Abstract
Double eyelidplasty is the most frequent cosmetic procedure for Asians; however, the epicanthal fold has been a conundrum that has limited the cosmetic results of Asian blepharoplasty. To achieve satisfactory results in an Asian double eyelidplasty, the key is an understanding of the true nature of the epicanthus. We propose that the epicanthus developed in the eyelid's evolutionary process. Selective detachment and superomedial reposition of the preseptal portion of the upper orbicularis muscle can resolve the primary cause of epicanthal formation without functional impairment. The vertical skin shortage and resultant skin tension of the upper eyelid can be corrected by subcutaneous dissection and transverse advancement of skin flap. An epicanthoplasty is part of the core surgery for Asian double eyelidplasty, especially when forming a parallel type of double eyelid. Combined epicanthoplasty and double eyelidplasty need to be considered as one complete and inseparable procedure in surgery of the Asian eye.
Keywords: eyelid evolution, epicanthus, epicanthoplasty, double eyelid, double eyelidplasty, Asian blepharoplasty
History and Dilemma
Double eyelidplasty is the most frequent cosmetic procedure for Asians; however, the epicanthus has been a conundrum that limits the cosmetic results of a double eyelidplasty. A double eyelidplasty without epicanthoplasty tends to be unattractive or unnatural. Aesthetically, the epicanthal fold is worsened when performing double eyelidplasty without epicanthoplasty because double eyelid formation aggravates the vertical tension on epicanthal skin. It has been a longstanding dilemma for plastic surgeons as to which procedure to choose: an infold-type double eyelidplasty with a less satisfactory result or an outfold-type double eyelidplasty with concomitant epicanthoplasty with the risk of a hypertrophic scar on the Asian eyelid. When the epicanthal fold is severe, the surgical incision for a skin flap also becomes longer; a scar can be easily visible in the conventional method, which is based on the concept of a local skin flap and lacks a consideration of the upper orbicularis muscle and vertical epicanthal tension. Although it has been reasoned that combined epicanthoplasty is helpful in Asian double eyelidplasty, there has not been a clear understanding of the epicanthal fold, promoting treatment controversy. Early on, many epicanthoplasty methods were developed, mostly based on the skin flap concept. Current methods include combined techniques such as skin excision, Z-plasty, myotomy or myectomy of preseptal orbicularis muscle, skin redraping, plication of medial canthal ligament, and so on.1 2 3 4 5 However, the development of incomplete methods has been unavoidable due to a lack of understanding of the true nature of the epicanthus. As the clinical significance of the epicanthus is mainly related to an Asian double eyelidplasty, an essential epicanthoplasty should be undertaken for all types of double eyelid surgery including the high outfold type (parallel type). But there has not yet been an effective epicanthoplasty method that provides a universal solution for an Asian double eyelidplasty. Our approach addresses the formative causes of epicanthal deformity and their relationship with the double eyelid.
Actual Shape of the Medial Canthus and Differences in the Asian Eyelid
The eyelashes are the true boundaries of the palpebral fissure. The eyelash of a Caucasian is exposed completely and the eyes look clear. Also, the eye looks bigger with the parallel supratarsal crease of eyelid. In contrast, the Asian eye without a supratarsal crease is veiled by various amounts of skin drooping and the eyeline where the lashes grow is hidden beneath the soft tissues called epiblepharon. The more the eyelid tissues droops down, the smaller and the puffier the eyes look. The canthus of a Caucasian eye is exposed completely, whereas the inner part of the medial canthus of the Asian eye is veiled by the epicanthus. The shapes of the canthal angle are varied, but generally Asian canthal angles are rounder and shorter than those of Caucasians. There are various distortions of canthal shape in the Asian medial canthus, as a result of the evolution of the eyelid. Devolutional epicanthoplasty can restore the original shape of the medial canthus and reveal it completely. An epicanthoplasty can also restore the length of the palpebral fissure and refine the nasocanthal contour.
What Is the Epicanthus?
The epicanthus exists as a normal characteristic in Asian ethnicity; however, it is peculiar to East Asians. The true incidence of the Asian epicanthus is uncertain. But most people have epicanthi to varying degrees with either the absence or the incomplete presence of a supratarsal crease.6 We reasoned that hypertrophy of the orbicularis oculi muscle was instrumental in the evolution of the epicanthus. The affected areas of the eyelid can be divided into three parts in the evolutional process: (1) The epicanthus with vertical skin shortage and tension on upper medial eyelid, (2) the epiblepharon with loss of crease on the rest of the upper eyelid, and (3) skin fold on the lower eyelid (Fig. 1).
Fig. 1.
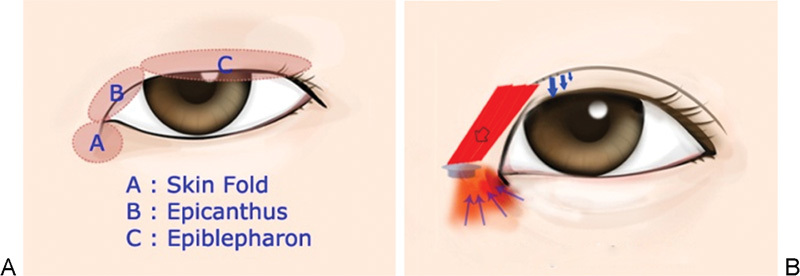
(A) Three parts of the eyelid that are affected by evolutional processes. (B) The epiblepharon is formed after epicanthus formation for additional veiling of the eye. Severe epicanthus-related skin fold on the lower eyelid develops after epicanthus formation, but before the complete loss of a supratarsal crease in the eyelid's evolution.
The main aspect of the Asian eyelid's evolution is the bulging epicanthus of the upper medial eyelid. The upper medial eyelid bulges with soft tissue directed toward the eyelash, settling inferomedial to the medial canthal ligament along the rudimentary supratarsal crease. Under the skin of the epicanthus, there are dense fibrous tissues and various amounts of orbicularis oculi muscle fibers. The next aspect is the skin fold on the lower-eyelid inferior to the medial canthal ligament. The skin fold and related wrinkles on the lower eyelid are formed by a pulling-up traction mechanism. Finally, the epiblepharon (lateral to the point S in Fig. 2) formed after the loss of the midlateral supratarsal crease and displacement of the orbicularis muscle as in the epicanthus. In short, the epicanthus is the result of atrophy and fibrous degeneration of the hypertrophied orbicularis oculi muscle, which occurred in the evolution of the Asian eyelid.
Fig. 2.

(A) A Caucasian eyelid on strong frowning who has a hypertrophied orbicularis muscle. Notice the angular point (point S) on which sheer stress is concentrated. (B) An Asian single eyelid on strong frowning. (C) Relaxed eyelid with drawing of supratarsal crease. (D) Open eyelid with crease formation by stick.
Von Ammon first used the term “epicanthus” in 1860.7 As a basis for our understanding of the evolution of the eyelid, we need to define correctly the term “epicanthus,” which can be the epicanthus itself with or without a skin fold on the lower eyelid. So far the epicanthus means “a vertical fold of skin over the angle of the inner canthus.” The use of the word “fold” is not good. And the commonly used term “epicanthal fold” is inappropriate in the case of the Asian epicanthus. It may mislead plastic surgeons to think of the epicanthus as a fold. When we describe the skin fold on the lower eyelid, “epicanthus-related skin fold of the lower eyelid” is a more appropriate term considering its location. The epicanthus-related skin fold on the lower eyelid is just a skin fold by traction force that resulted from the pulling-up of the origin point during contraction of the preseptal orbicularis muscle. Formation of the prominent fold on the lower eyelid is an ancillary manifestation that occurs with the formation of the epicanthus and the complete loss of supratarsal crease over time. The epiblepharon forms as a result of the loss of a midlateral crease and displacement of orbicularis muscle. The epiblepharon is a continuous structure with the epicanthus in the upper eyelid and is of the same composition as the epicanthus. The epicanthus and epiblepharon are purposeful structures that provide eye protection, but the skin fold on the lower eyelid is an unnecessary byproduct. If we include the epicanthus itself and skin fold on the lower eyelid into the meaning of “epicanthus,” the epiblepharon should also be included in relational to the evolutional aspect. It is appropriate that “epicanthus” means epicanthus itself excluding skin fold on lower eyelid. The main component in eyelid evolution is the upper medial portion of preseptal orbicularis oculi muscle. The epicanthal skin region was originally a crease. The epicanthus bulged from a concave crease to a convex shape with concurrent loss of medial crease consequent to the detachment of aponeurotic expansion. The shape of bulging convexity is due to the gravitational displacement of the anterior lamella including hypertrophied preseptal orbicularis muscle (Fig. 2). So it would be appropriate to call the epicanthus an “epicanthal bulging” instead of an “epicanthal fold.” Nevertheless, bulging or fold only means or indicates a part of the affected eyelid areas. We need to better define each part—“epicanthus,” “epiblepharon,” “epicanthus-related skin fold”—separately to remove any confusion.
The epicanthus presents as a remnant fibromuscular volume on the upper medial canthal region with vertical (actually diagonal, relative meaning in relation to the horizontal supratarsal crease) skin shortage and tension that causes difficulty in horizontal skin folding. It acts as a major hindrance to double eyelid formation in Asian blepharoplasty. The fibrous tissues and malpositioned orbicularis muscle prevents the even transmission of levator muscle power toward the medial skin because the aponeurotic fibers have been detached and do not extend to the epicanthal skin area any more. The pre-existing vertical skin tension acts as tensional stress on the newly formed surgical crease. The epicanthal skin tension is considered a major inhibitory factor to the sustainability of a surgical crease in an Asian double eyelidplasty. Also, the malpositioned orbicularis muscle can be reactivated as a vertically acting inhibitor that causes active tensional stress on a midlateral surgical crease, especially when an outfold-type double eyelidplasty without epicanthoplasty has been performed. The epicanthus veils various amounts of inner medial canthus, so it makes Asian eyes look stuffy aesthetically.
Evolution of the Epicanthus (Kwon's Theory): Etiology and Processes
Underdeveloped nasal bone, an excess of horizontal medial canthal skin relative to the vertical skin shortening, an excess of orbicularis muscle, and abnormal skin tension are causes of the epicanthus according to plastic surgeons. There is an anthropological hypothesis that the epicanthus is an outward phenotype that is the result of evolutionary adaptation to relevant environments. Genetically, all modern humans are included in the subspecies Homo sapiens sapiens, a subspecies of Homo sapiens. It has been posited that the racial differences in modern humans are just phenotypic variations.8 9 However, the developmental mechanism of Asian epicanthus has not been defined clearly. Our consideration of the epicanthus did not include any stereotypes. As is the standard for all evolutionary adaptation, the human muscle system would evolve in its efforts to increase survivability. It is clear that the evolution of eyelid muscles is based upon how humans lived in their respective environments. We focused on the orbicularis oculi muscle, which is the main composition of the eyelid, especially the preseptal portion (Fig. 3).
Fig. 3.

(A) One year after a conventional double eyelidplasty. As a clue of a past evolutional process, notice the aggravation of vertical tension on the epicanthus and attenuated medial crease. This eyelid is similar with the stage of compressional stress before the loss of the midlateral supratarsal crease in the eyelid's evolution. (B) A natural Asian eyelid with an epicanthus and incomplete presence of an attenuated supratarsal crease. Notice the loss of medial crease, epicanthal bulging, appearance of lesser crease along the malpositioned preseptal muscle, and skin fold of the lower eyelid. This eyelid shows vestiges of the eyelid's evolution.
Lee at al first stated that the orbicularis oculi muscle fibers running through the epicanthal fold mostly belong to the preseptal portion.10 They thought that selective resection of the orbicularis oculi muscle could reduce the epicanthus. Hirohiko et al and Yulan et al verified that the preseptal orbicularis muscle was the anatomical etiologic factor of the epicanthus in their anatomical examination.11 12 Hirohiko et al found that the preseptal orbicularis fasciculi ran obliquely around the epicanthus and coincided with the direction of the epicanthus in their anatomical study. They also reasoned that the epicanthus formation depended on the intermuscular fibers of the oblique direction of the preseptal orbicularis muscle. Beside anatomical studies, we found clinical evidence from botulinum injection of preseptal orbicularis muscle. To confirm the significance of the upper preseptal orbicularis oculi muscle, we tried botulinum injection of medial preseptal orbicularis muscle. We observed that the epicanthal bulging gets attenuated after botulinum injection of the preseptal portion of upper medial orbicularis muscle. We therefore concluded that epicanthal bulging and a lesser crease are associated with preseptal orbicularis muscle. We also could guess the displacement of preseptal orbicularis muscle from the results of a botulinum injection. After a botulinum injection, a higher crease could be formed more easily by tape or stick under lesser epicanthal tension (Fig. 4). This means that the epicanthus inhibits the formation of a double eyelid. There was no improvement of the epicanthus after botulinum injection on the preseptal portion of lower medial orbicularis muscle. We postulated that the key to the epicanthus is the upper preseptal orbicularis muscle. We focused on the developmental mechanism of epicanthal formation and the role of the orbicularis oculi muscle in the evolution of the eyelid.
Fig. 4.
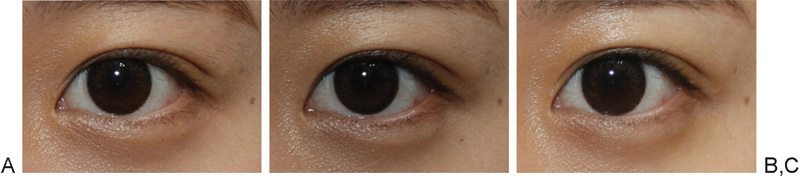
(A) Preinjection view. Notice the epicanthal bulging. (B) Ten days after injection of botulinum toxin. The epicanthal bulging decreased after botulinum toxin injection on medial preseptal orbicularis oculi muscle. (C) The higher medial crease can be formed better by stick and sustained more stably under weakened epicanthal tension.
What are the differences in orbicularis oculi muscle between a double eyelid without the epicanthus and an Asian single eyelid with the epicanthus? The orbicularis oculi muscle of the upper eyelid is known to be hypertrophied in Asians. Hirohiko et al found that the thickness of orbicularis muscle was different in a double eyelid and single eyelid in the Japanese population: It was thinner at the skin crease and at 10 mm from the eyelid margin in double eyelids, whereas it was10 mm from the eyelid margin in the single eyelid upon microscopic examination. The location of 10 mm from the eyelid margin marks the location of the preseptal portion of orbicularis muscle.11
Why did the preseptal orbicularis oculi muscle become thickened or hypertrophied? We do not know the etiologies exactly. We can find a clue from the causal relationship between climate factors and frowning. Climate factors such as the strong ultraviolet light, the Siberian cold, and the yellow dust of northeast Asia can be potential causes of excessive frowning, and repeated excessive frowning can induce orbicularis muscle hypertrophy (Fig. 2). Anthropologists have already presumed these factors to be causes of the epicanthus. There would be a strong repeated contraction of upper orbicularis muscle and depressor supercilii muscle in the Asian eyelid from frowning. Excessive muscle contraction would be an unavoidable action in the protection of eyes from environmental harshness. Hence, environmental adaptation would be a basic cause for the formation of the epicanthus.
We can understand muscle hypertrophy reasonably, but why were the preseptal muscle fibers displaced? We reasoned that hypertrophy of the orbicularis muscle and resultant attenuation/detachment of the aponeurotic expansion is the main cause of gravitational displacement and gradual malposition of preseptal orbicularis muscle (Fig. 5). Electron microscopic studies have confirmed that aponeurotic fibers penetrate the orbicularis muscle in both single and double eyelids of Asians. This finding suggests that Sayoc's theory of the “levator expansion” had been incorrect.13 Cheng et al stated that the orbicularis muscle bundles are arrayed in a stratified manner and muscle tissues are dense in the group without double eyelid, also that levator fibers do not pass through the muscle in their microscopic examination. And in double eyelids formed gradually after adolescence, orbicularis muscle tissue was denser than that of the muscle bundles lying transverse in double eyelids formed congenitally. They stated that in the group with double eyelids that formed gradually, levator aponeurosis fibers which penetrated through orbicularis muscle were looser than those seen in the double eyelid formed congenitally. It was shown that when orbicularis muscle bundles were arrayed sparsely and spacing was larger, levator aponeurosis fibers penetrate easily through orbicularis bundles and fuse with subcutaneous fibers in microscopic examination. When spacing is tighter, levator fibers were not observed to pass through muscle.14 This finding can mean that when excessive hypertrophy of orbicularis muscle develops, levator expansion can become sparse or loose, eventually nearly effaced in the anterior lamella during the eyelid's evolution.
Fig. 5.
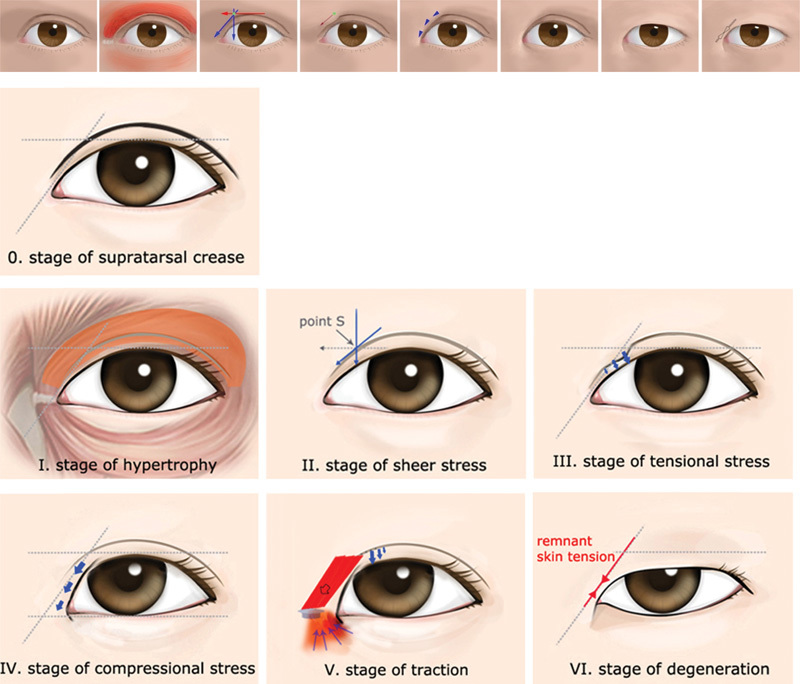
The stages of the evolution of the eyelid according to the main action of the orbicularis oculi muscle in Kwon's theory. Loss of a medial crease, formation of the epicanthus, loss of a midlateral crease, and formation of the epiblepharon occur in sequence.
Why does the supratarsal crease not exist although aponeurotic fibers do penetrate the orbicularis muscle in the Asian single eyelid? The answer is not “not previously existed,” but “lost” during evolution. The complete detachment of attenuated aponeurotic expansion to subcutaneous tissue can occur by additional tensional stress such as contraction of the orbicularis muscle and the depressor supercilii muscle. During frowning, the levator aponeurotic fibers get tightened and more vulnerable to tensional stress by muscles of anterior lamella. The possible locations of aponeurotic detachment are (1) beneath/within the orbicularis muscle, which results in crease loss and gravitational displacement of the anterior lamella, or (2) over the orbicularis muscle, which results in crease loss and only skin displacement. We reasoned that loss of medial crease and displacement of preseptal muscle occurred inceptively by this detachment mechanism on point S as shown in Fig. 5.
The stages of eyelid evolution according to the main action of the orbicularis oculi muscle in Kwon's theory (Fig. 5):
Hypertrophy: The hypertrophy of orbicularis oculi muscle and depressor supercilii muscle develop by repeated frowning. The hypertrophy of the orbicularis oculi muscle causes attenuation of the aponeurotic expansion, which penetrates through the orbicularis muscle. The aponeurotic penetrations loosen and become sparse.
Sheer stress: Complete detachment of aponeurotic expansions with loss of supratarsal crease takes place on point S by sheer stress. The detachment of aponeurotic fibers can occur beneath the orbicularis muscle or on the orbicularis muscle. Orbicularis oculi muscle contraction acts as sheer tensional stress with depressor supercilii muscle. The depressor supercilii muscle plays an ancillary role.
Tensional stress: The successive loss of medial crease below point S results from displacement of preseptal orbicularis oculi muscle toward eyelash and the vicious cycle between malpositioned muscle hypertrophy and crease loss. The orbicularis oculi muscle contraction mainly acts as tensional stress on the remaining aponeurotic fibers and medial crease.
Compressional stress: Excessive contraction of the orbicularis oculi muscle acts as compressional stress on the overlying skin of the upper medial eyelid with resultant vertical skin shortage and tension. The tight tension band develops due to vertical skin shortening of the upper medial eyelid.
Traction and tensional stress: Contraction of the orbicularis oculi muscle acts as tensional stress on the remaining supratarsal crease, resulting in successive loss of the supratarsal crease on the upper eyelid superiorly, and/or acts as traction force causing skin tent toward point P on the lower eyelid inferiorly. During and after formation of a tight tension band by vertical skin shortage, the orbicularis oculi muscle contraction causes a prominent skin fold on the lower eyelid by pulling-up the muscle point of origin (like setting up a tent pole) during contraction. The preseptal orbicularis muscle pulls up its origin superolaterally with a skin tent on the lower eyelid during contraction.
Degeneration: Atrophy of the orbicularis oculi muscle and accompanying degenerative fibrosis develop, leaving the epicanthus with an incomplete crease or epicanthus without a crease. The hypertrophied orbicularis oculi muscle becomes atrophied and replaced by fibrosis, but there remains vertical skin shortage and tension left on the upper eyelid and skin fold and wrinkles on the lower eyelid. Also there has been left centripetal fibrosis toward point P in Fig. 6 under the skin of the lower eyelid.
Fig. 6.
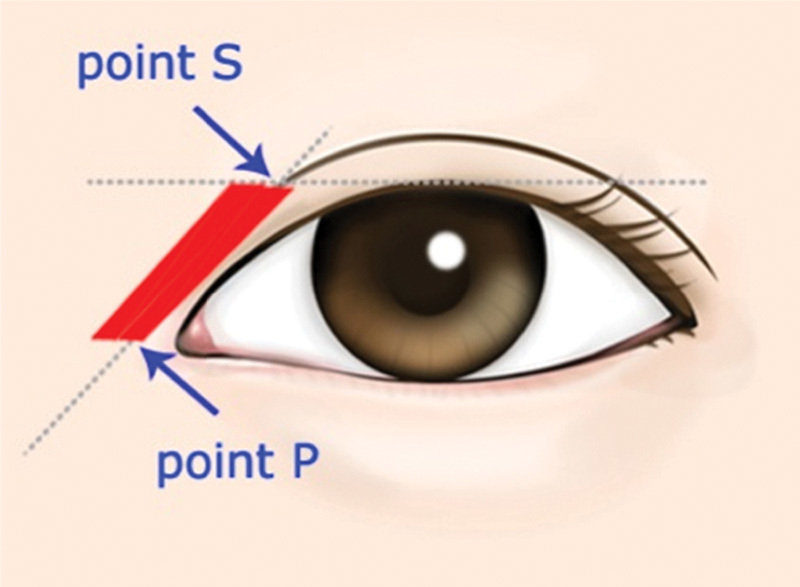
Schematic diagram for the formation of a tension band in the early compressional stage. Point S: It is point of the highest sheer stress. Point P: It is the inferior end of the tension band (lateral end of preseptal orbicularis muscle origin on the medial canthal ligament) and acts as a pulling-up tether, like setting up a tent pole, during contraction of the orbicularis muscle. The medial canthal ligament can be elongated and displaced consequently by a repeated traction mechanism.
We think that the hypertrophied orbicularis oculi muscle and the depressor supercilii muscle are the main reasons for the initial loss of the medial crease. The depressor supercilii muscle would play an ancillary role in this process. The highest sheer tensional stress would be at point S. Point S is the spot on which the tensional vectors of the depressor supercilii muscle, medial orbicularis muscle, and middle orbicularis muscle cross, and sheer tensional stress is concentrated. We already know that there is a high incidence and hyperactivity of hypertrophic scar at this point. And point S is the inceptive point at which surgical crease begins to fade away after a double eyelidplasty. Repeated sheer stress against aponeurotic expansion causes complete detachment of each aponeurotic fiber gradually, which already had been attenuated by muscle hypertrophy. The detachment of aponeurotic fibers causes skin laxity with crease loss and gravitational displacement of preseptal orbicularis muscle toward eyelash. The constant dynamic pulling of malpositioned muscles under the skin of the upper medial eyelid acts as tensional stress on the remaining medial aponeurotic expansions. Tensional stress induces more attenuation or loss of medial crease successively. A gradual convex change of the skin surface is accompanied by muscle displacement and hypertrophy. The malposition of muscle and resultant stronger contraction viciously accelerate the loss of aponeurotic expansions and excessive muscle hypertrophy. The more the orbicularis oculi muscle becomes malpositioned and hypertrophied, the stronger the tensional stress becomes on aponeurotic expansions by contraction of orbicularis oculi. The excessive tensional stress by contraction of hypertrophied orbicularis oculi muscle causes complete loss of the medial crease. Subsequently, the vertical skin shortage along the malpositioned muscle can develop by excessive contraction of the preseptal orbicularis muscle, which acts as a compressional stress on the overlying skin of the upper medial eyelid. If the remaining midlateral supratarsal crease is lost immediately after loss of the medial crease for additional veiling, the compressional stress would be short and the skin fold on the lower eyelid would develop minimally. If loss of the remaining midlateral supratarsal crease is delayed, a tight tension band can form after skin shortening of the medial upper eyelid (Fig. 6). Additionally, the formation of a severe skin fold on the lower eyelid is accelerated by the upward traction of the origin point on the medial canthal ligament. We think that excessive contraction of the orbicularis muscle pulls up the muscle origin point of the medial canthal ligament, resulting in upward displacement whenever the muscle contracts. Upward displacement of the origin point causes development of skin tenting on the lower eyelid during muscle contraction. A relatively longer Asian medial canthal tendon would result from this traction mechanism. Elongation and consequent displacement of the medial canthal ligament would affect canthal distortion and skin fold. The skin fold on the lower eyelid is a secondary manifestation resulting from excessive preseptal orbicularis muscle contraction and the mechanism of upward traction at its origin point.
If tensional stress is sufficient for the detachment of aponeurotic expansions, complete loss of midlateral supratarsal crease occurs with less development of lower eyelid skin fold. The fusional part of the orbital septum and levator aponeurosis in Caucasian double eyelid is typically in the skin crease. If loss of the remaining supratarsal crease was delayed due to insufficient tensional stress, isolated attenuation of the supratarsal crease occurs or a lowered smaller crease is formed inferior to the fusional part with orbicularis muscle displacement. Also a severe skin fold could develop if loss of the remaining supratarsal crease is delayed. The time when complete loss of the supratarsal crease is accomplished, is the determining factor for the development of vertical skin shortage and the formation of severe skin fold. This process continues until the eye is veiled sufficiently by the epicanthus or the epiblepharon for eye protection. The end point of the evolutional process would be the time when the orbicularis oculi muscle does not need to contract excessively any more.
The epicanthal folds have been divided by Duke-Elder into four types depending on the anatomical site from which the fold arises.15 They are supraciliary, palpebral, tarsal, and inverted types. This classification is based on the horizontal position of point P (Fig. 6). However, we think this classification is not significant clinically for Asian eyelids. We cannot find any supraciliary type in Asian eyelids, and this classification focuses on epicanthus-related skin fold similar to most previous surgical methods. When we perform an epicanthoplasty only in a single eyelid, the most important factor is the amount of veiled canthus by the epicanthus. Because the epicanthal deformity results from displacement of the upper orbicularis muscle, and the main sequelae of the epicanthal evolution are vertical skin shortage and skin tension in all aspects of Asian double eyelidplasty, vertical skin tension on the upper eyelid and malpositioned preseptal orbicularis muscle are the most significant factors in the surgery of combined double eyelidplasty instead of point P location (Figs. 7 and 8).
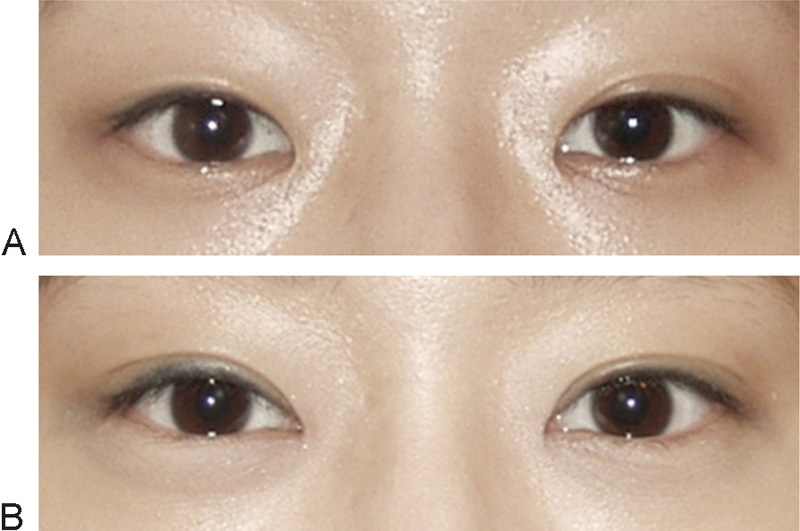
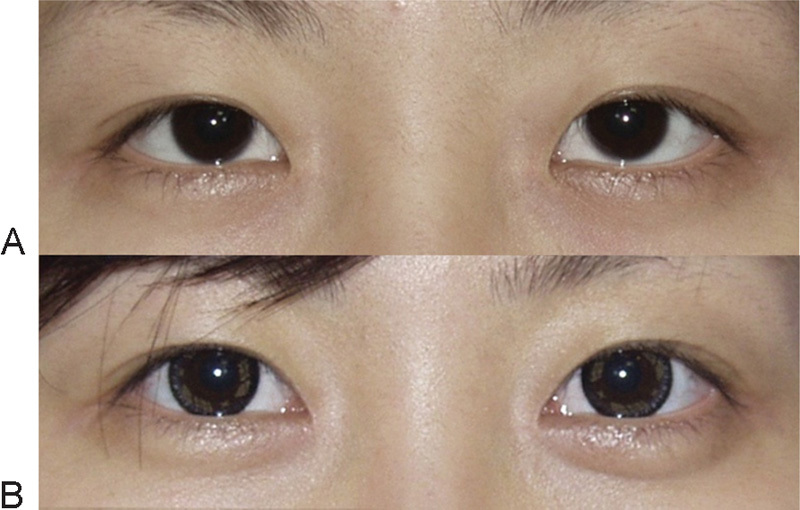
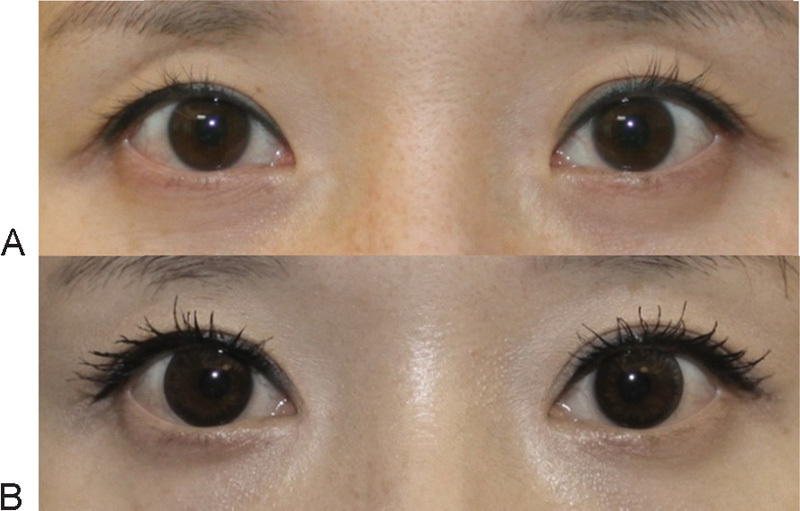
Fig. 7.
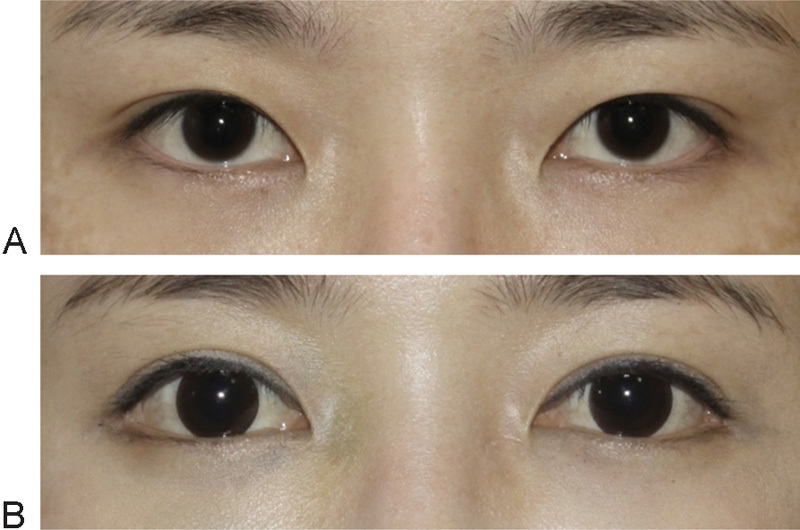
We can convert easily an infold-type crease to in-outfold type crease by a combined epicanthoplasty and double eyelidplasty. (A) Preoperative view. (B) An epicanthoplasty resolved the vertical skin tension and orbicularis muscle displacement for a higher crease formation. Combined epicanthoplasty and double eyelidplasty, with a lateral canthoplasty 2 years postoperative . There are cosmetic lenses on the eyes.
Fig. 8.
A case of severe skin tension on the upper eyelid. (A) A result of conventional double eyelidplasty without epicanthoplasty. We can see blepharoptosis, sausage phenomenon, an attenuated crease with a drooping eyelid that is veiling the eyelash line. (B) Three months postoperative. Revisional double eyelid surgery, epicanthoplasty, blepharoptosis correction improved the surgery-look eye and refined the epicanthus and crease. There are cosmetic lenses on the eyes .
The more tension on upper eyelid skin, the longer the transverse incision and the more horizontal advancement flap will be necessary for adding skin in the vertical dimension in the epicanthoplasty. According to the skin tension present, the design for the median end point of the incision or intraoperative lengthening of incision can vary. However, it is difficult to assess skin tension quantitatively through inspection. We can roughly estimate skin tension through simulating the double eyelid with forceps in the consultation room. We propose an improved classification of epicanthus taking into account the related supratarsal crease (Fig. 9).
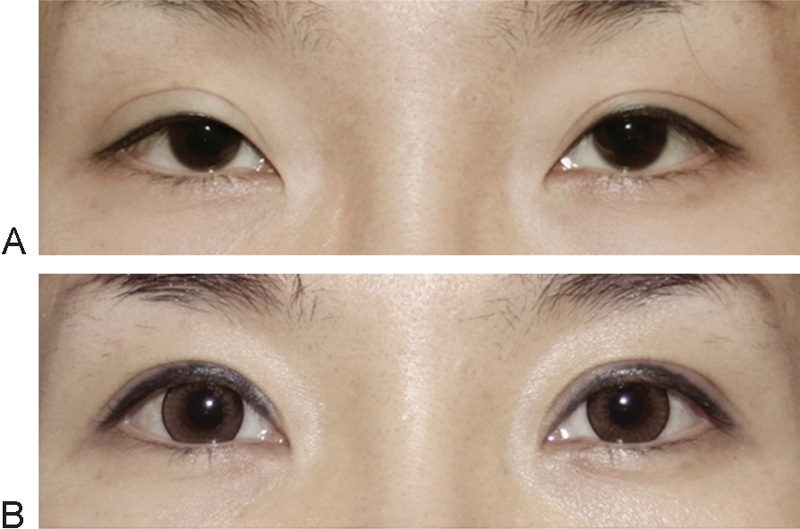
Fig. 9.
Classification of the epicanthus in relation to the supratarsal crease. Type I: Attenuated original crease without an epicanthus (exophthalmic Asian eyelid). Type II: Minimal epicanthus without a crease (without epiblepharon). Type III: Epicanthus with an attenuated original crease. Type IV: Epicanthus with a lowered infold crease. Type V: Epicanthus without a crease (epicanthus and epiblepharon ).
In conclusion, the epicanthus is a remnant manifestation of the eyelid's evolution that resulted from hypertrophy of the upper orbicularis muscle and related aponeurotic attenuation. The more fibrous tissues and less muscle of the epicanthal region would be due to subsequent degenerative changes. Increased blood supply induced by a hypertrophied orbicularis muscle and climate factors would cause hypertrophy and pseudoherniation of preaponeurotic fat. Displacement of the orbicularis muscle and fat pad would affect the levator muscle and Müller's muscle. A relatively longer medial canthal ligament and underdeveloped nasal bone would be additional evolutional manifestations by hypertrophy of the orbicularis oculi and excessive tension.16 Using this theory, the primary purpose of an Asian epicanthoplasty is the anatomical restoration of the medial canthus and eyelid soft tissues, which are basic to double eyelid formation in Asian eyelids. For this we apply the devolutional concept that reverses the evolutional processes.
Epicanthoplasty Based on the Devolutional Concept (Kwon's Method)
The clinical significance of the epicanthal fold is mainly associated with a double eyelidplasty in Asians. The epicanthal fold is worsened when performing a double eyelidplasty without epicanthoplasty as a double eyelid aggravates tension on the epicanthal skin. The aesthetic results of a double eyelidplasty without epicanthoplasty tend to be unnatural or unattractive. When performing outfold-type eyelidplasty without epicanthoplasty, prolonged swelling retention (so-called sausage phenomenon) occurs due to the blockage of lymphatic flow by vertical tension and the fading away of double eyelids are frequently noted (Figs. 9 and 10). Unless the epicanthoplasty releases skin tension and removes the potential inhibition factors of crease loss, the surgical crease will not look natural or not be able to last over time (Fig. 11).
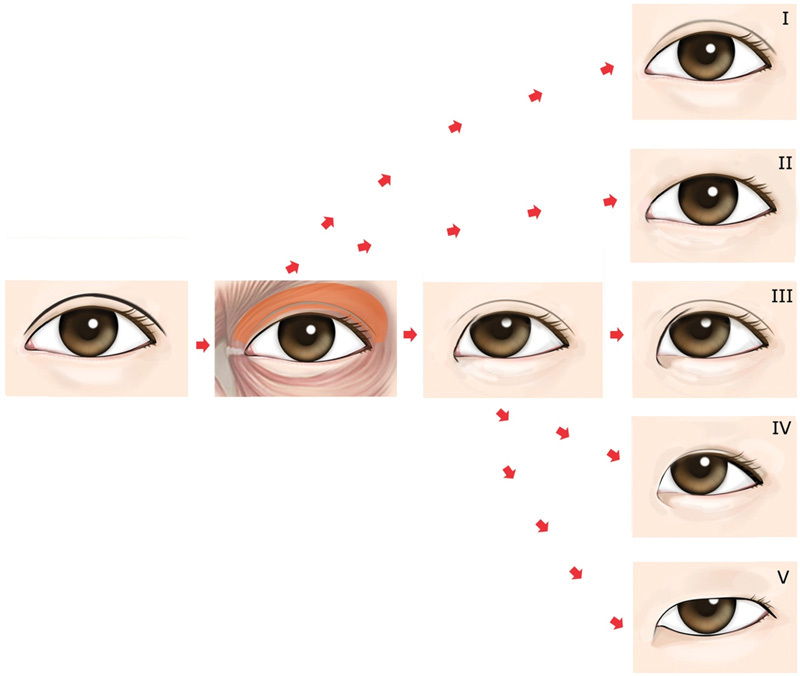
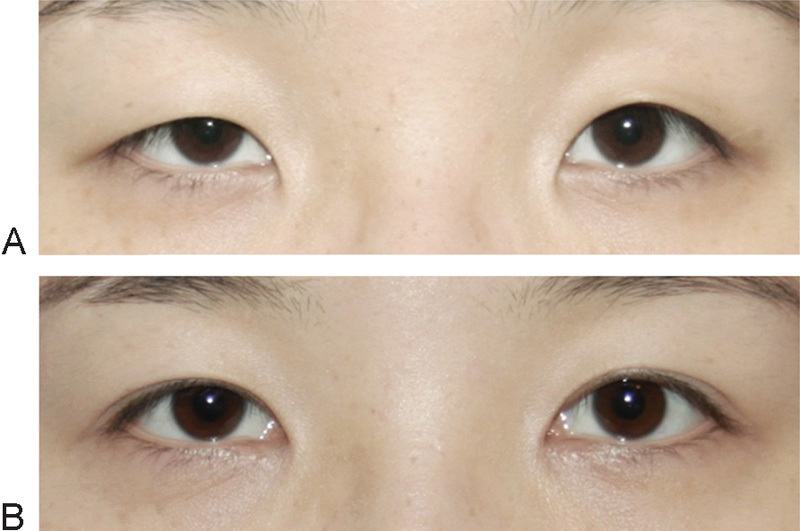
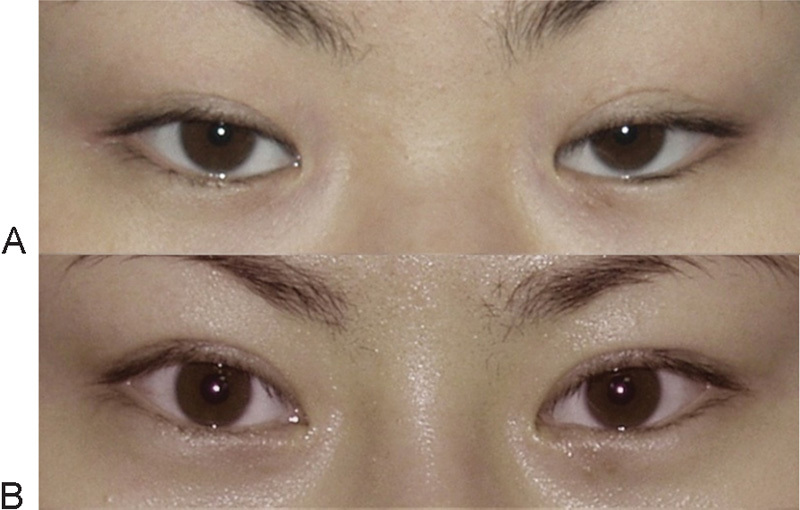
Fig. 10.
(A) A result of double eyelidplasty without epicanthoplasty. Sausage phenomenon, prolonged swelling retention due to blockage of lymphatic drainage by vertical tension. (B) Five months postoperative. Epicanthoplasty and revisional double eyelid surgery refined the surgery-look eyes. Devolutional epicanthoplasty resolves vertical tension intraoperatively and prevents retention of edema.
Fig. 11.
(A) A result of conventional double eyelidplasty without epicanthoplasty. Notice loss of surgical crease on right eyelid. (B) Three months postoperative. Epicanthoplasty and revisional double eyelid surgery refined the epicanthus and the double eyelid.
In the early days of epicanthoplasty surgery, numerous surgical methods based on the concept of local flaps were introduced to correct the redundant skin fold. However, their disadvantages such as difficulty in design and resultant prominent scars limited their use. Recently, new epicanthoplasty methods have been introduced to correct Asian anatomical differences such as excessive skin, abnormal skin tension, malpositioned orbicularis muscle, fibroadipose tissue, elongated medial canthal ligament, and so on. However, none could be a treatment of choice as they lacked an exact understanding of the malposition of the upper orbicularis muscle and vertical skin tension in relation to the double eyelid. The surgical methods based on a defective/inadequate understanding of the true nature of the epicanthus are not optimal for an Asian eyelidplasty. We developed an epicanthoplasty using a devolutional method based on our understanding of epicanthal formation and its causal relationship with the double eyelid.
What we consider in an epicanthoplasty in relation to double eyelidplasty preoperatively:
Exposing the true eyelid margin of the medial canthus and the medial upper eyelid
Unfolding of the lower skin fold and accessory wrinkles
Debulking of fibrous tissue on the upper canthal region for easy skin folding
Repositioning of the malpositioned upper orbicularis oculi muscle and soft tissues of the anterior lamella
Releasing the underlying vertical tension in relation to the designed crease
Restoring the horizontal canthal shape if distorted
Correcting the elongated, displaced medial canthal ligament
Preventing orbicularis oculi muscle reactivation as a cause of double eyelid crease disappearance
Avoiding any noticeable scar in the medial canthal area
What we do in a combined epicanthoplasty and double eyelidplasty in sequence:
Design both the epicanthoplasty and double eyelid surgery simultaneously
Mark the marginal transverse incision along the skin tension line of the original canthal margin on the lower eyelid
Incision for the epicanthoplasty and double eyelidplasty
Elevation of a composite flap including skin and fibrosis on the lower eyelid
Subcutaneous dissection of the upper eyelid
Shaving excessive fibrous tissues under the upper epicanthal skin flap, if necessary
Detachment and superomedial repositioning of the preseptal orbicularis oculi muscle
Additional releasing of fibrosis on the lower eyelid for restoration of canthal shape, if necessary
Correction of the medial canthal ligament, if necessary
Advancement of the skin flap to add vertical skin length for tensionless crease, if necessary
Confirming the absence of vertical tension and smooth skin folding along the designed crease by simulation of crease folding
Anchoring canthal skin on the turning axis of the medial canthal tendon as first anchoring of the double eyelid with anchoring of the nasal skin flap simultaneously
Anchoring the suture for crease formation (double eyelidplasty)
Skin closure
Botulinum injection for additional relaxation of the orbicularis muscle, if needed
The incision is designed along the original canthal margin of the lower eyelid, preserving the skin tension line. The shape of the incision line is not always transverse in the relaxed state due to past skin tension on the lower eyelid. However, when medial traction is applied for restoration of the original horizontal canthal shape, the drawn design becomes nearly transverse. The location of the median end of the incision (Fig. 12, point D) can vary according to the design of the combined double eyelidplasty. When a high parallel crease is planned, point D is located more medially. Due to the pulling-up of point P just as in setting up a tent pole, one-quarter of centripetal fibrosis develops under the palpebral skin, but we can use this fibrosis to reduce the discrepancy of each flap in the skin closure of an epicanthoplasty (Fig. 12). It is a good condition for a devolutional eyelidplasty, unlike the vertical skin shortage of the upper eyelid. According to the location of point P (the pulling-up point, the lateral end point of the preseptal orbicularis muscle origin) (Fig. 12), the strength of traction force on palpebral skin, the elongation and displacement of the medial canthal ligament, and the shape of the skin fold varies.
Fig. 12.
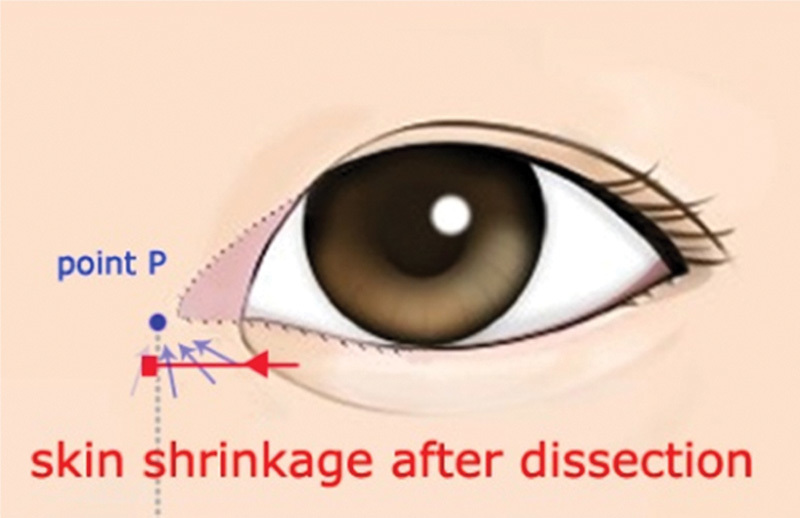
Notice the direction of remnant fibrosis on lower eyelid (gray arrows). After fibrocutaneous dissection of the lower eyelid, we can expect transverse flap shrinkage by centripetal fibrosis. Point P acts as a pulling-up tether under the skin, like setting up a tent pole, during the eyelid's evolution. There has been one-quarter of centripetal fibrosis left on the lower eyelid. The shape of the skin fold on the lower eyelid varies according to the location of point P, strength of traction force on palpebral skin, and the elongation and displacement of the medial canthal ligament.
We can presume that when the original supratarsal crease is high, point P (Fig. 12) is positioned more medially. When point P is located much below the horizon of the lower eyelid (it means more elongation and downward displacement of the medial canthal tendon) and the force of traction is strong on the palpebral skin, distortion of the canthal shape including severe eversion of the lower eyelid can occur in addition to skin fold and wrinkles (Fig. 13). However, we should bear in mind that this distortion is caused mainly by skin traction, and there is no structural change in the canthus itself or the lower orbicularis muscle. This is very important when we design the incision line for a devolutional epicanthoplasty. In a severely distorted case, the marginal skin tension line of the original canthus exists much apart from the eyelash at a relaxed state. If we want to restore the original shape of the canthus, we should preserve the original skin tension line of the canthal margin, and the design should be drawn just below the original skin tension line. After incision and dissection of the lower fibrocutaneous flap, we can see the spontaneous restoration of the everted canthal shape intraoperatively. We can easily find the original transverse skin tension line, which exists along the canthal margin by traction that restores the canthus to an original shape. Also we can correct an elongated or displaced medial canthal ligament, if needed. We can often see the rudimentary line of a supratarsal crease in the single eyelid of Asians—and hence the design of the incision line for devolutional epicanthoplasty.
Fig. 13.
Severe skin tension on the upper eyelid and everted lower eyelid. (A) Preoperative view. (B) Combined epicanthoplasty and double eyelidplasty, 5 weeks postoperative .
On the lower eyelid, a fibrocutaneous flap (a composite flap with skin and fibrosis) dissection is performed for releasing one-quarter of the centripetal fibrosis that resulted from upward skin traction. The dissection plane for flap dissection is between the fibrosis and muscle. It is better to preserve centripetal fibrosis within the fibrocutaneous flap during dissection so that the longer lower flap more easily matches up with the shorter canthal flap at skin closure. If the fibrocutaneous flap is elevated evenly over muscle, we can expect transverse shrinkage of the flap; therefore, trimming of the flap is not necessary in most cases. When the fibrocutaneous flap is elevated in both the upper eyelid and lower eyelid, point D (Fig. 14) of the nasal flap moves toward superolaterally. It is better for point D of the nasal flap to move laterally if we consider vertical skin shortage and crease formation on the upper eyelid. Therefore, the fibrocutaneous flap on the lower eyelid and the cutaneous flap on the upper eyelid are both most beneficial (Fig. 14).
Fig. 14.
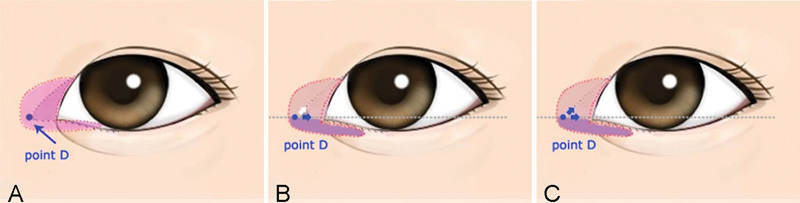
(A) Range of dissection. Fibrocutaneous dissection of the lower eyelid is done minimally until the skin fold completely disappears. It is not necessary to dissect to the end of the fold. Subcutaneous dissection of the upper eyelid and reposition of muscle are done gradually until the designed crease is formed without tension (B). When the fibrocutaneous flap is elevated in the lower eyelid and the cutaneous flap in upper eyelid, point D of the nasal flap tends to move laterally. Notice the transverse shrinkage of the fibrocutaneous flap on the lower eyelid. (C) When the fibrocutaneous flap is elevated in both the upper and lower eyelids, point D of the nasal flap tends to move superolaterally .
The even elevation of the fibrocutaneous flap through an accurate plane is also important for inducing spontaneous restoration of the canthus toward its original anatomical shape. We leave the lower orbicularis oculi muscle intact to restore the original canthal shape and to prevent atrophy of the muscle, resulting in eversion of the lower eyelid and loss of the lower eyelid love band.
On the upper eyelid, the dissection plane changes to a subcutaneous plane to make a thinner skin flap for a natural skin folding on the designed crease and to prevent fibrous shrinkage in the vertical dimension in a combined double eyelidplasty. After subcutaneous dissection, selective detachment and superomedial reposition of the preseptal portion of the muscle can reverse malpositioned soft tissue and remove the primary cause of the epicanthal formation without functional impairment (Fig. 15). An anchoring suture for a double eyelid formation prevents relapse of the orbicularis muscle displacement after repositioning. Kwon et al have described that a superior reposition of the upper orbicularis muscle is significant in revisional epicanthoplasty.17 In our surgical experience, after muscle detachment and reposition, the shape of the distorted canthus can be restored spontaneously or by additional release of remnant pericanthal fibrous tissues. When performing a combined double eyelidplasty, we can advance the skin flap laterally for the vertical skin lengthening of the upper eyelid. In case of a double eyelidplasty for a high outfold type that needs more skin relaxation, lengthening of the incision and flap advancement are frequently needed. When there is increased tension on the upper eyelid skin, the longer incision line for the horizontal advancement of a flap will be necessary for adding skin in the vertical dimension. It is better that lengthening of the incision is adjusted intraoperatively as little as possible after other dissection and repositioning maneuvers are done.
Fig. 15.
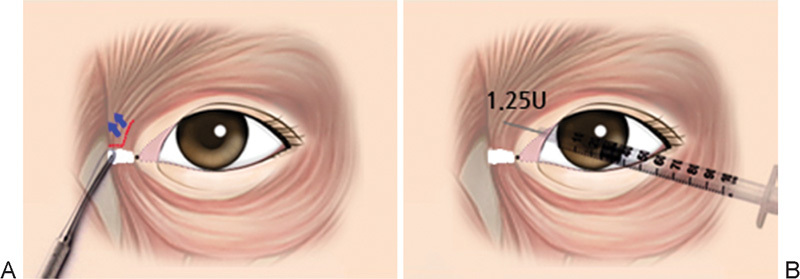
(A) Detachment and superomedial reposition of a malpositioned medial orbicularis oculi muscle in an epicanthoplasty. Anchoring suture for double eyelid formation prevent relapse of orbicularis muscle displacement. (B) 1.25 to 2.5 U of botulinum is injected into the medial orbicularis muscle and depressor supercilii .
Depending on the case, 1.25 to 2.5 U of botulinum can be injected into the medial orbicularis muscle and/or depressor supercilii muscle for additional muscle relaxation and atrophy. The effect of botulinum lasts approximately 3 or 4 months, which is enough time for acute wound healing and tissue repositioning.18 We have experienced the effectiveness of botulinum with a decreased occurrence of a medial hypertrophic scar. It means less tensional stress on the wound and less risk of fading-away of the surgical crease. Botulinum toxin is effective for lessening tensional stress on the crease and weaker hypertrophic wound healing. Patients also feel more comfortable during the early wound healing period after botulinum injection due to less hypertrophic activity on the wound. Pretreatment of botulinum also can be considered in patients who have an obviously hypertrophic muscle and increased skin tension onthe upper eyelid (Fig. 15).
Kwon's method is based on the devolutional concept that restores original pericanthal structure for stable double eyelid formation without anatomical distortion. It can be accomplished by just rearranging the soft tissue without the risk of severe complications or noticeable scar. We think that our theory of eyelid evolution and surgical method could help surgeons to understand the dynamics of the epicanthus and simplify the epicanthoplasty for universal use in Asian eyelidplasty.
Unlike conventional methods, Kwon's method has additional aesthetic effects such as (Figs. 16 17 18 19):
Fig.16.
Notice the spontaneous reinforcement of the lower eyelid love band after a devolutional epicanthoplasty; it develops by the relative hypertrophy of the lower orbicularis oculi muscle. Improvement of mild blepharoptosis also appeared. (A) Preoperative view. (B) Epicanthoplasty, 3 months postoperative. This case shows the relationship of three muscles (the upper orbicularis oculi muscle, lower orbicularis oculi muscle, and levator muscle ).
Fig. 17.
By devolutional epicanthoplasty, we can improve eyelash prickling that results from eyelid inversion by epicanthal traction. (A) Preoperative view. (B) Combined epicanthoplasty and double eyelidplasty with ptosis correction, 5 months postoperative .
Fig. 18.
Notice the spontaneous improvement in edema retention after a devolutional epicanthoplasty. It results from resolving vertical tension and normalizing lymphatic drainage. (A) Natural Asian eyelid with accessory lacrimal punctum on right lower eyelid, preoperative view. (B) Epicanthoplasty, 1 year postoperative. This case shows the causal relationship between vertical tension and the prolongation of edema .
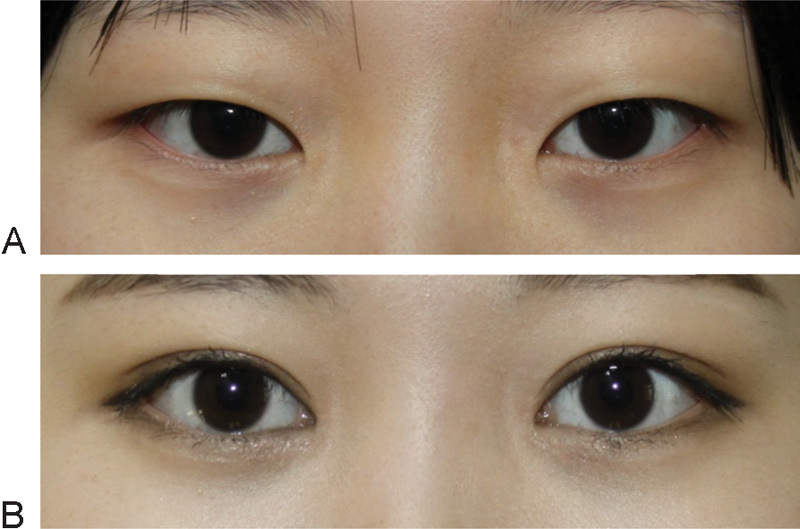
Fig. 19.
We can convert the infold type to an outfold type of double eyelid by combining epicanthoplasty and double eyelidplasty. (A) Preoperative view. (B) Combined epicanthoplasty and double eyelidplasty with fat injection in the upper eyelid, 3 months postoperative .
Improvement of accessory wrinkles around the fold and dark circles by releasing skin fibrosis on lower eyelid
Improvement of canthal distortion including inversion and eversion
Improvement of prolonged edema from lymphatic blockage that is caused by vertical tension
Restoration of the horizontal axis of the lower canthal line from a slanted shape, between the punctum and canthal angle
Reinforcement of the love band by hypertrophy of the lower orbicularis oculi muscle relative to atrophy of the upper orbicularis oculi muscle
Ease in converting the infold type crease to outfold type
Ease in refining the unnatural outfold crease that was formed by a double eyelidplasty only
What Should We Not Do in an Epicanthoplasty?
Do not dissect the lower orbicularis muscle (no myotomy or myectomy): Injury to the lower orbicularis muscle results in eversion, loss of love band, and atrophy of the lower eyelid
Do not remove the fibrosis of the lower eyelid
Do not trim the fibrocutaneous flap of the lower eyelid if possible: Avoid tension and eversion, if possible. Direct closure can be accomplished in most cases if the fibrocutaneous flap is elevated evenly.
Do not destroy the skin tension line that exists along original canthal eyelid margin for an aesthetically attractive eyeline
Structural Eyelidplasty in the Asian Eyelid: Combined Epicanthoplasty and Double Eyelidplasty as One Surgery
Until now, it was thought that an epicanthoplasty was just an ancillary procedure because plastic surgeons have not had a full understanding of the epicanthus. It could be argued that there is no difference in the basic anatomical structure of the eyelid between Asians and other ethnicities. The presence of the epicanthus or the absence of a supratarsal crease is one of the differences of phenotype based on environment. For an Asian blepharoplasty, we need to understand the evolution of the eyelid and reverse evolutional processes to increase the stability of surgical crease with a minimally invasive technique. An epicanthoplasty should be considered part of the core surgery for Asian double eyelidplasty, as there is a close relationship between the loss of the supratarsal crease and development of the epicanthus and epiblepharon. There are many differences between a devolutional eyelidplasty and a conventional eyelidplasty not based on the devolutional concept. The epicanthus and epiblepharon is the same manifestation except for their location. Both are composed of preseptal orbicularis muscle and degenerative fibrous tissues that have replaced atrophied orbicularis oculi muscles. There are more incidences of mild blepharoptosis in Asian eyelids. We think mild blepharoptosis in the Asian eyelid is related to the eyelid's evolution. After the evolutional process, the loading conditions of the levator muscle worsened. The fibrous tissues within the epicanthus and the epiblepharon, vertical skin tension on the upper eyelid, hypertrophied orbicularis oculi muscle, and hypertrophied preaponeurotic fat pad increase loading onto the levator and Müller muscle, and act as causal factors of blepharoptosis. Patients can often experience the improvement of mild blepharoptosis after devolutional epicanthoplasty. When we evaluate blepharoptosis, we should consider the epicanthus-related factors. When we perform blepharoptosis surgery with a devolutional epicanthoplasty simultaneously, correction of blepharoptosis becomes complete and better results are expected. Also in devolutional eyelidplasty, destructive procedures on the surgical crease for stronger adhesion become less necessary. The tensional stress on the crease by vertical skin tension is the main cause of crease loss after a double eyelidplasty in Asians. Contraction of a malpositioned orbicularis oculi muscle in a vertical direction is also a potential cause of tensional stress on surgical crease. Because we have resolved the possible causes of crease loss with devolutional epicanthoplasty, an aggressive adhesion performed by a conventional method is less necessary. In more cases, we can apply a nonincisional method for crease formation except for an excessively thick skin condition with true epiblepharon. When we must remove excessive and malpositioned soft tissues in cases of droopy eyelids with epiblepharon, a conservative resection for resolving the displaced soft tissues of the anterior lamella and partial removal of preaponeurotic fat in the posterior lamella is enough without experiencing unnecessary tissue injury. The overactive resection and resultant unnecessary tissue injury only cause prolonged swelling and a depression scar. A review of the conventional procedures for an Asian blepharoplasty and the theoretical background for adjusting to a devolutional Asian blepharoplasty is appropriate. With a better understanding of the eyelid's evolution and the epicanthus in relation to the double eyelid, an Asian double eyelidplasty needs to be refined more in combination with an epicanthoplasty.
Conclusion
We propose that the epicanthus developed in the eyelid's evolutionary process. Under this theory of the eyelid's evolution, we developed a new method for an Asian eyelidplasty. Through more than 5,000 cases of patients who already underwent a devolutional eyelidplasty, our method has proven to be a very satisfactory and universally applicable method for the Asian eyelid. The surgical outcomes are very natural (Fig. 20). We can lessen the rate of sausage phenomenon, loss of surgical crease, and hypertrophic scar. Many recent anatomical studies and clinical experience support our theory. Our epicanthoplasty is a surgery based on the devolutional concept that reverses evolutional processes, so it is the universal solution for the Asian epicanthus.
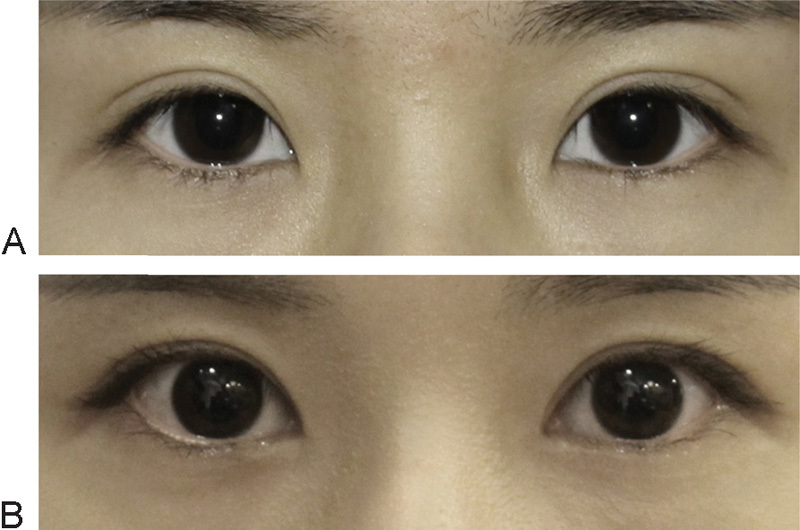
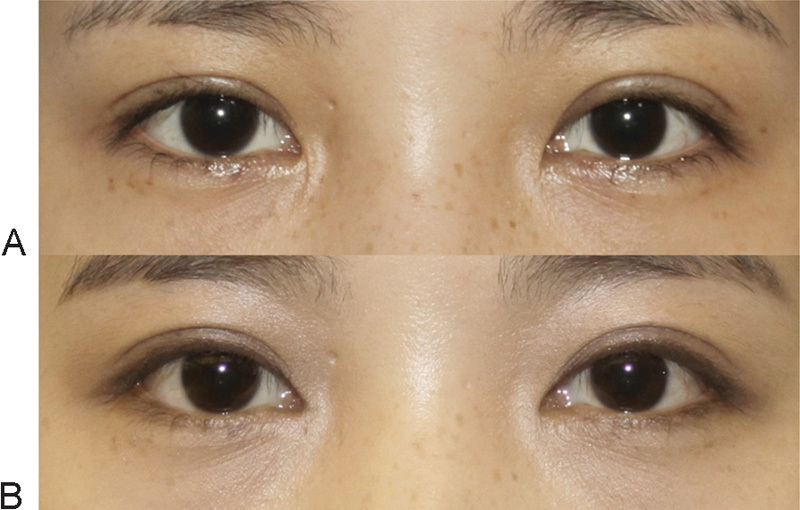
Fig. 20.
Combined epicanthoplasty and nonincisional double eyelidplasty, with blepharoptosis correction. (A) Preoperative view. (B) Three months postoperative .
An epicanthoplasty needs to be considered as a core surgery for the Asian double eyelidplasty, especially when forming the parallel-type of double eyelid. Epicanthoplasty is not an ancillary surgery in an Asian double eyelidplasty, but a combined epicanthoplasty and double eyelidplasty deserve one complete “structural eyelidplasty” for Asians. For a minimally invasive structural eyelidplasty, we need to reconsider the conventional procedure of a double eyelidplasty and ptosis correction under a devolutional concept. More research needs to be conducted on the eyelid's evolution and its mechanism.
Acknowledgment
We thank Sangah Oh, MD (Department of Plastic and Reconstructive Surgery, College of Medicine, Dankook University, Cheonan, South Korea) for help with the illustrations.
References
- 1.Park J I. Z-epicanthoplasty in Asian eyelids. Plast Reconstr Surg. 1996;98(4):602–609. doi: 10.1097/00006534-199609001-00002. [DOI] [PubMed] [Google Scholar]
- 2.Yoo W M Park S H Kwag D R Root z-epicanthoplasty in Asian eyelids Plast Reconstr Surg 200210962067–2071., discussion 2072–2073 [DOI] [PubMed] [Google Scholar]
- 3.Kao Y S, Lin C H, Fang R H. Epicanthoplasty with modified Y-V advancement procedure. Plast Reconstr Surg. 1998;102(6):1835–1841. doi: 10.1097/00006534-199811000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Oh Y W, Seul C H, Yoo W M. Medial epicanthoplasty using the skin redraping method. Plast Reconstr Surg. 2007;119(2):703–710. doi: 10.1097/01.prs.0000246713.59153.bb. [DOI] [PubMed] [Google Scholar]
- 5.del Campo A F. Surgical treatment of the epicanthal fold. Plast Reconstr Surg. 1984;73(4):566–571. doi: 10.1097/00006534-198404000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Ohmori K. Philadelphia, PA: Saunders; 1990. Aesthetic Surgery in the Asian Patient; pp. 2420–2426. [Google Scholar]
- 7.Von Ammon F A. Der epikanthus und das epiblepharon. Separatabdruck aus Behrendts und Hildebrand's Journal für Kinderkrankheiten. 1860;34:313. [Google Scholar]
- 8.Jurmain R, Kilgore L, Trevathan W, Ciochon R L. Independence, KY: Wadsworth-Cengage Learning; 2014. Introduction to Physical Anthropology. 2013–2014 ed; pp. 389–426. [Google Scholar]
- 9.Relethford J. New York: McGraw-Hill; 2012. The Human Species: An Introduction to Biological Anthropology, 9th ed; pp. 379–399. [Google Scholar]
- 10.Lee Y, Lee E, Park W J. Anchor epicanthoplasty combined with out-fold type double eyelidplasty for Asians: do we have to make an additional scar to correct the Asian epicanthal fold? Plast Reconstr Surg. 2000;105(5):1872–1880. doi: 10.1097/00006534-200004050-00042. [DOI] [PubMed] [Google Scholar]
- 11.Kakizaki H, Takahashi Y, Nakano T. et al. The causative factors or characteristics of the Asian double eyelid: an anatomic study. Ophthal Plast Reconstr Surg. 2012;28(5):376–381. doi: 10.1097/IOP.0b013e31825e6a88. [DOI] [PubMed] [Google Scholar]
- 12.Liu Y, Lei M, Wang Y, Mu X. Lazy S-curve epicanthoplasty in Asian blepharoplasty. Aesthetic Plast Surg. 2012;36(2):254–260. doi: 10.1007/s00266-011-9806-9. [DOI] [PubMed] [Google Scholar]
- 13.Sayoc B T. Absence of superior palpebral fold in slit eyes; an anatomic and physiologic explanation. Am J Ophthalmol. 1956;42(2):298–300. doi: 10.1016/0002-9394(56)90934-5. [DOI] [PubMed] [Google Scholar]
- 14.Cheng J, Xu F Z. Anatomic microstructure of the upper eyelid in the Oriental double eyelid. Plast Reconstr Surg. 2001;107(7):1665–1668. doi: 10.1097/00006534-200106000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Duke-Elder S, ed. Textbook of Ophthalmology St. Louis, MO: Mosby; 19524653–4658. [Google Scholar]
- 16.Cho B C, Lee K Y. Medial epicanthoplasty combined with plication of the medial canthal tendon in Asian eyelids. Plast Reconstr Surg. 2002;110(1):293–300, discussion 301. doi: 10.1097/00006534-200207000-00049. [DOI] [PubMed] [Google Scholar]
- 17.Kwon B S, Kong J S, Kim Y W, Kang S R. Corrective epicanthoplasty in patients with unnatural results of prior epicanthoplasty: rearrangement of the orbicularis oculi muscle above the medial canthal tendon. Ann Plast Surg. 2014;73(1):12–15. doi: 10.1097/SAP.0b013e318270386e. [DOI] [PubMed] [Google Scholar]
- 18.Okumus S, Coskun E, Erbagci I. et al. Botulinum toxin injections for blepharospasm prior to ocular surgeries. Clin Ophthalmol. 2012;6:579–583. doi: 10.2147/OPTH.S30277. [DOI] [PMC free article] [PubMed] [Google Scholar]


