Abstract
BACKGROUND
There have been no comprehensive studies across an organized statewide trauma system using a standardized method to determine cost.
STUDY DESIGN
Trauma financial impact includes the following costs: verification, response, and patient care cost (PCC). We conducted a survey of participating trauma centers (TCs) for federal fiscal year 2012, including separate accounting for verification and response costs. Patient care cost was merged with their trauma registry data. Seventy-five percent of the 2012 state trauma registry had data submitted. Each TC’s reasonable cost from the Medicare Cost Report was adjusted to remove embedded costs for response and verification. Cost-to-charge ratios were used to give uniform PCC across the state.
RESULTS
Median (mean ± SD) costs per patient for TC response and verification for Level I and II centers were $1,689 ($1,492 ± $647) and $450 ($636 ± $431) for Level III and IV centers. Patient care cost–median (mean ± SD) costs for patients with a length of stay >2 days rose with increasing Injury Severity Score (ISS): ISS <9: $6,787 ($8,827 ± $8,165), ISS 9 to 15: $10,390 ($14,340 ± $18,395); ISS 16 to 25: $15,698 ($23,615 ± $21,883); and ISS 25+: $29,792 ($41,407 ± $41,621), and with higher level of TC: Level I: $13,712 ($23,241 ± $29,164); Level II: $8,555 ($13,515 ± $15,296); and Levels III and IV: $8,115 ($10,719 ± $11,827).
CONCLUSIONS
Patient care cost rose with increasing ISS, length of stay, ICU days, and ventilator days for patients with length of stay >2 days and ISS 9+. Level I centers had the highest mean ISS, length of stay, ICU days, and ventilator days, along with the highest PCC. Lesser trauma accounted for lower charges, payments, and PCC for Level II, III, and IV TCs, and the margin was variable. Verification and response costs per patient were highest for Level I and II TCs.
Both the cost and financial impact of a hospital’s participation in a trauma system have remained largely a mystery in the United States. This is despite the critical nature of trauma care to the overall health care of our nation. Our study attempts to answer some essential questions about the Trauma Financial Impact (TFI) on trauma centers (TCs) by the use of an innovative system-wide methodology that allows us to view financial factors, including standardized costs alongside pertinent patient clinical factors. This article will lay out the background and methodology of our survey and will report on substantive initial findings of the survey.
Arkansas developed a statewide trauma system in 2009, with legislation that established, among other things, funding for TCs, an integrated statewide trauma call system, uniform trauma triage guidelines, implementation of the American College of Surgeons National Trauma Data Base registry in all TCs, and use of a unique Trauma Band ID number assigned to each patient, which follows them through the trauma system. The Arkansas Department of Health oversees the trauma system with the advice of the Trauma Advisory Committee, composed of representatives of all of the major providers and professional organizations dealing with trauma. The Arkansas Trauma System recognizes the need to include TCs in adjacent states that care for the citizens of our state and, as of July 2014, has incorporated 5 TCs in Tennessee, Texas, and Missouri, along with 64 Arkansas hospitals into the Arkansas Trauma System. The initial funding for hospitals during the start-up phase has been by a grant mechanism, allocating a priori assigned block grants to the 4 levels of TCs, along with a portion allocated to pay-for-performance funding for achievement of certain goals and targets. As the trauma system progresses, one of the goals of our system will be to match the allocation of funding to the TFI for various levels of TCs, as well as certain types of trauma patients with resource-intensive requirements. The Trauma Financial Survey was designed to help answer questions about appropriate funding to assure the sustainability of our system. The aim of this article is to outline the background, development, learning lessons, methodology, and initial results of this survey.
METHODS
Survey purpose and design
In 2011, the Arkansas Trauma System underwent an American College of Surgeons Trauma System Consultation and, from that review, a series of recommendations were issued, with one calling for improvements in cost analysis. They explained that “routine collection of financial data from all participating health care facilities is encouraged to fully identify the costs and revenues of the trauma system, including costs and revenues pertaining to patient care, administrative, and trauma center operations.”1 The report also recommended that Arkansas: “Actively engage the Arkansas Hospital Association (and other associations as relevant) in resource and cost identification, best practice, performance improvement, cost-effectiveness and capacity-building strategies, including on a contractual basis if necessary and appropriate.”1
Based on their recommendations, the Finance Committee of the Trauma Advisory Committee formed a workgroup consisting of members of the Finance Committee and the Arkansas Hospital Association to develop a system-wide trauma financial survey. The survey was designed to deliver a comprehensive analysis of the cost of caring for trauma patients, using a methodology thatwould allow for comparisons of similar patient care costs (PCC) across the hospitals participating in our trauma system. The workgroup noted that the Arkansas Trauma System had several characteristics and assets that would allow us an unprecedented opportunity to examine the cost drivers for the care of the trauma patient. These assets included the development of a trauma band ID, which is a unique number assigned to an armband that was attached to every patient at entry into the trauma system. This trauma band and ID number allowed the Arkansas Trauma System to identify and track all trauma patients from prehospital through rehabilitation, including transfers within the trauma system. Another asset was a statewide, uniform collection of patient care data in a state trauma registry. All hospitals in the trauma system were supplied and trained on the American College of Surgeons trauma registry software. These TCs submitted their data to the Arkansas Trauma Registry, allowing the Trauma System to collect a standardized set of clinical data on every patient, using a standard set of inclusion criteria and a uniform data dictionary.2 This enabled us to then link relevant clinical data to the financial billing information for that patient, allowing us to correlate clinical factors with revenue and cost information from participating TCs.
The workgroup also determined that it would be advantageous to have a separate accounting of the costs of a hospital to become and maintain the status of an Arkansas TC (termed verification costs) and the costs incurred in being able and capable of responding to incoming trauma patients by activation of a trauma team (termed response costs). A consulting and accounting firm with specialized expertise in hospital and health care accounting, BKD LLP, was brought in as an advisor to help assist the work-group in devising a unique methodology to accomplish these aims. BKD LLP had a long history of working closely with many of the hospitals in Arkansas and surrounding states, and had the expertise and infrastructure to ably advise the workgroup on the critical elements of such a survey. The workgroup submitted its recommendations for the Trauma Financial Survey to the Arkansas Department of Health, which authorized funding to conduct the survey under the guidance of the Arkansas Hospital Association, which in turn selected BKD LLP as the agent to conduct the survey. Due to the sensitive and competitive nature of hospital pricing and financial data, one initial concern was that few hospitals would want to share their data for such a survey. However, having the Arkansas Hospital Association involved from the start, and adding the expertise and history of BKD LLP, helped ensure confidentiality and good participation of the TCs in the survey. To encourage TCs to participate in the survey, a portion of the TC funding for fiscal year 2013 was set aside as a pay-for-performance grant for each hospital completing the survey. Pay-for-performance was based on the number of patients submitted with complete data, divided into the available funds. This dollar-per-patient conversion factor was then used to determine the pay-for-performance bonus for each participating hospital. This encouraged TCs to participate by offsetting the cost of collecting and translating these data into a uniform format usable for the survey. The survey process began in 2013 and concluded in the spring of 2014.
Methodology of estimating uniform cost data
BKD LLP used the most recently filed Medicare Cost Report (MCR) as a starting point to help with the relative comparability of each facility. Medicare requires all participating hospitals to submit annual cost reports that are prepared based on very detailed provider reimbursement guidelines. Using the MCR provides the following main benefits: It allows use of standard Medicare guidelines for which expenses are considered reasonable and included in the cost of patient care; costs are grouped into standardized cost centers (radiology, pharmacy, etc); and all overhead costs are allocated through the step-down process to appropriate cost centers using reasonable statistics and standard methods.
Because the MCR disallows physician and nurse anesthetist costs for direct patient care, it is necessary to add these items back to fully identify the costs associated with providing trauma care. These costs were identified through a brief survey completed by each participating TC. These costs were then accumulated and added to the relevant cost center within the cost report for each TC.
Physician and other costs associated with verification costs were captured separately, summed for each TC, and removed from the MCR. Examples of such costs would be financial support for the trauma medical director, trauma program staff, and for maintenance of the trauma registry. Response costs (eg, trauma activation costs) were also identified through the provider survey and removed in a process similar to that identified here for verification costs. Because 100% of these costs are attributable to participation as a TC in the Trauma System, as opposed to a nontrauma hospital caring for trauma patients, removing them avoids duplication of attributing these expenses to the cost of trauma patient care.
After these adjustments were made, revised cost-to-charge ratios (CCR) were calculated for the individual cost centers. Each participating TC provided a listing of trauma claims and procedure-level charge details. In addition, a crosswalk was provided between the procedure codes and Medicare cost center or a crosswalk between department and Medicare cost center, depending on the method the provider used to complete their MCR.
The crosswalks were then used to map each charge to its respective standardized cost center. This allowed the charges to be multiplied by the appropriate CCR to estimate cost. These estimated costs were then summarized by claim and TC to estimate the overall cost of the direct patient care–related portion of providing trauma services. The data elements captured in the PCC portion of the survey included those from the Arkansas Trauma Registry data dictionary3 plus payer status or insurance classification, charges, and payment amounts.
Financial measures were defined for each patient as total charges, total payments, estimated cost, and total margin. Total margin was defined as total payment minus estimated cost. Factors impacting TC payment were primarily determined by insurance/payer status. The multiple payer classes were grouped into the following primal groups: Medicare (including Medicare Advantage), Medicaid, other third party (eg, commercial insurance, worker’s compensation, etc), and self-pay. Potential drivers of cost measured for each patient included length of stay (LOS), Injury Severity Score (ISS), ICU days, and ventilator days.
Once the data were analyzed by BKD LLP, they prepared a de-identified dataset by removing all protected health care information from each record, and substituted a unique patient identifier number for the trauma band ID number. Hospital identity was blinded except for the verified level of Arkansas TC.
Statistical methods
Patient demographic, medical, and financial characteristics were summarized using descriptive statistics. Specifically, means, SD, and medians were used to summarize variables that were continuous or ordinal in nature, and percentages and counts were used to summarize categorical variables. Kruskall-Wallis tests and Wilcoxon rank-sum tests were used to compare TCs with respect to continuous and ordinal variables, and Pearson’s chi-square tests were used for categorical variables. In addition, Spearman’s rho correlation coefficient was used to assess the association between financial measures and patient medical or hospitalization characteristics (eg, ISS, and LOS). Summaries are presented for all patients, but detailed summaries are presented for patients with LOS ≥2 days.
Methodology for accounting for verification and trauma response costs
The accounting of these costs into standard cost categories varied widely between hospitals, with no common theme as to how response or verification costs were included in the MCR. For example, some hospitals did not pay for physician on-call services, and others had compensation for those physicians on call for the trauma team. Other hospitals had employed physicians serving on the trauma team, and it was sometimes challenging to determine what portion of their salary was due to on-call trauma-related services. Each hospital’s MCR underwent meticulous study by BKD LLP to tease out these various costs associated with becoming and maintaining a TC and the response to trauma patients arriving at the TC. The on-call requirements for numbers and types of specialists were significantly greater for Level I and II TCs than for Level III and IV TCs. Many Level II TCs offered on-call services that were equal to Level I TCs. We combined the response and verification costs for Level I and II centers into one grouping and Level III and IV centers into another grouping to best compare the baseline resources required for these 2 major groupings of TCs. Due to the wide variability in how TCs accounted for these expenditures, and the large differences in numbers of patients treated, we believed the most straightforward method for presentation was as the median and mean total cost of response and verification cost per patient treated.
RESULTS
Demographics and characteristics of trauma centers surveyed
Of the 69 TCs in the Arkansas Trauma System, 32 submitted clinical and financial data from 13,215 patients for the trauma financial survey. In total, 17,539 patients were included in the Arkansas Trauma Registry for the same time period as the study, and the Trauma Financial Survey included 75.3% of that total. There was participation by the following numbers of hospitals, by level of TC: Level I: n = 3, Level II: n = 5, Level III: n = 12, and Level IV: n = 12. In addition to the clinical and financial data on individual trauma patients, 27 hospitals were also able to submit detailed information for verification and response costs for the separate calculation of those expenditures. One hospital did not supply payment data on their patients. After those patients were excluded, along with other patients having only partial clinical or financial data, this left 11,175 patients to include in the patient cost portion of this study. With respect to those patients with an LOS ≥2 days, there were 5,426 patients, or 48.6% of the total patients treated, with complete data. Not surprisingly, Level I TCs in our system tended to have patients with higher mean ISS, higher mortality rates, and longer LOS than patients seen in Level II or Level III and IV TCs (Table 1).
Table 1.
Summary of Demographic, Medical, and Financial Characteristics of Patients Constituting the Entire Sample
| Level of TC | Patient care costs per patient, $ | Response and verification costs per patient, $ | Total cost per patient, $ | ISS | LOS, d | ICU days | Ventilator days | Age, y | Male, % | Mortality, % | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total cost | Payments | Margin | ||||||||||
| I (n = 2,332) | ||||||||||||
| Mean | 13,057 | 11,571 | (1,486) | 1,492 | 14,549 | 10.5 | 5.7 | 2.2 | 1.4 | 42.4 | 72 | 4.00 |
| SD | 23,457 | 30,823 | 22,498 | 647 | 24,104 | 10.0 | 10.3 | 6.4 | 6.0 | 18.6 | ||
| Median | 4,696 | 1,602 | (1,116) | 1,689 | 6,385 | 9.0 | 2.5 | 0 | 0 | 39.5 | ||
| II (n = 4,029) | ||||||||||||
| Mean | 8,758 | 10,020 | 1,262 | 1,492 | 10,250 | 8.5 | 4.3 | 1.6 | 0.7 | 50.4 | 59 | 3.70 |
| SD | 13,017 | 22,419 | 17,346 | 647 | 13,664 | 7.6 | 5.8 | 4.2 | 2.9 | 23.7 | ||
| Median | 4,426 | 4,358 | 50 | 1,689 | 6,115 | 5.0 | 2.7 | 0 | 0 | 51.0 | ||
| III and IV (n = 5,239) | ||||||||||||
| Mean | 5,201 | 3,817 | (1,384) | 636 | 5,837 | 6.3 | 2.2 | 0.4 | 0.2 | 48.9 | 54 | 2.00 |
| SD | 8,547 | 8,054 | 7,765 | 431 | 8,978 | 5.3 | 3.2 | 1.9 | 1.3 | 26.2 | ||
| Median | 2,394 | 1,091 | (443) | 450 | 2,844 | 4.0 | 1.1 | 0 | 0 | 51.0 | ||
Summaries are stratified by the level of trauma center at which a patient was treated. ISS, Injury Severity Score; LOS, length of stay; TC, trauma center.
Trauma center response and verification costs
Table 1 contains a summary of the costs for verification and response, PCC, along with other patient characteristics for the various levels of TC for all patients. For the 27 TCs reporting their costs, the total expense burden for both TC response and verification was $11,969,470, with Level I costs (2 reporting hospitals) of $4,397,224, Level II costs (5 reporting hospitals) of $5,102,454, and Level III and IV costs (20 hospitals) of $2,469,792.
Patient care costs
We empirically divided the patient cost data into 3 groups. All patients constituted the first group, regardless of LOS or ISS score. We then divided this group into 2 subgroups based on the LOS. Our attempt was to define and study a group of patients that could reasonably be expected to consume a major amount of hospital resources, representing the typical inpatient trauma patient. We empirically defined that typical inpatient group as those patients with an LOS of at least 2 days (defined as 48 hours) in the TC. Length of stay was calculated as the difference in total hours, beginning with the time and day of arrival to the emergency department and the time and day of discharge from the hospital. The prime analytic focus of this article is the comparison of the all-patient group with patients with a LOS of ≥2 days. The third group was defined as those patients with an LOS of <2 days (≤47 hours). We hypothesized that this latter group of patients was composed of two types of patients: those with minimal trauma and short emergency department or hospital stays and, conversely, another group that sustained major trauma and died quickly or survived to be transferred out to a higher level TC before 2 days. We will focus on this group of patients in a subsequent article.
Analysis of Trauma Financial Impact by level of trauma center and Injury Severity Score grouping
One option of viewing the TFI is to consider the overall financial effect on a TC based on the impact of all patients treated. We analyzed the financial metrics, patient characteristics, and potential cost drivers by the level of TC, comparing our two focus groups of patients. This analysis gives us a view into the TFI and allows us to see the typical patient treated at that level of TC for these 2 subsets of patients. We combined the patients treated at Level III and IV TCs into 1 level, as these TCs had smaller total patient volumes and tended to treat similar patients from the standpoint of severity of injury. By the same token, Level I and II TCs were analyzed separately to see if there were substantial differences on TFI or patient characteristics for these 2 types of TCs. Table 1 presents a summary of the demographic, medical, and financial characteristics for all patients in our sample, stratified by the level of TC in which they were treated.
For the entire sample, the TCs were found to differ with respect to ISS (p < 0.001, Kruskal-Wallis test), LOS (p < 0.001, Kruskal-Wallis test), the proportion requiring an ICU stay (p < 0.001, chi-square test) and the proportion requiring a ventilator (p < 0.001, chi-square test). For ISS, all of the TCs were found to be statistically different from one another (p < 0.0001 for all tests, Wilcoxon rank-sum tests; see Table 1). For LOS, however, the Level III/IV TCs differed from Level I (p < 0.001, Wilcoxon rank-sum tests) and Level II (p < 0.001), but the Level I and II TCs were not statistically different (p > 0.10). All 3 TCs differed from one another with respect to the proportion of patients requiring ICU (29.9% for Level I TC, 20.3% for Level II TC, and 6.7% for Level III/IV TC; p < 0.0001 for all pairwise comparisons). Similarly, all 3 TCs differed from one another with respect the proportion of patients requiring a ventilator (17.6% for Level I TC, 6.7% for Level II TC, and 2.1% for Level III/IV TC; p < 0.0001 for all pairwise comparisons). Patients with an LOS ≥2 days comprised roughly half of the total patients in the survey. When compared with patients with LOS ≥2 days, the costs for the entire sample were lower, but the mortality rates were higher. This is likely due to the short-stay patients (LOS <2 days) who were either mildly injured or who were severely injured and died shortly after being admitted. In both cases, these patients would be expected to consume fewer resources. Combining the median PCC for those patients with a LOS ≥2 days with the median verification and trauma response costs for those levels of TC treating these patients, we found that the per patient cost to treat this type of patient presenting to the TC is $15,401 for a Level I TC; $10,244 for a Level II TC; and $8,565 for the Level III and IV TCs (see Table 2).
Table 2.
Data for Levels of Trauma Center, for Patients with Length of Stay ≥2 Days
| Level of TC | Charges, $ | Payments, $ | Total estimated cost, $ | Margin, $ | Response and verification costs, $ | Total cost per patient, $ | ISS | LOS, d | ICU days | Ventilator days | Age, y | Male, % | Mortality, % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I (n = 1,177) | |||||||||||||
| Mean | 85,353 | 20,577 | 23,241 | (2,665) | 1,492 | 24,733 | 14.5 | 9.6 | 4.0 | 2.6 | 45.0 | 70.8 | 3.0 |
| SD | 131,480 | 41,083 | 29,164 | 30,925 | 647 | 29,811 | 10.1 | 12.3 | 8.3 | 8.1 | 18.8 | ||
| Median | 47,782 | 8,385 | 13,712 | (3,640) | 1,689 | 15,401 | 12.0 | 5.9 | 1.0 | 0.0 | 43.0 | ||
| II (n = 2,313) | |||||||||||||
| Mean | 54,251 | 14,882 | 13,515 | 1,368 | 1,492 | 15,007 | 9.6 | 6.8 | 2.7 | 1.2 | 56.0 | 53.6 | 1.7 |
| SD | 60,622 | 27,782 | 15,296 | 22,263 | 647 | 15,943 | 7.4 | 6.5 | 5.1 | 3.8 | 22.2 | ||
| Median | 34,254 | 7,837 | 8,555 | 22 | 1,689 | 10,244 | 9.0 | 4.7 | 0.0 | 0.0 | 57.0 | ||
| III and IV (n = 1,950) | |||||||||||||
| Mean | 30,420 | 7,784 | 10,719 | (2,935) | 636 | 11,355 | 7.1 | 5.0 | 0.9 | 0.3 | 60.8 | 43.9 | 1.6 |
| SD | 32,403 | 11,412 | 11,827 | 11,870 | 431 | 12,258 | 5.2 | 3.8 | 2.8 | 2.0 | 21.9 | ||
| Median | 23,752 | 6,584 | 8,115 | (1,147) | 450 | 8,565 | 5.0 | 3.9 | 0.0 | 0.0 | 63.0 | ||
ISS, Injury Severity Score; LOS, length of stay; TC, trauma center.
Trauma Financial Impact by Injury Severity Score and level of trauma center
We reasoned that resource consumption in patients with an LOS 2+ days would be proportional to LOS, ICU days, or ventilator days and that the best approach to test that hypothesis would be to analyze patients according to traditional groupings of ISS scores. We divided those patients with a LOS of 2+ days into 5 groups: 2 groups with ISS score categories of 0 to 8 (minor trauma) and 9 to 75 (major trauma), plus 3 additional groupings of 9 to 15, 16 to 24, and ≥25. We then analyzed each group, ignoring the level of TC at which they were treated. Patient demographics, mortality, LOS, ICU days, and ventilator days were also analyzed for these 5 groups, giving us a look at the typical patient in each group. Lastly, we analyzed the 4 groupings of ISS scores, 0 to 8, 9 to 15, 16 to 25, and ≥25, by the level of TC delivering care, to better understand the patient and financial dynamics within each level of TC. Similar to the TC-level analysis noted here, we combined the patients from Level III and Level IV TCs into 1 group for analysis. The impact of ISS scores on TFI and the associated patient characteristics that might be drivers of cost are shown in Table 3. We found that median costs for those patients with an LOS ≥2 days rose with increasing ISS. The LOS, ICU days, and ventilator days also increased with increasing ISS scores. Charge, cost, payment, and total margin data, along with these potential drivers of cost, are shown in Table 3.
Table 3.
Data for Injury Severity Score Groups: All Patients with Length of Stay ≥2 Days
| ISS and LOS | Charges, $ | Total estimated cost, $ | Payments, $ | Margin, $ | Level of TC | ISS | LOS, d | ICU days | Ventilator days | Age, y | Male, % | Mortality, % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ISS <9, LOS 2+ d, “minor trauma” (n = 2,463) | ||||||||||||
| Mean | 30,056 | 8,827 | 7,646 | (1,181) | 2.37 | 4.06 | 4.79 | 0.58 | 0.19 | 58.29 | 46.1 | 1.0 |
| SD | 25,968 | 8,165 | 11,575 | 10,483 | 0.72 | 1.52 | 3.61 | 1.68 | 1.22 | 22.17 | ||
| Median | 23,375 | 6,787 | 5,323 | (550) | ||||||||
| ISS 9+, LOS 2+, “major trauma” (n = 2,978) | ||||||||||||
| Mean | 70,942 | 19,404 | 18,467 | (937) | 1.99 | 14.47 | 8.44 | 3.56 | 1.98 | 52.92 | 60.2 | 2.8 |
| SD | 99,037 | 23,325 | 35,082 | 27,790 | 0.77 | 7.95 | 9.52 | 6.92 | 6.27 | 21.87 | ||
| Median | 41,683 | 11,961 | 10,000 | (1,230) | ||||||||
| ISS 9–15, LOS 2+ (n = 2,031) | ||||||||||||
| Mean | 49,829 | 14,340 | 13,398 | (942) | 2.14 | 10.18 | 6.43 | 1.74 | 0.66 | 55.6 | 55.1 | 1.4 |
| SD | 23,963 | 18,395 | 15,516 | 22 | 0.77 | 1.75 | 6.06 | 3.82 | 2.74 | 21.8 | ||
| Median | 34,357 | 10,390 | 9,588 | (817) | ||||||||
| ISS 16–24, LOS 2+ (n = 593) | ||||||||||||
| Mean | 87,649 | 23,615 | 22,299 | (1,316) | 1.72 | 18.80 | 10.11 | 4.80 | 2.48 | 47.34 | 71.5 | 1.9 |
| SD | 83,502 | 21,883 | 36,987 | 30,253 | 0.69 | 2.38 | 8.07 | 5.95 | 4.77 | 20.53 | ||
| Median | 57,937 | 15,698 | 9,339 | (3,319) | ||||||||
| ISS 25+, LOS 2+ (n = 354) | ||||||||||||
| Mean | 164,092 | 41,407 | 41,132 | (275) | 1.56 | 31.82 | 17.12 | 9.81 | 7.54 | 47.11 | 70.3% | 11.9 |
| SD | 203,284 | 41,621 | 63,885 | 54,967 | 0.65 | 8.19 | 18.43 | 12.67 | 13.36 | 21.76 | ||
| Median | 106,468 | 29,792 | 15,896 | (4,893) | ||||||||
ISS, Injury Severity Score; LOS, length of stay; TC, trauma center.
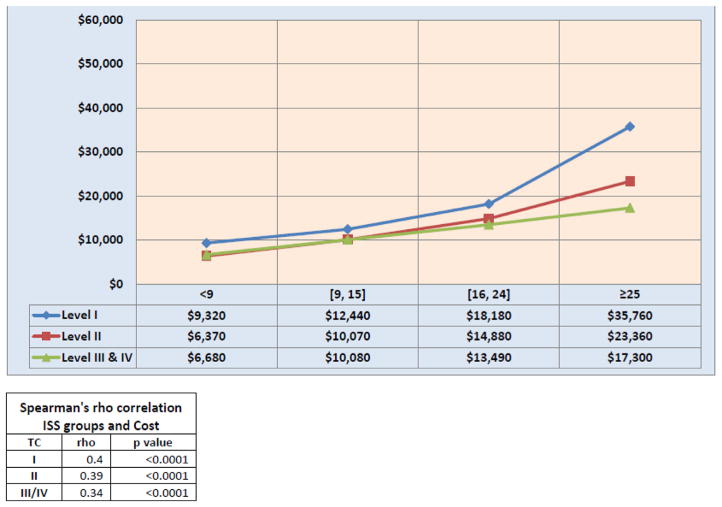
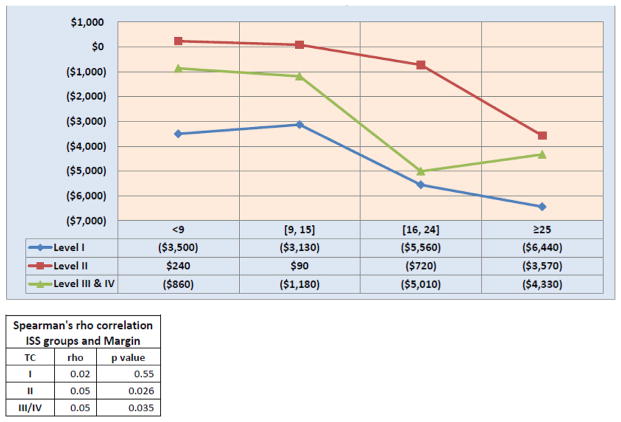
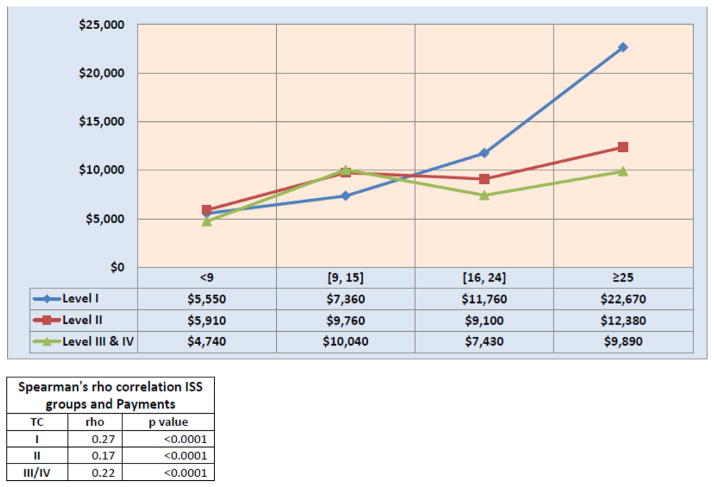
Next, we examined the association between ISS and various financial characteristics (ie, total estimated cost, payment, and margin) for patients with LOS ≥2 days. Separate analyses were performed for each TC level. For ease of presentation, we grouped ISS values into one of the following classes: 0 to 8, 9 to 15, 16 to 24, or 25+. Because of the wide range of costs, payments, and margins in these smaller groups of patients, we chose to show the median, interquartile ranges (25th and 75th percentiles), and mean values for those variables, with the results displayed in Table 4; median values of these same data are shown graphically in Figures 1 to 3. For each TC level, we found strong positive correlations between ISS and charges (p < 0.0001), payments (p < 0.0001), and total estimated costs (p < 0.0001). There was weak evidence of an association between ISS and margin for Level II TC (p = 0.026) and Level III/IV TC (p = 0.035), but there was no evidence of an association for Level I TC (p > 0.55).
Table 4.
Data for Injury Severity Score Groups: All Patients with Length of Stay ≥2 Days, by Level of Trauma Center Treatment
| Trauma center | Charges, $
|
Estimated costs, $
|
Payments, $
|
Total margin, $
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | 25th %tile | Median | 75th %tile | Mean | 25th %tile | Median | 75th %tile | Mean | 25th %tile | Median | 75th %tile | Mean | 25th %tile | Median | 75th %tile | |
| Level I | ||||||||||||||||
|
| ||||||||||||||||
| ISS <9 | 41,830 | 19,600 | 29,550 | 57,340 | 12,210 | 5,880 | 9,320 | 15,350 | 8,240 | 0 | 5,550 | 10,930 | (3,960) | (8,280) | (3,500) | 670 |
|
| ||||||||||||||||
| ISS 9–15 | 63,120 | 23,170 | 40,040 | 72,450 | 18,230 | 7,230 | 12,440 | 22,850 | 14,510 | 0 | 7,360 | 16,990 | (3,730) | (10,510) | (3,130) | 3,250 |
|
| ||||||||||||||||
| ISS 16–24 | 90,450 | 36,270 | 63,520 | 114,790 | 25,680 | 8,820 | 18,180 | 37,420 | 23,130 | 0 | 11,760 | 30,230 | (2,550) | (14,050) | (5,560) | 7,080 |
|
| ||||||||||||||||
| ISS 25+ | 200,380 | 66,020 | 134,900 | 235,130 | 49,320 | 15,820 | 35,760 | 69,010 | 51,050 | 7,170 | 22,670 | 58,820 | 1,730 | (23,980) | (6,440) | 18,000 |
|
| ||||||||||||||||
| Level II | ||||||||||||||||
|
| ||||||||||||||||
| ISS <9 | 33,090 | 16,400 | 25,770 | 40,870 | 8,340 | 3,700 | 6,370 | 10,250 | 9,220 | 3,360 | 5,910 | 10,680 | 880 | (3,110) | 240 | 2,630 |
|
| ||||||||||||||||
| ISS 9–15 | 55,650 | 26,180 | 41,110 | 65,070 | 13,980 | 6,090 | 10,070 | 16,330 | 16,000 | 3,990 | 9,760 | 16,400 | 2,020 | (5,860) | 90 | 4,590 |
|
| ||||||||||||||||
| ISS 16–24 | 94,250 | 31,060 | 64,930 | 127,510 | 22,800 | 7,130 | 14,880 | 32,390 | 24,370 | 370 | 9,100 | 22,090 | 1,570 | (12,550) | (720) | 8,520 |
|
| ||||||||||||||||
| ISS 25+ | 131,850 | 42,990 | 96,910 | 189,590 | 32,740 | 10,040 | 23,360 | 46,780 | 33,400 | 720 | 12,380 | 36,760 | 660 | (18,700) | (3,570) | 12,030 |
|
| ||||||||||||||||
| Level III–IV | ||||||||||||||||
|
| ||||||||||||||||
| ISS <9 | 24,320 | 12,040 | 20,010 | 30,090 | 8,480 | 4,020 | 6,680 | 10,070 | 6,010 | 470 | 4,740 | 9,160 | (2,480) | (5,330) | (860) | 1,380 |
|
| ||||||||||||||||
| ISS 9–15 | 34,720 | 19,110 | 27,870 | 41,930 | 12,310 | 6,910 | 10,080 | 14,110 | 9,700 | 3,530 | 10,040 | 11,990 | (2,610) | (6,720) | (1,180) | 2,250 |
|
| ||||||||||||||||
| ISS 16–24 | 55,520 | 26,920 | 42,970 | 62,250 | 19,880 | 9,030 | 13,490 | 22,200 | 12,390 | 0 | 7,430 | 23,530 | (7,480) | (13,490) | (5,010) | 3,030 |
|
| ||||||||||||||||
| ISS 25+ | 88,840 | 20,490 | 42,920 | 107,080 | 32,250 | 7,860 | 17,300 | 31,710 | 15,820 | 1,500 | 9,890 | 16,200 | (16,430) | (18,620) | (4,330) | 700 |
ISS, Injury Severity Score; LOS, length of stay; TC, trauma center.
Figure 1.
Median costs by level of trauma center (TC) and Injury Severity Score (ISS) groups, patients with length of stay ≥2 days.
Figure 3.
Median margin by level of trauma center (TC) and Injury Severity Score (ISS) groups, patients with length of stay ≥2 days.
These results are presented in Tables within Figures 1 to 3.
DISCUSSION
When a hospital takes the steps necessary to become a verified TC, is this decision a financial boon or a disaster for the hospital? What are the costs of becoming and maintaining the standards of a TC? Is the financial impact equal among all TCs, or is there a difference between the various levels of TC? And, what are the potential drivers of cost for trauma patients, and what impact might they have on the total margin for care of a trauma patient? These questions are just some of many that spurred the state of Arkansas in 2010 to invest in studying the TFI on hospitals that were becoming TCs. These questions are not new. Almost 25 years ago, 3 young surgeons named Eastman, Rice, and Richardson, explored the same territory.4 The existing literature about costs associated with TC care, although well done and intriguing, still provides few, if any, answers to these questions, due to the difficulty of getting complete and accurate financial data.5–21 The success or failure of our trauma systems as a whole might hinge on the answers, particularly if financial support was inadequate or mismatched to meet the needs of TCs for long-term sustainability. We believe that we have found some answers to these questions in the rich data that our survey has gathered.
Lessons learned: hospital financial survey methodology
We gained substantial knowledge about the conduction of a large-scale hospital financial survey and the methodology on how to adjust/analyze the data to allow meaningful comparisons between TCs. One of our advantages was the robust participation of our TCs by sharing their cost and patient data. This is in marked contrast to other states, where there has not been this level of transparency. This lack of transparency was recently noted by Tepas and colleagues,5 in the discussion of their 2013 American Association for the Surgery of Trauma plenary paper dealing with effects of unregulated promulgation of TCs: “One of the reasons there is no data for comparison is that the other institutions will not share their data.” The development of the Arkansas Trauma System in 2009 allowed regulation of TC development in our state, careful evaluation of outcomes across the multiple levels of trauma care, and an infrastructure that enables and encourages this type of essential research. Another important lesson gained was to identify the wide variability of hospital financial accounting from one center to another and to understand how this variability can influence the financial results of any survey, if not properly refined. In retrospect, this survey would never have been completed, or completed with major discordance in findings, had we not had the aid and assistance of an accounting and consulting firm with the deep knowledge base and expertise that they brought to the survey. The survey took longer than anticipated to complete due primarily to the task of matching and then aligning the various TC departmental expenses reported. Additionally, accounting for the various employment models, call pay structures, and physician financial support programs added another layer of complexity to the accounting of PCC, trauma response, and verification costs. Many hospitals had relatively simple accounting structures, perfectly suitable for their smaller size, but complicating the task of teasing out the important details of cost-accounting necessary for this study. These data all had to be rectified into a common cost structure by hospital department, so that we could account and compare costs across the TCs participating in the survey without either double counting or missing expenses. We believed that having each hospital’s cost calculated by using the CCR at the departmental cost level was an advantage in accuracy compared with having to rely on formulaic estimates of cost or using the CCR of the MCR at the state level.5–7 Large hospitals had much more sophisticated cost accounting processes in place, and they regularly estimate costs internally. We used those centers’ internal cost data to test the reasonableness of the adjusted MCR estimated costs used in this study. The variances ranged from <2% to 14%, and we believed this supported the methodology we used to estimate cost as being reasonable and accurate.
Another important lesson gained was the benefit of having a uniform, statewide trauma registry from which to glean patient information. The American College of Surgeons Trauma Registry dataset is a rich collection of clinical information that was extremely useful in this survey by allowing us to correlate the impact of clinical events on expenses. Having the trauma registry located in one data collection center also allowed us to ensure uniform integrity of the data collected and simplified reporting and collation of the data for the survey. The trauma registry’s inclusion of both Abbreviated Injury Scores and ISS allowed us to avoiding calculating ISS scores from ICD-9 diagnosis codes.7–9 Similarly, we were able to avoid relying on a statistical sampling technique for the survey, which had been used by others to sample only some of the patients.6,7 Instead, we were able to link every patient’s financial data (submitted by the TCs) with the data on that same patient collected in the trauma registry using the Arkansas trauma band ID number assigned to each patient.
Trauma center response and verification costs
The cost encumbered by a TC goes beyond just the PCC. There are also costs associated with maintaining an accurate trauma registry that is up to date, a vigorous performance improvement plan in place, and a trained team of experts and resources available to quickly treat injured patients.14 Too often these costs are ignored, discounted, or subsumed within the existing cost structure of a TC and therefore go unappreciated as to their magnitude. As displayed in Tables 1 and 2, we found that the decision to become a TC adds roughly $1,500 of additional costs per patient for Level I and II TCs and $600 for Level III and IV TCs, beyond any PCC. The differences in costs between these two groupings of TC were largely driven by two factors: the additional costs of specialists required to be on call for the upper levels of TC and the infrastructure costs of a TC, driven by the costs for dedicated nurses and trauma registry coordinators that increases proportionally with the volume of trauma patients treated. In some states, trauma response cost is offset by insurance payments for a trauma activation fee, but in the case of Arkansas’s hospitals, as a general rule, trauma activation fees have not been reimbursed by insurance carriers.5,18,22 The Arkansas Trauma System provides infrastructure support for the TCs in the system, through a grant mechanism, but this support falls far short of matching the actual costs of trauma response and verification.
Patient care costs relationship to Injury Severity Score, length of stay, intensive care unit, and ventilator days
There was a direct relationship between ISS levels and the costs required to care for the patients with an LOS ≥2 days (Tables 2 to 4); this finding was not unexpected and was similar to other studies.11–13,15–17 There was also an increased cost for patient care as the level of TC increased from Levels III and IV to Levels I and II. This increased cost was proportional to the increased resources consumed as reflected in the mean ISS of the patients treated at the various centers, along with increased LOS, ICU, and ventilator days. The increased costs rose along with the mean ISS. We found that Level III and IV TCs had the occasional patient with high levels of ISS that stayed ≥2 days, but more commonly, these TCs transferred the badly injured patients on to Level I and II TCs. The typical levels of ISS, LOS, ICU, and ventilator days were the greatest in Level I and II TCs. The increased cost of caring for the most injured patients fell largely on the upper two levels of TCs, particularly the Level I TCs. However, this increased cost was not offset by increased payment, resulting in an increasing net-negative median margin for those TCs treating patients with higher ISS (Table 2). Our findings are in contrast to those of Taheri and colleagues,20 who showed an increasing positive margin with increased levels of trauma. However, 95% of the population they treated had some form of insurance coverage, therefore, influencing the positive financial outcomes. Breedlove and colleagues18 also found that net margin was increased in the more severely injured patients admitted to their TC. However, close inspection of their study revealed that their hospital in Ohio received trauma activation fees, and our hospitals in Arkansas typically receive no, or infrequent, payment for trauma activation. This is an important finding and points out the important positive effect that payment of a trauma activation fee has on TCs to support their ability to care for trauma patients. Without trauma activation fees, the financial costs of participating in a trauma system fall on the general revenues of the hospital. Our study demonstrates that this cost is substantial.
Analysis of the data for patients with an LOS ≥2 days by ISS grouping and by levels of TC gives more insight into the financial impact of caring for trauma patients, particularly cost drivers. Table 4 and Figures 1 to 3 display this cumulative information by level of TC and by ISS grouping. Median cost of patient care treatment for each group of ISS was consistently higher for Level I TCs than for the other levels. Although payments were higher for Level I TCs than the other levels of TC, their PCC were higher and resulted in a more negative median net margin. Level II TCs did have several patients with high charges and payments, which resulted in more patients with very positive net margins, that influenced the total net margin for Level II hospitals. This can be seen in Table 4, where the mean values for payment are considerably higher than the median values. Figures 1 to 3 display a graphic representation of these data, showing the median cost, payments, and margin for each ISS grouping by level of TC.
Comparing the data in Tables 1 to 4 shows the potential negative impact of TCs dropping out of the trauma system. The net margin is more negative in the subset of patients with longer LOS and in those with higher ISS (Tables 2 to 4). However, adding in equal numbers of patients with shorter LOS and lower ISS (Table 1) improves the net margin for each level of TC across the board. This finding agrees with that of Fakhry and colleagues,15,17 who noted a direct relationship of LOS with increased cost, and resonates with that of Rutledge and colleagues,21 who found that referral of very sick trauma patients out of rural hospitals to major centers would likely improve the margin of the smaller hospitals. This is relevant to the trauma system itself and speaks to the positive impact of wide participation of hospitals in any trauma system. If hospitals drop out of the system due to poor financial support, the patients that will have a greater net-negative margin effect will be funneled into the remaining upper level TCs, worsening their financial burden.19 Assuming that a hospital drops out of the trauma system and continues to treat the less injured, but sends the most severely injured patients to the higher level of TC, the effect would be to improve the net margin of the non-TCs and worsen the net margin of the higher-level TC. This is clearly due to the shifting of the higher cost and higher negative-net margin patients to the remaining hospitals participating as TCs. Wide participation of hospitals in a trauma system has other potential beneficial effects, in that the burden of treating the more severely injured is spread evenly across our state and not shunted to just a few TCs. It is our general belief that there is no obvious “wallet biopsy” that influences referrals to another TC, but this is an area of additional research and review that is planned to test our assumption. The summary conclusion of our work is that it is critical to understand the TFI on TCs so that we can properly argue for adequate financial support to sustain both TCs and the trauma system as a whole.
Strengths and weaknesses
Our study benefited from the overall design of the Arkansas Trauma System, as well as the cooperation of the participating TCs and the Arkansas Department of Health. However, we caution that the discussed results are a top-level view of a large quantity of data that are still undergoing additional examination and analysis. For instance, as a “first-view” approach to the data, we arbitrarily chose to look at all patients with an LOS of ≥2 days as one group of patients. The results of a positive or negative margin might not be the same if we were to parse out the data by LOS, as Fakhry and colleagues15,17 have done. By the same token, we divided the ISS levels into 4 groups, but the cost, payment, and margin might turn out to be quite different for patients with very high ISS vs those with an ISS of 9, which was the threshold for our “major trauma” designation. We clearly need to delve into complex patients to more fully understand their cost drivers, not just by ISS, but by major types of trauma leading to the higher ISS levels. Lastly, as for the verification and response costs, the reporting of these expenses as separate items by a TC is a relatively new experience and is nonuniform from one TC to another. We are concerned that some expenses that could be legitimately charged to these two areas might have been under-reported or even missed. Our plan to remedy these concerns is to conduct a follow-up survey of these specific costs in conjunction with the Arkansas Hospital Association and the Arkansas Department of Health, to better understand and assure a proper accounting of the cost of verification and trauma response.
CONCLUSIONS
We have found that our methodology of applying a uniform technique of surveying, use of the MCR and CCR for estimation of cost, and inclusion of the statewide trauma registry provides data that are quite helpful in understanding the TFI and drivers of cost for treatment of the trauma victim. We determined that estimated cost of care rose with increasing levels of ISS, LOS, ICU days, and ventilator days, particularly for patients with LOS ≥2 days and ISS 9+. Taking all patients admitted, Level I TCs had the highest mean ISS, LOS, ICU days, and ventilator days, along with the highest PCC. Lesser degrees of trauma accounted for lower charges, payments, and PCC for Level II, III, and IV TCs, and the margin was variable. Verification and response costs per patient were highest for Level I and II TCs. Determination of TFI across a state system using a novel methodology offers the opportunity to better understand the drivers of TFI, determine the lowest cost per best outcomes for a given level and type of trauma, and better allocate scarce resources within a TC and across a trauma system.
Discussion
DR RONALD M STEWART (San Antonio, TX): First, I congratulate you and your team of authors for (in the span of 5 short years) building a robust and growing trauma system for the citizens of Arkansas. It is clear that the Arkansas system was designed and implemented with great foresight, which laid the groundwork for this paper, and I am sure many to come. I congratulate the surgeons of Arkansas for both leading and working together so successfully.
Getting right to the bottom line: Net margin or profit essentially falls with increasing severity of injury and is worst at the level I trauma center. If there is a “sweet spot” with respect to profitability from Arkansas, it rests with level II trauma centers, the only group of trauma centers with a positive median net margin. I have 4 questions for you:
Because there are large variations in state payer mix and funding methods, do you believe these results are generalizable to other states or the country as a whole?
Did net margin take into account other nonpatient care revenue, such as local property taxes and state programs to offset the care of trauma patients without health care coverage?
Did you examine, or do you plan to examine, the impact of blunt vs penetrating trauma or direct transport patients vs inter-hospital transfer patients?
There are clearly many reasons why hospitals and their surgeons want to be a trauma center. Level I trauma centers are specifically responsible for and charged with development of future leaders and research, but clearly, are the least profitable. How do you propose to encourage the level I trauma centers in Arkansas to continue as healthy, financially viable trauma centers? As a corollary, how do you keep all hospitals from aspiring to become level II trauma centers?
DR SAMIR FAKHRY (Charleston, SC): Let me start by first congratulating the authors on taking on the always daunting task of understanding the costs associated with the care we deliver, trauma care included. Because of the way our health care system is designed, or rather distorted, determining the actual cost of any particular service or encounter ranks among the great mysteries of American health care. At a time in our history when we are inching ever closer to the cure for cancer, breaking down the complexities of the inflammatory response, and finally resolving the debate about crystalloids and colloids (in favor of crystalloids), we are still challenged to answer the seemingly simple question of what something costs in health care.
To illustrate the point, at a recent meeting with the Centers for Medicare and Medicaid Services, none of us could answer the ostensibly simple question, “What does a trauma activation cost?” Of course, that matters, as payers would like to reimburse relative to costs. Absent that information, it is difficult to justify the wide variation in charges for services, such as the trauma activation fees that have been reported. No business would accept that as part of their business model because it not only interferes with accurate profit and loss assessments but also undermines market valuations and negotiations with purchasers of those services. This will only be exaggerated in the evolving world of value-based purchasing.
Trauma care stakeholders in Arkansas were presented with a unique opportunity to evaluate the trauma financial impact of trauma centers and a trauma system. I suggest that similar efforts in other specialties are needed. I have a few comments and questions for the authors.
As you point out in the discussion in the manuscript, a major accomplishment of this work is convincing a large group of centers to share their financial data and developing a methodology that combines the disparate source data into a single dataset that can be meaningfully analyzed. Congratulations on accomplishing that feat. Was the guarantee of confidentiality the prime driver for that process? What other elements contributed to that success?
I also commend you on implementing the Arkansas Trauma Band ID Number. Do you plan to use that resource to study other important post-discharge outcomes of trauma care besides financials, such as 6- and 12-month survival, mental health/post-traumatic stress disorder prevalence, functional status, and return to work?
Even with your extensive efforts, you continue to refer to “estimated costs.” Did you include both direct and indirect costs in your calculations? If you included both, how did you correct for the variation in attributable indirect costs that occur because of different cost accounting systems at different hospitals?
You describe removing the costs associated with trauma activation from the Medicare Cost Report. What are those costs and how did you select them? We have struggled to find a uniformly applicable methodology to accomplish that over a large number of centers.
In Table 4 in the manuscript, you show that the mean estimated costs, charges, and payments are approximately twice as high as the respective medians. This suggests that there is a small outlier population that has high associated costs and charges. In a paper we presented at the 2012 meeting of this Association, we determined that population to be the Medicare-age patient with multiple comorbidities and ICU stays of greater than 10 days. If that was your experience and with that population expected to grow dramatically, should we be working on contracting strategies that allow us to recoup the high outlier costs of this population instead of accepting Diagnosis-Related Group-based or capitated payments based on our mean estimated costs?
Figure 2.
Median payments by level of trauma center (TC) and Injury Severity Score (ISS) groups, patients with length of stay ≥2 days.
Acknowledgments
Support: This study was funded by grants from the Blue & You Foundation for a Healthier Arkansas, the Arkansas Department of Health, and the Arkansas Hospital Association. This study was also supported, in part, by the Translational Research Institute (TRI), grant UL1TR000039 through the NIH National Center for Research Resources and National Center for Advancing Translational Sciences.
Abbreviations and Acronyms
- CCR
cost-to-charge ratio
- ISS
Injury Severity Score
- LOS
length of stay
- MCR
Medicare Cost Report
- PCC
patient care costs
- TC
trauma center
- TFI
Trauma Financial Impact
Footnotes
Disclosure Information: Nothing to disclose.
Presented at the Southern Surgical Association 126th Annual Meeting, Palm Beach, FL, November 30–December 3, 2014.
Author Contributions
Study conception and design: Mabry, Maxson
Acquisition of data: Mabry, Spencer
Analysis and interpretation of data: Mabry, Kalkwarf, Betzold, Spencer
Drafting of manuscript: Mabry, Kalkwarf, Betzold, Spencer, Robertson, Sutherland, Maxson
Critical revision: Mabry, Kalkwarf, Betzold, Spencer, Robertson, Sutherland, Maxson
References
- 1.Healthy Arkansas. American College of Surgeons Trauma Systems Consultation of the Arkansas Trauma System. Little Rock, AR: 2011. [Accessed August 3, 2014]. Available at: http://www.healthy.arkansas.gov/programsServices/injuryPreventionControl/TraumaticSystems/Documents/trauma/Reports/ARFinalACSReport.pdf. [Google Scholar]
- 2.Healthy Arkansas. Arkansas Trauma Registry. Little Rock, AR: [Accessed August 31, 2014]. Available at: http://www.healthy.arkansas.gov/programsServices/healthStatistics/Pages/TraumaRegistry.aspx. [Google Scholar]
- 3.Healthy Arkansas. Arkansas Trauma Registry Data Dictionary. Little Rock, AR: 2014. [Accessed August 31, 2014]. Available at: http://www.healthy.arkansas.gov/programsServices/healthStatistics/Documents/Trauma/ArkansasTraumaDataGuide.pdf. [Google Scholar]
- 4.Eastman AB, Rice CL, Bishop G, Richardson JD. An analysis of the critical problem of trauma center reimbursement. J Trauma. 1991;31:920–925. doi: 10.1097/00005373-199107000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Tepas JJ, Kerwin AJ, Ra JH. Unregulated proliferation of trauma centers undermines cost efficiency of population-based injury control. J Trauma Acute Care Surg. 2014;76:576–581. doi: 10.1097/TA.0000000000000125. [DOI] [PubMed] [Google Scholar]
- 6.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. The national study on costs and outcomes of trauma. J Trauma. 2007;63(Suppl):S54–S67. doi: 10.1097/TA.0b013e31815acb09. [DOI] [PubMed] [Google Scholar]
- 7.Glance LG, Dick AW, Osler TM, et al. The association between cost and quality in trauma: is greater spending associated with higher-quality care? Ann Surg. 2010;252:217–222. doi: 10.1097/SLA.0b013e3181e623f6. [DOI] [PubMed] [Google Scholar]
- 8.Ceslo B, Tepas J, Langland-Orban B, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60:371–378. doi: 10.1097/01.ta.0000197916.99629.eb. [DOI] [PubMed] [Google Scholar]
- 9.Durham R, Pracht E, Orban B, et al. Evaluation of a mature trauma system. Ann Surg. 2006;243:775–785. doi: 10.1097/01.sla.0000219644.52926.f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rogers FB, Osler T, Shackford SR, et al. Charges and reimbursement at a rural level I trauma center: a disparity between effort and reward among professionals. J Trauma. 2003;54:9–14. doi: 10.1097/00005373-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Taheri PA, Wahl WL, Butz DA, et al. Trauma service cost: the real story. Ann Surg. 1998;227:720–725. doi: 10.1097/00000658-199805000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taheri PA, Butz DA, Greenfield LJ. Paying a premium: how patient complexity affects costs and profit margin. Ann Surg. 1999;229:807–811. doi: 10.1097/00000658-199906000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lanzarotti S, Cook CS, Porter JM, et al. The cost of trauma. Am Surg. 2003;69:766–770. [PubMed] [Google Scholar]
- 14.Rotondo MF, Bard MR, Sagraves SG, et al. What price commitment: what benefit? The cost of a saved life in a developing level I trauma center. J Trauma. 2009;67:915–923. doi: 10.1097/TA.0b013e3181b848e7. [DOI] [PubMed] [Google Scholar]
- 15.Fakhry SM, Couillard D, Liddy CT, et al. Trauma center finances and length of stay: identifying a profitability inflection point. J Am Coll Surg. 2010;210:817–823. doi: 10.1016/j.jamcollsurg.2010.01.030. [DOI] [PubMed] [Google Scholar]
- 16.Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. 2005;33:1266–1271. doi: 10.1097/01.ccm.0000164543.14619.00. [DOI] [PubMed] [Google Scholar]
- 17.Fakhry SM, Martin B, Al Harakeh H, et al. Proportional costs in trauma and acute care surgery patients: dominant role of intensive care unit costs. J Am Coll Surg. 2013;216:607–614. doi: 10.1016/j.jamcollsurg.2012.12.031. [DOI] [PubMed] [Google Scholar]
- 18.Breedlove LL, Fallon WF, Cullado M, et al. Dollars and sense: attributing value to a level I trauma center in economic terms. J Trauma. 2005;58:668–673. doi: 10.1097/01.ta.0000159240.39354.96. [DOI] [PubMed] [Google Scholar]
- 19.Newgard CD, Staudenmayer K, Hsia RY, et al. The cost of overtriage: more than one-third of low-risk injured patients were taken to major trauma centers. Health Aff. 2013;32:1591–1599. doi: 10.1377/hlthaff.2012.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taheri PA, Butz DA, Watts CM, et al. Trauma services: a profit center? J Am Coll Surg. 1999;188:349–354. doi: 10.1016/s1072-7515(99)00021-6. [DOI] [PubMed] [Google Scholar]
- 21.Rutledge R, Shaffer VD, Ridky J. Trauma care reimbursement in rural hospitals: implications for triage and trauma system design. J Trauma. 1996;40:1002–1008. doi: 10.1097/00005373-199606000-00025. [DOI] [PubMed] [Google Scholar]
- 22.Fakhry SM, Potter C, Crain W, Maier R. Survey of national usage of trauma response charge codes: an opportunity for enhanced trauma center revenue. J Trauma. 2009;67:1352–1358. doi: 10.1097/TA.0b013e3181c3fdd4. [DOI] [PubMed] [Google Scholar]