Abstract
In contrast with Caucasian blepharoplasty, which is usually done for rejuvenation purposes, eyelid surgery for Asians is mainly done for cosmetic reasons. Here the authors present preoperative evaluation methods of Asian eyelids to overcome anatomical variations and determine the right aesthetic options. Proper selection of the most suitable operative methods guarantees optimal surgical results.
Keywords: Asian eyelid anatomy, Asian eyelid, eyelid anatomy, Asian eyelid morphology, Asian blepharoplasty, Asian double crease, Asian oculoplastic surgery, epicanthoplasty, blepharoptosis, eyelids
15 Things to Consider: Upper Lid, Palpebral Shape, and Lower Lid
Upper Lid
Forehead and Brow
Forehead wrinkles or hyperactive frontalis are often caused by hidden brow ptosis or blepharoptosis (Figs. 1 and 2). However, in a young patient who does not have thick skin or forehead wrinkles yet, it is difficult to find the hidden frontalis or levator hyperfunction. After correction of blepharoptosis, the brow usually descends and sets at a lower position (Fig. 3). To find this hidden hyperactivity, the Berke test is a useful tool.
Fig. 1.

(A) A young Asian woman without brow elevation. (B) Hyperactive frontalis due to hidden blepharoptosis.
Fig. 2.

(A) Without brow elevation. (B) Correction of ptosis improves brow position and frontalis hyperactivity.
Fig. 3.

(A) Preoperative primary gaze: margin reflex distance 1 (MRD1) = 2 mm. (B) Postoperative brow elevation. (C) Brow descends when postoperative primary gaze is MRD1 = 5.5 mm.
Berke Test
Try to hold the patient's brow while looking down as much as possible, then ask him to look to the front; check the position of lid margin while blocking the upward movement of the brow. Both eyelids are not always at the same level. The more ptotic eyelid tends to have a higher brow position and a forehead wrinkle. If one were to elevate the eyebrow by 10 mm, this will increase the size of the eye by 1.8 mm.1
Upper Lid Skin Fat Evaluation
Asians have thicker skin and a puffier eyelid (Fig. 4). Thicker skin has less of a tendency to loosen with time, but does not promote a natural crease line. With thick skin, pretarsal fullness is often observed, which needs to be corrected to create a more natural looking double fold. Hypertrophied medial and middle fat bags also hinder crease formation and exacerbate lateral hooding of upper lid skin. Sometimes, lacrimal gland prolapse also exaggerates the lateral bulge (Figs. 5 and 6). Some patients with highly extensible eyelid skin may have floppy eyelid syndrome (Fig. 7). Because of skin laxity, canthal tendon modification surgery should be approached with caution.
Fig. 4.

Characteristics of the Asian eyelid: Puffiness, no fold, deep set, epicanthus, canthal tilt: up-slanting, vertically narrow.
Fig. 5.

Removal of hypertrophied fat is almost routinely done during Asian blepharoplasty. Pretarsal fullness is also observed.
Fig. 6.

Lacrimal gland prolapse also exaggerates the lateral bulginess.
Fig. 7.

Floppy eyelid syndrome in a patient who has highly extensible eyelid skin.
Eyelid Crease Evaluation
A person with a double fold appears to have a bigger eye than a person without a double fold (Fig. 8). However, it is difficult to find someone born with a natural crease in the Asian population. For somebody who has multiple creases or a single shallow crease, the most common cause is due to the brow ptosis or skin laxity. Patients who used tapes and glues for making double fold for a long period also present with multiple wrinkles, thick and hard upper lid skin. These wrinkles are not a crease. After making a single deep crease line for those who have multiple shallow lines, the multiple creases will disappear and the brow position is relocated to the original position (Fig. 9).
Fig. 8.

Margin reflex distance 1 is the same, but eyes look bigger with a crease line.
Fig. 9.

(A) Multiple shallow creases are usually located above the natural crease line. (B) After making a single deep crease line, multiple lines disappear and the brow is moved to its original position.
When the crease is at the level of the upper margin of the tarsus, it makes an on-fold crease. A patient may want to have a high crease line, thinking that will resemble a Caucasian look; however, it results in an unnatural, ethnic-eradicating appearance. When the crease line meets the Mongolian fold, it is called an on-fold crease. When the crease goes over the Mongolian fold, it is an out-fold crease. When the crease goes below the Mongolian fold, it is an in-fold crease (Figs. 10 and 11). Though an on-fold crease line is suitable for most Asian patients, many patients want to have a high-fold (out-fold) crease. A high-fold crease should be done only in patients who have all of the following requirements: more than 30 mm of palpebral fissure length, exophthalmic, no epicanthal fold, good levator function, minimal amount of orbital fat, no pretarsal fullness, and thin skin.
Fig. 10.

Crease shape: The relationship between the epicanthal fold and the height of the crease.
Fig. 11.

Criteria for fold height.
Over time, the operated crease line can deteriorate and become a shallow crease as the holding suture weakens. Subsequent eyelash inversion and skin laxity can be observed again. Deepening of the fold line through levator-dermal or tarso-dermal suturing helps to evert the direction of eyelashes for a more vivid look (Fig. 12).
Fig. 12.

(A) Shallow crease: Weakening of crease line causes eyelash inversion and skin laxity, which gives a tired look. (B) Deep crease: Deepening of the crease line helps to evert eyelash direction to give a more vivid look.
Upper Cilia Direction
A significant number of Asians have a Mongolian fold and epiblepharon that hinders the everting motion of the cilia. The downturn of cilia causes trichiasis, which is more common among Asians than Caucasians. Making the double fold helps to evert the direction of cilia and can be a treatment option for some trichiasis patients. When ptosis surgery is done too much, it sometimes causes upturned cilia with exposure of palpebral conjunctiva. Therefore, evaluation of ciliary direction is essential before Asian blepharoplasty including ptosis surgery (Fig. 13).
Fig. 13.

Upturned cilia with exposure of palpebral conjunctiva after ptosis surgery.
Position of Upper Lid Margin (Ptosis)
The average margin reflex distance 1 (MRD1) of Caucasians is 4 to 4.5 mm, whereas the average MRD1 of Asians is 3 to 3.5 mm. Therefore, the average Asian patient has mild ptosis (Fig. 14). In unilateral ptosis cases, eye dominance can affect the result of blepharoplasty. When the dominant eye has ptosis, the nondominant eye has a tendency to hyperfunction, but when the nondominant eye has ptosis, hyperfunctioning of the dominant eye is less possible. Because hidden hyperfunction of the frontalis or levator muscle can affect the result of blepharoplasty, a thorough preoperative evaluation of eye dominance and muscle function is essential (Figs. 15 16 17 18).
Fig. 14.

Criteria for cosmetic surgery of the Asian eyelid.
Fig. 15.
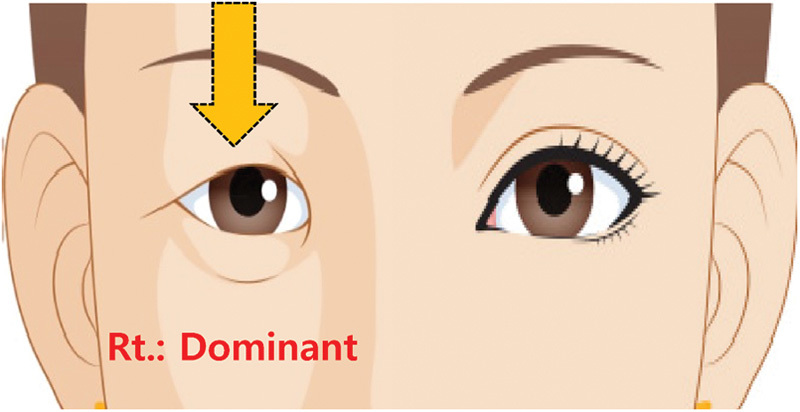
Right (Rt.) dominant eye and right ptosis. The patient feels discomfort because the dominant eye is affected. There is compensatory hyperfunction of the left levator (left eye looks normal) with the possibility of postoperative ptosis of the left eye due to Hering's law.
Fig. 16.
Left (Lt.) dominant eye and right ptosis. The patient feels less discomfort because the dominant eye is not affected. There is no compensatory hyperfunction of the right levator (the right eye looks ptotic) with less possibility of postoperative ptosis of the left eye.
Fig. 17.

Right (Rt.) dominant eye and left ptosis. The patient feels less discomfort because the dominant eye is not affected. There is no compensatory hyperfunction of the left levator (the left eye looks ptotic) with less possibility of postoperative ptosis of the right eye.
Fig. 18.

Left (Lt.) dominant eye and left ptosis. The patient feels discomfort because the dominant eye is affected. There is compensatory hyperfunction of the right levator (the right eye looks normal) with the possibility of postoperative ptosis of the right eye due to Hering's law.
When the MRD1 is more than 5.5 mm, the cause of the eyelid retraction must be evaluated. Fat deficiency due to involutional atrophy or fat removal surgery is currently one of the most common causes of lid retraction.
When the MRD1 is less than 3.5 mm, a determination must be made to see if it is real ptosis or pseudoptosis. If making a crease line with a wire creaser improves ptosis, it has a high possibility of being pseudoptosis (blepharochalasis). If the crease line is not formed well and still ptotic even when the creaser is applied firmly, then it can be considered real ptosis.
Miles Test
Keep both eyes open and aimed at a distant point through a hole made with the patient's hands.2 The observer aligns the hole with one of his eyes, or asks the patient to move the hands toward the eye while keep staring at an object (Fig. 19).
Fig. 19.

Miles test: Dominant eye.
Palpebral Shape
Slant of Palpebral Fissure - Upward, Downward, Horizontal
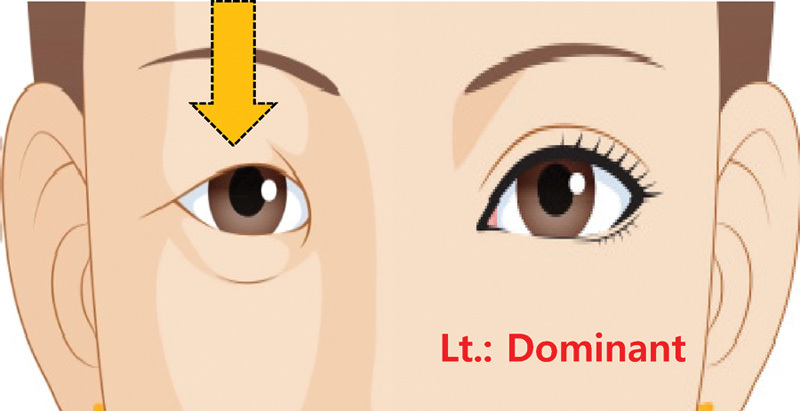
Usually Asians have larger degrees of upward palpebral fissure slanting than Caucasians (Fig. 20). Canthal tilt should be evaluated preoperatively, and lateral canthoplasty is recommended to lower the lateral canthal position in case of a positive canthal tilt.3 Slant reduction surgery that lessens the upward excursion of the lid at the outer corner is currently common among Asian populations. Slant reduction will expand the area of lateral sclera. The ideal ratio of medial and lateral sclera is 1:1.5 (Figs. 21 and 22). A patient who already has a horizontal or downward slant is not a good candidate for slant reduction surgery because overcorrection of the slant will cause a Treacher-Collins look (Fig. 23). Additionally, slight undercorrection should be done for someone who has negative vector (malar hypoplasia) or floppy eyelid syndrome. The slant reduction surgery can weaken the lateral canthal structures (tendon or raphe).
Fig. 20.

Degree of upward palpebral fissure slanting of the Asian eyelid.
Fig. 21.
Criteria to be used in the evaluation of Asian eyelids.
Fig. 22.

Slant reduction surgery (lateral canthal lengthening and vertical enlargement). (A) Preoperative. (B) Postoperative 2 weeks. (C) Postoperative 4 weeks.
Fig. 23.
Preoperative evaluation for vertical enlargement of the palpebral aperture.
Length of Palpebral Fissure
Palpebral length of the average Asian patient usually measures between 25 to 28 mm. Patients with less than 25 mm of length should consider epicanthoplasty together with a lateral canthal lengthening procedure (Figs. 24 and 25). Palpebral length more than 28 to 30 mm usually would look normal, although the aesthetic proportion is highly dependent on the width of the face.
Fig. 24.

Slant reduction surgery (lateral canthal lengthening and vertical enlargement).
Fig. 25.

Lateral canthal lengthening procedure.
Width of Palpebral Fissure
To accomplish an MRD1 of more than 4.5 mm, the width should be more than 10 mm without reverse ptosis. If the height is less than 10 mm, check if the patient has ptosis or reverse ptosis. A vertical enlargement procedure will correct a narrow palpebral aperture. When the upper margin of lower lid meets the corneoscleral junction, it is generally accepted as a normal shape.
Mongolian (Epicanthal) Fold
The medial canthal fold exhibits distinct anatomical variations according to the shapes of the folds, and is classified into four types.4 Type 3 is the most common form of fold in nonoperated Asian eyes and type 2 is the most desirable form for operated eyes. Type 1 looks Caucasian and usually is not suitable for Asian patients who desire to preserve an ethnic appearance (Fig. 26).
Fig. 26.

Classification of medial epicanthal fold. Source: Arch Aesthetic Plast Surg 2014 Feb;20(1):15-19. Available at: http://dx.doi.org/10.14730/aaps.2014.20.1.15
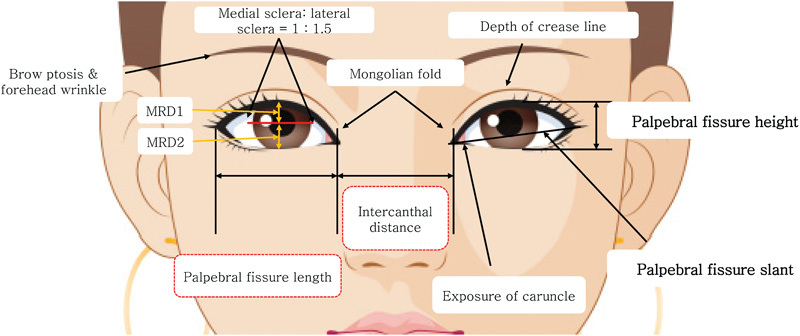
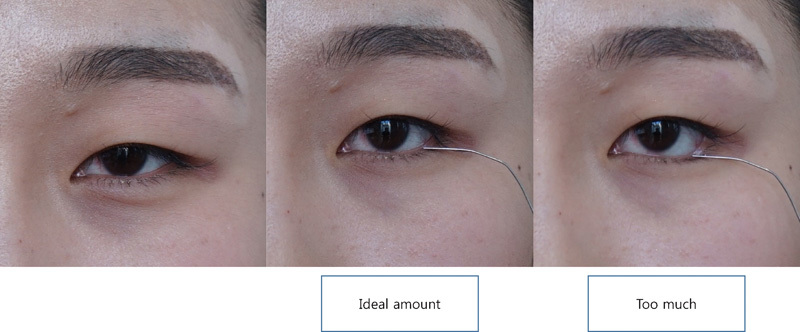
Measure the distance between the medial canthus with a ruler. Interepicanthal distance less than 32 mm is not good for epicanthoplasty. By slightly stretching the medial canthal skin, the medial caruncle will be exposed and reveal the anticipated postoperative look (Fig. 27). If the medial skin is pulled too medially, the caruncle will be too exposed and the scar will be quite obvious (Fig. 28). With the help of a skin tape, you can predict the result of epicanthoplasty and double fold procedure (Figs. 29 and 30).
Fig. 27.

Medial canthal stretching test: Stretching of the medial canthus to find the proper point to lengthen the fissure.
Fig. 28.

Evaluating the amount to be removed: Medial canthal stretching test.
Fig. 29.

Medial canthal stretching test with tapes.
Fig. 30.

Preoperative measurement of epicanthoplasty and double fold making.
Lateral Canthal Web
Apply an ocular speculum and measure the depth of the web (lateral canthus to the junction of bulbar and palpebral conjunctiva) with a caliper. Or palpate the medial margin of the lateral orbital rim and measure the length of the web with a caliper (Fig. 31). The depth (length of the web) is the amount to be lengthened. A canthal stretching test will give a clue as to whether lateral canthal lengthening surgery will yield good results (Figs. 32 and 33).
Fig. 31.

Measure the length of canthal web.
Fig. 32.

Lateral canthal stretching test.
Fig. 33.

(A) Lateral canthal stretching test: Tight canthus patient with tight canthal web displays limited exposure of conjunctiva. (B) Lateral canthal stretching test: Loose canthus patient with loose canthal web displays exposure of bulbar and palpebral conjunctiva.
Lower Lid
Position of Lower Lid Margin (Reverse Ptosis)
When the margin of the lower lid meets the corneoscleral junction in primary gaze, this is a normal look. The normal range of MRD2 is between 4.5 to 5.5 mm. If the lower lid covers too much of the limbus, the result will be a slit-eye appearance (Fig. 34). More than 5.5 mm of MRD2 will show too much sclera and be regarded as a diseased look (e.g., proptotic, Grave's disease).
Fig. 34.

Slant reduction surgery for reverse ptosis: Vertical enlargement procedure. (A) Preoperative. (B) Postoperative 2 weeks.
Lower Lid Tone, Skin Laxity Evaluation
A small, tight, narrow eye shape has less of a tendency toward lower lid laxity. However, iatrogenic injury of the lateral canthal tendon, which is inevitable in lateral canthal lengthening procedures currently common in Asians, needs to be considered before a lower blepharoplasty is performed. Canthal lengthening procedures should be limited to younger patients who have overtilted and real narrow eyes. The snap back test and the distraction test are most commonly used to evaluate lower lid tone (Fig. 35).
Fig. 35.

Evaluating lower lid tone. (A) Snap back test. (B) Distraction test.
Pretarsal Fullness (Love Band)
Pretarsal fullness (love band) gives a happy look. When we smile, our facial elevator muscles contract and pull up the cheek fat pad, which increases the gathering of pretarsal and preseptal orbicularis oculi muscle and makes pretarsal fullness. Filler injection or fat graft can augment the pretarsal volume (Fig. 36). A person with a pretarsal fullness appears to have a bigger and happier eye than a person without a pretarsal fullness.
Fig. 36.

Pretarsal augmentation (love band). (A) Preoperative: Looks normal and natural. (B) Postoperative: Slightly overexaggerated, but the patient is satisfied with the results. Beauty is in the eyes of the beholder.
Tear Trough Deformity
The tear trough ligament is between the palpebral and orbital part of the orbicularis oculi muscle.5 The tear trough ligament continues laterally as the bilayered orbicularis retaining ligament.6 Compared to the orbicularis retaining ligament, the tear trough ligament is thicker and densely adherent to the bony orbital rim (Figs. 37 and 38). Without removing the connection between dermis and the tear trough ligament, the tear trough deformity cannot be corrected effectively.
Fig. 37.

Tear trough ligament: Orbicularis retaining ligament complex. OOM, orbicularis oculi muscle; ORL, orbicularis retaining ligament.
Fig. 38.

Part of the periosteum where tear trough ligament arises is more densely adherent to the orbital rim than that of the orbicularis retaining ligament.
Lower Lid Fat Bulging
One of the most common causes of lower lid fat bulging is malar hypoplasia. Compared to Caucasians, Asians generally have bigger cheek bones, which are better supporting structures for the lower lid. Pretarsal fullness and fat bulging often make a double bubble shape. Release of the tear trough ligament and orbital retaining ligament with pedicled fat flap transposition will recover the lid-cheek contour while maintaining the love band (Fig. 39).
Fig. 39.
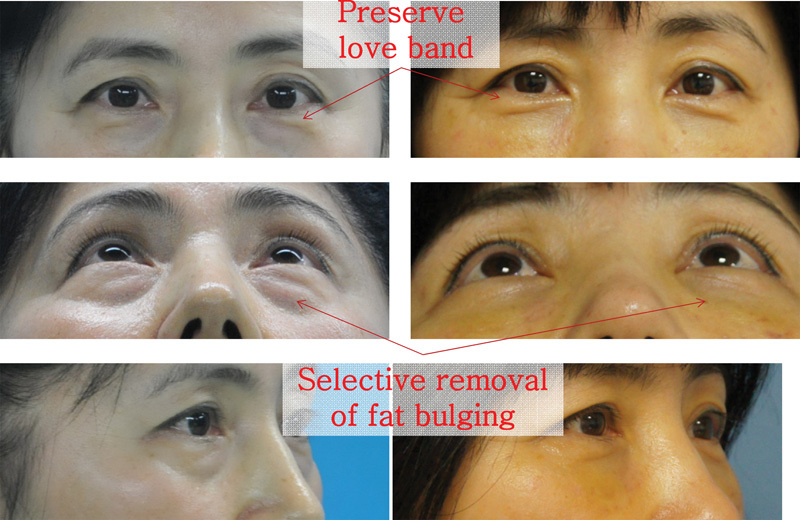
Selective removal of fat bulging while maintaining love band.
Conclusion
To overcome several anatomical obstacles that are sometimes more prevalent in Asian eyelids or more often hidden, the plastic surgeon needs to know how to elicit as much information as possible from a patient prior to surgery about his or her condition through the examination. Additionally, we should learn to predict the results of each patient from the gathered information to optimize our surgical results.
References
- 1.Lee E I, Kim N H, Park R H, Park J B, Ahn T J. The relationship between eyebrow elevation and height of the palpebral fissure: should postoperative brow descent be taken into consideration when determining the amount of blepharoptosis correction? Arch Aesthetic Plast Surg. 2014;20(1):20–25. [Google Scholar]
- 2.Miles W R. Ocular dominance demonstrated by unconscious sighting. J Exp Psychol. 1929;12(2):113–126. [Google Scholar]
- 3.Glat P M Jelks G W Jelks E B Wood M Gadangi P Longaker M T Evolution of the lateral canthoplasty: techniques and indications Plast Reconstr Surg 199710061396–1405., discussion 1406–1408 [DOI] [PubMed] [Google Scholar]
- 4.Park J I. Z-epicanthoplasty in Asian eyelids. Plast Reconstr Surg. 1996;98(4):602–609. doi: 10.1097/00006534-199609001-00002. [DOI] [PubMed] [Google Scholar]
- 5.Wong C H, Hsieh M K, Mendelson B. The tear trough ligament: anatomical basis for the tear trough deformity. Plast Reconstr Surg. 2012;129(6):1392–1402. doi: 10.1097/PRS.0b013e31824ecd77. [DOI] [PubMed] [Google Scholar]
- 6.Mendelson B C Muzaffar A R Adams W P Jr Surgical anatomy of the midcheek and malar mounds Plast Reconstr Surg 20021103885–896., discussion 897–911 [DOI] [PubMed] [Google Scholar]


