Abstract
Context
Climate change adaptation strategies that address locally specific climate hazards are critical for preventing negative health outcomes, and local public health officials are key foci for adaptation planning.
Objective
To assess New York State Local Health Department officials’ perceptions and preparedness related to climate-sensitive health areas, and compare these with a national sample.
Design
Online survey instrument, originally used in a national survey of Local Health Department (LHD) officials.
Setting
New York State
Participants
Eligible participants included all New York State city and county LHD officials, one respondent per LHD.
Main Outcome Measures
LHD officials’ perceptions of local 1) climate-related public health effects, 2) preparation status and programming areas of LHDs, and 3) necessary resources to better address climate-related health risks.
Results
Survey participants, representing a 54% response rate (with 93% of respondents completing more than 90% of the questions), perceived climate change as relevant to public health, and most noted that some of their existing programs already use or are planning to use climate adaptation strategies. Overall, fewer New York State respondents identified concerns or related expertise compared to the previous national survey. Many respondents expressed uncertainty regarding necessary additional resources.
Conclusions
This type of assessment makes clear the high variability in perceived impacts and capacity at the level of local health department jurisdictions, and underscores the importance of sustained support for local climate change preparedness programming. The implications of these findings are germane to other states with similar decentralized jurisdiction of public health. Findings from such surveys can bolster existing LHD programs, as well as inform long-term and emergency planning for climate change.
Introduction
Effects of climate change are already being experienced across the globe and current concentrations are sufficiently high that some impacts can be expected to continue over the next fifty years, even under the most aggressive greenhouse gas emissions reduction strategies.1,2 Consequently, there has been a growing emphasis on climate change adaptation, particularly in the area of human health where the magnitude of risks will depend largely on population and infrastructure preparedness and anticipation of vulnerable groups,3–5 balanced against regionally variable weather and climate change impacts.6 Thus, strategies that specifically address local climate hazards in conjunction with vulnerability factors are critical for preventing negative health outcomes and local public health officials are key foci for adaptation planning.7–9
New York State contains a wide range of human and natural systems, with a correspondingly broad array of vulnerabilities to climate change impacts across the state.10 A recent assessment of regional climate change10 found that mean temperatures are extremely likely to increase across the State over the coming century, as well as probable increases in extreme heat events, coastal flooding, extreme precipitation, and drought. This range of climatic shifts, combined with the diversity of the State’s environment, pose distinct preparedness challenges for local health departments (LHD). Furthermore, New York State’s public health system is decentralized such that programming authority rests at the local level, making LHD officials’ perceptions of threats, needs and capacity critical to effective adaptation planning and funding allocation at the state level.
In an effort to identify regionally- and locally-specific mitigation and adaptation challenges, the New York State Climate Action Council was formed by Executive Order in 2009 with the mandate to conduct a statewide climate change adaptation assessment.11 Additionally, the New York State Energy Research and Development Authority (NYSERDA) funded the Integrated Assessment for Effective Climate Change Adaptation Strategies in New York State, known as ClimAID, which brought together researchers and stakeholders from multiple fields such as energy, transportation, agriculture, water, and public health to identify local vulnerabilities and suggest effective policy and preparedness strategies.10 This study was carried out to complement regional public health sector analysis, including input from local government and community stakeholders.12
While climate change impacts and adaptation strategies are discussed widely in public health literature, there was relatively little work on understanding local public health officials’ climate change perceptions and preparedness in the United States. One exception is the 2007 “Are We Ready” survey of members of the National Association of County and City Health Officials (NACCHO) conducted by George Mason University's Center for Climate Change Communication and the Environmental Defense Fund.13,14 The results of that national sample demonstrated widespread perception of climate change as a current and future threat to public health, but one for which most local public health departments (LHDs) did not yet have a specific adaptation or prevention programs. These survey results echo findings of insufficient funding for and prioritization of climate change on the national policy-making agenda.15
In the present study, we surveyed city and county health department officials across New York State to assess perceptions, preparedness and programming related to local climate change impacts. As with the national survey, preparedness questions were grouped into four primary areas: 1) local health department officials’ perceptions of climate change and its potential public health effects; 2) the preparation status of local health departments regarding health impacts of climate change; 3) current or planned activities of local health departments that can help prevent further climate change; 4) resources needed by local health departments to better address climate change-related health risks.
Methods
The survey instrument used in this study was adapted to be self-administered and internet-based from the original phone survey used in the NACCHO national sample, publicly available online at: http://www.edf.org/sites/default/files/7846_AreWeReady_April2008.pdf.14 The original survey was pretested for length, clarity and comprehension with a convenience sample. The adapted online survey was tested by three researchers for length and usability on multiple computer systems and was estimated to take 25–30 minutes to complete. The online format enabled participants to save their responses and resume the survey at a later time.
Outreach to LHD officials in New York State began at the November 2009 monthly meeting of New York State Association of County Health Officials (NYSACHO) commissioners, where a one-page description of the survey objectives and researchers was distributed. NYSACHO is a membership association of public health officials representing the 58 local health departments in New York State.16 The link to the electronic survey, with an accompanying cover letter of support from NACCHO’s Executive Director describing the purpose of the survey, assuring anonymity, and encouraging participation, was then emailed to the LHD officials. Three reminder messages were sent via email at points 10 days, three weeks, and 4 ½ weeks following the reintroduction with notification of the survey closing date. The survey was closed six weeks after opening.
The survey involved Likert-type items – a response scale assessing agreement with survey statements,17 prioritization questions, and open-ended questions. Additionally, there were questions targeting specific climate-related health issues, including: heat waves and heat-related illnesses; storms, including hurricanes and floods; droughts, forest fires or brush fires; vector-borne infectious diseases; water- and food-borne diseases; anxiety, depression or other mental health conditions; quality or quantity of fresh water available to the local jurisdiction; quality of the air, including air pollution, in the local jurisdiction; unsafe or ineffective sewage and septic system operation; food safety and security; housing for residents displaced by extreme weather events; and health care services for people with chronic conditions during service disruptions, such as extreme weather events. The survey instrument has previously been described in detail.13,14 While the method of administration differed between the national sample and this state-based survey, the questions and response choices were unchanged.
Non-respondent analysis and comparability with national sample
Comprehensive non-respondent analysis was not possible with this anonymous survey. However, NYSACHO provides 2008 employee totals for all health departments, and these were compared to the survey responses. Mean staff size of all New York State local health departments is 223 with a median of 81.5,18 while mean staff size of participating departments was 106 with a median of 70. Based on a comparison of employees reported by our survey participants (range=15–400) against 2008 NYSACHO annual LDH survey findings,18 we can conclude that neither Suffolk County (full-time employees=1600) nor New York City (full- and part-time employees=5246), New York State’s two largest metropolitan LDHs, responded. Therefore, though some but not all of New York State’s metropolitan areas were represented, median staff-size within 12 employees between our respondents and all New York State LHDs indicates that this survey reasonably captured the statewide distribution of LHD sizes.
The 2007 “Are We Ready” national sampling frame followed a systematic design across regions and jurisdictional population sizes, with equal representation from small (<50,000 population), medium (50,000–499,999 population), and large (>500,000 population) jurisdictions.13 Given that LHD staff size is proportional to jurisdiction population, we can make certain inferences about jurisdiction sizes represented in our survey and comparability with national survey sample. Within the “Are We Ready” sampling design criteria, six New York State LHDs (including Suffolk and NYC) would have been characterized as representing “large” jurisdictions18, indicating that even if our sample captured the other four “large” LHDs, it would still be relatively skewed toward “small” and “medium” jurisdictions. While stratified national survey results were not available for comparison, interpretation of our survey results and comparability to the national sample may be most appropriate for New York State’s small and medium jurisdictions.
The Human Research Protection Program at Columbia University approved this study protocol.
Results
Our survey included 56 of 58 New York State city and county health departments for whom email contact information was attainable, of which 30 department officials responded, yielding an initial response rate of 54%. Of those who responded, 22 completed the survey for an overall survey completion rate of 39%. Among incomplete surveys, six of the eight participants completed >90% of the questions, and all available data were included in the analysis. Based on job title information provided by respondents, 24 were commissioners, directors or assistant commissioners. The other six respondents included environmental health division directors, emergency preparedness director and not specified.
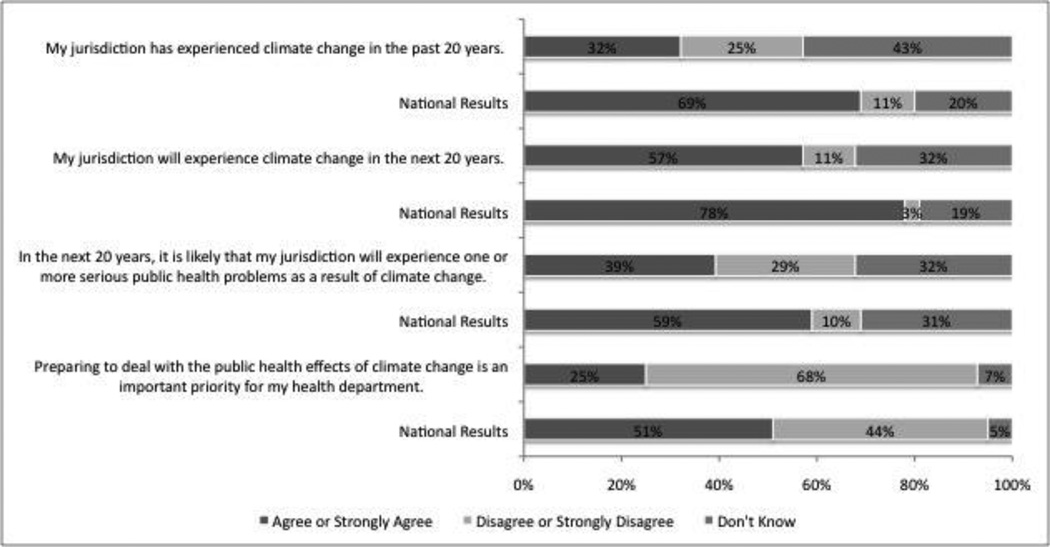
Research area #1 - Perceptions of climate change and its potential public health effects
Thirty-nine percent of New York respondents perceived climate change as a relevant threat to public health in the coming two decades (Figure 1) and 32% thought that their jurisdiction had experienced climate change in the past 20 years. This result contrasts with the national survey, where a higher percentage (59%) perceived climate change as a relevant public health threat and 69% reported that their jurisdiction had already experienced climate change. Consistent with this previous finding, a higher percentage of New York respondents reported that they did not know if climate change had been experienced locally (43% vs. 19% nationally), if it would be experienced locally in the next 20 years (32% vs. 19%), or if it would manifest in health problems (32% vs. 31%).
Figure 1.
New York State versus national LHD officials’ perceptions about climate change in their jurisdictions
One quarter of the respondents perceived climate change as an important priority for the LHD while the majority (68%) disagreed or strongly disagreed with this idea. When asked if preventing or preparing for the public health consequences of climate change was among the top ten priorities of their LHD only 7.1% (n=2) responded affirmatively, with 26 out of 28 officials answering “no” or “don’t know.” Nationally, the percentage of respondents who perceived climate change as an important priority for their local health department (LHD) was 51% and 19% reported preventing or preparing for impacts of climate change as among their department’s top ten priorities.
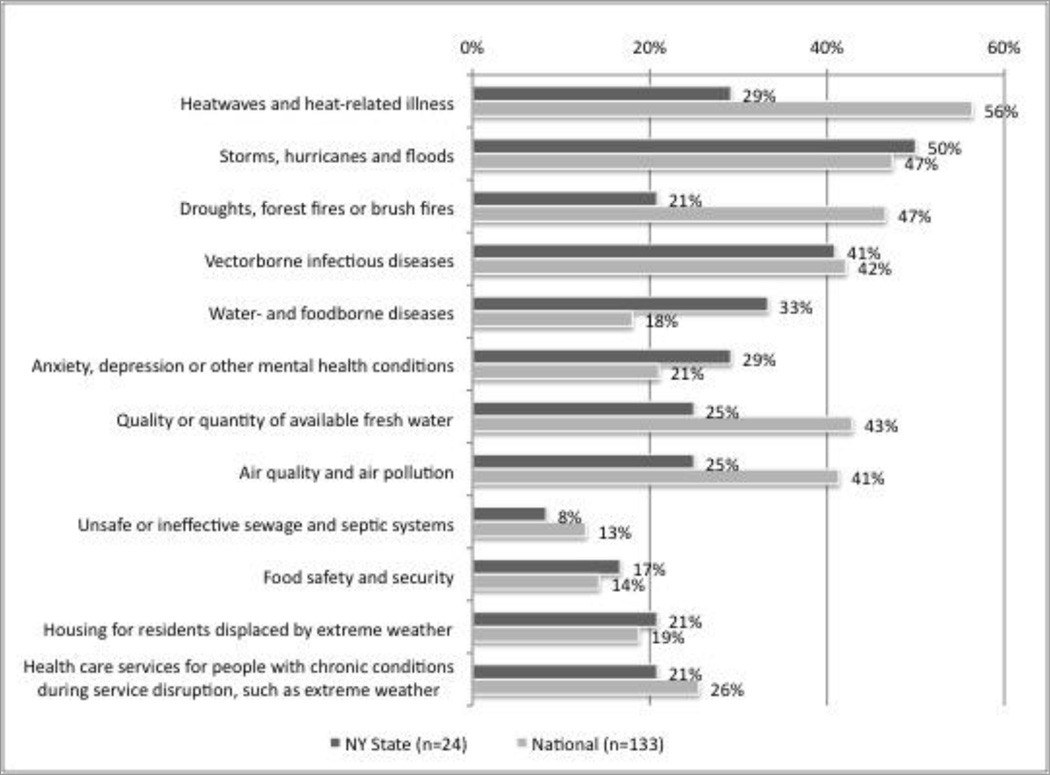
Issues for which at least a quarter of the officials were concerned about existing public health impacts of climate change included heat waves and heat-related illness; storms, hurricanes, and floods; vector-borne diseases; water-and food-borne diseases; anxiety, depression or other mental health conditions; quality and quantity of available fresh water; and air quality and air pollution. Other possible health impacts or exposures that respondents reported to be influenced by climate change included: severe cold and ice; hunger in the event of agricultural crop loss; loss or damage of shoreline and wetlands; and saltwater intrusion of groundwater.
Research area #2 - Preparation status of local health departments regarding potential health impacts of climate change
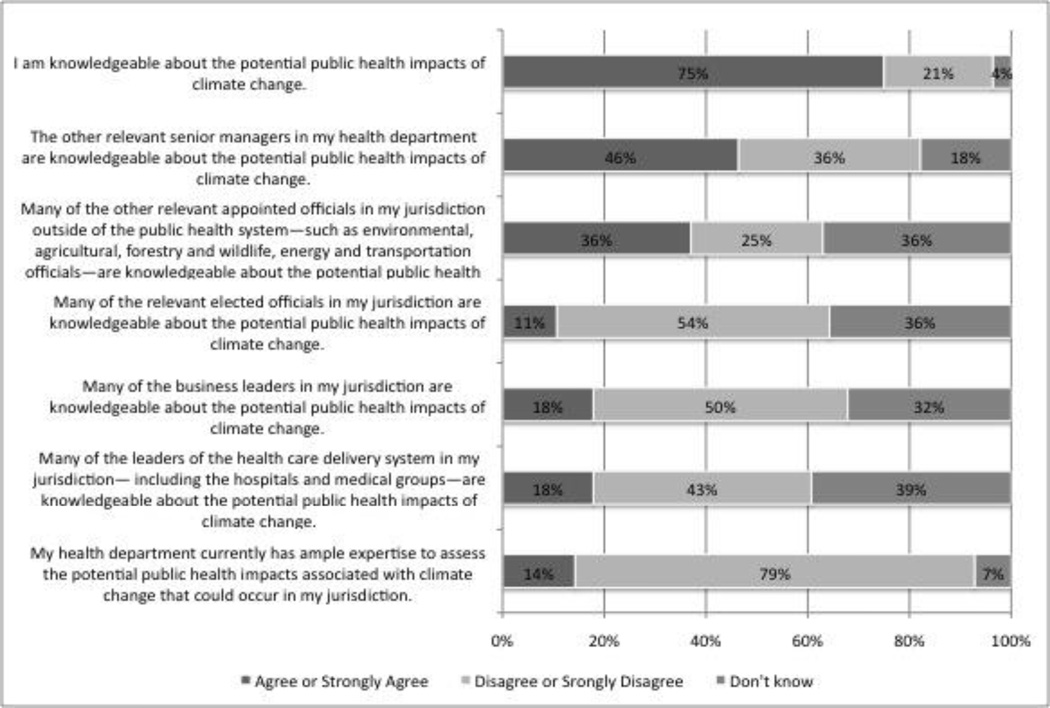
Perceived Knowledge
Three quarters of the respondents felt that they were knowledgeable about the potential health effects of climate change. This response matched the response at the national level. A smaller proportion of the respondents felt that other community leaders were knowledgeable about this topic (Figure 2).
Figure 2.
Knowledge of potential health impacts of climate change among health department officials, local leaders, and decision-makers
Perceived Expertise
The large majority of respondents (79%) disagreed that the local health department had “ample” expertise to assess potential public health risks of climate change in their jurisdiction (Figure 2). This response also matched the response at the national level.
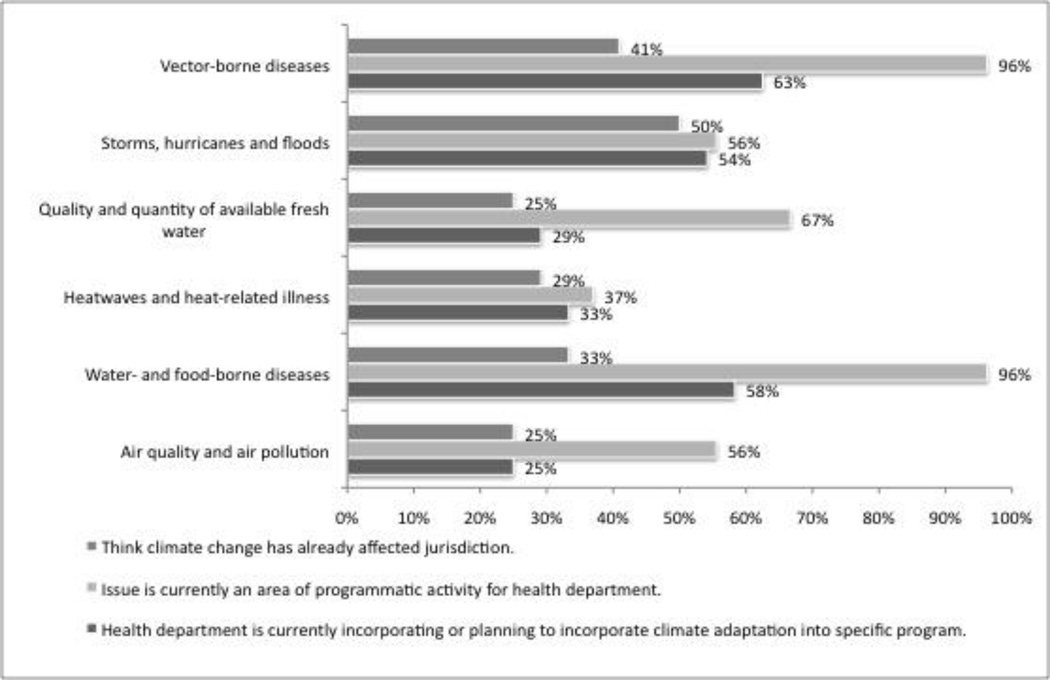
Current Programs of the Health Department
Already existing programs at the local health departments -- not specific to climate change planning -- addressed the following issue: vector-borne disease monitoring and interventions (96%); water- and food-borne diseases (96%); food safety and security (74%); unsafe or ineffective sewage or septic systems (70%); healthcare services for people with chronic conditions (70%); quality or quantity of available fresh water (67%); extreme storm preparedness (56%); air quality programs (56%); and heat-related illness interventions (37%). Fifty six percent of respondents believed that these climate-related health issues were likely to increase in frequency and severity over the next 20 years. The national response had a similar prevalence of programs. The least common areas of programmatic activity in both surveys were those addressing anxiety, depression and mental health conditions; droughts, forest fires and brush fires; and housing for residents displaced by extreme weather events. Figure 3 shows a comparison of perceived public health impacts from climate change, existing programs, and adaptation planning for specific climate-related health issues.
Figure 3.
Programming capacity for climate-related health issues among NY State LHD officials
Current or Planned Climate Change Adaptation Programs of the Health Department
Of programs currently in place, New York State reported generally higher percentages of LHDs having already incorporated climate change adaptation measures, as compared to the national survey, with exceptions of issues related to drought and forest fires (4% in New York State vs. 14% of national sample) and housing for residents displaced by extreme weather events (13% in New York State vs. 19% of national sample). In contrast with the national sample, New York State LHD officials reported fewer plans to expand climate change adaptation programming, with a notable exception for issues related to anxiety, depression or other mental health conditions (17% in New York State vs. 8% of national sample).
Use of Long-Range Weather or Climate Information
The percentage of health departments reporting use of long-range weather climate information in planning or operating their programs was only 19%, whereas the national percentage for this response was slightly higher at 29%.
Research area #3 - Current or planned activities of local health departments that can help prevent further climate change
While the emphasis of this study was toward assessing local adaptation capacity, LHD expertise and actions related to avoiding greenhouse gas emissions (i.e. mitigation) that would contribute to climate change was also assessed. No LHD officials reported ample expertise at the local level to create an effective climate change mitigation plan, while a modestly larger number believed that expertise within the State health department (13%) and the Centers for Disease Control and Prevention (29%) could effectively support local mitigation planning. However, almost half reported programs in areas consistent with mitigation objectives, such as programs that encourage active transportation such as cycling and walking (49%) and programs that encourage purchase of local grown, organic or plant-based foods (35%). These programmatic findings were consistent with national findings.
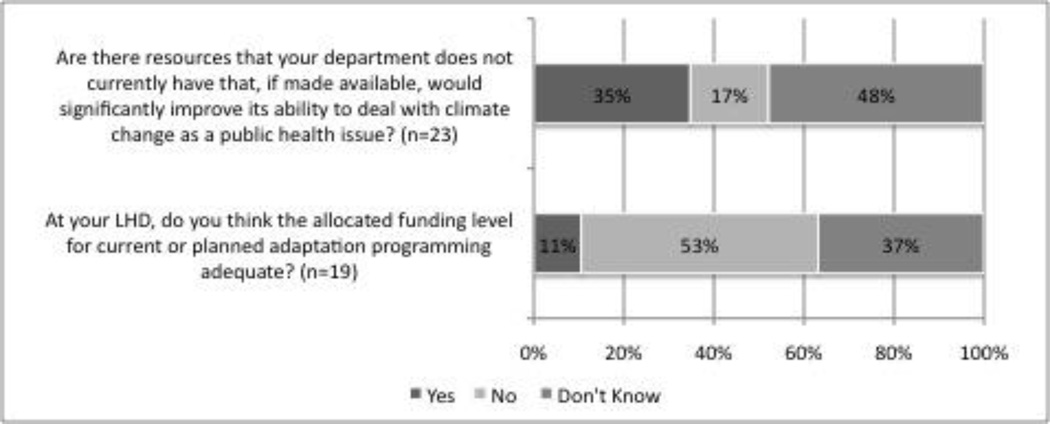
Research area #4 - Resource needs of local health departments to better address climate change
Almost half of respondents (48%) reported that they did not know if additional resources would be helpful to address climate change as a public health issue (Figure 4). About a third of respondents (35%) reported that additional resources would significantly improve their department’s ability to deal with this issue, citing the following examples: additional staff (80%), staff training (80%), additional funding to support the activity (60%), and equipment (40%). A small group (17%) reported that additional resources were not needed.
Figure 4.
Perceptions of resource needs and appropriateness of available funding among NY State LHD officials
Compared to the national survey, New York State respondents were less certain about the role additional resources would play in addressing climate change as a public health issue, whereas additional staff and staff training were disproportionately identified by the New York respondents as a specific need in this area (Figure 5). Examples of New York State respondent explanations include:
With the current fiscal crisis in our region we are challenged to achieve basic health department mandated functions. We also do not have the expertise to address this issue nor the funds to expand the programs we currently run.
The local health department has not traditionally had a primary response role to environmentally related issues although we do support the emergency services department. While we understand that this is a role that public health should have, current fiscal restraints prevent us from being able to address climate change health effects in a suitable manner. Issues with food, water, etc. are covered by New York State Department of Health.
Figure 5.
New York State versus national LHD officials’ perceived impact of additional resources toward addressing climate change, by public health issue
Discussion
Similar to responses from the national sample, the majority of New York State health department officials perceives climate change as relevant to public health and reports at least some specific programs that are already using or planning to use climate adaptation strategies. However, nearly half don’t know what, if any, resources would improve their health department’s ability to deal with climate change as a public health issue. So while, on the one hand it seems that most are aware of and directing resources toward the issue of public health impacts of climate change, many also seem unsure of how to best address these issues and harness existing program capacity. Furthermore, some health departments perceived these issues as outside their designated role.
The only other example of regional analysis of climate change preparedness7 known to the authors found similar patterns of insufficient funding and political support for local adaption planning. In that California-based study, Bedsworth concluded that LHDs in may be better prepared to initiate adaptation planning than department officials perceive through building on existing program areas, echoing a key recommendation from the ClimAID Public Health Sector for New York State.12 In the economic climate of funding reductions, adaptation approaches need, even more, to align with other public health strategies.4,5,20 Although community-based adaptation strategies were not addressed in this survey, LHD engagement with local communities to build preparedness capacity can strengthen LHD ongoing planning and programming as well as reduce population vulnerability through social capital development.4
This type of local assessment makes clear how varied impacts and capacity are at this relatively fine policy and funding scale, signaling the importance of local studies such as this one. As of 2009, only 5 states had published a strategic climate change plan that included a public health response including: California, Maryland, New Hampshire, Virginia, and Washington. Twenty-eight other states had strategic climate plans without specific public health components.19
Using the same survey instrument as the 2007 national “Are We Ready?” survey14 was a key strength of this study and allowed for comparison of trends between surveyed New York State officials and a representative national sample. While national-level data is invaluable for federal policymaking and the larger public health community, local perceptions, priorities and capacity can be expected to vary as widely as projected climate impacts. Therefore, it is essential for regional and local jurisdictions to utilize this type of self-assessment tool for long-term and emergency planning under climate change.
A possible limitation of this survey, for both the national and New York State sample, is that the questions might not fully explore the existing programs related to climate change health effects but not labeled as such officially by the organization or within the perception of the individual responding to the survey. This issue is somewhat addressed by the general programmatic question: “Are the following health issues currently areas of programmatic activity for your health department?” and includes an array of responses without reference to whether or not there is a perception of any relatedness to climate change.
A key limitation of this study is the low response rate. Due to time constraints of the project, additional efforts such as more outreach at the monthly commissioner meetings, a paper mailing reminder, or additional emails were not possible. Though anonymous surveys are limited by the extent of non-respondent analysis possible, we compared reported respondents’ staff size with documented numbers18 to better understand representativeness of our sample for New York State. Median staff sizes of participating LHDs and NYSACHO documented state median were within 12 employees of each other, indicating reasonable representativeness across New York State. While under-representation of LHDs serving large (>500,000 population) jurisdictions limits generalizability of our findings to the entire state, here we may capture unique challenges faced by small and medium sized jurisdictions related to reliance on state-operated facilities and programs, such as diagnostic laboratories.21 Despite these limitations, the responses do provide a valuable starting point for discussion among New York public health officials, and also for public health professionals in other states and outside the U.S., regarding methods for assessing local perceptions and preparedness about climate change.
A diverse state, with populations spread unevenly over urban and rural service areas, New York is one of 26 states with primary reliance on a county-based system for service delivery.22 In New York State, LHDs operate under either county legislature or local board of health authority, creating a highly decentralized system with non-uniform provision of core services. For example, environmental health services are provided by LHDs in 37 out of 62 counties while other areas are provided service by the state Department of Health.23 While some of the challenges to implementing adaptation programming identified by New York State LHD officials stem from the diversity of climate and ecosystem factors, other challenges relate to the decentralized nature of the State’s public health structure.
In 2003, the New York State Public Health Council identified the legal decentralization of public health service delivery as a key obstacle to efficient coordination of programming and data resources, elements that could affect climate-health preparedness, recommending regional, multi-county initiatives as proven models for more efficient and equitable distribution of expertise and services.22 Therefore, exploring variations in LHD officials’ climate change perception and adaption priorities can not only inform state and federal funding and planning processes but also highlight climate-related health issues for potential collaboration and preparedness networks across the state, particularly among states with similarly decentralized public health systems.
Acknowledgments
The authors would like to acknowledge Ed Maibach, Linda Wagner (NYSACHO); Michelle Chuk, Jennifer Li, and Robert M. Pestronk (NACCHO); and the ClimAID team.
Funding:
The survey was conducted as part of ClimAID – a New York statewide, multi-sector climate change adaptation assessment bringing together researchers and stakeholders to identify local vulnerabilities and suggest effective policy and preparedness strategies. ClimAID was funded by the New York State Energy Research and Development Authority, and the full report is available on line at: http://www.nyserda.org/programs/environment/emep/climate_change_newyork_impacts.asp.
The Earth Institute at Columbia University provided additional research funding.
P. Sheffield was supported by National Institutes of Health Research Training Program in Environmental Pediatrics (NIH #5T32 HD049311).
Footnotes
Conflicts of Interest and Funding Disclosure:
The authors report no conflict of interest.
REFERENCES
- 1.Confalonieri U, Menne B, Akhtar R, et al. Human Health. In: Parry M, Canziani O, JP P, van der Linden P, Hansen C, editors. Climate Change 2007: Impacts, adaptation and vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge: Cambridge University Press; 2007. pp. 339–431. [Google Scholar]
- 2.Patz JA, Gibbs HK, Foley JA, Rogers JV, Smith KR. Climate change and global health: quantifying a growing ethical crisis. Eco Health. 2007;4:397–405. [Google Scholar]
- 3.Balbus JM, Malina C. Identifying vulnerable subpopulations for climate change health effects in the United States. J Occup Environ Med. 2009 Jan;51(1):33–37. doi: 10.1097/JOM.0b013e318193e12e. [DOI] [PubMed] [Google Scholar]
- 4.Ebi KL, Semenza JC. Community-based adaptation to the health impacts of climate change. Am J Prev Med. 2008 Nov;35(5):501–507. doi: 10.1016/j.amepre.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 5.St Louis ME, Hess JJ. Climate change: impacts on and implications for global health. Am J Prev Med. 2008 Nov;35(5):527–538. doi: 10.1016/j.amepre.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 6.IPCC. Summary for Policymakers. In: Parry M, Canziani O, JP P, van der Linden P, Hansen C, editors. Climate Change 2007: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge: Cambridge University Press; 2007. pp. 7–22. [Google Scholar]
- 7.Bedsworth L. Preparing for climate change: a perspective from local public health officers in California. Environ Health Perspect. 2009 Apr;117(4):617–623. doi: 10.1289/ehp.0800114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ebi KL. Public health responses to the risks of climate variability and change in the United States. J Occup Environ Med. 2009 Jan;51(1):4–12. doi: 10.1097/JOM.0b013e31816fd67b. [DOI] [PubMed] [Google Scholar]
- 9.Keim ME. Building human resilience: the role of public health preparedness and response as an adaptation to climate change. Am J Prev Med. 2008 Nov;35(5):508–516. doi: 10.1016/j.amepre.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 10.NYSERDA ClimAID Team. Integrated Assessment for Effective Climate Change Adaptation Strategies in New York State. Albany, New York: New York State Energy Research and Development Authority (NYSERDA); 2010. [Google Scholar]
- 11.New York State Climate Action Council (NYSCAC) Climate Action Council Interim Report. [Accessed 15 March 2011];2010 http://www.nyclimatechange.us/ewebeditpro/items/O109F24141.pdf. [Google Scholar]
- 12.Kinney P, Carr JL, Ostfeld R, Sheffield P. Public Health. In: Rosenzweig C, Solecki W, DeGaetano A, Hassol S, Grabhorn P, O’Grady M, editors. Responding to Climate Change in New York State, the Synthesis Report of the Integrated Assessment for Effective Climate Change Adaptation Strategies in New York State. Albany, New York: New York State Energy Research and Development Authority (NYSERDA); 2010. [Google Scholar]
- 13.Maibach EW, Chadwick A, McBride D, Chuk M, Ebi KL, Balbus J. Climate change and local public health in the United States: preparedness, programs and perceptions of local public health department directors. PLoS One. 2008;3(7):e2838. doi: 10.1371/journal.pone.0002838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balbus J, Ebi KL, Finzer L, et al. Are we ready? Preparing for the public health challenges of climate change. Wasington, DC: Environmental Defense Fund; 2008. [Google Scholar]
- 15.Ebi KL, Balbus J, Kinney PL, et al. U.S. Funding is insufficient to address the human health impacts of and public health responses to climate variability and change. Environ Health Perspect. 2009 Jun;117(6):857–862. doi: 10.1289/ehp.0800088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.New York State Association of County Health Officials (NYSACHO) Home page. [Accessed 23 February 2011];2011 http://www.nysacho.org/i4a/pages/index.cfm?pageid=1. [Google Scholar]
- 17.Likert R. A Technique for the Measurement of Attitudes. Archives of Psychology. 1932;140:1–55. [Google Scholar]
- 18.New York State Association of County Health Officials (NYSACHO) NYSACHO Survey. [Accessed 3 March 2010];2008 http://www.nysacho.org/i4a/pages/index.cfm?pageid=3379. [Google Scholar]
- 19.Trust for America's Health. Health Problems Heat Up: Climate Change and the Public’s Health. [Accessed 17 February, 2011];2009 http://healthyamericans.org/reports/environment/. [Google Scholar]
- 20.Schmidt CW. Beyond mitigation: planning for climate change adaptation. Environ Health Perspect. 2009 Jul;117(7):A306–A309. doi: 10.1289/ehp.117-a306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Public Health Institute. Health Reform and Local Health Departments: Opportunities for the Centers for Disease Control and Prevention. [Accessed 28 August, 2011];2010 http://www.phi.org/pdf-library/PHI_CDC_Health_Reform_and_Local_Health_Departments.pdf. [Google Scholar]
- 22.New York State Public Health Council (NYSPHC) Strengthening New York’s Public Health System for the 21st Century: Report to the Commissioner of Health, Antonia C. Novello MD, MPH, DrPH. [Accessed 12 February, 2010];2003 http://www.health.state.ny.us/press/reports/century/ph_21stcent.pdf. [Google Scholar]
- 23.Public Health Association of New York City (PHANYC) Strengthening New York City’s Public Health Infrastructure. [Accessed 17 February 2011];2001 http://www.phanyc.org/pdfs/NYCphiW2.pdf. [Google Scholar]