Abstract
The recently developed dynamic jaw technology of tomotherapy can reduce craniocaudal dose spread without much prolonging the treatment time. This study aimed to investigate the efficacy of the dynamic jaw mode for tomotherapy of breast cancer. Static tomotherapy plans of the whole breast and supraclavicular regional lymph nodes, and plans for the whole breast only were generated in 25 patients with left-sided breast cancer. Plans with a field width of 2.5 or 5 cm with the dynamic or fixed jaw modes were made for each patient. The prescribed dose was 50 Gy in 25 fractions. In whole breast and supraclavicular nodal radiotherapy, dose distributions and homogeneity of the planning target volume (PTV) with the dynamic jaw mode were slightly inferior to those with the fixed jaw mode with a 5-cm field width (P < .05). However, lung low-dose volumes and mean doses of the larynx, thyroid, skin, and all the healthy tissues combined were smaller with the dynamic jaw mode than with the fixed jaw mode with a 5-cm field width (P < .001). In whole breast radiotherapy, mean doses of the skin and healthy tissues were lower with the dynamic jaw mode than with the fixed jaw mode with a 5-cm field width (P < .001) without significant differences in PTV dose distributions, homogeneity, and conformity. The dynamic jaw mode provided better sparing of organs at risks with minimal disturbance of dose–volume indices of PTV. Considering the treatment time, the 5-cm-field dynamic jaw mode is more efficient than the 2.5-cm fixed jaw mode.
Keywords: dynamic jaw mode, static tomotherapy delivery, breast cancer
Introduction
Whole breast radiotherapy is proven to be effective for reducing the risk of locoregional recurrence in patients undergoing lumpectomy for early stage breast cancer.1 Whole breast and supraclavicular nodal radiotherapy is beneficial in reducing the locoregional recurrence risk, especially in patients with ≥4 positive lymph nodes.2 Recently, intensity-modulated radiation therapy (IMRT) is increasingly used for patients with breast cancer to improve planning target volume (PTV) dose homogeneity and reduce doses to the organs at risk (OARs). Several studies reported that IMRT reduced the adverse events of the skin as compared with conventional radiation therapy.3–5
Tomotherapy is considered one of the suitable IMRT modalities for breast cancer.6–9 However, helical tomotherapy plans produce larger low-dose volumes of the other OARs compared with plans with conventional techniques.6,7 The static tomotherapy delivery mode (TomoDirect) can reduce doses to the contralateral breast and low-dose irradiated volume in the lung for patients with breast cancer.8–10 With the conventional fixed jaw mode of tomotherapy, the craniocaudal dose penumbra is a concern; this problem can be partly solved by using a narrower jaw width, but treatment time becomes much longer. More suitable compromise between craniocaudal dose spread and treatment time may be the use of the recently developed dynamic jaw technology with dynamic adaptation of field width at cranial and caudal edges of a target.11–14 This dynamic jaw mode of tomotherapy was recently introduced in our institution first in Japan. Figure 1 shows the difference between the dynamic jaw and conventional fixed jaw (constant field width) modes. The dynamic jaw mode can be used in conjunction with both helical and static tomotherapy delivery modes. The purpose of this study was to investigate the efficacy of the dynamic jaw mode for static tomotherapy of breast cancer.
Figure 1.
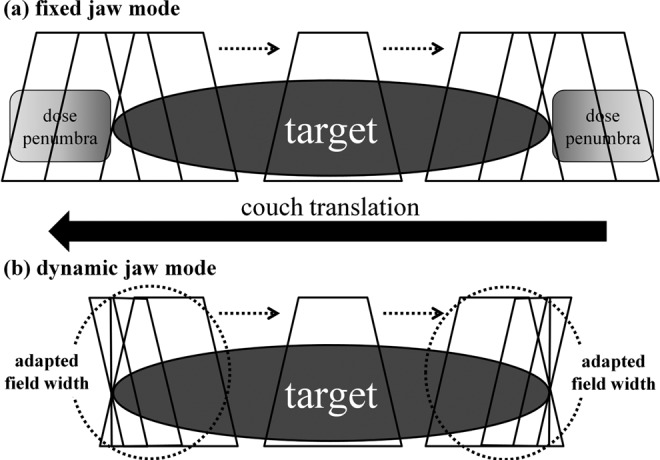
Illustrations of tomotherapy delivery modes. A, Conventional fixed jaw mode yields considerable dose penumbras above and below a target. B, Dynamic jaw mode reduces dose penumbras with dynamic adaptation of field width at cranial and caudal edges of a target.
Materials and Methods
Patients and Computed Tomography Simulation
Twenty-five patients who had been irradiated for a primary left-sided breast cancer after lumpectomy were selected for the present study. Written informed consent had been obtained from all patients regarding their treatment and possible use of their data for research purposes. Computed tomography (CT) scans were performed with a slice thickness of 3.2 mm using a 4-row multidetector CT (Mx8000; Philips Medical Systems, Best, the Netherlands) in the supine position under free but shallow breathing as described previously.15,16 The CT images were reconstructed with a 2.5-mm thickness. The CT simulation and contouring data sets were transferred to the tomotherapy planning station via a Digital Imaging and Communications in Medicine - Radiation Therapy (DICOM-RT) protocol.
Planning Target Volume and OAR Definition and Contouring
The PTV and OARs were contoured on the CT images using the Pinnacle3 treatment planning system (Philips Medical Systems, Best, the Netherlands). The clinical target volume was not defined. The PTV for whole breast radiotherapy including the chest wall with the pectoralis muscle, chest wall muscles, and ribs, and excluding the outermost 3 mm from the superficial skin surface, covered the superior border at the base of the sternal manubrium joint and the inferior border at 1 cm below the inframammary line. The medial border was usually the sternum, and the lateral border was the midaxillary line. The PTV for whole breast and supraclavicular nodal radiotherapy included the supraclavicular, infraclavicular, axillary, apical lymph node areas, and the ipsilateral internal mammary nodes in addition to the PTV for whole breast radiotherapy.17
Delineated OARs were the ipsilateral, contralateral, and bilateral lungs, esophagus, spinal cord, heart, contralateral breasts, stomach, skin, larynx, thyroid gland, trachea, and all the healthy tissues combined. The skin was defined as the volume with a depth of 3 mm from the external surface which was automatically outlined from 2 cm below to 2 cm above the PTV in the craniocaudal direction. The esophagus was contoured from 2 cm below the base of the sternal manubrium joint to 2 cm above the PTV in the craniocaudal direction. The spinal cord and stomach were contoured from 2 cm below to 2 cm above the PTV in the craniocaudal direction. All the healthy tissues combined were defined as the volume of the planning CT set minus the PTV.
Treatment Planning
Treatment plans were created and optimized with the TomoTherapy version 5.0.1 treatment planning station (Accuray, Inc, Sunnyvale, California). Details of the inverse planning algorithm used, the optimization method, and several parameters associated with the optimization in the tomotherapy planning station have been described previously.10,18,19 Treatment plans of the whole breast and supraclavicular regional lymph nodes, and plans for the whole breast only were generated with the static tomotherapy delivery. Whole breast and supraclavicular nodal radiotherapy was planned with 6 gantry angles. Whole breast radiotherapy was planned with 2 gantry angles. On the outer edges, we expanded the beam angle for 3 leaves (1.875 cm) for the respiratory motion. Plans with a field width of 2.5 or 5 cm with the dynamic or fixed jaw modes were made for each patient. The 5-cm field plans were generated with a pitch of 0.5, and the 2.5-cm field plans were generated with a 0.25 pitch. A modulation factor was determined as 2.0, and an actual modulation factor ranged from 1.780 to 2.039 (median 1.894). Maximum dose and dose–volume histogram objectives were defined and regulated during optimization for PTVs and OARs with differential penalties to obtain uniform and adequate PTV coverage with maximum OAR sparing.
Definition and Comparison of Dose–Volume Indices
The prescribed dose was defined as the mean dose of the PTV (Dmean). The prescribed dose was 50 Gy in 25 fractions. As dose constraints for the PTV, (1) D95% > 90% of the prescribed dose, (2) D2% < 107% of the prescribed dose, and (3) V90% > 95% were satisfied. Dx% was defined as the minimum dose delivered to x% of the PTV and OARs. Vx% was defined as the percentage of the PTV and OARs receiving at least x% of the prescribed dose. The Vx Gy represented the percentage of the PTV and OAR volume receiving x Gy. Differences in Dmean between plans with a field width of 2.5 and 5 cm with the dynamic and fixed jaw modes were adjusted within 0.2 Gy for whole breast and supraclavicular nodal radiotherapy, and within 0.1 Gy for whole breast radiotherapy.
Conformity index (CI) was calculated according to the following formula to evaluate the target dose conformity.20,21
where TV = PTV volume, TVRI = target volume covered by the 95% isodose line, and VRI = volume encompassed by 95% isodose line. An ideal CI is 1.
Homogeneity index (HI) was calculated by the following formula to evaluate the target dose homogeneity.22
An ideal HI is zero.
Comparisons of dose–volume parameters of the PTV and OARs and treatment time between plans with a 2.5- or 5-cm field width with the dynamic or fixed jaw modes were carried out using the factorial analysis of variance (ANOVA) followed by the Bonferroni/Dunn post hoc test. All statistical analyses were performed using StatView 5.0 (SAS Institute Inc, Cary, North Carolina). Statistical significance was defined as P ≤ .05. All planning and evaluation were performed by one radiation oncologist (CS). All doses evaluated were calculated physical doses on the planning workstation.
Results
Plans for the Whole Breast and Supraclavicular Regional Lymph Nodes
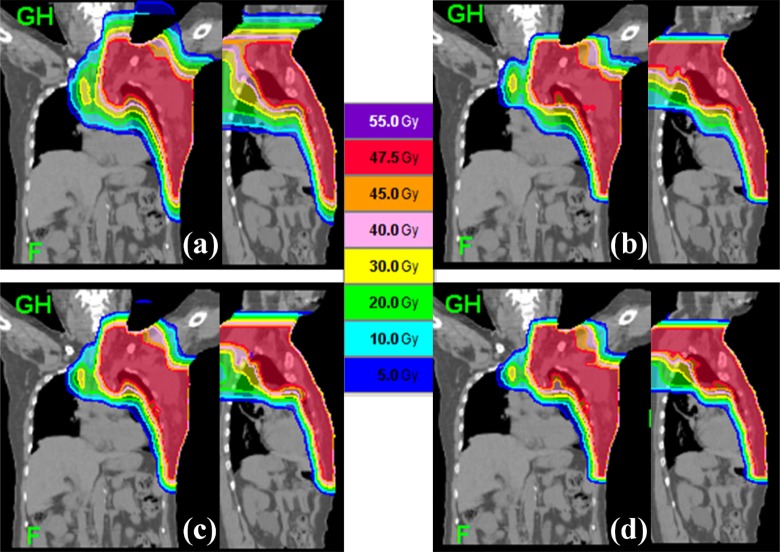
Representative dose distributions of plans for the whole breast and supraclavicular regional lymph nodes are shown in Figure 2. Table 1 summarizes the dose–volume parameters and treatment times of plans of whole breast and supraclavicular regional lymph nodes with a field width of 2.5 or 5 cm with the dynamic or fixed jaw modes in 25 patients. For the PTV, D2% (P < .001), D95%, and HI (P < .05) with the dynamic jaw mode were slightly inferior to those with the fixed jaw mode with a 5-cm field width. D2% and HI with a 5-cm field width were slightly inferior to those with a field width of 2.5 cm. With a 5-cm field width, V5 Gy of the left lung, V5 Gy of the bilateral lungs, Dmean of the larynx, Dmean of the thyroid, Dmean of the skin, and Dmean of all healthy tissues were smaller with the dynamic jaw mode than with the fixed jaw mode (P < .001). D2% of the spinal cord with the dynamic jaw mode was higher than that with the fixed jaw mode (P < .01); however, Dmean of the spinal cord with the dynamic jaw mode was lower than that with the fixed jaw mode (P < .05). With a 2.5-cm field width, Dmean of the skin (P < .001), Dmean of the larynx (P < .01), Dmean of the thyroid, and Dmean of all healthy tissues (P < .05) were lower with the dynamic jaw mode than with the fixed jaw modes. The use of a 5-cm width instead of 2.5 cm reduced the treatment time by approximately 40%. The use of the dynamic jaw instead of the fixed jaw prolonged the treatment time by approximately 6%.
Figure 2.
Representative dose distributions of plans for the whole breast and supraclavicular regional lymph nodes. A, 5-cm field width with the fixed jaw mode; B, 5-cm field width with the dynamic jaw mode; C, 2.5-cm field width with the fixed jaw mode, and D, 2.5-cm field width with the dynamic jaw mode. Dose penumbras above and below the target are reduced with (B) and (D).
Table 1.
Comparison of Dose–Volume Parameters and Treatment Times (mean ± SD) of 4 Plans for Whole Breast and Supraclavicular Regional Lymph Nodes in 25 Patients.
| Structure | Statistics | 5-cmW Fix | 5-cmW Dyn | 2.5-cmW Fix | 2.5-cmW Dyn |
|---|---|---|---|---|---|
| Treatment | Time (seconds) | 296 ± 13a,b,c | 316 ± 13b,c,d | 495 ± 24a,c,d | 529 ± 25a,b,d |
| PTV | Dmean (Gy) | 50.2 ± 0.2 | 50.2 ± 0.2 | 50.1 ± 0.2 | 50.1 ± 0.2 |
| D95% (Gy) | 48.5 ± 0.9e | 48.0 ± 0.7f | 48.3 ± 0.9 | 48.1 ± 0.8 | |
| D2% (Gy) | 51.9 ± 0.3a,g | 52.4 ± 0.3b,d,g | 52.0 ± 0.3a | 52.2 ± 0.3h,i | |
| CI | 0.59 ± 0.06j,k | 0.58 ± 0.07g,l | 0.63 ± 0.06f,i | 0.63 ± 0.06f,i | |
| HI | 0.09 ± 0.04e | 0.11 ± 0.03f | 0.10 ± 0.03 | 0.10 ± 0.03 | |
| Bilateral lungs | Dmean (Gy) | 11.1 ± 1.2b,c | 10.6 ± 1.2c,l | 9.8 ± 1.0d,i | 9.5 ± 1.0a,d |
| V5 Gy (%) | 34.7 ± 3.8a,b,c | 30.8 ± 3.2c,d,j | 29.0 ± 2.7d,e | 27.3 ± 2.7a,d | |
| V20 Gy (%) | 22.8 ± 2.7b,c | 21.9 ± 2.9c,j | 20.0 ± 2.4d,e | 19.3 ± 2.4a,d | |
| Left lung | Dmean (Gy) | 22.0 ± 2.2b,c | 21.5 ± 2.1c,l | 19.9 ± 1.9d,i | 19.6 ± 1.9a,d |
| V5 Gy (%) | 64.6 ± 4.7a,b,c | 59.2 ± 3.6c,d,j | 56.6 ± 3.8d,e | 54.1 ± 3.7a,d | |
| V20 Gy (%) | 48.5 ± 4.6b,c | 47.0 ± 4.7c,l | 43.4 ± 4.7d,i | 42.3 ± 4.4a,d | |
| Right lung | Dmean (Gy) | 2.3 ± 1.0c,l | 2.0 ± 0.8k | 1.7 ± 0.7h | 1.5 ± 0.6d,e |
| V5 Gy (%) | 10.4 ± 6.1c,j | 8.2 ± 4.6 | 7.0 ± 4.3f | 5.9 ± 3.5d | |
| V20 Gy (%) | 2.4 ± 1.7c,l | 1.9 ± 1.5k | 1.4 ± 1.1h | 1.0 ± 0.8d,e | |
| Spinal cord | D2% (Gy) | 14.0 ± 4.9i | 17.9 ± 4.2g.h,l | 14.1 ± 4.7i | 14.8 ± 4.2i |
| Dmean (Gy) | 4.5 ± 1.2c,e,j | 4.0 ± 0.7f,k,l | 3.5 ± 0.9f,i | 3.1 ± 0.7d,e | |
| Larynx | Dmean (Gy) | 15.8 ± 2.9a,b,c | 11.7 ± 2.3d,g | 11.7 ± 2.5d,g | 9.4 ± 2.1d,i,l |
| Esophagus | Dmean (Gy) | 22.8 ± 2.8c,l | 22.3 ± 3.1g,j | 20.4 ± 2.8e,h | 19.6 ± 2.6d,i |
| Thyroid | Dmean (Gy) | 30.4 ± 3.4a,c,l | 26.9 ± 2.8d | 27.7 ± 3.3h,k | 25.9 ± 2.7d,j |
| Trachea | Dmean (Gy) | 25.7 ± 4.8k | 24.1 ± 5.1 | 23.6 ± 4.8 | 22.2 ± 4.6f |
| Heart | Dmean (Gy) | 6.8 ± 2.6j,k | 7.0 ± 2.3g,l | 5.2 ± 2.1f,i | 5.2 ± 2.0f,i |
| Stomach | Dmean (Gy) | 4.8 ± 3.2k | 3.8 ± 2.3 | 3.6 ± 2.4 | 3.1 ± 2.1f |
| Right breast | Dmean (Gy) | 2.6 ± 1.3 | 2.9 ± 1.4j,k | 2.1 ± 1.1e | 2.1 ± 1.0e |
| Skin | Dmean (Gy) | 15.7 ± 0.7a,b,c | 14.7 ± 0.6b,c,d | 14.1 ± 0.6a,c,d | 13.5 ± 0.5a,b,d |
| Tissues | Dmean (Gy) | 9.6 ± 0.8a,b,c | 8.8 ± 0.8b,c,d | 7.9 ± 0.7a,c,d | 7.4 ± 0.6a,b,d |
Abbreviations: PTV, planning target volume; cmW, cm field width; Fix, fixed jaw mode; Dyn, dynamic jaw mode; Tissues, all healthy tissues combined.
a Versus 5 cmW Dyn (P < .001).
b Versus 2.5 cmW Fix (P < .001).
c Versus 2.5 cmW Dyn (P < .001).
d Versus 5 cmW Fix (P < .001).
e Versus 5 cmW Dyn (P < .05).
f Versus 5 cmW Fix (P < .05).
g Versus 2.5 cmW Dyn (P < .01).
h Versus 5 cmW Fix (P < .01).
i Versus 5 cmW Dyn (P < .01).
j Versus 2.5 cmW Fix (P < .05).
k Versus 2.5 cmW Dyn (P < .05).
l Versus 2.5 cmW Fix (P < .01).
Plans for the Whole Breast
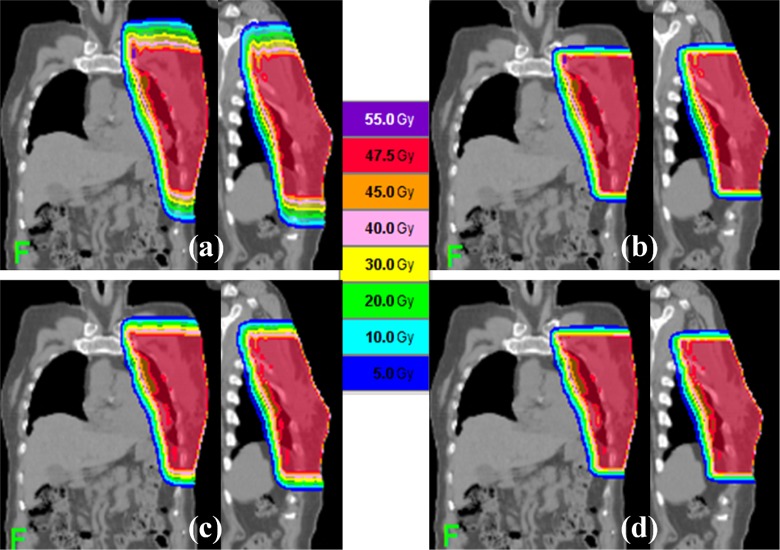
Figure 3 shows representative dose distributions of plans for the whole breast. Table 2 shows the dose–volume parameters and treatment times of plans for whole breast with a 2.5- or 5-cm field width with the dynamic or fixed jaw modes in 25 patients. For the PTV, D95%, Dmean, D2%, CI, and HI were similar in the 4 plans. With a 5-cm field width, Dmean of the skin and all healthy tissues were lower with the dynamic jaw mode than with the fixed jaw mode (P < .001). With a 2.5-cm width, Dmean of all of the healthy tissues (P <.001) and Dmean of the skin (P < .01) were lower with the dynamic jaw mode than with the fixed jaw mode. Dmeans of the contralateral lung, contralateral breast, spinal cord, esophagus, and trachea were less than 1 Gy; therefore, doses to these OARs were considered clinically negligible. No dose–volume parameters were inferior in the 5-cm dynamic jaw plans to those in the 2.5-cm fixed jaw plans. The use of a 5-cm width instead of 2.5 cm reduced the treatment time by approximately 40%. The dynamic jaw mode prolonged the treatment time by approximately 5% compared to the fixed jaw mode.
Figure 3.
Representative dose distributions of plans for the whole breast. A, 5-cm field width with the fixed jaw mode; B, 5-cm field width with the dynamic jaw mode; C, 2.5-cm field width with the fixed jaw mode, and D, 2.5-cm field width with the dynamic jaw mode. Dose penumbras above and below the target are reduced with (B) and (D).
Table 2.
Comparison of Dose–Volume Parameters and Treatment Times (mean ± SD) of 4 Plans for Whole Breast in 25 Patients.
| Structure | Statistics | 5-cmW Fix | 5-cmW Dyn | 2.5-cmW Fix | 2.5-cmW Dyn |
|---|---|---|---|---|---|
| Treatment | Time (seconds) | 214 ± 21a,b | 223 ± 20a,b | 343 ± 48b,c,d | 369 ± 41c,d,f |
| PTV | Dmean (Gy) | 50.0 ± 0.1 | 50.0 ± 0.1 | 50.0 ± 0.1 | 50.0 ± 0.1 |
| D95% (Gy) | 48.4 ± 0.3 | 48.4 ± 0.4 | 48.4 ± 0.4 | 48.4 ± 0.4 | |
| D2% (Gy) | 52.0 ± 0.5 | 52.0 ± 0.5 | 52.0 ± 0.5 | 52.1 ± 0.5 | |
| CI | 0.76 ± 0.13 | 0.78 ± 0.13 | 0.79 ± 0.13 | 0.80 ± 0.13 | |
| HI | 0.09 ± 0.02 | 0.09 ± 0.02 | 0.09 ± 0.02 | 0.09 ± 0.02 | |
| Bilateral lungs | Dmean (Gy) | 4.6 ± 1.1 | 4.6 ± 1.1 | 4.3 ± 1.1 | 4.3 ± 1.1 |
| V5 Gy (%) | 13.0 ± 3.3 | 12.9 ± 3.3 | 11.9 ± 3.1 | 11.9 ± 3.1 | |
| V20 Gy (%) | 8.8 ± 2.5 | 8.8 ± 2.5 | 8.0 ± 2.4 | 8.0 ± 2.4 | |
| Left lung | Dmean (Gy) | 9.9 ± 2.2 | 9.8 ± 2.1 | 9.1 ± 2.1 | 9.1 ± 2.1 |
| V5 Gy (%) | 29.1 ± 6.1 | 28.7 ± 6.1 | 26.6 ± 5.8 | 26.4 ± 5.8 | |
| V20 Gy (%) | 19.5 ± 4.9 | 19.5 ± 4.8 | 17.7 ± 4.7 | 17.7 ± 4.7 | |
| Heart | Dmean (Gy) | 4.8 ± 1.6 | 4.7 ± 1.6 | 4.4 ± 1.5 | 4.3 ± 1.5 |
| Stomach | Dmean (Gy) | 4.4 ± 2.7e | 3.3 ± 2.3 | 3.4 ± 2.3 | 2.9 ± 2.1g |
| Skin | Dmean (Gy) | 13.6 ± 0.9b,d,f | 12.6 ± 0.9c | 12.9 ± 1.0g,h | 12.1 ± 0.9c,i |
| Tissues | Dmean (Gy) | 4.2 ± 0.4a,b,d | 3.6 ± 0.4b,c,f | 3.7 ± 0.4b,c,j | 3.2 ± 0.4a,c,d |
Abbreviations: cmW, cm field width; Fix, fixed jaw mode; Dyn, dynamic jaw mode; Tissues, all healthy tissues combined.
a Versus 2.5 cmW Fix (P < .001).
b Versus 2.5 cmW Dyn (P < .001).
c Versus 5 cmW Fix (P < .001).
d Versus 5 cmW Dyn (P < .001).
e Versus 2.5 cmW Dyn (P < .05).
f Versus 2.5 cmW Fix (P < .05).
g Versus 5 cmW Fix (P < .05).
h Versus 2.5 cmW Dyn (P < .01).
i Versus 2.5 cmW Fix (P < .01).
j Versus 5 cmW Dyn (P < .05).
Discussion and Conclusion
To our knowledge, this is the first study that evaluated the efficacy of the dynamic jaw mode with static tomotherapy delivery mode for breast cancer treatment. Compared to the fixed jaw mode, the dynamic jaw mode enabled to reduce the doses of some OARs. The dynamic jaw mode seemed to be more effective for the plans of the whole breast and supraclavicular regional lymph nodes compared with the plans of the whole breast in reducing the number of OARs for which radiation doses could be lowered. For this purpose, the dynamic jaw mode was more effective for the 5-cm plans as compared with the 2.5-cm plans. Although D2%, D95%, and HI of the PTV with the dynamic jaw mode were slightly inferior to those with the fixed jaw mode with a 5-cm field width, the differences in the dose–volume indices for the PTV seemed to be clinically acceptable. The slight deterioration of dose–volume indices of the PTV using the dynamic jaw mode with a 5-cm field width for the plans of the whole breast and supraclavicular regional lymph nodes may be caused by sharply cutting the craniocaudal edges of the PTV and should be taken into account in treatment planning.
The doses of the skin and all the healthy tissues with the dynamic jaw mode were significantly lower than those with fixed jaw modes in both plans of the whole breast with supraclavicular regional lymph nodes and plans of the whole breast. With the dynamic jaw mode, the reduction of doses to the skin and all the healthy tissues would be owing to the decrease in the craniocaudal dose penumbra by sharply cutting the craniocaudal edges of the PTV. The reduction of skin dose might reduce the adverse events of the skin and might improve quality of life, pain scores, and cosmesis.3,4 The reduction of doses to all the healthy tissues combined might reduce the possibility of second malignancies owing to larger volumes of normal tissues exposed to lower radiation dose. In the plan of the whole breast and supraclavicular regional lymph nodes, the low-dose volumes of the lungs were lower with the 5-cm dynamic jaw mode than with the fixed jaw modes. The reduction of the lung volume receiving lower dose may reduce the possibility of radiation pneumonitis.23
Although helical tomotherapy is an excellent treatment modality enabling precise and sophisticated IMRT, relatively long time required for daily treatment has been considered to be a drawback of conventional mode of tomotherapy. It has been reported that attempts at reducing the treatment time by shortening the time for positioning and registration, changing the pitch, and limiting the use of 1-cm field width resulted in shortening the overall time by 7.7 minutes on average.24 In the present study, the dynamic jaw mode prolonged the treatment time by 5% to 6% compared to the fixed jaw mode of the same size. This is due to the relatively slower couch speed in the dynamic jaw mode to keep acceptable dose distribution at the craniocaudal edges of the PTV. However, the treatment time was much shorter compared to the smaller field treatment while the dose distributions were comparable or not much inferior. Using the dynamic jaw mode with a wider field width would contribute to further reducing the time while maintaining the treatment quality.
This study has several limitations. First, only the dynamic jaw mode was applied in this study with no use of the dynamic couch delivery,11–13 because the latter mode is not yet available. If the dynamic jaw and dynamic couch delivery is applied, the doses of the OARs existing at the level of the PTV (eg, the lung and heart) are expected to be reduced, but the treatment time is estimated to be prolonged. Second, the candidates of this study were limited to patients with left-sided breast cancer similar to previous studies, because the heart was considered to be one of the most important OARs.7,8 The dose of the liver might possibly be affected if the patients with right-sided breast cancer are evaluated. Third, comparison with conventional radiotherapy and IMRT using a linear accelerator was not carried out in this study. Reducing the craniocaudal dose penumbra by sharply cutting the craniocaudal edges of the PTV with the dynamic jaw mode may produce more favorable dose distribution compared to the methods using a linear accelerator. Further investigation is warranted.
In conclusion, for postoperative breast irradiation with static tomotherapy, the dynamic jaw mode was effective in reducing the treatment time and the doses of OARs in both of the plans of the whole breast with supraclavicular regional lymph nodes and those of the whole breast. Slight deterioration of dose–volume indices of the PTV using the dynamic jaw mode with a 5-cm field width was found for the plans of the whole breast and supraclavicular regional lymph nodes, but it seemed to be clinically acceptable.
Acknowledgments
This study was carried out by an offered mechanical option of tomotherapy from Accuray Japan K.K. without any financial support.
Abbreviations
- IMRT
intensity-modulated radiation therapy
- OAR
organ at risk
- PTV
planning target volume
- Dmean
the mean dose of PTV and OARs
- Dx%
the minimum dose delivered to x% of PTV and OARs
- Vx%
the percentage of PTV and OARs receiving at least x% of the prescribed dose
- Vx Gy
the percentage volume receiving x Gy of PTV and OARs
- CI
conformity index
- HI
homogeneity index.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366 (9503):2087–2106. [DOI] [PubMed] [Google Scholar]
- 2. Grills IS, Kestin LL, Goldstein N, Mitchell C, Martinez A, Ingold J, Vicini FA. Risk factors for regional nodal failure after breast-conserving therapy: regional nodal irradiation reduces rate of axillary failure in patients with four or more positive lymph nodes. Int J Radiat Oncol Biol Phys. 2003;56 (3):658–670. [DOI] [PubMed] [Google Scholar]
- 3. Keller LM, Sopka DM, Li T, et al. Five-year results of whole breast intensity modulated radiation therapy for the treatment of early stage breast cancer: the Fox Chase Cancer Center experience. Int J Radiat Oncol Biol Phys. 2012;84 (4):881–887. doi: 10.1016/j.ijrobp.2012.01.069. [DOI] [PubMed] [Google Scholar]
- 4. Pignol JP, Olivotto I, Rakovitch E, et al. A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J Clin Oncol. 2008;26 (13):2085–2092. doi: 10.1200/JCO.2007.15.2488. [DOI] [PubMed] [Google Scholar]
- 5. Yang Z, Chen J, Xie J, et al. Simultaneous integrated boost in breast conserving radiotherapy: is replanning necessary following tumor bed change? Technol Cancer Res Treat. 2013;12 (2):115–122. doi: 10.7785/tcrt.2012.500309. [DOI] [PubMed] [Google Scholar]
- 6. Zhou GX, Xu SP, Dai XK, et al. Clinical dosimetric study of three radiotherapy techniques for postoperative breast cancer: Helical Tomotherapy, IMRT, and 3D-CRT. Technol Cancer Res Treat. 2011;10 (1):15–23. [DOI] [PubMed] [Google Scholar]
- 7. Goddu SM, Chaudhari S, Mamalui-Hunter M, et al. Helical tomotherapy planning for left-sided breast cancer patients with positive lymph nodes: comparison to conventional multiport breast technique. Int J Radiat Oncol Biol Phys. 2009;73 (4):1243–1251. doi: 10.1016/j.ijrobp.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 8. Schubert LK, Gondi V, Sengbusch E, et al. Dosimetric comparison of left-sided whole breast irradiation with 3DCRT, forward-planned IMRT, inverse-planned IMRT, helical tomotherapy, and topotherapy. Radiother Oncol. 2011;100 (2):241–246. doi: 10.1016/j.radonc.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 9. Reynders T, Tournel K, De Coninck P, et al. Dosimetric assessment of static and helical TomoTherapy in the clinical implementation of breast cancer treatments. Radiother Oncol. 2009;93 (1):71–79. doi: 10.1016/j.radonc.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 10. Murai T, Shibamoto Y, Manabe Y, et al. Intensity-modulated radiation therapy using static ports of tomotherapy (TomoDirect): comparison with the TomoHelical mode. Radiat Oncol. 2013;8:68 doi: 10.1186/1748-717X-8-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Krause S, Beck S, Schramm O, et al. Tomotherapy radiosurgery for arteriovenous malformations--current possibilities and future options with helical tomotherapy dynamic jaws? Technol Cancer Res Treat. 2013;12 (5):421–428. doi: 10.7785/tcrt.2012.500335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sterzing F, Uhl M, Hauswald H, et al. Dynamic jaws and dynamic couch in helical tomotherapy. Int J Radiat Oncol Biol Phys. 2010;76 (4):1266–1273. doi: 10.1016/j.ijrobp.2009.07.1686. [DOI] [PubMed] [Google Scholar]
- 13. Krause S, Beck S, Schubert K, et al. Accelerated large volume irradiation with dynamic Jaw/Dynamic Couch Helical Tomotherapy. Radiat Oncol. 2012;7:191 doi: 10.1186/1748-717X-7-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Manabe Y, Shibamoto Y, Sugie C, Hayashi A, Murai T, Yanagi T. Helical and static-port tomotherapy using the newly-developed dynamic jaws technology for lung cancer [published online ahead of print June 16, 2014]. Technol Cancer Res Treat. doi: 10.7785/tcrtexpress.2013.600280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shibamoto Y, Naruse A, Fukuma H, Ayakawa S, Sugie C, Tomita N. Influence of contrast materials on dose calculation in radiotherapy planning using computed tomography for tumors at various anatomical regions: a prospective study. Radiother Oncol. 2007;84 (1):52–55. doi: 10.1016/j.radonc.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 16. Tatekawa K, Iwata H, Kawaguchi T, et al. Changes in volume of stage I non-small-cell lung cancer during stereotactic body radiotherapy. Radiat Oncol. 2014;9:8 doi : 10.1186/1748-717X-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Truong PT, Olivotto IA, Whelan TJ, Levine M; Steering committee on clinical practice guidelines for the care and treatment of breast cancer. Clinical practice guidelines for the care and treatment of breast cancer: 16. Locoregional post-mastectomy radiotherapy. CMAJ. 2004;170 (8):1263–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sugie C, Shibamoto Y, Ayakawa S, et al. Craniospinal irradiation using helical tomotherapy: evaluation of acute toxicity and dose distribution. Technol Cancer Res Treat. 2011;10 (2):187–195. [DOI] [PubMed] [Google Scholar]
- 19. Kissick MW, Fenwick J, James JA, et al. The helical tomotherapy thread effect. Med Phys. 2005;32 (5):1414–1423. [DOI] [PubMed] [Google Scholar]
- 20. van't Riet A, Mak AC, Moerland MA, Elders LH, van der Zee W. A conformation number to quantify the degree of conformality in brachytherapy and external beam irradiation: application to the prostate. Int J Radiat Oncol Biol Phys. 1997;37 (3):731–736. [DOI] [PubMed] [Google Scholar]
- 21. Feuvret L, Noël G, Mazeron JJ, Bey P. Conformity index: a review. Int J Radiat Oncol Biol Phys. 2006;64 (2):333–342. [DOI] [PubMed] [Google Scholar]
- 22. The International Commission on Radiation Units and Measurements ICRU Report No. 83: Prescribing, Recording, and Reporting Photon-Beam Intensity-Modulated Radiation Therapy (IMRT). J ICRU. 2010;10 doi:10.1093/jicru/ndq002. [Google Scholar]
- 23. Aibe N, Yamazaki H, Nakamura S, et al. Outcome and toxicity of stereotactic body radiotherapy with helical tomotherapy for inoperable lung tumor: analysis of Grade 5 radiation pneumonitis. J Radiat Res. 2014;55 (3):575–582. doi: 10.1093/jrr/rrt146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Piotrowski T, Czajka E, Bak B, et al. Tomotherapy: implications on daily workload and scheduling patients based on three years' institutional experience. Technol Cancer Res Treat. 2014;13 (3):233–242. doi: 10.7785/tcrt.2012.500374. [DOI] [PubMed] [Google Scholar]