Abstract
Background
Many neurological diseases are accompanied by an increase in the cerebrospinal fluid (CSF) protein concentration, which indicates dysfunction of the blood-CSF/blood–brain barrier. However, the significance CSF protein concentration of patients with cryptococcal meningitis (CM) is not fully understood. The aim of the present was to determine whether CSF protein concentrations correlated with the responses of patients to treatment with antifungal drugs.
Methods
We conducted a retrospective study of the analytical data of 623 lumbar punctures of 46 patients with CM who were treated at West China Hospital. We divided the patients into groups with good or poor responses to antifungal treatment. We used a generalized linear mixed model (GLMM) to evaluate the significance of the differences between the two groups.
Results
The baseline CSF protein concentrations of the good antifungal response group (GR-group) (median = 0.97 g/L) were higher compared with those of the poor antifungal response group (PR-group) (median = 0.72 g/L). Analysis using the GLMM indicated that the CSF protein concentration of the GR-group decreased at a rate of 1.8 mg/L per day after antifungal treatment started and was 2.1 mg/L higher compared with that of the PR-group.
Conclusions
Compared with poor responders, we found that the baseline CSF protein concentrations of good responders were higher and decreased at faster rate after the initiation of antifungal treatment.
Keywords: Cryptococcal meningitis, Cerebrospinal fluid protein concentration, Antifungal treatment
Background
Cryptococcal meningitis (CM) caused by Cryptococcus neoformans and Cryptococcus gattii [1] is notorious for prolonged treatment and high mortality [2–4]. There is an increasing number of cases caused by Cryptococcus gattii, which infects both immunosuppressed and immunocompetent individuals [5]. In contrast, there are reports of immunocompetent patients infected with C. neoformans [6–8]. This disease imposes a great burden worldwide, particularly in sub-Saharan Africa [3].
Lumbar puncture (LP) is advocated for the diagnosis and management of patients with CM [9, 10]. Analyses of the cerebral spinal fluid (CSF) of patients with CM patients provide a wealth of clinical data acquired through the use of the India ink stain, microbial culture, and biochemical tests. The CSF protein concentration is important as well, because increased concentrations are present in patients with neurological diseases. This condition is referred to as blood-CSF/blood–brain barrier dysfunction [11]. However, the clinical implication of differences in CSF protein concentrations in patients with CM is not fully understood.
The clinical interpretation of the levels of CSF protein concentrations is difficult, because the values change during treatment, and most studies report a single data point data rather than a time course. In the present study, we conducted a retrospective analysis of patients with CM who received antifungal treatment in our hospital and evaluated the clinical implication of the longitudinal data of CSF protein concentrations and the association with patients’ outcomes.
Methods
Patients and definitions
We analyzed the data for 46 patients who were admitted to West China Hospital from 2009 to 2014. CM was diagnosed according to clinical symptoms and a positive culture of the CSF or the results of the India ink stain. Patients with CM were included in this study if they met all the criteria as follows: 1) monitored for more than 30 days, 2) treated with antifungals for no longer than 7 days before admission, 3) not suspected of intracranial infection with other pathogens, and 4) CSF data acquired on a regular basis. All patients were administered antifungal treatment according to ithe guidelines of the Infectious Diseases Society of America [9]. Typically, patients require multiple LPs for regular follow-up after discharge. The Ethics Committee in West China Hospital approved this retrospective study.
LPs and assay of CSF protein concentration
LPs were routinely performed approximately once each week for each patient. The CSF samples were immediately sent to the laboratory and analyzed for cryptococcal antigen, cell counts, and biochemical parameters. India ink staining and fungal cultures were performed as well. The India ink stain, fungal cultures, biochemical tests, and cell counts were compulsory and the other tests were optional. The CSF protein concentration data for each patient were sorted in chronologically with the baseline data (before antifungal treatment) listed first for each patient.
Definitions of patients’ responses to antifungal drugs
We aimed to explore the association between patients’ responses to treatment with antifungal drugs and CSF protein concentrations. Patients were assigned to the poor antifungal response group (PR-group) according to the criteria as follows: persistent positive culture or positive India ink stain of the CSF 30 days after initiation of antifungal therapy. The other patients were assigned to the good antifungal response group (GR-group).
Statistical analysis
A generalized linear mixed model (GLMM) was used for the statistical analysis. This model is suitable for analyzing repeated measures data [12]. The data acquired using the GLMM were analyzed using R software [13] and the nlme [14] and ggplot2 [15] packages. The values of categorical variables are represented as frequencies, and the values of continuous variables are presented as the mean, standard deviation (SD), range, or median values. The Student t test and the Wilcoxon rank sum test were used to evaluate the significance of differences between the values of continuous variables. Spearman’s rank correlation test was used to test bivariate correlations. The Fisher’s exact test were used to evaluate the significance of differences between the values of categorical variables.
Results
There were no significant differences between age, sex, and underlying diseases of the GR and PR groups (Table 1). The observation periods ranged from 32 days to 457 days. Patients received antifungal treatment within several days after admission. Two patients died while hospitalized.
Table 1.
Demographics and underlying diseases of patients with CM
| Variables | PR-group (n = 28) | GR-group (n = 18) | P-value |
|---|---|---|---|
| Age, year | |||
| Mean/SD | 35.07/12.48 | 41.00/13.67 | 0.15 |
| Range (min-max) | 16-60 | 18-67 | - |
| Sex, male | 19(67.9 %) | 13(72.2 %) | 1.00 |
| Diabetes mellitus | 2(7.14 %) | 2(11.1 %) | 0.63 |
| Kidney diseases | 1(3.57 %) | 0(0.00 %) | 1.00 |
| Autoimmune diseases | 3(10.7 %) | 2(11.1 %) | 1.00 |
| HIV positive | 2(7.14 %) | 2(11.1 %) | 0.64 |
| Malignancy | 1(3.57 %) | 0(0.00 %) | 1.00 |
| Hypertension | 0(0.00 %) | 1(5.56 %) | 0.43 |
| Respiratory infection | 8(28.6 %) | 4(22.2 %) | 0.74 |
| Cardiovascular diseases | 1(3.57 %) | 0(0.00 %) | 1.00 |
| HBV positive | 4(14.3 %) | 1(5.56 %) | 0.64 |
Clinical treatment of patients with CM employs amphotericin B (AMB) and flucytosine to decrease the fungal burden in the central nervous system (CNS) [16]. To achieve a better outcome, most patients receive treatment that includes AMB [17]; however, we found that the implementation of antifungal strategies varied because of practical considerations such as costs, side effects, and availability of drugs (e.g. flucytosine was temporarily unavailable). The antifungal strategies are listed in Table 2, and analysis using the Fisher's exact test did not reveal significant differences between the groups.
Table 2.
Antifungal treatment strategies
| Antifungal strategies | PR-group (n = 28) | GR-group (n = 18) | P-value |
|---|---|---|---|
| AMB | 1(3.57 %) | 1(5.56 %) | 1.00 |
| AMB+ flucytosine | 5(17.9 %) | 5(27.8 %) | 0.73 |
| AMB+ fluconazole | 5(17.9 %) | 2(11.1 %) | 0.70 |
| AMB+ fluconazole + flucytosine | 13(46.2 %) | 7(38.9 %) | 0.79 |
| AMB+ voriconazole | 0(0.00 %) | 1(5.56 %) | 0.44 |
| Fluconazole | 3(10.7 %) | 0(0.00 %) | 0.29 |
| Fluconazole + flucytosine | 0(0.00 %) | 2(11.1 %) | 0.17 |
| Voriconazole | 1(3.57 %) | 0(0.00 %) | 0.62 |
Responses to antifungal treatment
Thirty days after initiating antifungal treatment, the CSFs of 18 (39.1 %) of 46 good responders were sterile, and the India ink stains were positive for the other 28 (60.9 %) patients. However, the clinical responses of the groups did not correspond completely with the CSF data described below.
CSF protein concentrations
Analysis using the Wilcoxon rank sum test revealed significant difference between the median values of baseline CSF protein concentrations of the groups (P = 0.04) (Fig. 1). The median value of the CSF protein concentration of patients in the good response group was 0.97 g/L and was >0.45 g/L (the upper limit of the normal value) for 16 patients (88.8 %). In contrast, median value of the CSF protein concentrations of patients in the poor antifungal response group was 0.72 g/L, and the CSF protein concentrations were >0.45 g/L for 18 (64.2 %) patients.
Fig. 1.

Baseline CSF protein concentrations. The difference between groups was statistically significant (P = 0.04). *G: GR-group; P: PR-group
Analysis using the GLMM revealed the relationship between CSF protein concentrations and time (Fig. 2). Further, the data indicated that the CSF protein concentrations of patients in the good antifungal response group decreased at an average rate of 1.8 mg/L per day after antifungal therapy started. This value was 2.1 mg/L higher compared with that of the poor antifungal response. The CSF protein concentration of the GR-group before antifungal treatment was 0.8500 g/L, 0.3221 g/L higher compared with that of the PR-group (Table 3). These results indicate that the CSF protein concentrations were higher among the patients in the good antifungal response group before therapy started and that the concentrations decreased faster compared with those among patients in the poor antifungal response group (Fig. 2).
Fig. 2.
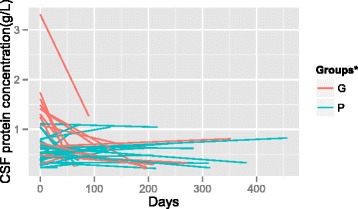
CSF protein concentrations after initiation of antifungal therapy. *G: GR-group; P: PR-group
Table 3.
Parameters of the GLMM estimation
| Parameters | Estimation | SE | P-value |
|---|---|---|---|
| Intercept | 0.8500 | 0.0755 | 0.0000 |
| Time (days) | −0.0018 | 0.0004 | 0.0000 |
| Groups# | −0.3221 | 0.0847 | 0.0004 |
| Times (days) by Groups# | 0.0021 | 0.0005 | 0.0000 |
#0 = GR-group; 1 = PR-group
Discussion
We show here that patients in the good antifungal response group had higher baseline CSF protein concentrations, which indicates an increased inflammatory response in the CNS [18]. A plausible hypothesis to explain the data is that the intensity of the inflammatory response influences the antifungal response, and the CSF protein concentrations simply represent the intensity of inflammatory responses. Another study of patients with CM found that those infected with hepatitis B virus (HBV) had lower CSF white blood cell (WBC) counts and lower percentages of total protein in the CSF > 0.45 g/L, indicating a lower intensity of immune inflammation compared with patients with CM who were not infected with HBV who had a lower survival rate [19]. These findings indicate a correlation between the intensity of inflammatory responses and clinical outcomes.
A prospective study of patients with CM indicates that the baseline number of CSF colony-forming units (CFUs) is a prognostic factor, because patients with a lower number of CSF CFUs had better clinical outcomes [20]. Another study found a negative correlation between protein concentrations and fungal burdens in the CSF [21]. The higher baseline CSF protein concentrations reported here indicate a lower fungal burden, which indicated a better antifungal response. Others found that a higher WBC correlates with a good clinical response [21, 22] as well as a positive correlation between WBC count and CSF protein concentration was found in this study(Spearman’s rank correlation: R = 0.34, P = 0.00). Because drug concentrations in the CSF may be higher during inflammation of the CNS compared with those of patients without inflammation [23, 24], an elevated CSF protein concentration might indicate a higher level of inflammation that increases the transport of AMB to the CNS [24]. The rapid decrease of the CSF protein concentration in the GR-group indicates faster attenuation of inflammation, which led to a more effective antifungal response.
There are differences between the findings of the present study and those of other reports. For example, Lu et al., (1999) reported no significant difference in CSF protein concentrations between treatment failures and cured or improved groups [22]. However, the value of a single LB was not sufficient to evaluate the significance of changes in CSF protein concentrations during treatment. The difference may be attributed to the type of data analysis used compared with that of the present study. In the present study, we determined the time course of changes in CSF protein concentrations. Patients with CM are frequently immunocompromised, for example, those with infected with HIV [1]. However, only four (8.70 %) patients studied here were infected with HIV, which is lower compared with the rates reported by others [25]. The multiple polymorphisms in the genes encoding mannose-binding lectin and the Fc-gamma receptor 2B (FCGR2B) in the Han population, which is the largest ethnic group in China, might contribute to the discrepancies between studies [26]. The mortality rates (4.34 %) of patients treated at our hospital are lower compared with those of other studies [1]. The lower proportion of HIV-related infections may explain the discrepancy as well, and observations over eight years reveal that mortality rates are lower for patients with CM who are not infected with HIV [27].
Conclusions
The present study supports the hypothesis that there is a correlation between antifungal responses and CSF protein concentrations. These findings must be confirmed by prospective studies of larger numbers of patients. However, we recommend that the treatment of patients with CM should include detailed analyses of CSF protein concentrations with focus on their variability.
Acknowledgments
We thank the staff of the Center of Infectious Diseases, West China Hospital, Sichuan University for management of patients and maintenance of the clinical data. We thank the Information Center of West China Hospital, Sichuan University for data retrieval. This study was supported by funding provided by the West China Hospital, Sichuan University.
Abbreviations
- CFUs
Colony-forming units
- SD
Standard deviation
- SE
Standard error
- WBC
White blood cell
- HIV
Human immunodeficiency virus
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
H.L. and L.X. designed the study; H.L. Y.H. QJ. Liu Yanbin Z.C. T.G. Liu Ying, and Y.Y. collected data; H.L. Y.H. and L.X. wrote the manuscript; H.L. analyzed the data; and all authors read and approved the final manuscript.
Contributor Information
Liang Huang, Email: 2013324020009@stu.scu.edu.cn.
Hui Ye, Email: yehuidt@163.com.
Junyan Qu, Email: 371402610@qq.com.
Yanbin Liu, Email: 439089407@qq.com.
Cejun Zhong, Email: barryzcj@163.com.
Guangmin Tang, Email: 52930382@qq.com.
Ying Liu, Email: 113445865@qq.com.
Yao Huang, Email: 18990385310@qq.com.
Xiaoju Lv, Email: lv.xiao.ju@hotmail.com.
References
- 1.Sloan DJ, Parris V. Cryptococcal meningitis: epidemiology and therapeutic options. Clin Epidemiol. 2014;6:169–182. doi: 10.2147/CLEP.S38850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meda J, Kalluvya S, Downs JA, Chofle AA, Seni J, Kidenya B, et al. Cryptococcal meningitis management in Tanzania with strict schedule of serial lumber punctures using intravenous tubing sets: an operational research study. J Acquir Immune Defic Syndr. 2014;66(2):e31–36. doi: 10.1097/QAI.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 3.Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. Aids. 2009;23(4):525–530. doi: 10.1097/QAD.0b013e328322ffac. [DOI] [PubMed] [Google Scholar]
- 4.Orsini J, Blaak C, Mahmoud D, Young-Gwang J. Massive cerebral edema resulting in brain death as a complication of Cryptococcus neoformans meningitis. J Community Hosp Intern Med Perspect. 2015;5(1):26098. doi: 10.3402/jchimp.v5.26098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Franco-Paredes C, Womack T, Bohlmeyer T, Sellers B, Hays A, Patel K, et al. Management of Cryptococcus gattii meningoencephalitis. Lancet Infect Dis. 2014;15(3):348–55. doi: 10.1016/S1473-3099(14)70945-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newsome J, Nguyen D. Cryptococcal meningitis caused by Cryptococcus neoformans in an immunocompetent soldier. Mil Med. 2014;179(9):e1059–1061. doi: 10.7205/MILMED-D-14-00020. [DOI] [PubMed] [Google Scholar]
- 7.Niknam N, Niknam N, Dushaj K, Restrepo E. A case of recurrent cryptococcal meningoencephalitis in an immunocompetent female. Case Rep Infect Dis. 2014;2014:407348. doi: 10.1155/2014/407348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Day JN, Hoang TN, Duong AV, Hong CT, Diep PT, Campbell JI, et al. Most cases of cryptococcal meningitis in HIV-uninfected patients in Vietnam are due to a distinct amplified fragment length polymorphism-defined cluster of Cryptococcus neoformans var. grubii VN1. J Clin Microbiol. 2011;49(2):658–664. doi: 10.1128/JCM.01985-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2010;50(3):291–322. doi: 10.1086/649858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gaskell KM, Rothe C, Gnanadurai R, Goodson P, Jassi C, Heyderman RS, et al. A prospective study of mortality from cryptococcal meningitis following treatment induction with 1200 mg oral fluconazole in Blantyre Malawi. PLoS One. 2014;9(11):e110285. doi: 10.1371/journal.pone.0110285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huhmer AF, Biringer RG, Amato H, Fonteh AN, Harrington MG. Protein analysis in human cerebrospinal fluid: Physiological aspects, current progress and future challenges. Dis Markers. 2006;22(1–2):3–26. doi: 10.1155/2006/158797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cnaan A, Laird NM, Slasor P. Using the general linear mixed model to analyse unbalanced repeated measures and longitudinal data. Statist Med. 1997;16(20):2349–2380. doi: 10.1002/(SICI)1097-0258(19971030)16:20<2349::AID-SIM667>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 13.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria. 2014. http://www.R-project.org/.
- 14.Pinheiro J, Bates D, DebRoy S, Sarkar D, R Core Team: (nlme): Linear and Nonlinear Mixed Effects Models. 2014; Vol. R package version 3.1-118. http://CRAN.R-project.org/package=nlme.
- 15.Wickham H. ggplot2: Elegant graphics for data analysis. Springer New York, 2009. http://had.co.nz/ggplot2/book.
- 16.van der Horst CM, Saag MS, Cloud GA, Hamill RJ, Graybill JR, Sobel JD, et al. Treatment of cryptococcal meningitis associated with the acquired immunodeficiency syndrome. National Institute of Allergy and Infectious Diseases Mycoses Study Group and AIDS Clinical Trials Group. N Engl J Med. 1997;337(1):15–21. doi: 10.1056/NEJM199707033370103. [DOI] [PubMed] [Google Scholar]
- 17.Day JN, Chau TT, Lalloo DG. Combination antifungal therapy for cryptococcal meningitis. N Engl J Med. 2013;368(26):2522–2523. doi: 10.1056/NEJMc1305981. [DOI] [PubMed] [Google Scholar]
- 18.Mak W, Cheng TS, Chan KH, Cheung RT, Ho SL. Cerebrospinal fluid to serum glucose ratio in non-hypoglycorrhachic neurological conditions. Hong Kong Med J. 2005;11(6):457–462. [PubMed] [Google Scholar]
- 19.Zhong YH, Tan F, Li M, Liu J, Wang X, Yuan Y, et al. Comparisons of presentations and outcomes of cryptococcal meningitis between patients with and without hepatitis B virus infection. IJID. 2014;20:31–36. doi: 10.1016/j.ijid.2013.11.017. [DOI] [PubMed] [Google Scholar]
- 20.Brouwer AE, Rajanuwong A, Chierakul W, Griffin GE, Larsen RA, White NJ, et al. Combination antifungal therapies for HIV-associated cryptococcal meningitis: a randomised trial. Lancet. 2004;363(9423):1764–1767. doi: 10.1016/S0140-6736(04)16301-0. [DOI] [PubMed] [Google Scholar]
- 21.Jarvis JN, Bicanic T, Loyse A, Namarika D, Jackson A, Nussbaum JC, et al. Determinants of mortality in a combined cohort of 501 patients with HIV-associated Cryptococcal meningitis: implications for improving outcomes. Clin Infect Dis. 2014;58(5):736–745. doi: 10.1093/cid/cit794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lu CH, Chang WN, Chang HW, Chuang YC. The prognostic factors of cryptococcal meningitis in HIV-negative patients. J Hosp Infect. 1999;42(4):313–320. doi: 10.1053/jhin.1998.0610. [DOI] [PubMed] [Google Scholar]
- 23.Kethireddy S, Andes D. CNS pharmacokinetics of antifungal agents. Expert Opin Drug Metab Toxicol. 2007;3(4):573–581. doi: 10.1517/17425255.3.4.573. [DOI] [PubMed] [Google Scholar]
- 24.Nau R, Sörgel F, Eiffert H. Penetration of Drugs through the Blood-Cerebrospinal Fluid/Blood–brain Barrier for Treatment of Central Nervous System Infections. Clin Microbiol Rev. 2010;23(4):858–883. doi: 10.1128/CMR.00007-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pyrgos V, Seitz AE, Steiner CA, Prevots DR, Williamson PR. Epidemiology of cryptococcal meningitis in the US: 1997–2009. PLoS One. 2013;8(2):e56269. doi: 10.1371/journal.pone.0056269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fang W, Fa Z, Liao W. Epidemiology of Cryptococcus and cryptococcosis in China. Fungal Genet Biol. 2014;78:7–15. doi: 10.1016/j.fgb.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 27.Abhilash K, Mitra S, Arul J, Raj PM, Balaji V, Kannangai R, et al. Changing paradigm of Cryptococcal meningitis: An eight-year experience from a tertiary hospital in South India. Indian J Med Microbiol. 2015;33(1):25–29. doi: 10.4103/0255-0857.148372. [DOI] [PubMed] [Google Scholar]


