Abstract
The ideal shape and height of the double eyelid varies widely depending on the patient and the culture. Patients may be dissatisfied after a double eyelid operation for the following reasons: scar, low versus high fold, shallow versus deep fold, triple folds, pretarsal fullness, ptosis, and asymmetry. Here the author describes the complications experienced after double eyelid surgery and corrective procedures.
Keywords: revision blepharoplasty, complication of double eyelid operation
Aesthetic standards for eyelids vary across ethnic groups and cultures. Although a certain contemporary aesthetic standard may be satisfactory to large numbers of patients, complications after double eyelid operations are specific to each individual patient. As such, I believe that an outcome that fails to meet realistic patient expectations qualifies as a practical definition for a complication of an aesthetic operation.
In the context of East Asian blepharoplasty, the most common complications are scar, problems of crease height (low vs high), fold depth (shallow vs deep), extraneous creases (triple folds), pretarsal fullness, ptosis, and asymmetry. In this chapter, I identify either the mistake or the problem behind each complication, describe its causes, and present the solution.1
Scars
Eyelid skin does not develop a hypertrophic response in most cases. Therefore, in many instances, the problem is not with the patient, but with the surgeon who has performed the index operation. A common mistake is leaving sutures in for more than 5 days. Stich marks from delayed suture removal are unacceptable. In younger patients, skin excisions do not have to be extended along the full length of the eyelid to create a crease of desired length. A shorter incision design is usually sufficient. Eyelid scars are more noticeable when they are depressed. Such scars result from excessive removal of the orbicularis muscle or connective tissue or from deep fold/ectropion (Fig. 1).
Fig. 1.
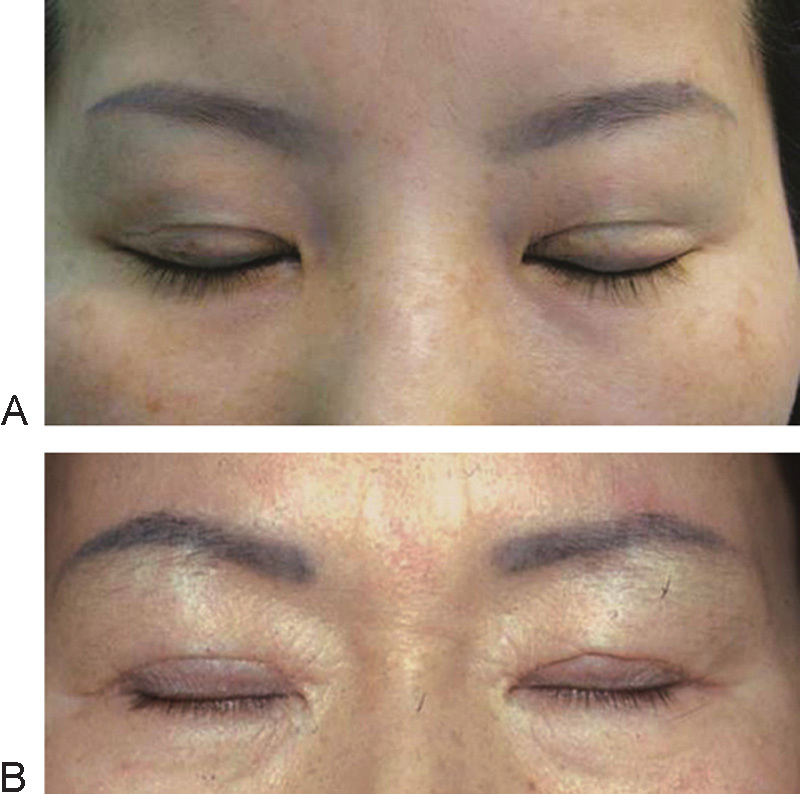
Postoperative depressed scar. (A) Caused by pretarsal oculi muscle excision. (B) Caused by ectropion.
Scar Revision
The operation must remain as precise as possible. All layers—not just skin—should be approximated with as little tension as possible because skin tension can make a wide and depressed scar. The missing layer of orbicularis oculi must be reconstructed by undermining and advancing the muscle edges from both the upper and lower flaps. An eversion suture is necessary to make a flat scar, and not a depressed scar.
Depth Problems
All surgically created eyelid creases attenuate during the first few months. This change might be minimal, or the fold might disappear altogether. The degree to how much a postoperative fold softens is determined by patient characteristics and surgical techniques. Patient-related factors that promote softening or loss of crease are (1) thick skin and abundant soft tissue, (2) blepharoptosis, (3) a sunken eyelid, (4) enophthalmos, (5) a previous history of failed double eyelid operation, (6) younger age, (7) the presence of an epicanthal fold, and( 8) extreme weight gain. These factors may lead to a high degree of fold-resistant eyelid. Operative factors associated with technical failure are (1) inaccurate approximation of connective tissue, (2) insufficient fixation to the tarsal plate, (3) low-set fixation, and (4) loosening of the fixation due to hematoma or edema. Inadequate soft tissue removal along the top margin of the tarsal plate can prevent close approximation of the connective tissue. A surgically created eyelid fold is a consequence of the adhesion between the anterior and posterior lamella. Postoperative folds can soften and/or disappear over time because of repetitive eyelid movements. To prevent such losses, the adhesions—not the suture material—must be stronger.
Preventing Loss of a Surgically Created Fold
To prevent the loss of folds, the suture must be tied while avoiding the intrusion of soft tissue between the levator aponeurosis and dermis or the orbicularis muscle into the loop. If a patient has fold-resistant eyelids, it is important to create a fold that is deep enough to result in the slight ectropion, which will subside within a short postoperative duration. Excessively deep fixations can result in persistent ectropion, even if the fold becomes shallower over time.
Correction of a Shallow Fold
At times, there is extraneous fat or connective tissue in the pretarsal space. This is especially common in the medial side of the upper eyelid, where pretarsal fat is abundant. Partial resection of this connective tissue can aid in forming an adhesion. If a patient has blepharoptosis or a definite epicanthal fold, these elements must be dealt with first to reduce fold resistance. Otherwise, a deeper fold is necessary. If there is adhesion in the lower flap with softening of the fold, the adhesion will interfere with the formation of the new crease. As such, the lower flap must be released and redraped prior to tarsal fixation. In patients whose eyelid skin lacks the elasticity after the previous operation, the newly created fold should be deeper than usual to prevent a repetitive loss of fold.
Deep Folds or Ectropion
Deep folds and ectropion are caused by creases that were fixated too high on the eyelid. Unfortunately, this will place an undue upward tension on the lower flap and evert the eyelid margin. A patient often complains about the unintended but aggressive impression of the everted eyelids. The depressed scar is visible when the eyes are closed. The patient may also complain of a tugging sensation in the eyelids. In cases of severe ectropion, the mucous membrane is exposed. The mucocutaneous junction becomes keratinized—leading to dry eye syndrome.
Correction of a Deep Fold or Ectropion
The first step in correcting the fold depth is to release the adhesions and reapproximate the layers at a lower point along the eyelid. If this first part of the operation does not resolve the ectropion, the lower flap must be undermined and redraped over the tarsal plate to decrease the everting force of the adhesion in the lower flap.
Crease Height
Low Crease
A crease that is too low will show very little skin between the eyelid margin and the crease. This is usually a problem of the actual crease design being too low, but a shallow fold also can sometimes give the appearance of a low crease. Redundancy of skin can also make a crease lower than it really is.
Correction of a Low Crease
There are three approaches to correcting a low fold. The first is an open blepharoplasty by which the skin and orbicularis muscle is excised above the previous crease. The second approach is to create a mechanically overriding crease above the previous one. The third combines soft tissue excision and higher crease formation above the prior crease (Fig. 2).
Fig. 2.
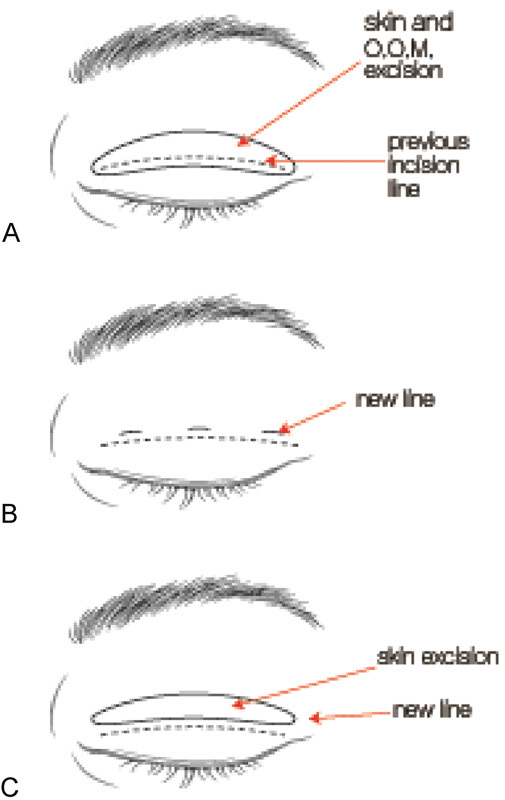
Corrective methods for low fold. (A) Excision of drooping skin and orbicularis oculi muscle. (B) Minimal incision method above the previous line. (C) Combination of A and B. OOM, orbicularis oculi muscle.
The first approach (open blepharoplasty) can incorporate scar revision and allows for the excision of redundant skin in older patients. The second approach (tarsal fixation) allows considerable elevation of the fold crease, but will create an additional scar if secondary incisions were necessary. This approach is more appropriate for patients who have inconspicuous scars from the first operation and wish for the eyelid fold to be higher. The combined approach of open blepharoplasty and mechanical fixation is reserved for patients with very low folds and great redundancy of skin.
High Crease
In many East Asian cultures, a high eyelid crease is associated with an aggressive or antagonistic personality.2 High creases are usually accompanied by deep folds, and patients complain of an unnatural appearance, a depressed scar, and excessive eversion of eyelashes. Patients may also complain about pretarsal fullness that has not improved with time. Slight blepharoptosis can be seen in patients with an adhesion between the skin and the levator aponeurosis that prevents recursion of the levator muscle.
Causes of a High Crease
High creases can be caused by high skin crease design, high fixation, excessive skin excision, unintended adhesion, blepharoptosis, or a sunken eyelid. Among these, high crease design from the initial operation is the most common (Fig. 3A). Fixation of the lower flap to a high point can result in high folds with ectropion (Fig. 3B). The problem can also result from excessive skin resection, which leaves insufficient skin to cover the crease.
Fig. 3.

High fold (A) caused by high crease design and (B) caused by high point fixation.
High creases can be observed with deep, normal, or shallow fold depths. The most common form type is a fold that is both high and deep, which is often accompanied by ectropion. At times, patients might have folds of varying depth (i.e., a fold that is shallow on the medial side, but deep over the pupils).
Correction of a High Crease
As with all things, high creases should be corrected according to the cause. Generally, the secondary operation incorporates an open blepharoplasty with skin excision. The upper margin of this excision is along the fold that is to be revised, and the lower margin marks the new crease height. If the skin lacks redundancy and lagophthalmos is expected, skin is not resected. Rather, a lower incision can be used to undermine the upper flap and release the high fold through either the preaponeurotic layer or preseptal layer. Deep folds respond to dissection of the upper flap. However, a deep fold may remain even with adequate release beneath the upper flap. In such situations, the lower flap might also contribute to fold depth and should be released from the underlying tissue. The lower flap should then be fixed at the lower height. This also addresses the problem of ectropion, if present. High creases with neutral fold depth can be addressed by simple open blepharoplasty, as described above. High crease and shallow eyelid folds are corrected in a similar manner to neutral folds by open blepharoplasty. The lower flap may also have severe adhesions on the lower flap, requiring adhesiolysis and adequate fixation at the desired height.
Failures after Correction of a High Crease
The two major problems that occur after high fold correction are ectropion and multiple folds. Failure rates for high fold correction can be unacceptable. The technical consequence is that surgeons do not completely release the tissue around the old eyelid crease. The secondary reason for failure is from re-adhesion of the tissue that was adequately freed. The problem of triple folds is so common that it is discussed as its own topic later in this chapter.
To prevent these secondary complications, the surgeon must maintain sufficient tissue volume, thoroughly free the adhered tissue planes, and make efforts to prevent readhesion. To accomplish this, it is important to resect only the skin and leave the scar tissue to reinforce the upper flap (Fig. 4). Other procedures for the prevention of triple folds are mentioned in the section on triple folds.
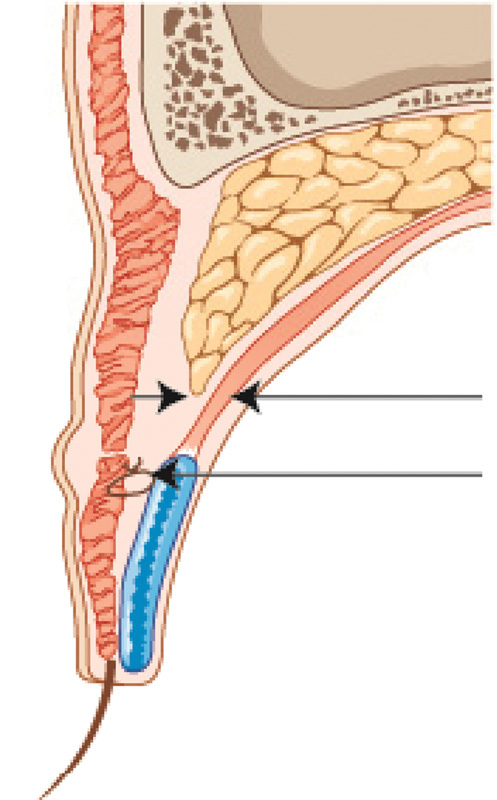
Fig. 4.
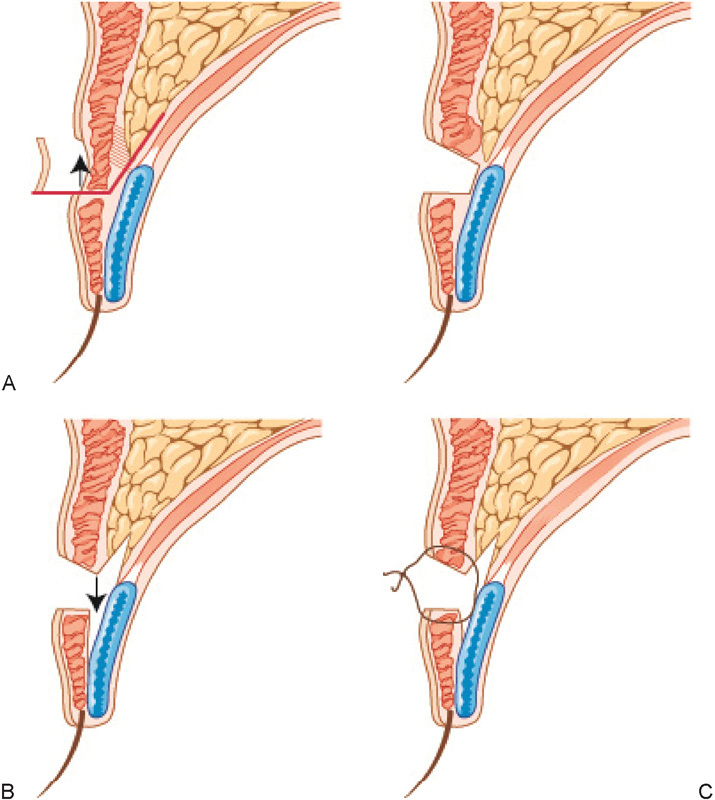
(A–C) High fold correction. (A) Skin is resected (width is from new planned incision to previous high fold incision). Internal scar tissue is left in place with the upper flap to add volume. (B) The scarred tissue plane is released immediately anterior to tarsus and levator aponeurosis. (C) New lower level crease formation is performed with surgeon's technique of choice.
Pretarsal Fullness
Commonly, pretarsal fullness observed with high creases. Pretarsal fullness is also described as “sausage eyelid” among Korean patients. It refers to the unwanted soft tissue projection in the area over the tarsal plate in postblepharoplasty eyelids. Preoperative factors that predict pretarsal fullness include thick eyelid skin and orbicularis muscle. Patients with these features should receive eyelid folds that are designed lower than usual to counteract this propensity.
Pretarsal fullness increases in proportion to the square of the height of the pretarsal soft tissue compartment, which implies that small changes in height can result in great changes in volume of this compartment (Fig. 5). For example, an eyelid crease that changes the height from 4 to 3 mm when opening the eye will have a volume reduction close to 50% (9/16).
Fig. 5.
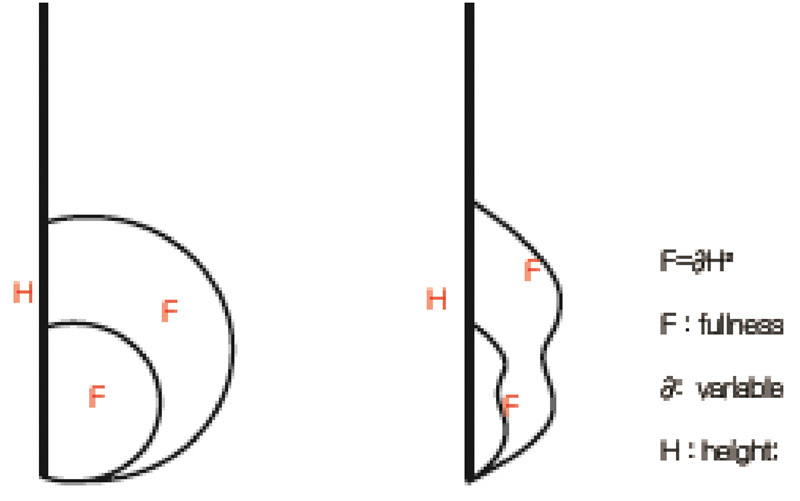
Pretarsal fullness. Relationship between eyelid crease height and pretarsal fullness.
Correction of Pretarsal Fullness
A common misconception is that pretarsal fullness can be corrected by removing the contents of the pretarsal compartment, such as the pretarsal portion of orbicularis muscle. This attempt at reducing volume is futile. To decrease the soft tissue volume in the pretarsal area, one must recognize the heigh–volume relationship mentioned above. Once this principle is understood, the technical solution is to perform a secondary operation (open blepharoplasty) to lower the crease and effectively reduce the height and volume of the pretarsal soft tissue compartment.
Asymmetry
From the perspective of clinical management, there are two main causes of postoperative eyelid asymmetry. Inexperienced surgeons often operate on a pre-existing asymmetry that was not noticed during the preoperative examination. A thorough examination should include palpebral fissure height, redundancy of the eyelid skin, height of the brow, and unequal eyelashes. A less common cause of eyelid asymmetry is technical failure on the part of the surgeon, whose operative maneuvers are not consistent from the left to the right eyelid.
Multiple Creases (Triple Folds)
Multiple eyelid creases, or triple folds, can form from various reasons and can be classified by clinical presentation. Primary triple folds are found in patients without any prior surgical history and are caused by the loss of fat volume (subcutaneous or deep fat) in the upper eyelid above a naturally existing supratarsal fold. Secondary triple folds are present in patients after the index blepharoplasty. Overzealous soft tissue removal in the upper flap can create adhesion and subsequently result in the extra eyelid crease above the surgically created fold.3 In particular, removal of the medial retro-orbicularis oculi fat (ROOF) may lead to a triple fold and should be avoided as much as possible. At times, pretarsal or the preaponeurotic soft tissue is removed to facilitate adhesion and formation of an eyelid crease. However, removal of this tissue above the point of fixation should be avoided because doing so may result in triple fold formation (Fig. 6). Tertiary triple folds form after secondary operations for correction of high fold, ectropion, or eyelid retraction. The extra creases are all consequences of re-adhesion of the deconstructed fold (Fig. 7).
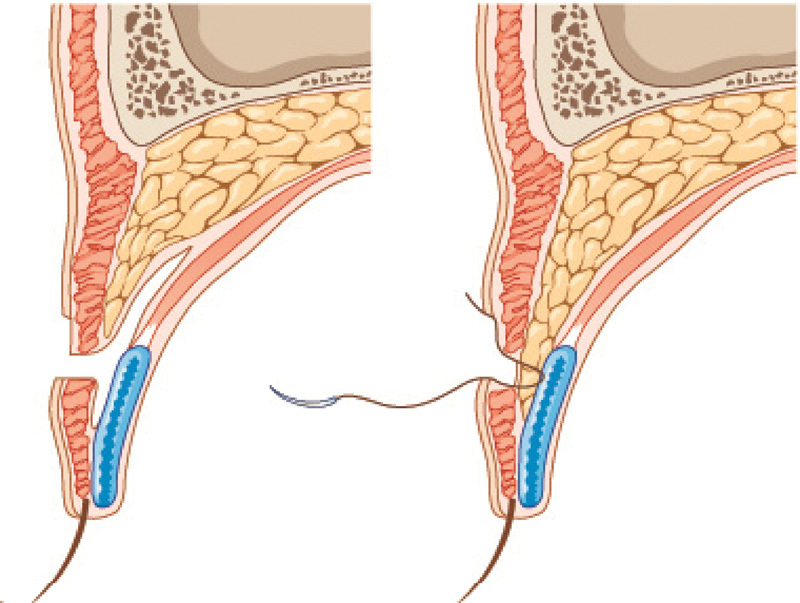
Fig. 6.

Mechanism of triple fold after primary operation.
Fig. 7.
Mechanism of triple fold after high fold or ectropion correction.
Correction of Multiple Creases (Triple Folds)
If the extraneous crease is shallow, fat injection alone might be enough to bolster the skin and prevent further progression of the crease. In most cases, open access is required for the meticulous release of adhesions and to perform preventive measures. The upper flap should be released between the levator aponeurosis and orbital septum. Usually, this is sufficient in itself in releasing the adhesion forming the extraneous crease. If not, the space between the postorbicularis fascia and the orbital septum should be cleared for additional separation of outer and inner elements. Readhesion is prevented by the inferior displacement of a well-organized septum and orbital fat between the orbicularis oculi and the levator aponeurosis (Fig. 8).4 The postorbicularis fascia and muscle is lowered from its previous site of adhesion and anchored to the tarsal plate (Fig. 9). Another method to prevent readhesion is to create a roll with the skin and orbicularis oculi muscle of the upper flap: Pass the needle under and through the skin and orbicularis oculi just beneath the crease, then through the orbicularis oculi and skin of the upper flap creating a slightly bunched kind of roll; applying adhesive tape to an area in high risk of triple fold can also be effective (Fig. 10).5 Postoperative blepharoptosis can co-exist with multiple creases. In such cases, early corrective operation of ptosis is effective in separating the anterior and posterior portions thath were previously adhered.
Fig. 8.
Orbital fat transposition.
Fig. 9.
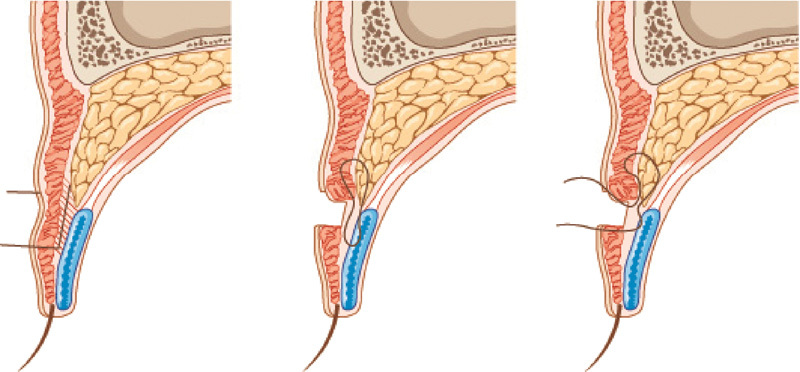
Triple fold correction method with posterior oculi muscle fascia and muscle pulled low and anchored to the tarsal plate.
Fig. 10.

Triple fold correction method with DuoDERM (ConvaTec, Skillman, NJ) strip applied and skin roll formation.
Removal of an Eyelid Fold
Several facts must be presented by the surgeon and those facts understood by the patient before an operation is performed to remove a surgically created eyelid fold. The first fact is that a visible scar will be present even when the eyes are open. The second is that the fold can reappear with time. The third is that the eyelid may appear and feel bulkier due to the scar tissue, injection of fat graft, or inferior displacement of fat and septum down to the area in risk of readhesion. Because of these potential issues, I usually recommend an inner eyelid fold rather than total removal of eyelid fold. Inner eyelid folds are created in a similar manner to the operation correcting high creases. The adhesion forming the existing crease is deconstructed, and orbital fat and septum is interposed between the layers to prevent readhesion. Eversion should be achieved during skin closure. The incision site is taped for longer than the usual 3 to 5 days.
Conclusion
Blepharoplasty complications are too numerous and varied to allow a comprehensive discussion within a chapter. However, the basic principles of reconstructive surgery are applicable to a majority of these complications. The first principle is to understand the normal and abnormal function and anatomy of the eyelid. The second principle is to undo, or deconstruct, the postoperative tissue changes causing the complication. The third principle is to redo the initial operation without making the same mistake.
References
- 1.Cho I C The Art of Blepharoplasty Seoul, South Korea: Koonja Publishing; 201384–124. (in Korean) [Google Scholar]
- 2.Chang S H, Chen W P, Cho I C, Ahn T J. Comprehensive review of Asian cosmetic upper eyelid oculoplastic surgery: Asian blepharoplasty and the like. Arch Aesthet Plast Surg. 2014;20(3):129–139. [Google Scholar]
- 3.Chen W P. The concept of a glide zone as it relates to upper lid crease, lid fold, and application in upper blepharoplasty. Plast Reconstr Surg. 2007;119(1):379–386. doi: 10.1097/01.prs.0000244908.04694.32. [DOI] [PubMed] [Google Scholar]
- 4.Kim Y W, Park H J, Kim S. Revision of unfavorable double eyelid operation by repositioning of preaponeurotic fat. J Korean Soc Plast Reconstr Surg. 2000;27:99–104. [Google Scholar]
- 5.Lew D H, Kang J H, Cho I C. Surgical correction of multiple upper eyelid folds in East Asians. Plast Reconstr Surg. 2011;127(3):1323–1331. doi: 10.1097/PRS.0b013e318205f32b. [DOI] [PubMed] [Google Scholar]


