Abstract
Obsessive-compulsive disorder (OCD) often co-occurs with psychotic and bipolar disorders; this comorbidity complicates the clinical management of these conditions. In this population-based longitudinal and multigenerational family study, we examined the patterns of comorbidity, longitudinal risks, and shared familial risks between these disorders. Participants were individuals with a diagnosis of OCD (n = 19814), schizophrenia (n = 58336), bipolar disorder (n = 48180), and schizoaffective disorder (n = 14904) included in the Swedish Patient Register between January 1969 and December 2009; their first-, second-, and third-degree relatives; and population-matched (1:10 ratio) unaffected comparison individuals and their relatives. The Swedish Prescribed Drug Register was used to control for the potential effect of medication in the longitudinal analyses. Individuals with OCD had a 12-fold increased risk of having a comorbid diagnosis of schizophrenia and a 13-fold increased risk of bipolar disorder and schizoaffective disorder. Longitudinal analyses showed that individuals first diagnosed with OCD had an increased risk for later diagnosis of all other disorders, and vice versa. The risk of bipolar disorder was reduced, but not eliminated, when the use of selective serotonin reuptake inhibitors was adjusted for. OCD-unaffected first-, second-, and third-degree relatives of probands with OCD had a significantly increased risk for all 3 disorders; the magnitude of this risk decreased as the genetic distance increased. We conclude that OCD is etiologically related to both schizophrenia spectrum and bipolar disorders. The results have implications for current gene-searching efforts and for clinical practice.
Key words: OCD, schizophrenia, schizoaffective disorder, bipolar disorder, genetic epidemiology
Introduction
Obsessive-compulsive disorder (OCD) is often comorbid with other mental disorders to the extent that patients with no comorbidities are the exception rather than the rule. By far, the most frequently co-occurring conditions are unipolar depression, anxiety disorders, and other OCD-related disorders,1,2 but OCD can also co-occur with other severe mental disorders, such as schizophrenia, schizoaffective disorder, and bipolar disorder, more frequently than what would be expected by chance.3–8 For example, a recent meta-analysis of schizophrenia studies has indicated a 14% and 30% prevalence of OCD and subclinical obsessive-compulsive symptoms (OCS), respectively.9 Furthermore, “transitions” from OCD to schizophrenia spectrum disorders have been described in the classic literature.10–12 Clinically, the presence of OCD or OCS in schizophrenia spectrum disorders is associated with poorer cognitive functioning, increased levels of depression, more severe positive and negative symptoms, poorer social functioning, and higher rates of hospitalization.13–16 Though less studied, the prevalence of comorbid bipolar disorder in OCD samples is also substantial (13%–23%) and may be associated with a more episodic course of OCD, increased severity, comorbidity, suicide risk, and overall impairment.7,8,17–20
The clinical management of such comorbidities is often complex because it requires careful optimization of medication regimes. For example, there is some evidence that atypical antipsychotics may trigger or exacerbate OCS in patients with schizophrenia,21–27 particularly in genetically vulnerable individuals.28 Similarly, in individuals with OCD and bipolar disorder, prescription of antidepressant medication might trigger or exacerbate manic or hypomanic episodes.7,17
Given these important clinical considerations, there is a need to understand the nature of the association between OCD and these complex psychiatric comorbidities. One possibility is that OCD shares a common genetic etiology and pathophysiology with these disorders, as has already been suggested for other severe mental disorders,29,30 but other explanations are also possible. Because many of the abovementioned studies were conducted in specialized clinical settings, the association between these disorders may be spurious. That is, people with comorbidities may be more likely to seek help than people with a single mental disorder.4 Artificial comorbidity may also arise if the treatment for one disorder causes the other, as in the case of antipsychotic-induced OCS or antidepressant-induced mania. Furthermore, it may sometimes be difficult to distinguish an obsession with poor insight from a true psychotic delusion, leading to possible misdiagnoses.4
In this cohort, longitudinal and multigenerational family study, we linked national Swedish registers to shed new light on the nature of the relationships between OCD, schizophrenia, and bipolar disorder. For completeness, we also included schizoaffective disorder in the analyses. We first examined the comorbidity patterns between OCD, schizophrenia, schizoaffective disorder, and bipolar disorder at the population level. We next employed longitudinal analyses to examine the sequential risks of these disorders in individuals first diagnosed with OCD, and vice versa. In these analyses, we controlled for the potential effects of medication. Finally, we investigated the risks of schizophrenia, schizoaffective disorder, and bipolar disorder in relatives of individuals with OCD with differing genetic distances to the probands. This family-based approach removes many of the disease-related factors that may create spurious associations between these disorders.
Methods
National Registers
Following approval from the Regional Ethics Committee in Stockholm, we linked 4 Swedish national registers, using the individual personal identification numbers assigned at birth or, for resident immigrants, upon arrival to the country. The Total Population Register contains demographic information on all individuals registered as Swedish inhabitants since 1968 and is extended by the Multi-Generation Register, which contains information about the identity of biological parents of all individuals born in Sweden since 1932 and living in Sweden since 1961. The latter register allows the reconstruction of family pedigrees for all individuals with relatives at increasing genetic and environmental distances from each index person. The Swedish National Patient Register31 covers psychiatric inpatient care since 1969 and outpatient care since 2001. The Swedish Prescribed Drug Register contains data on all dispensed prescribed drugs since July 2005.32 Using the codes from the Anatomical Therapeutic Chemical Classification System, we identified all dispensed prescriptions of atypical antipsychotics (clozapine, olanzapine, quetiapine, risperidone, and aripiprazole) in patients with schizophrenia and schizoaffective disorder and of antidepressants (selective serotonin reuptake inhibitors [SSRI], serotonin and norepinephrine reuptake inhibitors [SNRI], and other antidepressants [including clomipramine]) in persons with OCD. The study period spans 40 years (January 1969–December 2009).
Validity of International Classification of Diseases Codes for OCD
OCD probands were defined as individuals identified in the National Patient Register with at least one International Classification of Diseases (ICD)-10 diagnosis of OCD (F42). The ICD codes for OCD have been recently subject to validation (Rück et al, in preparation). Briefly, we obtained a random sample of patient records from 3 Swedish counties (N = 68). Each file was carefully reviewed and blindly rated by 2 independent clinicians specialized in OCD. The ICD-10 codes, which represent approximately 80% of the OCD cases in the Register, had excellent validity, with a positive predictive value (true positives/true positives + false positives) of 91% (rater 1) and 98% (rater 2). The inter-rater agreement between the 2 raters was outstanding (κ = 0.98, P < .001). ICD-8 and ICD-9 patients were not included in this study because the validation study suggested relatively high rates of false positives.
Classification of Schizophrenia, Bipolar Disorder, and Schizoaffective Disorder
Schizophrenia was defined as at least one inpatient episode with a discharge diagnosis of schizophrenia (ICD-8: 295.0–295.6, 295.8, 295.9; ICD-9: 295A-295G, 295W, 295X; ICD-10: F20). Inpatient diagnoses of schizophrenia have a 94% agreement when compared with research diagnoses based on semi-structured interviews and medical records.33
Bipolar disorder was defined according to a validated algorithm based on the following codes in the National Patient Register: ICD-8/9: 296 and ICD-10: F30–F31, with the exclusion of individuals whose identification relied solely on ICD-8: 296.2 or ICD-9: 296B. This algorithm, which requires at least 2 discharge diagnoses of bipolar disorder, showed 92% agreement when compared with reassessed diagnostic status based on medical records.34
Schizoaffective disorder was defined as at least one inpatient or outpatient diagnosis of the disorder (ICD-8: 295.7, ICD-9: 295H, and ICD-10: F25).
Statistical Analysis
We first examined the risks of schizophrenia, bipolar disorder, and schizoaffective disorder in individuals with OCD (index persons) compared with individuals without OCD at the time of the first diagnosis of the index persons. For each individual with OCD, 10 individuals matched by birth year, sex, and county of residence at the time of the first OCD diagnosis of the index person were randomly selected from the general population. They had to be alive, living in Sweden, and not diagnosed with OCD at the time of the first OCD diagnosis of the index person.
In longitudinal analyses, we estimated the risk that individuals with OCD would receive a later diagnosis of schizophrenia, bipolar disorder, or schizoaffective disorder compared with individuals without an OCD diagnosis during the follow-up period. Conversely, we also examined the risk that individuals first diagnosed with each of these 3 disorders would later receive a diagnosis of OCD compared with individuals without such diagnoses during the follow-up period. We also calculated the median number of years (plus interquartile range [IR]) between the first diagnosis (eg, OCD) and the subsequent diagnoses (eg, schizophrenia). These longitudinal analyses were only done for patients first diagnosed in ICD-10 to ensure equal follow-up periods for all disorders. For patients first diagnosed after July 2005 (the start date of the Swedish Prescribed Drug Register), we further examined whether these sequential risks were maintained after adjusting for the dispensation of atypical antipsychotics in persons first diagnosed with schizophrenia or schizoaffective disorder and for the dispensation of antidepressants in persons first diagnosed with OCD.
Finally, we used the family design to examine the possible etiological overlap between OCD and the other disorders of interest. Specifically, the risks of schizophrenia, bipolar disorder, and schizoaffective disorder in relatives of individuals with OCD who did not have a lifetime diagnosis of any of the 3 disorders were compared with the risks in relatives of individuals without a diagnosis of OCD, schizophrenia, bipolar disorder, or schizoaffective disorder. For each index person-relative pair, 10 randomly selected unexposed-relative pairs were matched by birth year and gender, and they had to be alive, living in Sweden, and without a diagnosis of OCD at the time of the first diagnosis of the index person. This method reduces potential bias introduced by individuals in the population registers entering the study at different times. OCD-affected relatives of individuals with OCD were excluded in order to control for the effect of independent transmission of these conditions. Shared familial (genetic and environmental) risk factors are assumed when individuals with the index disorder (ie, OCD) have relatives with the other disorder (ie, schizophrenia) but not the index disorder.35 First-, second-, and third-degree relatives were analyzed separately to examine the extent to which the familial associations were influenced by genetic and shared environmental factors. These analyses were based on the following assumptions: (1) first-degree relatives are more genetically similar than second-degree relatives, who in turn are more genetically similar than third-degree relatives and (2) maternal half-siblings are more similar in shared environmental exposures than paternal half-siblings because Swedish children continue to live predominantly (90%) with their mother following parental separation.36
To estimate the concurrent and longitudinal risks of schizophrenia, bipolar disorder, and schizoaffective disorder in individuals with OCD (and vice versa), we calculated risk ratios (RR) and corresponding 95% CIs using conditional logistic regressions. When assessing risks within families, CIs were obtained with a robust sandwich estimator function to adjust for the correlated data structure. All analyses were conducted in SAS version 9.3 (SAS Institute).
Results
We identified 19 814 individuals with OCD (43.5% males), 58336 individuals with schizophrenia (54.4% males), 48180 individuals with bipolar disorder (38.7% males), and 14 904 with schizoaffective disorder (41.2% males).
Individuals with OCD had a 12 times higher risk of having a comorbid diagnosis of schizophrenia compared with individuals without OCD. Similarly, individuals with OCD had a 13–14 times increased risk of bipolar disorder and schizoaffective disorder (table 1). These risks approximately doubled when the analyses were limited to individuals first diagnosed with OCD in inpatient settings (n = 3234; 46.2% males) but remained substantial in individuals first diagnosed with OCD in outpatient settings (n = 16 466; 42.6% males; supplementary table 1).
Table 1.
Risks of Schizophrenia, Bipolar, and Schizoaffective Disorders in Individuals With OCD Compared With Matched Individuals Without OCD From the General Population
| OCD Probands (n = 19700)a | Matched Comparison Individuals (n = 197000) | RRs (95% CIs) | |
|---|---|---|---|
| n (%) | n (%) | ||
| Schizophrenia | 557 (2.83) | 476 (0.24) | 12.3 (10.9–14.0) |
| Bipolar disorder | 950 (4.82) | 734 (0.37) | 13.7 (12.4–15.1) |
| Schizoaffective disorder | 306 (1.55) | 232 (0.12) | 13.4 (11.3–15.9) |
Note: OCD, obsessive-compulsive disorder; RRs, risk ratios.
a19700 out of 19 814 identified individuals with OCD were used in these analyses. The remaining 114 individuals could not be assigned comparison individuals per the matching criteria.
Longitudinal analyses (ICD-10 only) showed that individuals first diagnosed with OCD had a 3-fold higher risk of receiving a later diagnosis of schizophrenia compared with individuals without OCD during the follow-up period (table 2). The median time between the first diagnosis of OCD and the subsequent first diagnosis of schizophrenia was 2.4 years (IR = 3.6). The risk of being diagnosed with schizoaffective disorder after having first received a diagnosis of OCD was approximately 5 times higher, with a median of 1.8 years between diagnoses (IR = 3.5). Finally, individuals with OCD had a 12 times higher risk of receiving a later diagnosis of bipolar disorder, with a median of 2.7 years between diagnoses (IR = 3.5).
Table 2.
Longitudinal Risks of Receiving a Later Diagnosis of Schizophrenia, Bipolar Disorder, and Schizoaffective Disorder After Receiving an Initial Diagnosis of OCD Compared With Individuals Without OCD During the Follow-up Period (ICD-10 Cases Only)
| Later Diagnosis | Initial Diagnosis | RRs (95% CIs) | |
|---|---|---|---|
| OCD (N = 18907)a | No OCD (N = 189070) | ||
| n (%) | n (%) | ||
| Schizophrenia | 114 (0.60) | 425 (0.22) | 2.7 (2.2–3.3) |
| Bipolar disorder | 787 (4.16) | 718 (0.38) | 11.6 (10.5–12.9) |
| Schizoaffective disorder | 106 (0.56) | 218 (0.12) | 4.9 (3.9–6.2) |
Note: Abbreviations are explained in the first footnote to table 1.
aOCD patients with prior diagnoses of schizophrenia, bipolar disorder, or schizoaffective disorder are excluded from the analyses.
These longitudinal risks were substantially higher, particularly for schizophrenia and schizoaffective disorder, when the analyses were limited to individuals first diagnosed as having OCD in inpatient settings (supplementary table 2). In outpatients with OCD, the magnitude of the risk was slightly reduced for all disorders and fell just short of significance for schizophrenia (supplementary table 2).
In a subsample of incident OCD cases diagnosed after July 2005 (N = 12520), the sequential risk of receiving a later diagnosis of bipolar disorder was substantially reduced, but not eliminated, when the use of SSRIs was controlled for in the analyses (adjusted RR = 8.8, CI = 7.5–10.2). No such reduction in risk was observed when we controlled for SNRIs or other antidepressant medication (supplementary table 3).
Individuals first diagnosed with schizophrenia had a 7 times higher risk of receiving a later diagnosis of OCD compared with individuals without schizophrenia during the same follow-up period (table 3). The median time between diagnoses was 3.7 years (IR = 4.9). Individuals with schizoaffective disorder had a 5 times higher risk of a later diagnosis of OCD compared with individuals without schizoaffective disorder, with a median time between diagnoses of 2.5 years (IR = 4.4). In a subsample of incident schizophrenia or schizoaffective disorder cases diagnosed after July 2005 (N = 5999), the sequential risk of receiving a later diagnosis of OCD was only marginally reduced when the use of atypical antipsychotics was controlled for in the analyses (adjusted RR = 5.1, CI = 3.3–7.8) (supplementary table 4). Finally, in individuals with bipolar disorder, the risk of a later diagnosis of OCD was approximately 1.2 times higher, with a median time between diagnoses of 1.1 years (IR = 2.0). The results survived when the analyses were restricted to outpatients with OCD, but the risks were generally higher among inpatients with OCD (supplementary table 5).
Table 3.
Longitudinal Risk of Developing OCD After Receiving an Initial Diagnosis of Schizophrenia, Bipolar Disorder, or Schizoaffective Disorder Compared With Individuals Without These Diagnoses During the Follow-up Period (ICD-10 Diagnoses Only)
| Later Diagnosis | Initial Diagnoses | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Schizophrenia | Bipolar Disorder | Schizoaffective Disorder | |||||||
| Present (N = 8841) | Absent (N = 87528) | RRs (CIs) | Present (N = 29322) | Absent (N = 293220) | RRs (CIs) | Present (N = 8278) | Absent (N = 81691) | RRs (CIs) | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| OCD | 109 (1.23) | 157 (0.18) | 7.0 (5.5–9.0) | 76 (0.26) | 630 (0.21) | 1.2 (0.9–1.5) | 93 (1.12) | 191 (0.23) | 5.0 (3.9–6.4) |
Note: Abbreviations are explained in the first footnote to table 1.
aSchizophrenia, bipolar disorder, and schizoaffective disorder patients who have a prior diagnosis of OCD are excluded from the analyses.
Table 4 presents the results of the family data. When the proband had OCD, their OCD-unaffected first-degree relatives had a significantly increased risk for all 3 disorders. Second- and third-degree relatives of OCD probands also had elevated risks for all 3 disorders, and the magnitude of this risk was significantly smaller than the risk for first-degree relatives for schizophrenia and bipolar disorder. The risks for full siblings tended to be higher than that of half-siblings, particularly for schizophrenia and bipolar disorder. Maternal and paternal half-siblings appeared to have similar risks. These familial risks were largely comparable (not significantly different) for outpatients vs inpatients with OCD (supplementary table 6).
Table 4.
Risks of Schizophrenia, Bipolar Disorder, and Schizoaffective Disorder in OCD-Unaffected Relatives of Individuals With OCD (Exposed) Compared With Relatives of Individuals Without OCD (Unexposed)
| Risk of Schizophrenia | Risk of Bipolar Disorder | Risk of Schizoaffective Disorder | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Exposed | Unexposed | RRs (CIs) | Exposed | Unexposed | RRs (CIs) | Exposed | Unexposed | RRs (CIs) | |
| n (%) | n (%) | n (%) | |||||||
| First-degree relatives | |||||||||
| Parents | 26 (0.19) | 114 (0.09) | 2.2 (1.5–3.4) | 38 (0.28) | 207 (0.16) | 1.8 (1.3–2.5) | 11 (0.08) | 54 (0.04) | 2.0 (1.1–3.6) |
| Children | 125 (0.39) | 750 (0.24) | 1.6 (1.4–2.0) | 248 (0.77) | 1512 (0.48) | 1.6 (1.4–1.9) | 60 (0.19) | 403 (0.13) | 1.5 (1.1–1.9) |
| Full siblings | 114 (0.51) | 533 (0.24) | 2.1 (1.7–2.6) | 138 (0.62) | 728 (0.33) | 1.9 (1.6–2.2) | 39 (0.18) | 262 (0.12) | 1.5 (1.1–2.0) |
| All first-degree relatives | 265 (0.39) | 1397 (0.21) | 1.9 (1.6–2.1) | 424 (0.63) | 2447 (0.37) | 1.7 (1.6–1.9) | 110 (0.16) | 719 (0.11) | 1.5 (1.2–1.8) |
| Second-degree relatives | |||||||||
| Maternal half-siblings | 18 (0.41) | 102 (0.29) | 1.3 (0.8–2.2) | 27 (0.61) | 142 (0.40) | 1.6 (1.1–2.3) | 4 (0.09) | 47 (0.13) | 0.6 (0.2–1.6) |
| Paternal half-siblings | 18 (0.32) | 143 (0.32) | 0.9 (0.6–1.5) | 23 (0.41) | 160 (0.36) | 1.3 (0.8–1.9) | 7 (0.13) | 48 (0.11) | 1.1 (0.5–2.4) |
| All half-siblings | 37 (0.37) | 253 (0.27) | 1.3 (0.9–1.8) | 52 (0.51) | 380 (0.41) | 1.3 (1.0–1.7) | 11 (0.11) | 98 (0.11) | 1.0 (0.5–1.8) |
| All second-degree relativesa | 329 (0.47) | 2399 (0.35) | 1.4 (1.2–1.5) | 342 (0.49) | 2758 (0.40) | 1.2 (1.1–1.4) | 121 (0.17) | 1008 (0.15) | 1.2 (1.0–1.4) |
| Third-degree relatives | |||||||||
| Cousins | 149 (0.20) | 1091 (0.15) | 1.4 (1.2–1.6) | 258 (0.34) | 2049 (0.27) | 1.3 (1.1–1.4) | 70 (0.09) | 511 (0.07) | 1.4 (1.1–1.7) |
Note: Abbreviations are explained in the first footnote to table 1. Statistically significant RRs are highlighted in bold.
aSecond-degree relatives include half-siblings, grandparents, grandchildren, uncles/aunts, and nephews/nieces.
Discussion
The results of the current population-based study confirm the findings of previous reports and meta-analyses, suggesting that schizophrenia, bipolar disorder, and schizoaffective disorder are far more common in individuals with OCD than would be expected by chance. In longitudinal analyses, we found that an initial diagnosis of OCD increased the risk of a later diagnosis of schizophrenia spectrum and bipolar disorders, and vice versa. Finally, the family analyses showed strong familial links between these disorders.
Compared with unaffected individuals, patients first diagnosed with OCD were approximately 3 times more likely to develop schizophrenia and 5 times more likely to develop schizoaffective disorder at a later point in time; this risk was higher in patients who were first diagnosed with OCD in an inpatient setting but also remained significant in outpatients with OCD. This confirms earlier observations derived mainly from clinical samples10–12 and a recent Danish population-based study37 and suggest that a small proportion of OCD cases (less than 1% in our study) may make a transition to psychosis although the possibility of misdiagnosis cannot be fully ruled out. It may be that patients that appear to make a transition from OCD to a schizophrenia spectrum disorder may have been psychotic all along despite the relatively long gap between the 2 diagnoses (a median of approximately 2 years). Research in first episode psychosis and ultrahigh-risk individuals has indicated that OCS can sometimes precede the onset of the first psychotic episode.38 Therefore, it is important for clinicians to be aware that OCD symptoms may sometimes constitute the initial manifestations of a psychotic syndrome.
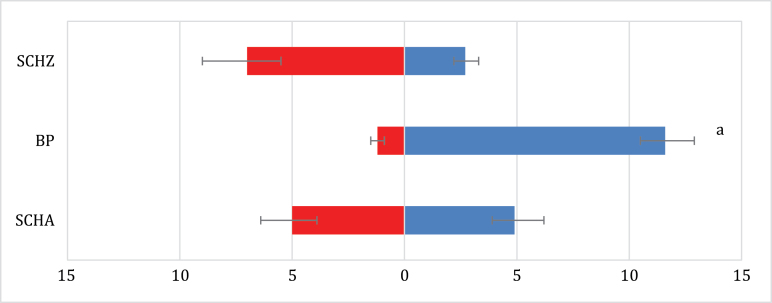
Conversely, individuals first diagnosed with schizophrenia or schizoaffective disorder were 5–7 times more likely to receive a later diagnosis of OCD (figure 1). This finding was largely independent of the prescription of atypical antipsychotics, which are known to sometimes trigger OCD symptoms.21,28 It may be that diagnosis of a psychotic disorder, which often requires hospitalization, increases the surveillance and thus detection of OCD. It is also possible that the progressive brain changes that occur in schizophrenia spectrum disorders39 may increase the risk for developing OCD. Finally, OCD patients with low insight or bizarre symptoms may initially be misdiagnosed as having schizophrenia though the relatively long gap between the diagnoses (3.7 years for schizophrenia and 2.5 for schizoaffective disorder) makes this somewhat less likely.
Fig. 1.
Longitudinal risks of receiving a diagnosis of schizophrenia, schizoaffective disorder, and bipolar disorder after having first received an initial diagnosis of obsessive-compulsive disorder (OCD, right side, in blue), and vice versa (left side, in red). Analyses are limited to ICD-10 diagnoses for all disorders to ensure equal follow-up periods. Values represent risk ratios (RRs) and CIs. SCHZ, schizophrenia; BP, bipolar disorder; SCHZA, schizoaffective disorder. aThe risk of receiving a diagnosis of bipolar disorder after an initial diagnosis of OCD was substantially reduced, but not eliminated, when the use of selective serotonin reuptake inhibitors (but not other types of antidepressants) was controlled for in the analyses (adjusted RR = 8.8, CI = 7.5–10.2). Also see supplementary table 3.
While the high comorbidity between OCD and bipolar disorder has been reported previously,6–8 the longitudinal relation between these disorders has rarely been investigated. The risk of receiving a diagnosis of bipolar disorder after an initial diagnosis of OCD was much greater than the risk of receiving a diagnosis of OCD after an initial diagnosis of bipolar disorder (figure 1). Consistent with the known association between antidepressant use and switch to mania in patients with bipolar disorder,40,41 the risk of receiving a diagnosis of bipolar disorder after an initial diagnosis of OCD was substantially reduced, but not eliminated, when the use of SSRIs (but not other antidepressants) was controlled for. Therefore, OCD may be an important risk factor for the future development of bipolar disorder42 over and above the potential mania-inducing effect of medications. Research into the optimal treatment options for OCD patients who may be at risk of developing bipolar disorders is warranted.
Our multigenerational family analyses provided a rigorous, though not probative, test of the possible etiological link between OCD and the other disorders. These family analyses yielded similar results in outpatients and inpatients with OCD, presumably due to a more rigorous control of potential confounders, such as Berkson’s bias, risk of misdiagnosis, or medication effects. Schizophrenia spectrum disorders and bipolar disorder were significantly more common in OCD-unaffected relatives of probands with OCD compared with relatives of matched comparison subjects. Furthermore, the risks were significantly larger for first-degree relatives (sharing, on average, 50% of the genes) compared with second-degree (sharing, on average, 25% of the genes) and third-degree (sharing, on average, 12.5% of genes) relatives. The risks for full siblings (sharing 50% of the genes) were higher than that of half-siblings (sharing 25% of the genes), particularly for schizophrenia and bipolar disorder. Maternal and paternal half-siblings had comparable risks (both with 25% genetic similarity but with maternal half-siblings sharing more environment),36 suggesting that shared environmental influences may be less important. Taken together, these findings are suggestive of a shared etiology, probably of genetic origin, between OCD and disorders of the schizophrenia and bipolar spectrum. Because gene-searching efforts in OCD are lagging considerably behind, with only 2 small genome-wide association studies published to date,43,44 there may be some value in the targeted exploration of genetic variants already known to confer risk to schizophrenia and bipolar disorder in patients with OCD.
While our results are consistent with a shared etiology between OCD and schizophrenia spectrum and bipolar disorders, disorder-specific genetic and environmental risk factors should not be discounted. For example, the risk of OCD is more than double the risk of schizophrenia spectrum and bipolar disorders in first-degree relatives of probands with OCD,45 suggesting disorder-specific genetic risk factors. Our longitudinal analyses further suggest that other mechanisms, over and above the possible shared genetic risks, may play a role in explaining the high comorbidity between these disorders, including the effects of medication, dynamic brain changes over time, or even possible misdiagnosis. Further longitudinal, etiologically informative studies may help to further tease apart these shared and unique risk factors across these disorders. Ultimately, cross-disorder genome wide association studies will be required to confirm the degree of genetic overlap and disorder specificity. One important challenge will be the known etiological heterogeneity within each of these disorders.46
The biggest limitation of the current study may be that OCD is underrepresented in the Swedish national patient register compared with the other disorders under study. This is largely due to the fact that OCD rarely requires hospitalization (outpatients were only included in the register from 2001) and that many sufferers do not seek help. Therefore, OCD patients with severe comorbidities (eg, psychotic and bipolar disorders) may be more likely to be represented in the register, particularly those who require inpatient admissions, thus inflating the true comorbidity rates and longitudinal associations. However, in general, the results survived when the analyses were restricted to outpatients with OCD. Furthermore, our family-based analyses are less likely to be affected by this limitation because the relatives were matched on the condition that they did not have a lifetime diagnosis of OCD. It is still possible that some relatives may have had OCD but not sought help for it.
To conclude, the high comorbidity, sequential risk, and shared familial risks between OCD and disorders of the schizophrenia and bipolar spectrum are suggestive of partially shared etiological mechanisms between these severe mental disorders. Clinicians should be aware that having OCD might increase the risk of developing other severe mental disorders several years later, particularly bipolar disorder, and vice versa. Careful consideration of the available treatment options (eg, cognitive behavior therapy) to minimize the risk of drug-induced psychopathology would be advisable, and more research in this area is warranted.
Supplementary Material
Supplementary material is available at http://schizophre niabulletin.oxfordjournals.org.
Funding
Swedish Research Council for Health, Working Life and Welfare (project 2012-1678), the Swedish Research Council (2011-2492). The funding organizations had no influence on the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Supplementary Material
Acknowledgments
M.C. and D.M.-C. designed the study. M.C., P.L., H.L., and D.M.-C. had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analyses. M.C. conducted the statistical analyses. M.C. and D.M.-C. drafted the manuscript. All authors critically reviewed successive drafts. The authors have no conflicts of interest relating to this work.
References
- 1. Murphy DL, Moya PR, Fox MA, Rubenstein LM, Wendland JR, Timpano KR. Anxiety and affective disorder comorbidity related to serotonin and other neurotransmitter systems: obsessive-compulsive disorder as an example of overlapping clinical and genetic heterogeneity. Philos Trans R Soc Lond B Biol Sci. 2013;368:20120435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Phillips KA, Stein DJ, Rauch SL, et al. Should an obsessive-compulsive spectrum grouping of disorders be included in DSM-V? Depress Anxiety. 2010;27:528–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tibbo P, Warneke L. Obsessive-compulsive disorder in schizophrenia: epidemiologic and biologic overlap. J Psychiatry Neurosci. 1999;24:15–24. [PMC free article] [PubMed] [Google Scholar]
- 4. Bottas A, Cooke RG, Richter MA. Comorbidity and pathophysiology of obsessive-compulsive disorder in schizophrenia: is there evidence for a schizo-obsessive subtype of schizophrenia? J Psychiatry Neurosci. 2005;30:187–193. [PMC free article] [PubMed] [Google Scholar]
- 5. Eisen JL, Beer DA, Pato MT, Venditto TA, Rasmussen SA. Obsessive-compulsive disorder in patients with schizophrenia or schizoaffective disorder. Am J Psychiatry. 1997;154:271–273. [DOI] [PubMed] [Google Scholar]
- 6. Krüger S, Cooke RG, Hasey GM, Jorna T, Persad E. Comorbidity of obsessive compulsive disorder in bipolar disorder. J Affect Disord. 1995;34:117–120. [DOI] [PubMed] [Google Scholar]
- 7. Hantouche EG, Kochman F, Demonfaucon C, et al. [Bipolar obsessive-compulsive disorder: confirmation of results of the “ABC-OCD” survey in 2 populations of patient members versus non-members of an association]. Encephale. 2002;28:21–28. [PubMed] [Google Scholar]
- 8. Angst J, Gamma A, Endrass J, et al. Obsessive-compulsive syndromes and disorders: significance of comorbidity with bipolar and anxiety syndromes. Eur Arch Psychiatry Clin Neurosci. 2005;255:65–71. [DOI] [PubMed] [Google Scholar]
- 9. Swets M, Dekker J, van Emmerik-van Oortmerssen K, et al. The obsessive compulsive spectrum in schizophrenia, a meta-analysis and meta-regression exploring prevalence rates. Schizophr Res. 2014;152:458–468. [DOI] [PubMed] [Google Scholar]
- 10. Berrios GE. Obsessive-compulsive disorder: its conceptual history in France during the 19th century. Compr Psychiatry. 1989;30:283–295. [DOI] [PubMed] [Google Scholar]
- 11. Tien AY, Eaton WW. Psychopathologic precursors and sociodemographic risk factors for the schizophrenia syndrome. Arch Gen Psychiatry. 1992;49:37–46. [DOI] [PubMed] [Google Scholar]
- 12. Allsopp M, Verduyn C. A follow-up of adolescents with obsessive-compulsive disorder. Br J Psychiatry. 1989;154:829–834. [DOI] [PubMed] [Google Scholar]
- 13. Berman I, Merson A, Viegner B, Losonczy MF, Pappas D, Green AI. Obsessions and compulsions as a distinct cluster of symptoms in schizophrenia: a neuropsychological study. J Nerv Ment Dis. 1998;186:150–156. [DOI] [PubMed] [Google Scholar]
- 14. Poyurovsky M, Hramenkov S, Isakov V, et al. Obsessive-compulsive disorder in hospitalized patients with chronic schizophrenia. Psychiatry Res. 2001;102:49–57. [DOI] [PubMed] [Google Scholar]
- 15. Nechmad A, Ratzoni G, Poyurovsky M, et al. Obsessive-compulsive disorder in adolescent schizophrenia patients. Am J Psychiatry. 2003;160:1002–1004. [DOI] [PubMed] [Google Scholar]
- 16. Cunill R, Castells X, Simeon D. Relationships between obsessive-compulsive symptomatology and severity of psychosis in schizophrenia: a systematic review and meta-analysis. J Clin Psychiatry. 2009;70:70–82. [DOI] [PubMed] [Google Scholar]
- 17. Perugi G, Akiskal HS, Pfanner C, et al. The clinical impact of bipolar and unipolar affective comorbidity on obsessive-compulsive disorder. J Affect Disord. 1997;46:15–23. [DOI] [PubMed] [Google Scholar]
- 18. Perugi G, Toni C, Frare F, Travierso MC, Hantouche E, Akiskal HS. Obsessive-compulsive-bipolar comorbidity: a systematic exploration of clinical features and treatment outcome. J Clin Psychiatry. 2002;63:1129–1134. [PubMed] [Google Scholar]
- 19. Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Timpano KR, Rubenstein LM, Murphy DL. Phenomenological features and clinical impact of affective disorders in OCD: a focus on the bipolar disorder and OCD connection. Depress Anxiety. 2012;29:226–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Scheltema Beduin AA, Swets M, Machielsen M, Korver N. Obsessive-compulsive symptoms in patients with schizophrenia: a naturalistic cross-sectional study comparing treatment with clozapine, olanzapine, risperidone, and no antipsychotics in 543 patients. J Clin Psychiatry. 2012;73:1395–1402. [DOI] [PubMed] [Google Scholar]
- 22. Ghaemi SN, Zarate CA, Jr, Popli AP, Pillay SS, Cole JO. Is there a relationship between clozapine and obsessive-compulsive disorder?: a retrospective chart review. Compr Psychiatry. 1995;36:267–270. [DOI] [PubMed] [Google Scholar]
- 23. Lykouras L, Zervas IM, Gournellis R, Malliori M, Rabavilas A. Olanzapine and obsessive-compulsive symptoms. Eur Neuropsychopharmacol. 2000;10:385–387. [DOI] [PubMed] [Google Scholar]
- 24. Khullar A, Chue P, Tibbo P. Quetiapine and obsessive-compulsive symptoms (OCS): case report and review of atypical antipsychotic-induced OCS. J Psychiatry Neurosci. 2001;26:55–59. [PMC free article] [PubMed] [Google Scholar]
- 25. Alevizos B, Lykouras L, Zervas IM, Christodoulou GN. Risperidone-induced obsessive-compulsive symptoms: a series of six cases. J Clin Psychopharmacol. 2002;22:461–467. [DOI] [PubMed] [Google Scholar]
- 26. Alevizos B, Papageorgiou C, Christodoulou GN. Obsessive-compulsive symptoms with olanzapine. Int J Neuropsychopharmacol. 2004;7:375–377. [DOI] [PubMed] [Google Scholar]
- 27. de Haan L, Beuk N, Hoogenboom B, Dingemans P, Linszen D. Obsessive-compulsive symptoms during treatment with olanzapine and risperidone: a prospective study of 113 patients with recent-onset schizophrenia or related disorders. J Clin Psychiatry. 2002;63:104–107. [DOI] [PubMed] [Google Scholar]
- 28. Kwon JS, Joo YH, Nam HJ, et al. Association of the glutamate transporter gene SLC1A1 with atypical antipsychotics-induced obsessive-compulsive symptoms. Arch Gen Psychiatry. 2009;66:1233–1241. [DOI] [PubMed] [Google Scholar]
- 29. Lichtenstein P, Yip BH, Björk C, et al. Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet. 2009;373:234–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lee SH, Ripke S, Neale BM, et al. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet. 2013;45:984–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wettermark B, Hammar N, Fored CM, et al. The new Swedish Prescribed Drug Register—opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16:726–735. [DOI] [PubMed] [Google Scholar]
- 33. Ekholm B, Ekholm A, Adolfsson R, et al. Evaluation of diagnostic procedures in Swedish patients with schizophrenia and related psychoses. Nord J Psychiatry. 2005;59:457–464. [DOI] [PubMed] [Google Scholar]
- 34. Sellgren C, Landén M, Lichtenstein P, Hultman CM, Långström N. Validity of bipolar disorder hospital discharge diagnoses: file review and multiple register linkage in Sweden. Acta Psychiatr Scand. 2011;124:447–453. [DOI] [PubMed] [Google Scholar]
- 35. Szatmari P, White J, Merikangas KR. The use of genetic epidemiology to guide classification in child and adult psychopathology. Int Rev Psychiatry. 2007;19:483–496. [DOI] [PubMed] [Google Scholar]
- 36.Statistics Sweden. Facts About the Swedish Family: Demographic Reports. Stockholm, Sweden: Statistics Sweden; 1994. www.scb.se/. Accessed May 21, 2012. [Google Scholar]
- 37. Meier SM, Petersen L, Pedersen MG, et al. Obsessive-compulsive disorder as a risk factor for schizophrenia: a nationwide study. JAMA Psychiatry. 2014;71:1215–1221. [DOI] [PubMed] [Google Scholar]
- 38. Sterk B, Lankreijer K, Linszen DH, de Haan L. Obsessive-compulsive symptoms in first episode psychosis and in subjects at ultra high risk for developing psychosis; onset and relationship to psychotic symptoms. Aust N Z J Psychiatry. 2011;45:400–406. [DOI] [PubMed] [Google Scholar]
- 39. DeLisi LE. The concept of progressive brain change in schizophrenia: implications for understanding schizophrenia. Schizophr Bull. 2008;34:312–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry. 2006;163:232–239. [DOI] [PubMed] [Google Scholar]
- 41. Viktorin A, Lichtenstein P, Thase ME, et al. The risk of switch to mania in patients with bipolar disorder during treatment with an antidepressant alone and in combination with a mood stabilizer. Am J Psychiatry. 2014;171:1067–1073. [DOI] [PubMed] [Google Scholar]
- 42. Henin A, Biederman J, Mick E, et al. Psychopathology in the offspring of parents with bipolar disorder: a controlled study. Biol Psychiatry. 2005;58:554–561. [DOI] [PubMed] [Google Scholar]
- 43. Stewart SE, Yu D, Scharf JM, et al. Genome-wide association study of obsessive-compulsive disorder. Mol Psychiatry. 2013;18:788–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mattheisen M, Samuels JF, Wang Y, et al. Genome-wide association study in obsessive-compulsive disorder: results from the OCGAS [published online ahead of print May 13, 2014]. Mol Psychiatry. doi: 10.1038/mp.2014.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mataix-Cols D, Boman M, Monzani B, et al. Population-based, multigenerational family clustering study of obsessive-compulsive disorder. JAMA Psychiatry. 2013;70:709–717. [DOI] [PubMed] [Google Scholar]
- 46. Iervolino AC, Rijsdijk FV, Cherkas L, Fullana MA, Mataix-Cols D. A multivariate twin study of obsessive-compulsive symptom dimensions. Arch Gen Psychiatry. 2011;68:637–644. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.