319) had a history of cerebrovascular accident; and 6% (18 of 319) were smokers.
The mean number of statin prescriptions written by each resident during the study period was 3.5 (SD, 0.2). Sixty-three percent of the residents wrote at least 3 statin prescriptions, and 16% (14 of 90) wrote more than 5 prescriptions during the study period. Brand name statins were prescribed in half (50%) of the encounters. We found considerable variation in brand versus generic statin prescribing among the residents (figure). For example, 20 of 90 residents (22%) prescribed brand name statins in less than 20% of eligible encounters, whereas 17 of 90 residents (19%) prescribed brand name statins in greater than 80% of eligible encounters.
FIGURE.
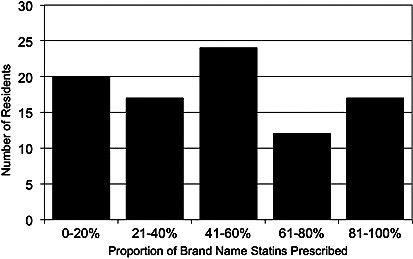
Variation in Generic Versus Brand Name Statin Prescribing Among Residents
This histogram shows the distribution of residents by quintile of brand name statin prescribing. The x-axis represents proportion of statin prescriptions that were written for brand name statins. The y-axis depicts the number of residents in each quintile.
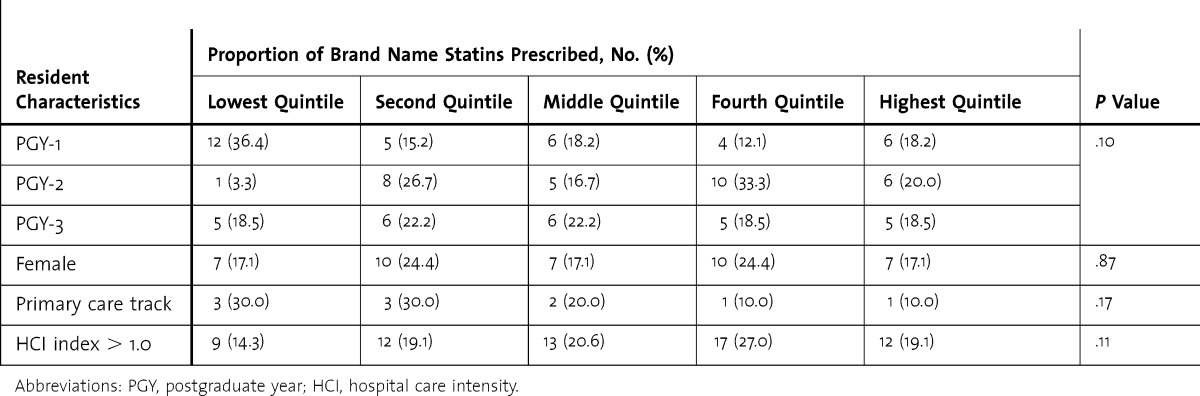
table 1 presents resident characteristics by quintile of brand name statin prescribing. Thirty-six percent (12 of 33) of PGY-1 residents were in the lowest quintile of brand name prescribing, and we did not observe a trend toward more generic prescribing for more senior residents. Although most primary care residents (60%, 6 of 10) were in the lowest 2 quintiles of brand name prescribing, this trend was not statistically significant (P = .17).
TABLE 1.
Resident Characteristics by Level of Brand Name Statin Prescribing
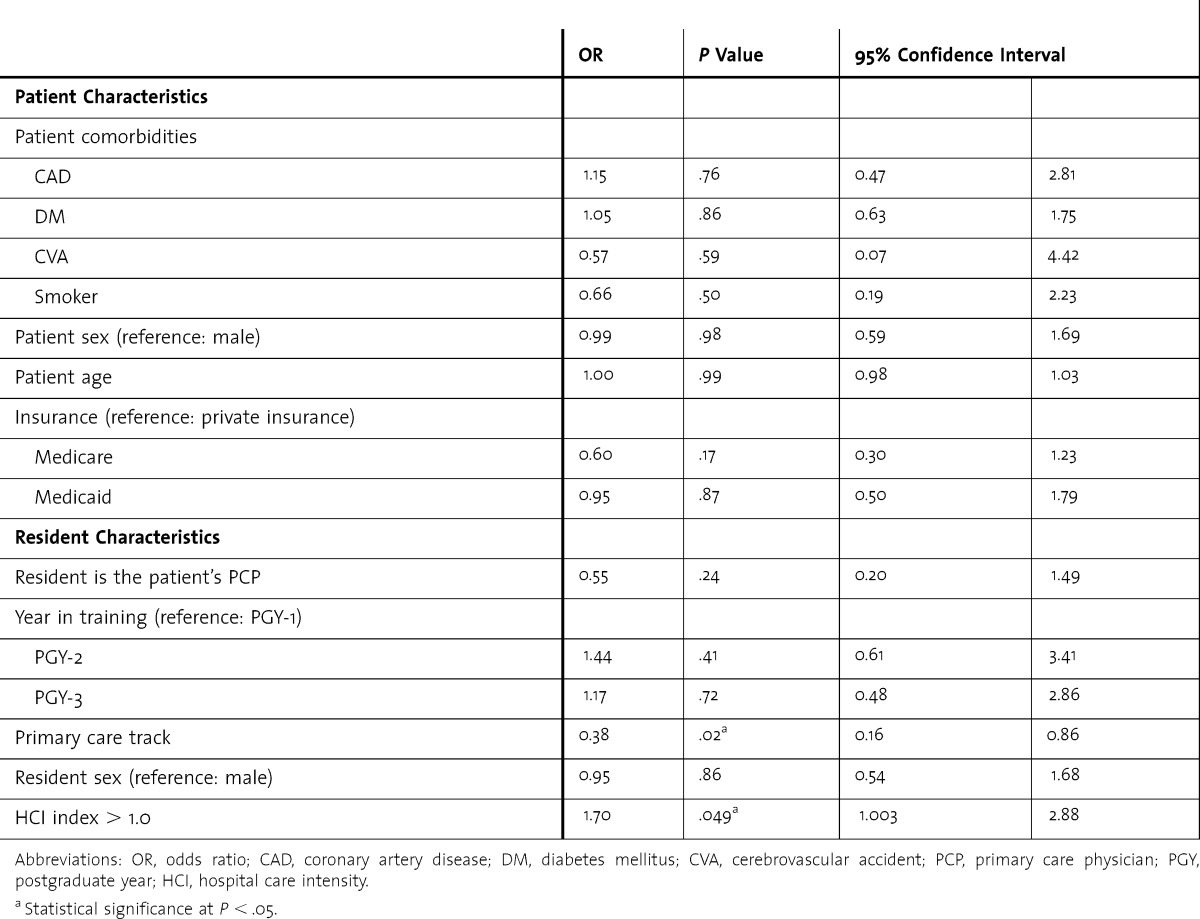
In the encounter-level analysis, after adjusting for patient characteristics, the supervising attending, and clustering at the resident level, we found that being in the primary care track was associated with lower odds of prescribing brand name statins (OR, 0.38; P = .02; 95% CI, 0.16–0.86; table 2). Being exposed to a high HCI environment during medical school was associated with increased odds of prescribing brand name statins in residency (OR, 1.70; P = .049; 95% CI, 1.003–2.88).
TABLE 2.
Factors Associated With Brand Name Prescribing, Controlling for Attending Effect
Discussion
We found sizable variations in brand name versus generic statin prescribing by residents in an ambulatory academic practice. After controlling for attending and patient factors, more intensive health care utilization environment in medical school was positively associated with brand name prescribing, and being in the primary care track was negatively associated with prescribing brand name statins.
We found no association between PGY in training and generic prescribing, suggesting that there was no consistent trend in prescribing patterns as residents progressed through training, which may imply that residents at all years of training could benefit from an intervention. Studies have shown residents welcome feedback regarding resource use relative to their peers.15,16 On the other hand, our findings suggest the possibility that factors early in medical training may play a role in prescribing behavior in residency. It also is not clear whether residents who tended to prescribe generics were more likely to match in the primary care track, or whether the primary care track experience influenced prescribing behavior.
Limitations of this study include a small sample size, a cross-sectional design, and the fact that we only studied a single academic practice reduces generalizability. We also were not able to control for other factors, such as patient request for a brand name statin, which may have influenced resident prescribing.
Larger multicenter studies are needed to better evaluate the relationship between the training environment and physicians' practice styles, as well as the effect of supervising attending physicians and other factors.
Conclusion
Despite ongoing efforts to incorporate cost awareness into medical training, we found that marked variation in generic prescribing exists at the resident level. Our findings represent the first report of factors associated with prescribing of high-cost medications by residents in an ambulatory practice. The hypotheses generated by this study should be tested in future research. A better understanding of the factors that influence practice patterns may inform educational interventions to promote efficient resource utilization by residents, which may have lasting implications for their resource utilization in practice.
Footnotes
Kira L. Ryskina, MD, is General Internal Medicine Fellow, Division of General Internal Medicine, University of Pennsylvania; Michael Pesko, PhD, is Assistant Professor, Division of Health Outcomes and Effectiveness, Department of Public Health, Weill Cornell Medical College; J. Travis Gossey, MD, is Assistant Professor, Department of Medicine, Weill Cornell Medical College; Erica Phillips Caesar, MD, is Associate Professor, Division of Clinical Epidemiology and Evaluative Sciences Research, and Department of Medicine, Weill Cornell Medical College; and Tara F. Bishop, MD, MPH, is Assistant Professor, Division of Health Outcomes and Effectiveness, Department of Public Health, and Department of Medicine, Weill Cornell Medical College.
Funding: The study was supported with WCIMA/Primary Care program funds.
Conflict of Interest: The authors declare they have no competing interests.
These data were presented in preliminary form as a poster during the 36th Annual Meeting of the Society of General Internal Medicine in Denver, Colorado, April 26, 2013.
The authors would like to thank Drs Judy Tung, Christina Harris, and Fred Pelzman for funding assistance.
References
- 1.Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group. National health care expenditure projections 2010–2020. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/proj2010.pdf. Accessed August 19, 2013. [Google Scholar]
- 2.Weinberger SE. Providing high-value, cost conscious care: a critical seventh general competency for physicians. Ann Intern Med. 2011;155(6):386–388. doi: 10.7326/0003-4819-155-6-201109200-00007. [DOI] [PubMed] [Google Scholar]
- 3.Cooke M. Cost consciousness in patient care: what is medical education's responsibility. N Engl J Med. 2010;362(14):1253–1255. doi: 10.1056/NEJMp0911502. [DOI] [PubMed] [Google Scholar]
- 4.Varkey P, Murad MH, Braun C, Grall KJ, Saoji V. A review of cost-effectiveness, cost-containment and economics curricula in graduate medical education. J Eval Clin Pract. 2010;16(6):1055–1062. doi: 10.1111/j.1365-2753.2009.01249.x. [DOI] [PubMed] [Google Scholar]
- 5.Eisenberg JM, Williams SV. Cost containment and changing physicians' practice behavior: can the fox learn to guard the chicken coop. JAMA. 1981;246(19):2195–2201. [PubMed] [Google Scholar]
- 6.Iwashyna TJ, Fuld A, Asch DA, Bellini LM. The impact of residents, interns, and attendings on inpatient laboratory ordering patterns: a report from one university's hospitalist service. Acad Med. 2011;86(1):139–145. doi: 10.1097/ACM.0b013e3181fd85c3. [DOI] [PubMed] [Google Scholar]
- 7.Sommers BD, Desai N, Fiskio J, Licurse A, Thorndike M, Katz JT, et al. An educational intervention to improve cost-effective care among medicine housestaff: a randomized controlled trial. Acad Med. 2012;87(6):719–728. doi: 10.1097/ACM.0b013e31825373b3. [DOI] [PubMed] [Google Scholar]
- 8.Schroeder SA, Myers LP, McPhee SJ, Showstack JA, Simborg DW, Chapman SA, et al. The failure of physician education as a cost containment strategy: report of a prospective controlled trial at a university hospital. JAMA. 1984;252(2):225–230. [PubMed] [Google Scholar]
- 9.Good Stewardship Working Group. The “top 5” lists in primary care: meeting the responsibility of professionalism. Arch Intern Med. 2011;171(15):1385–1390. doi: 10.1001/archinternmed.2011.231. [DOI] [PubMed] [Google Scholar]
- 10.American Board of Internal Medicine Foundation Choosing Wisely. http://www.choosingwisely.org. Accessed May 20, 2014. [Google Scholar]
- 11.Jones P, Kafonek S, Laurora I, Hunninghake D. Comparative dose efficacy study of atorvastatin versus simvastatin, pravastatin, lovastatin, and fluvastatin in patients with hypercholesterolemia (the CURVES study) Am J Cardiol. 1998;81(5):582–587. doi: 10.1016/s0002-9149(97)00965-x. [DOI] [PubMed] [Google Scholar]
- 12.Stender S, Schuster H, Barter P, Watkins C, Kallend D MERCURY I Study Group. Comparison of rosuvastatin with atorvastatin, simvastatin and pravastatin in achieving cholesterol goals and improving plasma lipids in hypercholesterolaemic patients with or without the metabolic syndrome in the MERCURY I trial. Diabetes Obes Metab. 2005;7(4):430–438. doi: 10.1111/j.1463-1326.2004.00450.x. [DOI] [PubMed] [Google Scholar]
- 13.Kale MS, Bishop TF, Federman AD, Keyhani S. “Top 5” lists top $5 billion. Arch Intern Med. 2011;171(20):1856–1858. doi: 10.1001/archinternmed.2011.501. [DOI] [PubMed] [Google Scholar]
- 14.Arora A True A; Dartmouth Atlas of Health Care. What kind of physician will you be: variation in health care and its importance for residency training. http://www.dartmouthatlas.org/downloads/reports/Residency_report_103012.pdf. Published October 30, 2012. Accessed August 5, 2013. [PubMed] [Google Scholar]
- 15.Dine CJ, Miller J, Fuld A, Bellini LM, Iwashyna TJ. Educating physicians-in-training about resource utilization and their own outcomes of care in the inpatient setting. J Grad Med Educ. 2010;2(2):175–180. doi: 10.4300/JGME-D-10-00021.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moriates C, Soni K, Lai A, Ranji S. The value in the evidence: teaching residents to “Choose Wisely.”. JAMA Intern Med. 2013;173(4):308–310. doi: 10.1001/jamainternmed.2013.2286. [DOI] [PubMed] [Google Scholar]


