Abstract
The preoperative comprehensive evaluation of aging Asian patients seeking an Asian upper blepharoplasty and brow lift is imperative and should be performed meticulously. There are many methods of upper Asian face rejuvenation. Among them, the proper selection of operative technique is necessary. The operative technique for an aging Asian upper blepharoplasty and brow lift should be performed based on anatomical structures and their relationship. Modifications to the procedure are correlated with the degree of periorbital aging. The height of double fold in an aging Asian upper blepharoplasty should not exceed 10 mm from the eyelid margin when the eye is closed. The preservation of orbital fat during a blepharoplasty is needed for the prevention of periorbital hollowing, which looks older. For satisfactory results in aging Asian upper blepharoplasty and brow lift, the harmonization of the position of the upper eyelid and eyebrow is important. Noninvasive rejuvenation such as botulinum toxin and filler are good options for facial rejuvenation.
Keywords: aging, Asian blepharoplasty, brow
Flowers1 suggested that blepharoplasties should be performed by those who fully understand the biomechanical relationship between the function of the frontal muscle and the eyebrows and its association with the upper eyelids in elderly patients. In the case of elderly Asians, it is recommended to examine the degree of eyebrow sagging to determine whether a browlift should be combined with an upper lid blepharoplasty or if it would be sufficient in and of itself before proceeding to an upper blepharoplasty. Flowers2 also suggested that after a blepharoplasty, the distance between the double eyelid line and the eyebrow should be at least 12 mm when the eyes are open. The length of the eyelid skin that goes into the double eyelid (invagination) when the eyes are open should be 10 mm.
The coronal incisions should be made to perform a forehead lift. However, now via endoscopic surgery, coronal incisions are not made and only several small incision lines are made to dissect below the frontal periosteum or above it to lift the forehead region and the eyebrows; thus good results can be obtained. Dingman3 advised that when forehead lifts are performed, an upper blepharoplasty can be performed without removing the orbital fat or extraorbital tissue. McCord et al4 advised that when blepharoplasties are performed, the upper lid skin and orbicularis oculi muscle can be dissected up to the eyebrow region to remove the brow fat pad below the eyebrow and lift the eyebrow to the desired position to internally fix it; hence eyebrow sagging could be prevented and good results obtained. In 1996, Yun et al5 suggested that among patients who visited their hospital with aging of the upper eyelid as their main complaint, they performed sub-brow skin excisions and upper lid blepharoplasties simultaneously on patients with eyebrow tattoos. Brow lifts are sometimes performed simultaneously with face lifts with good effects obtained in many cases.
Anatomy of the Upper Lid and Brow
Fig. 1 shows the anatomical differences between young and old people. A cross-sectional view of the periorbital structure is shown in Fig. 2. The periorbital structure changes in time; the most significant changes are laxity and sagging. To safely and effectively perform the operation, an understanding of the anatomy and changes in periorbital structure is essential. Asians lack the thin fibers that go from the levator palpebrae muscle to the skin, and thus do not have double folds in many cases. However, given that there are people who do not have double folds when they are born, but come to have double folds when they become old and those who do not have double folds in the morning but have double folds in the afternoon, the explanation that the upper levator palpebrae muscle fibers congenitally go to the dermis to form double folds is not sufficient. Therefore, double folds are determined by the thicknesses and amounts of various anatomical parts of the eyelids, and in particular, orbital fat, central connective tissue, subcutaneous fat, and pretarsal fat are all related with double folds.
Fig. 1.
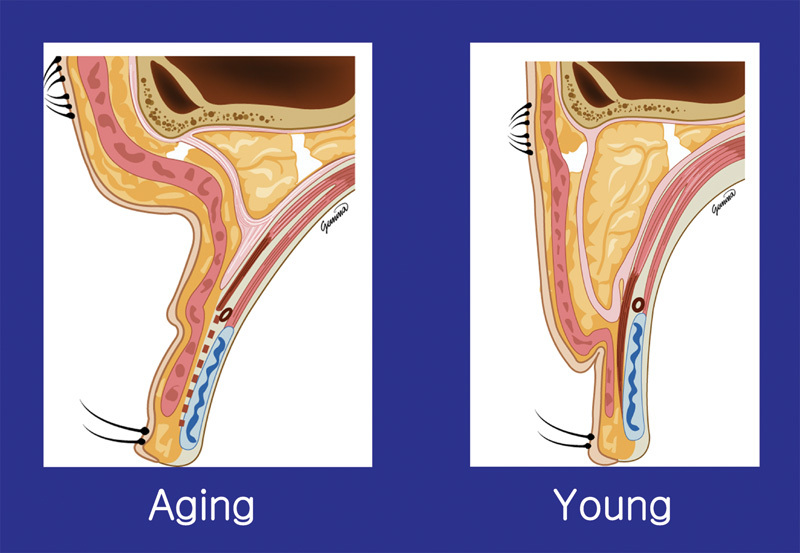
Difference of between the aging and young Asian upper lid.
Fig. 2.
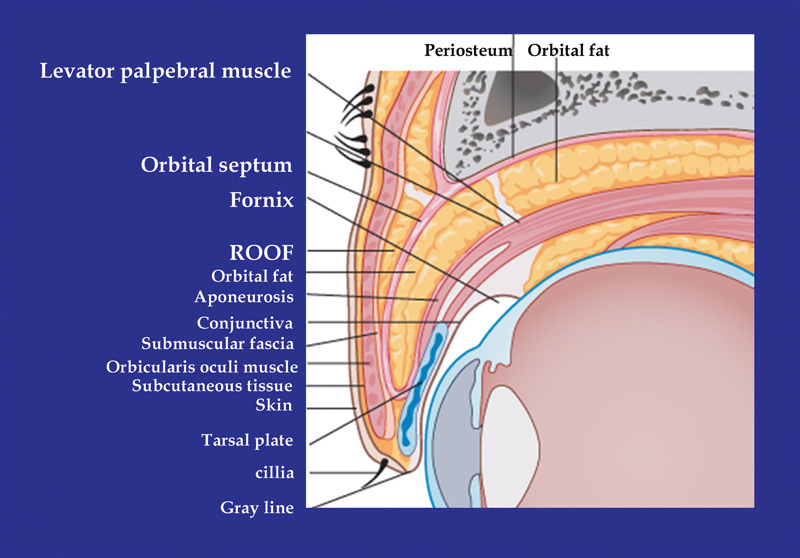
Cross-sectional view of Asian upper lid. ROOF, retro-orbicularis oculi fat.
Throughout the rejuvenation operation, patients can also have functionally good effects by not only providing cosmetic correction, but also removing obstacles to the visual field resulting from sagging eyelids. Senile upper eyelid changes are closely related with the drop of upper structures rather than the problem of upper eyelids only; thus, satisfactory outcomes cannot be obtained with just upper eyelid formation in many cases. That is, the natural shapes of the eyes and eyebrows can be expected only when sagging structures have been lifted to a level close to their original positions.
There is only one brow elevator—the frontalis muscle—whereas many muscles act as brow depressors, and those at the medial side of eyebrows are corrugator supercilii, depressor supercilii (DSM), procerus, and orbicularis oculi. However, the lateral one-third of the eyebrows mainly sag because the brow elevator—frontalis—is not attached to this area. The most lateral layer (orbital portion) of orbicularis oculi is known to pull down the eyebrows the most powerfully.6
The most important point of a forehead lift is to enhance the laterally sagging folds on the glabella to provide a gentle appearance while weakening brow depressors to raise the eyebrows as a result. If the endoscopic forehead lift is a physiologic elevation, then the open forehead lift can be said to be a mechanical lift.
In the frontal area, the supraorbital nerve (SON) and the supratrochlear nerve (STN) are important. Many branches of the STN pass through the corrugator supercilii at the origin area of corrugator supercilii; thus care should be used not to damage the STN while dissecting the corrugator supercilii. Supraorbital nerve branches can be lateral or deep branches, as well as medial or superficial branches and because the lateral branches run deep, they may be damaged.
In the temporal area, the frontal or temporal branches of the facial nerve are the most important followed by the sentinel vein (medial zygomatic temporal vein) that informs the risk of the facial nerve.
The classification of eyelid deformities resulting from aging was established by Castanares7 and Castanares8 and divided eyelid deformities into six types: blepharochalasis, dermachalasis, hypertrophy of the orbicular muscle of the eye, herniated orbital fat, and ptosis of the eyebrow and senile lid.
Preoperative Assessment and Selection of the Procedure
Preoperative Assessment
There are many things that should be noted and considered before surgery by those who wish to undergo blepharoplasty. The plastic surgeon should determine whether the patient should undergo the surgery, and select appropriate surgical methods. Through these processes, postoperative complications or unexpected unhappy events can be avoided or minimized.
Prior to surgery it is important to know which part of the patient's outward appearance is disliked by the patient and what the patient expects from the surgery. The patient should be given a mirror and point out the part which the patient dislikes. Sometimes, the patient overemphasizes his or her extremely minor shortcoming, while overlooking rather large shortcomings; this should be pointed out by the surgeon.
Medical and medication histories including and allergies and swelling should be taken; the determination of any thyroid disease, heart disease, bleeding tendency, and abnormal swelling is very important. For instance, patients with thyroid disease may look like they require an operation; however, what they need is medical treatment of their thyroid condition.
The patients should be asked if they are using anti-inflammatory agents such as aspirin or ibuprofen, vitamin E, and anticoagulants; any of these medications should be stopped before the week of surgery. This way, hemorrhagic complications that may occur before or after the surgery can be prevented. In addition, it should be known why the patient wants the surgery now, whether it is realistic, and whether the patient's expectation from the surgery is reasonable. The evaluation of balance between the entire face and the eyes should be also conducted and the doctor should focus not only the eyelids, but also the entire face of the patient.
The forehead and the eyebrows should also be reviewed to see if the eyebrow sagging is asymmetric and if it partially exists at the side of the nose or at the side of the temporal region.
Appropriate examination of the eyes, eyeballs, and auxiliary organs and eyesight tests is also necessary to prevent complications that may occur after blepharoplasty. If there is oculomotor paralysis, the eyes should be carefully examined. If Bell's phenomenon does not appear, damage to the cornea and ulcers may be induced after surgery; thus the eyes should be carefully observed.
The relationship between dry eye syndrome and blepharoplasty was intensively studied by Rees (1975)9 and Jelks and McCord (1981)10 they identified factors contributing to the insufficient production of tears, including smoking, menopause, abnormality in the thyroid, aging, and drugs.
Rees and LaTrenta (1988)11 reported that abnormalities in the orbit and surrounding structures could become factors that would induce dry eye syndrome (proptosis, loose lower eyelids, hypoplastic upper jaw, etc.). In severe eyebrow sagging, a simple blepharoplasty is not effective. To obtain good results, forehead lifts are necessary in these patients.
The eyebrow may be directly lifted or the forehead skin immediately above the eyebrow line may be partially incised in an oval shape; this method can be considered in elderly patients with severe forehead skin folds or in male pattern alopecia where coronal incisions are not adequate. Recently, eyebrow sagging is frequently corrected using endoscopes in cases where skin folds are not very severe.
Selection of the Procedure
As the name brow lift suggests, indications can be found by considering the effects that can be obtained by lifting the eyebrows. If the forehead and the eyebrow sag downward, this will affect the eyes too and the eyelids appear to be sagging. In this case, if a brow lift is performed disregarding the cause, the eyes will look heavier, double eyelid lines will become deeper to make a tougher appearance, and wrinkles around the eyes and the nasal root will be connected with double eyelid lines to become clearer than before the surgery. When there is asymmetry between eyebrows because of facial nerve paralysis or differences in power or habits between muscles around the eyebrows, the eyebrows may become symmetrical to some extent by making the degrees of dissection of the two sides different. A brow lift will make the forehead wider in persons with the narrow forehead because of the effect to expand the forehead and if the forehead is flat, making it convex using an implant or fat will enhance the effect. The skin will be straightened to become more elastic and since muscles will have a smaller contractile force as they are cut; wrinkles on the forehead, glabella, nasal root, and eye rims will be relieved. Although eyebrow sagging mainly occurs due to aging, it may also be developed congenitally. In this case, it is difficult to obtain satisfactory outcomes even in young women and thus a forehead lift should be considered.
In old facial palsy patients, sometimes brow lifts are necessary to excise appropriate amounts of the skin above the eyebrow to lift the eyebrow. Although cases of single palsy of the temporal branch of the facial nerve are the best indication, this suprabrow excision can also be performed in other cases such as partial paralysis or total paralysis.
The main candidates for sub-brow excision are Asians with blepharochalasis, thick eyelids, and Asian women aged 40 years or older with eyebrow tattoos whose upper eyelids are bulging and sagging while also having inner double eyelids.
Eyelid skin sagging and crow's feet in the lateral canthal areas are unavoidable natural eyelid aging phenomena. If the orbital fat protrudes, an eyelid deformation called baggy eyelid appears (Fig. 3).
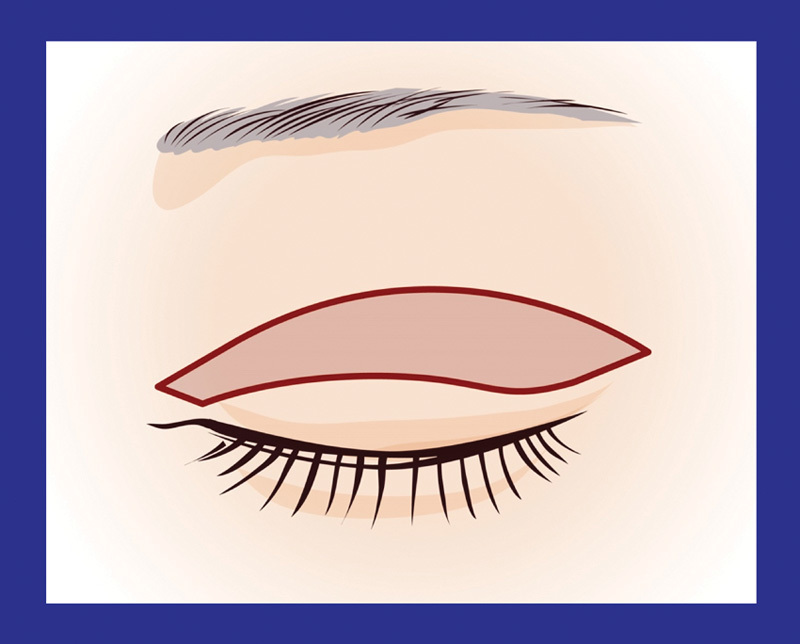
Fig 3.
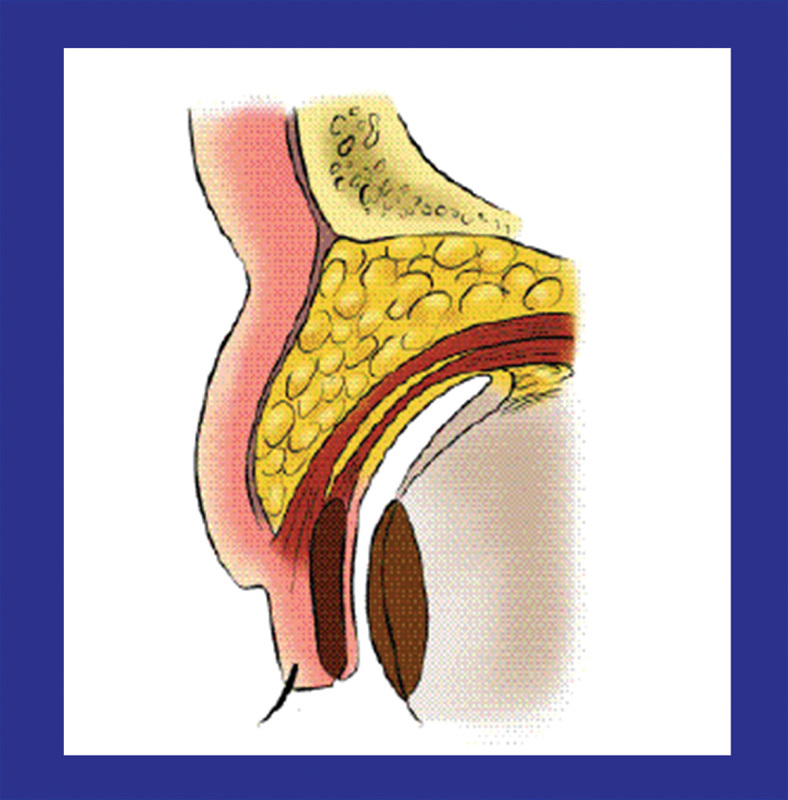
Aspect of the baggy eyelid. The orbital fat protrudes and skin loosens causing the eyelid line to be covered.
Operations that correct these changes completely or partially to make patients younger looking are collectively called blepharoplasties. These operations can produce functionally good effects by not only providing cosmetic correction but also by improving the visual field hampered by sagging eyelids.
Operative Techniques
Aging Asian Upper Blepharoplasty
The most important factors that must be considered in an aging Asian upper blepharoplasty include the degree of forehead sagging, the amount and degree of excessive skin folds on the upper eyelid and the lower eyelid, the amounts and locations of orbital fat protruding from the eyelids on both sides, the medial fat of the upper eyelid and the lateral fat of the lower eyelid in particular, the amounts and shapes of the orbicularis oculi muscles in the upper eyelid and the lower eyelid, pigmentation and senile and degenerative changes in the eyelid skin, the shape of the orbital bone, and the degree of sagging of the lacrimal glands. Analyzing these factors and appropriately adapting them during operations are important.
When performing a blepharoplasty, the upper eyelid skin should be excised sufficiently while excising lower eyelid skin conservatively. Surplus skin should be mainly excised from the lateral upper side of the lower eyelid and the skin should be sutured to the periosteum. In cases where the excision of the orbital fat is not necessary, just excising and suturing the skin can yield good results. In 1987, Oh et al12 advised that in blepharoplasties of Koreans, the amount of excised skin should be less than that of Westerners. Fat removal should be conducted several times, removing a small amount each time rather than removing a large amount. Safety and care should be taken to make lateral incision lines that do not extend outward too much, so that the approximations at both sides can match exactly during skin suturing.
Anesthesia in a blepharoplasty is performed diversely depending on the operator's personal preference. Although blepharoplasties can be performed under general or local anesthesia, local anesthesia is to be performed in principle. One percent Xylocaine (containing 100,000-fold diluted epinephrine, 1% lidocaine) is used or may be diluted two- to fourfold with saline. In cases where a blepharoplasty is performed in combination with another operation such as a forehead lift, using a diluted solution will reduce the absolute amount used and make using it in elderly persons safe.
Because removing a large amount of fat from the lower eyelid imposes considerable tension on deep structures and thus induces pain that cannot be relieved by local anesthesia only, it is important to perform local infiltration anesthesia on the side of the orbital fat.
Determination of Skin Excision Width
The skin excision is designed using Gentian violet or a water-based marking pen in a sitting position. The excision width is determined by having the patient open and close his or her eyes while holding the eyelid skin in the width to be removed with a pair of forceps (Fig. 4). Use the double eyelid line originally existing on the eye as the lower planned line, and determine and mark an excision width. In the case of a patient who does not have any clear double eyelid line, determine a double eyelid line at an appropriate height from the eyelash, considering the shape of the face and the wish of the patient when the extended skin has been slightly lifted upward; then determine an excision width (Fig. 5). In general, because the heights of Asians' double eyelids are in a range of 6 to 8 mm (although there are differences among individuals), the excision width should not exceed 10 mm. Although S-shaped suture lines with slow slopes going upward toward the lateral side are desirable to Westerners, in the case of Asians, designing suture lines along eyelid margins and suppressing the ascending slope toward the lateral side may be a better choice. Because scars can easily contract at the side of the medial canthus, it is important to design suture lines not to go out further than the medial canthus, and not to go out further than 1 cm outside the lateral margin of the orbit at the side of the lateral canthus. Although care should be used so that the final skin suture lines on the lateral ends of the upper and lower eyelids are not too close to each other, it should be ensured that the skin on the lateral side is removed more than the skin on the medial side (Fig. 5). Excise the skin after injecting the anesthetic, that is when the eyelid has swelled. When excising the skin, first incise the entire planned excision line only down to the subcutaneous tissue, making small incisions at the lateral ends of the lower and upper planned incision lines by thrusting the points with the blade of a no.15 knife and then thrusting the tip of one blade of pointed scissors to excise excessive skin by moving the scissors toward the medial side. Next, cover the skin excision site with a piece of saline gauze and proceed to excise the skin on the other side.
Fig. 4.
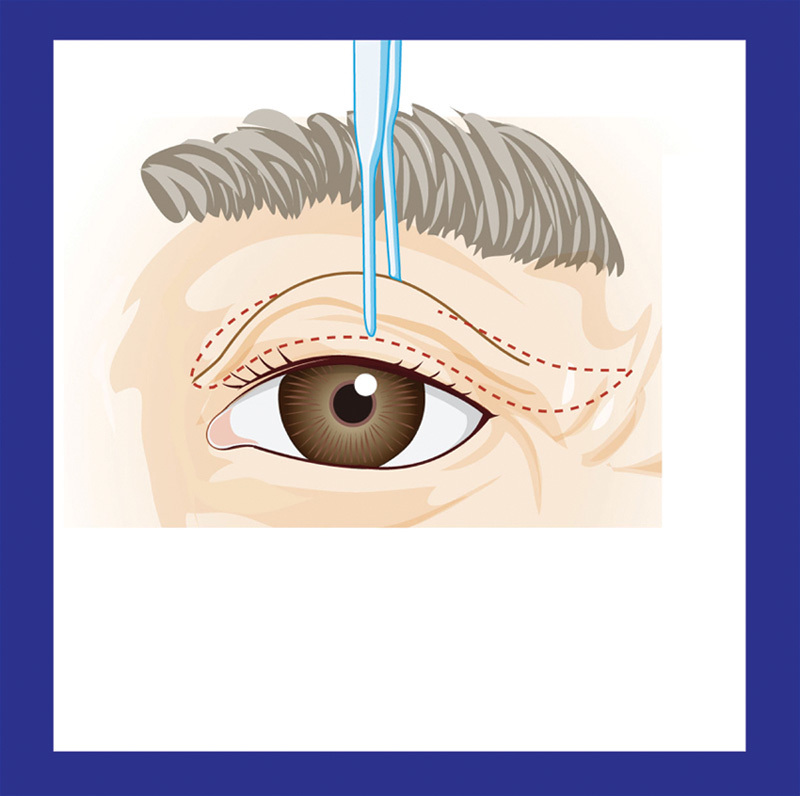
Measuring the extent of skin removal in aging Asian upper blepharoplasty is easily done with green forceps.
Fig. 5.
Design of an upper blepharoplasty.
Handling of the Orbicularis Oculi Muscle
The orbicularis oculi muscle is excised in a width slightly smaller than the skin incision width. By excising the orbicularis oculi muscle this way, the adhesion between the levator palpebrae muscle and the skin can be facilitated after the surgery so that double eyelids can be easily formed; the removal of the orbicularis oculi muscle facilitates the handling of the orbital fat or the levator palpebrae muscle. In this case, be careful not to cause damage to the connective tissue under the orbicularis oculi muscle or the superior levator palpebrae muscle. Then, the tarsal membrane is opened when the orbital fat is seen. When the patient has closed his or her eyes, if the eyeball is gently pressed, the orbital fat will be automatically exposed. However, good results can be also obtained by just removing the skin and suturing without removing the orbicularis oculi muscle, or the tarsal membrane may be opened without excising the orbicularis oculi muscle.
Handling of the Orbital Fat
Although it is not necessary to remove the orbital fat in many cases, sometimes it is necessary to identify two orbital fat sections that are considered to have excessive fat while gently pressing the eyeballs. A small incision is made on the tarsal membrane using pointed scissors, which causes orbital fat to protrude so it may be removed, or the tarsal membrane may be opened completely from the lateral side to the medial side to remove a large amount of orbital fat. However, the fat is generally excised by horizontally pinching an appropriate amount with mosquito forceps. To completely stop the bleeding from the end of the excised fat pinched by the forceps, use electrical coagulation or ligation with 6–0 Dexon. Gently place the forceps on the site to identify hemostasis. Sometimes, the lateral side of the upper eyelid may appear to protrude severely due to lacrimal gland sagging or fat deposition under the orbicularis oculi muscle. In this case, lift the lacrimal glands to the medial side of the superior margin of the orbit and fix there, or remove some of the lacrimal glands. May et al13 advised that if the fat (retro-orbicularis oculi fat [ROOF]) below the orbicularis oculi muscle, except for the lacrimal glands, were removed, cosmetically good results are obtained. After fat removal, cover the wound surface with a piece of saline gauze, then excise the fat on the other side in the same manner.
Wound Suture
In Asians, cases where patients originally had double eyelids and cases where they did not have double eyelids should be considered separately. In cases where patients originally had double eyelids, because it is not necessary to make new double eyelid folds, fixing sutures of the dermis with the levator palpebrae muscle or the tarsal plate are not necessary. However, fixing sutures are conducted in some cases to make clearer and symmetrical double eyelids. Wash the wound surface with saline solution or saline gauze and recheck hemostasis. Do not suture the tarsal membrane and the orbicularis oculi muscle. Using 6–0 or 7–0 nylon sutures, conduct continuous sutures or single sutures one by one beginning from the side of the medial canthus. In this case, use care not to leave dog ears at any of the two ends.
In cases where patients did not have double eyelids originally, surgical methods vary with patients' requirements or cases. In case the patient has a benign lesion on an upper eyelid like xanthelasma, not only surgical removal of xanthelasma but cosmetic upper blepharoplasty should to be considered (Fig. 6). If the patient does not want double eyelids or the patient is a male or an elderly patient, if an incision is made directly above the eyebrow, after the skin and subcutaneous tissue are removed and the wound is sutured, double eyelids at a very low level will exist but disappear soon; thus, the eyes will become natural and not much trace of the surgery will remain (Fig. 7).
Fig. 6.

Upper blepharoplasty with xanthelasma excision.
Fig. 7.
Blepharoplasty without forming a double eyelid. (A) Preoperative view. The patient had discomfort with visual disturbance caused by an upper eyelid crease, but he did not want a double eyelid line. (B) Postoperative view. Combined with a suprabrow lift.
If a patient who has no double eyelid wants double eyelids to be made during a blepharoplasty, three to five sites between the dermis and the levator palpebrae muscle or the tarsal plate should be sutured for fixation as with the double eyelid formation described above.14 In this case, to make the thick upper eyelid tissue thinner, the tissue located in front of the levator palpebrae muscle, the orbital fat, the central connective tissue, the tarsal membrane, the orbicularis oculi muscle, the subcutaneous fat, and the skin should be excised at different degrees depending on the degree of thickness of the upper eyelid. It has been found that if the different parts are three-dimensionally excised in different shapes such as triangles, squares, and diamond shapes, good effects can be obtained.15 When performing an upper lid blepharoplasty, a double eyelid formation, baggy eyelid correction, partial removal of lacrimal glands, eyebrow lift, or forehead lift should be performed together in many cases, depending on eyelid conditions. If aging eyelid sagging is also present, remove the orbicularis oculi muscle, completely open the tarsal membrane from the lateral to the medial side, remove both the medial and lateral orbital fat, then expose the levator palpebrae muscle aponeurosis. Suture the superior margin of the tarsal plate and the levator palpebrae muscle aponeurosis at around 7 to 8 mm above the superior margin of the tarsal plate with 6–0 nylon sutures, shorten the levator palpebrae muscle aponeurosis with plication, and then form double eyelids with buried sutures at three points between the dermis and the superior margin of the tarsal plate. This will considerably heal the lid ptosis and improve the visual field.
Cases
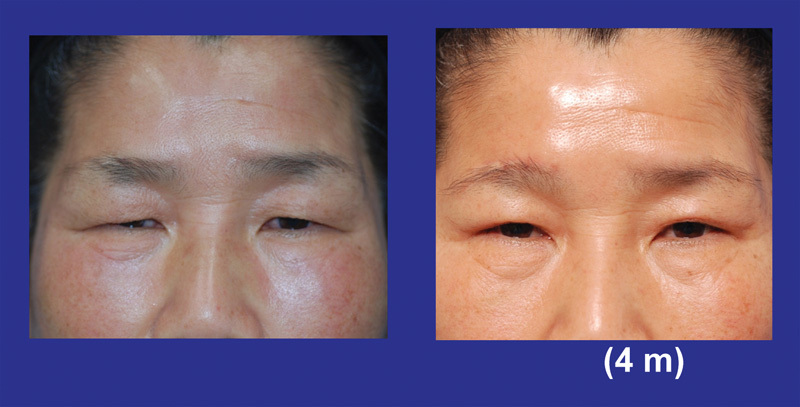
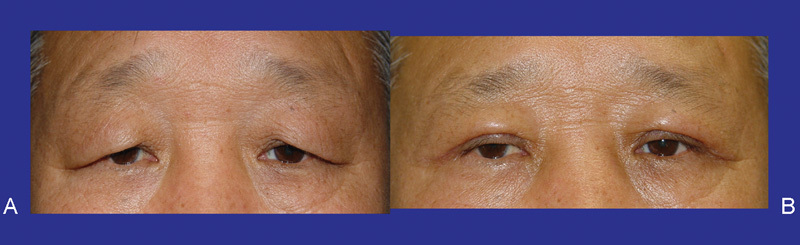
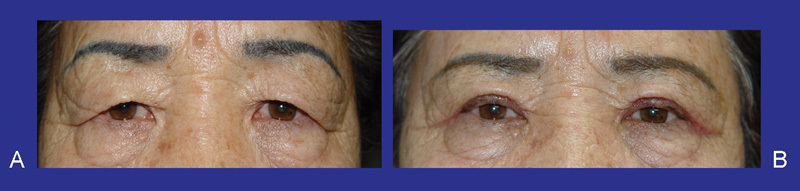
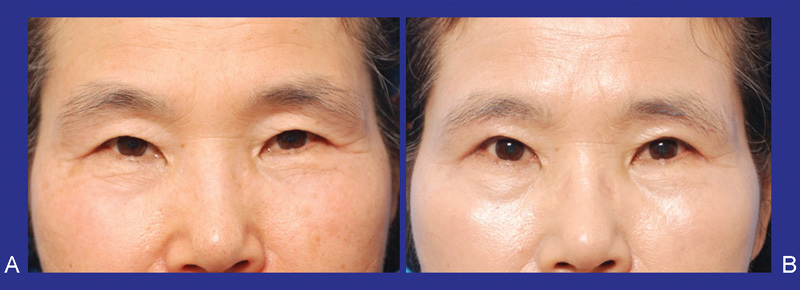
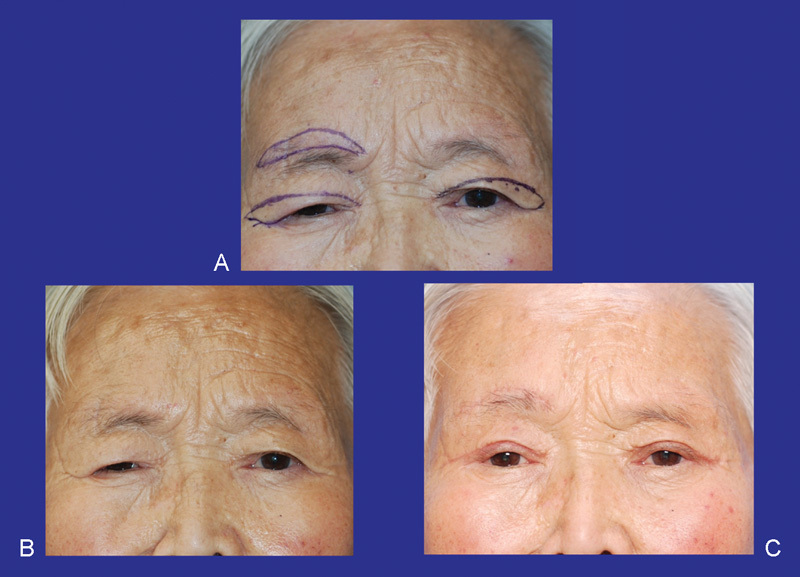
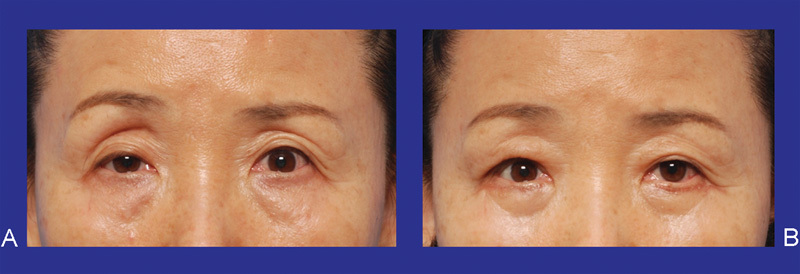
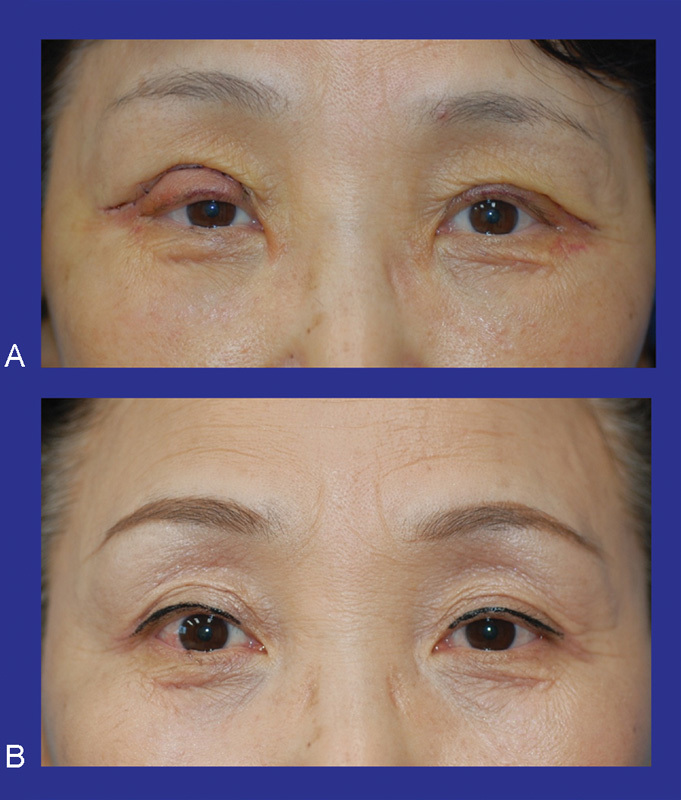
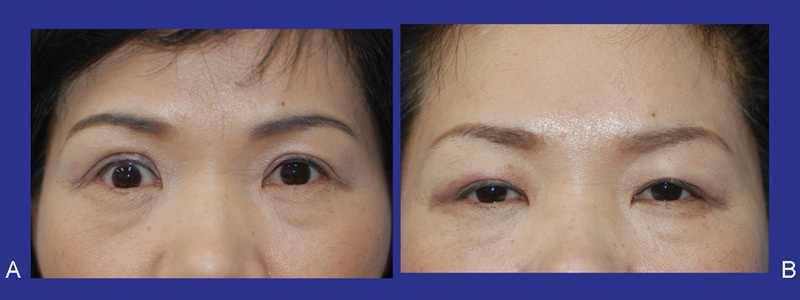
Fig. 8 illustrates a case where only the skin is excised: This technique is used when the patient has clear double eyelids, but the skin is sagging. Fig. 9 depicts a case where the skin is excised and then double eyelids are made by suturing the skin in order of skin–tarsal plate–skin. Fig. 10 shows a case where double eyelids are made by skin excision and buried tarsal sutures. Figs. 11 and 12 depict cases where there is acquired lid ptosis and an upper lid blepharoplasty is performed, accompanied by ptosis correction.
Fig. 8.
Upper blepharoplasty; skin excision only. (A) Preoperative. (B) Postoperative.
Fig. 9.
Upper blepharoplasty with a double fold formation by nonburied skin–tarsus–skin suture with a skin excision. (A) Preoperative. (B) Postoperative.
Fig. 10.
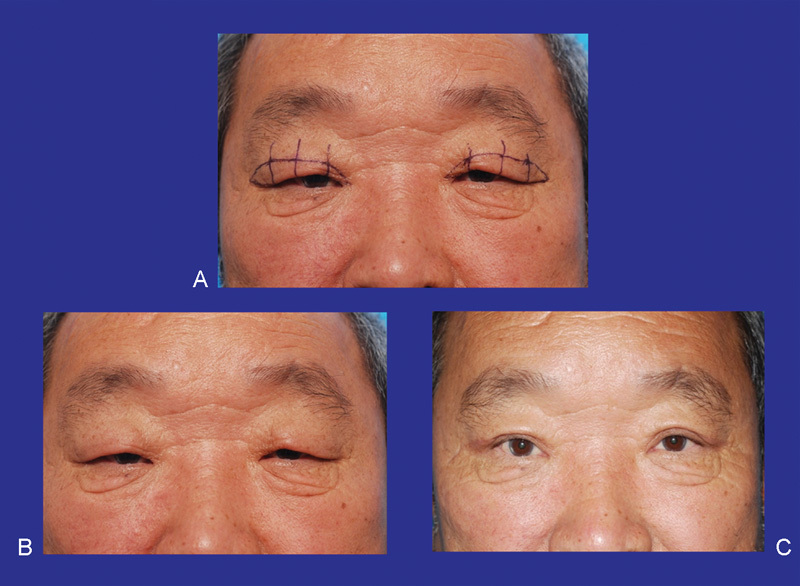
Blepharoplasty with double fold formation by buried suture on tarsal plate. (A) Design. (B) Preoperative. (C) 5 months postoperative.
Fig. 11.
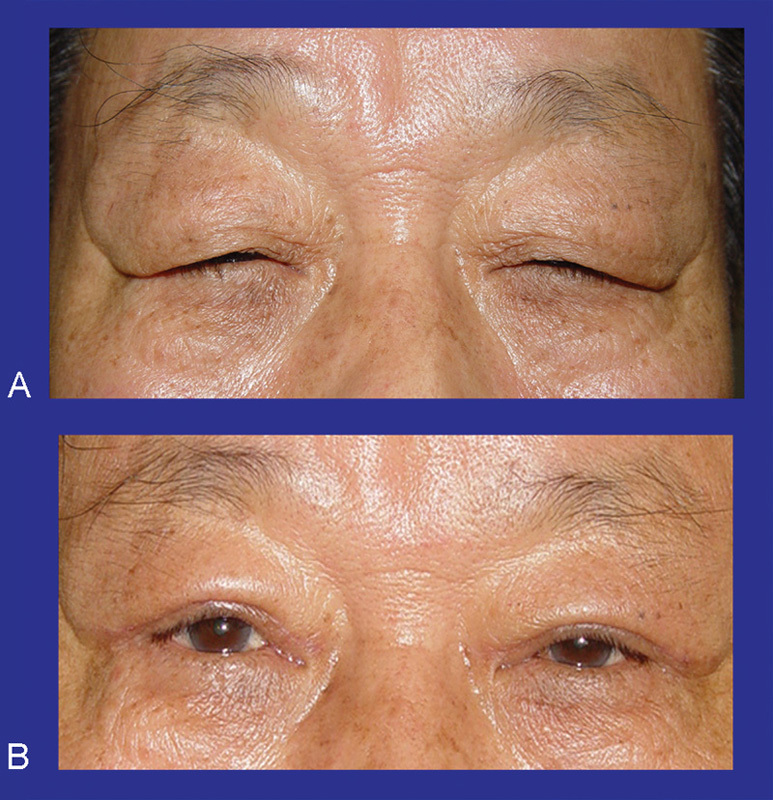
Upper blepharoplasty with levator aponeurosis plication. (A) Preoperative. (B) Postoperative.
Fig. 12.
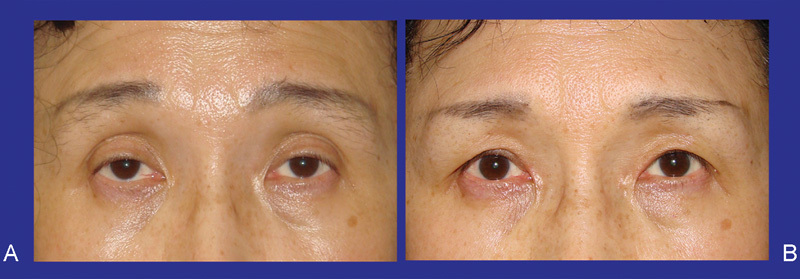
Upper blepharoplasty with ptosis correction. (A) Preoperative. (B) Postoperative.
Sub-Brow Excision
Sub-brow excision is a sort of rejuvenation surgery that excises the skin immediately below the eyebrows to lift sagging upper eyelids. Sub-brow excision is frequently performed because if just a double eyelid formation is performed, an impression of a “tough person” results. It is not easy obtaining a natural outcome. A forehead lift using an endoscope is an involved surgery, has a high probability for complications to develop, and is expensive. The main indications for a sub-brow excision are blepharochalasis and thick eyelids and women aged 40 years or older with eyebrow tattoos.
Design for Operation
As for preoperative design, first, draw a line in the center of the glabella, then mark the location of the supraorbital nerve 2.5 cm laterally to the center and mark the location of the supratrochlea nerve 1 cm medial to the mark (Fig. 13). In compliance with the way women trim their eyebrows, leave around one-fourth of the eyebrow at the medial side and design only three-quarters at the lateral side. Begin the medial side of the incision from the same location as the origin of the supratrochlea nerve and finish the lateral side of the incision at the point where the eyebrow or tattoo ends making around 4.5 to 5.2 cm long straight line.
Fig. 13.
Design of sub-brow excision.
Technique
The amount of skin to be excised may be determined to the same amount as the amount of skin to be excised when only the skin is excised in a blepharoplasty. The overall area of excision should be fusiform, making the length of the widest point to be around 8 to 12 mm. If a region above the fusiform excision line is incised, incising the region obliquely to be parallel to the direction of hair follicles thereby avoiding damage to the hair follicles will make the eyebrow cover the scar later so that the scar would not be easily visible.
If a region below the fusiform excision line is incised, incise vertically to make a straight line that passes the orbicularis oculi muscle and the posterior fascia of orbicularis oculi muscle. From the lateral side of the fusiform excision line, incise the skin and the orbicularis oculi muscle and the posterior fascia of orbicularis oculi muscle en bloc, and incise only the skin from the point of origin of the supraorbital nerve so that the supraorbital nerve and the supratrochlea nerve would not be damaged. In a region above the fusiform excision, dissect between the orbicularis oculi muscle plus posterior fascia of orbicularis oculi muscle and submuscular fat. Make an approximate 5-mm wide subcutaneous tunnel between the supraorbital nerve and the origin of the supratrochlea nerve. This is to pull the medial lower flap and suture for fixation later. Pull the posterior fascia of orbicularis oculi muscle on the lower flap upward and fix it to a periosteum and sub-brow fat at an appropriate position. The appropriate position should be a position that would not make too much tension when the posterior fascia of orbicularis oculi muscle is pulled, and this position is generally the same as the position of the margin of the upper flap. Use 5–0 PDS suture for the fixation and make three horizontal sutures on a region lateral to the supraorbital nerve and one vertical suture between the supraorbital nerve and the supratrochlea nerve to avoid damage to the nerves. In the case of subcutaneous sutures, seize part of the upper flap as it is thick and the entire layer of the lower flap as it is thin. Fig. 14 is a case of the sub-brow excision.
Fig. 14.
Upper blepharoplasty by sub-brow excision. (A) Preoperative view. The patient had discomfort caused by dermatochalasis of the upper eyelid. (B) Postoperative view. Excessive skin excision was done on both sub-brow areas.
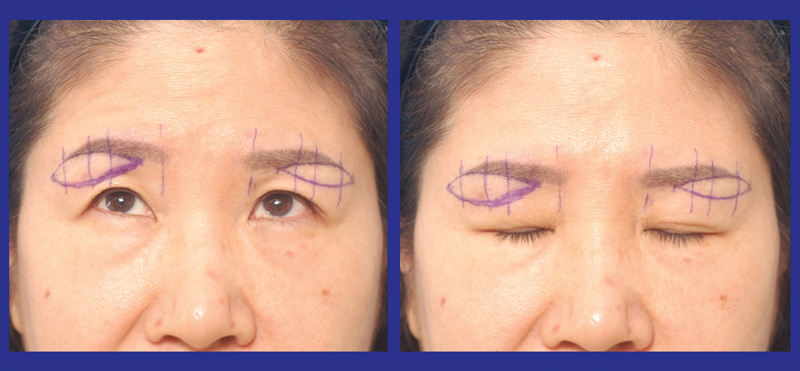
Suprabrow Excision
It is important to excise the region immediately above the eyebrow to the position a little higher than the top or to the top when the eyes are seen upward. With regard to upper eyelid skin excision, simple excision of the sagging skins on both sides is sufficient in many cases. In facial palsy patients, sometimes brow lifts are necessary that excise appropriate amounts of the skin above the eyebrow to lift the eyebrow. This suprabrow excision can also be performed in other cases such as partial paralysis or total paralysis. Fig. 15 is the design and a case of the suprabrow excision.
Fig. 15.
Upper blepharoplasty combined with supra-eyebrow excision. (A) Design. (B) Preoperative. (C) 1 month postoperative.
Forehead–Brow Lift
Although coronal incisions are mainly used in an open brow lift, mainly five regions (median line, regions around 4 to 5 cm away laterally from the median line and temporal region) are incised around 1.5 cm long in endoscopic surgery. In the frontal area, deep incisions are conducted to the subperiosteal plane and in the temporal area, the region between the temporo-parietalis and the deep temporal fascia becomes the incision surface. Devices for endoscopic surgery can be divided into an endoscope, a camera, a light source and dissecting devices. The endoscope to be used should have an angle cut to below 30 degrees and a diameter of 4 mm or 5 mm. The devices are divided into periosteum elevators, soft tissue dissectors, muscle graspers. In addition, monitors, storage devices and a stand on which all the above mentioned things can be laid are necessary.
When the processes to separate nerves from surrounding tissues have been completed, cut the corrugator supercilii. Fixation is necessary to lift dissected tissues to desired positions and maintain them. Because Asian skin is typically thick, if the dissected frontal skin flap and temporal skin flap are not fixed, the skin flaps will come down to their original positions to reduce the effect.
In an endoscopic brow lift, fixation in the frontal area fixes the frontal skin flap to the frontal bone by making a cortical tunnel on the skin layer of the frontal bone and fixing the frontal area skin flap to the tunnel with no. 2 PDS sutures. Although Endotine has been developed recently and can be used, it is expensive and its results are not better than other methods.
Free Fat Grafting and Fat Reposition
Recently, a free fat graft in tiny parcels and threads has been widely used after the probability of its success was enhanced by Coleman through careful surgeries. Fat is centrifuged for 3 minutes at 3,000 rpm in the tumescent method before being used. Free fat grafts are widely used; free fat has less risk of allergy or rejection reactions compared with artificial graft materials and recovery is fast and outcomes are good when this method is used. There are two methods according to the injection site: (1) injection on the septum of eyelid, and (2) injection on subcutaneous tissue. Fig. 16 shows a case of an upper blepharoplasty and fat graft on the upper lid to correct a sunken eyelid.
Fig. 16.
Fat graft combined with aponeurosis plication. (A) Preoperative view. She had discomfort with visual disturbance caused by left upper eyelid retraction and sunken eyelid on the right side. (B) 1 month postoperative. Combined with aponeurosis plication and fat graft.
Good results can be obtained by repositioning orbital fat upward to the orbital margin as if grafting it instead of removing the upper eyelid fat during the upper blepharoplasty. The tissue repositioning method corrects sunken eyelids by detaching the tissue adhering to the sunken region and repositioning other tissues such as orbital fat, or conducting double fold operation or ptosis correction. Fig. 17 is a diagram of orbital fat transposition and Fig. 18 shows an intraoperative view of orbital fat transposition. Fig. 19 depicts a case of orbital fat transposition combined with aponeurosis advancement.
Fig. 17.
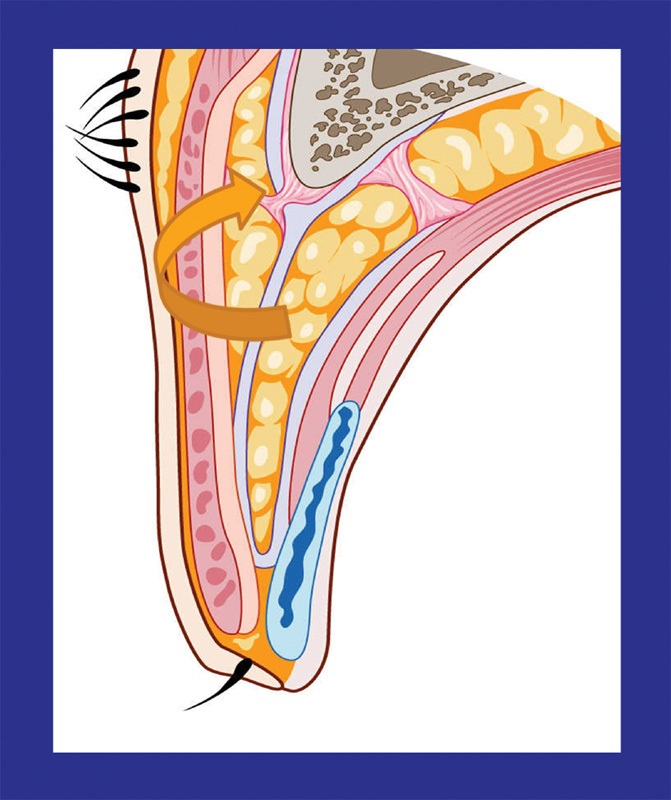
Diagram of orbital fat transposition.
Fig. 18.
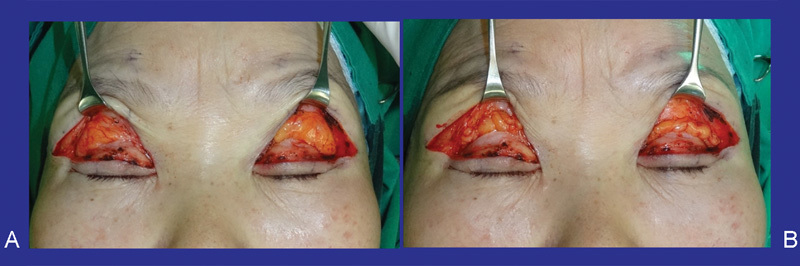
Intraoperative view of orbital fat transposition. (A) Orbital fat. (B) After fixation of orbital fat to the upper orbital margin.
Fig. 19.

Orbital fat transposition combined with aponeurosis advancement. (A) Preoperative. (B) Postoperative.
Complication and Its Management
Complications of Asian upper blepharoplasties can be divided into temporary complications and persisting complications. Temporary complications are developed just after surgery and are healed without particular problems in most cases, but hematoma is problematic in particular; thus, it is important to stop the bleeding. Persisting complications include asymmetry, ptosis, lagophthalmos, and scars—some of them require secondary eyelid formation.
Corneal Exposure or Dryness
Damage to the cornea or the conjunctiva can happen in surgery; if the cornea or the conjunctiva becomes dry during surgery, it will be damaged too. The damage may be also caused if a bandage is left on too long after surgery or if a bandage is placed with the eyes wide open.
Chemosis
Chemosis develops immediately after surgery or when some time has passed. This is attributable to (1) corneal drying, (2) incomplete eyelid closing, (3) allergic reactions to drugs or injections, and (4) subconjunctival edema. To treat it, the cornea and the conjunctiva should be frequently cleaned with eye lotions or ointment. A steroid should be applied locally and intraocular pressure should be periodically tested. In severe cases, the condition can be improved by preventing the exposure of the tarsal membrane and the conjunctiva by temporarily suturing the upper and lower eyelids or by additional procedures.
Hemorrhage and Hematoma
Ecchymosis and anterior hematomas do not require any particular treatment if there is simple petechiae. In the case of hematomas with clear boundaries, appropriate treatment may be necessary after removing the sutures.
Retrobulbar hemorrhage is a complication that frequently develops after eyelid formation, which results in blindness in rare cases. A major cause of retrobulbar hemorrhage is damage to blood vessels. The damage is not caused when the tarsal membrane has not been opened or when only the skin has been excised; it is caused when the fat has been excised and the ends of blood vessels have bled and gone deep into the orbit.
Epiphora or Dry Eye Syndrome
Dry eyes are caused by incomplete eyelid closing, temporary eyelid lags, lagophthalmos, or evaporation phenomena. Most conditions are naturally relieved within several weeks to several months. Causes of epiphora developed immediately after surgery are mostly edema or swelling developed in surgery sites that prevents the discharge of tears; thus, it is relieved in most cases as the edema disappears. Dry eye syndrome is mild and transient in most cases; complications are rarely experienced. However, there are many cases where eyelid formation is performed in patients who originally have dry eye syndrome, which aggravates the dry eye syndrome. Therefore, the appropriate tests should be conducted before surgery.
Asymmetry: Undercorrection and Overcorrection
Although the upper and lower eyelids on the two sides are not the same even before surgery, the asymmetry is covered to some extent as the skin is appropriately sagging and orbital fat increases; therefore, asymmetry may be unnoticed.
However, because the sagging skin and increased fat are removed after eyelid formation, the asymmetry is aggravated. In addition, because it is difficult to remove the two sides identically, patients are not satisfied with their results in many cases. On the other hand, if the orbital fat or central connective tissues contained in the upper and lower eyelids have not been appropriately removed, if the surplus skin has not been sufficiently removed, or if too much fat has been removed while removing too small amounts of skin thereby increasing wrinkles, the results may look like undercorrection.
Blepharoptosis
Although mild to moderate ptosis may appear in most patients after eyelid formation due to edema, if the ptosis is serious when observed for several days after surgery, the levator palpebrae muscle may have been damaged or the levator aponeurosis may have been cut during the surgery. Also, because many patients have ptosis before surgery, ptosis should be established before surgery. Fig. 20 shows a case of undercorrection and fold height asymmetry after an upper blepharoplasty with ptosis correction and its treatment. Fig. 21 illustrates an overcorrected case and its treatment.
Fig. 20.
Undercorrection: Right upper eyelid and asymmetry of double fold height. (A) Preoperative. (B) 5 months postoperative.
Fig. 21.
Overcorrection: Right upper eyelid. (A) Preoperative. (B) I year 4 months postoperative.
Hypertrophic Scars and Infection
Because the skin of the upper eyelid or lower eyelid is generally very thin, hypertrophic scars very rarely become problems; they are naturally relieved within 6 months in most cases. Hypertrophic scars may be made in the medial canthus and incision sites near the medial canthus. If sutures can be removed early, remove them at day 3 or 4 after surgery and fix the medial canthus region with tapes. If thickening progresses, locally inject a small amount of steroid and observe the progress. Although severe hypertropic scars can also be treated by locally injecting a steroid 2 or 3 times at intervals of 10 days, there may be complications from steroids. Ophthalmologic examinations including intraocular pressure measurement may be necessary in some cases.
References
- 1.Flowers R S, Caputy G G, Flowers S S. The biomechanics of brow and frontalis function and its effect on blepharoplasty. Clin Plast Surg. 1993;20(2):255–268. [PubMed] [Google Scholar]
- 2.Flowers R S. Upper blepharoplasty by eyelid invagination. Anchor blepharoplasty. Clin Plast Surg. 1993;20(2):193–207. [PubMed] [Google Scholar]
- 3.Dingman D L Transcoronal blepharoplasty Plast Reconstr Surg 1992905815–819., discussion 820 [PubMed] [Google Scholar]
- 4.McCord C D, Doxanas M T. Browplasty and browpexy: an adjunct to blepharoplasty. Plast Reconstr Surg. 1990;86(2):248–254. doi: 10.1097/00006534-199008000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Yun E S, Yun S H, Oh J W, Kim D I. Sub eyebrow skin lifts in persons with tattoos. J Korean Society Aesthet Plast Surg. 1996;2:32. [Google Scholar]
- 6.Gonzalez-Ulloa M, Stevens E. The treatment of palpebral bags. Plast Reconstr Surg Transplant Bull. 1961;27:381–396. doi: 10.1097/00006534-196104000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Castanares S. Blepharoplasty for herniated intraorbital fat; anatomical basis for a new approach. Plast Reconstr Surg (1946) 1951;8(1):46–58. [PubMed] [Google Scholar]
- 8.Castañares S. Classification of baggy eyelids deformity. Plast Reconstr Surg. 1977;59(5):629–633. [PubMed] [Google Scholar]
- 9.Rees T D. The “dry eye” complication after a blepharoplasty. Plast Reconstr Surg. 1975;56(4):375–380. doi: 10.1097/00006534-197510000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Jelks G W, McCord C D Jr. Dry eye syndrome and other tear film abnormalities. Clin Plast Surg. 1981;8(4):803–810. [PubMed] [Google Scholar]
- 11.Rees T D, LaTrenta G S. The role of the Schirmer's test and orbital morphology in predicting dry-eye syndrome after blepharoplasty. Plast Reconstr Surg. 1988;82(4):619–625. doi: 10.1097/00006534-198810000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Oh G S, Park C G, Kim J H. Clinical review of blepharoplasty. J Korean Society Plast Reconstr Surg. 1987;14:357. [Google Scholar]
- 13.May J W Jr, Fearon J, Zingarelli P. Retro-orbicularis oculus fat (ROOF) resection in aesthetic blepharoplasty: a 6-year study in 63 patients. Plast Reconstr Surg. 1990;86(4):682–689. doi: 10.1097/00006534-199010000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Sugimoto T. Blepharoplasty in Orientals for aging eyelids. Plast Reconstr Surg. 1991;1:510. [Google Scholar]
- 15.Chen W P. Concept of triangular, trapezoidal, and rectangular debulking of eyelid tissues: application in Asian blepharoplasty. Plast Reconstr Surg. 1996;97(1):212–218. doi: 10.1097/00006534-199601000-00035. [DOI] [PubMed] [Google Scholar]


