Abstract
Background
The goal of this study was to assess systems and processes involved in the operating room (OR) to intensive care unit (ICU) handoff in an attempt to understand the criticality of specific steps of the handoff.
Methods
We performed a failure modes, effects and criticality analysis (FMECA) of the OR to ICU handoff of deceased donor liver transplant recipients using in-person observations and descriptions of the handoff process from a multidisciplinary group of clinicians. For each step in the process, failures were identified along with frequency of occurrence, causes, potential effects and safeguards. A risk priority number (RPN) was calculated for each failure (Frequency x Potential effect x Safeguard; range 1-least risk to 1000-most risk).
Results
The FMECA identified 37 individual steps in the OR to ICU handoff process. In total, 81 process failures were identified, 22 of which were determined to be critical and 36 of which relied on weak safeguards such as informal human verification. Process failures with the highest risk of harm were lack of preliminary OR to ICU communication (RPN 504), team member absence during handoff communication (RPN 480) and transport equipment malfunction (RPN 448).
Conclusions
Based on the analysis, recommendations were made to reduce potential for patient harm during OR to ICU handoffs. These included automated transfer of OR data to ICU clinicians, enhanced ICU team member notification processes and revision of the postoperative order sets. The FMECA revealed steps in the OR to ICU handoff that are high risk for patient harm and are currently being targeted for process improvement.
Keywords: Critical care, patient handoff, transplantation, risk assessment, quality improvement
Introduction
Early postoperative complications following liver transplant can have devastating consequences.1–3 The sequelae of many of these complications, such as hepatic artery thrombosis and hemorrhage, are best mitigated by prompt detection and initiation of appropriate interventions. This requires communication and coordination of care and between surgical and critical care teams—the foundation of which is established during the operating room (OR) to intensive care unit (ICU) handoff. The purpose of the OR to ICU handoff is to engage in both a physical transfer of the patient and a knowledge of the patient’s clinical information from the OR surgical team to the accepting critical care team.
Effective handoffs include not only operative details but also anticipatory guidance that allows the critical care team to continue providing immediate post-operative care and to anticipate, detect, and facilitate timely management of postoperative complications. However, the OR to ICU handoff can be challenging, as it requires coordination of the physical transfer of the patient and of the knowledge transfer between multiple clinicians from anesthesia, surgery and critical care, typically performing in a busy clinical environment.4 The handoff involves multiple steps (e.g., physical preparation of patient to leave the OR, transport to ICU), many systems (e.g., OR, ICU, laboratory, pharmacy, blood bank), and processes (e.g., transfer of electronic health record, assembling the clinical teams for the handoff).5 While several studies have demonstrated the effect of the quality of a handoff on process metrics (e.g., information transfer, handoff duration, checklist compliance), little evidence exists to demonstrate the effect of the quality of a handoff on clinical outcomes.6
Failure modes, effects and criticality analysis (FMECA) is a risk assessment team methodology, developed in 1949 by the Department of Defense, and widely used in high-risk industries such as air carrier and nuclear energy.7–9 Over the past decade, the FMECA methodology has been increasingly used in healthcare to examine high-risk care processes such as medication administration, surgical procedures, and emergency care.10–12 This paper reports the results of an FMECA of the systems and processes involved in the OR to ICU handoff in an attempt to further understand the criticality of specific steps of the handoff. The identification of these steps should assist in better understanding the potential relationships between the handoff process and clinical outcomes.
Methods
Setting and Topic
We performed an FMECA of the OR to ICU patient handoff process for deceased donor liver transplant recipients at a tertiary academic hospital. Deceased donor liver transplant recipients were chosen as a model of the critically ill surgical patient population due to their complexity, dedicated surgical, anesthesia, and OR teams, and nearly universal postoperative transfer to the ICU. Institutional Review Board approval was received prior to data collection.
Ethnographic Observations
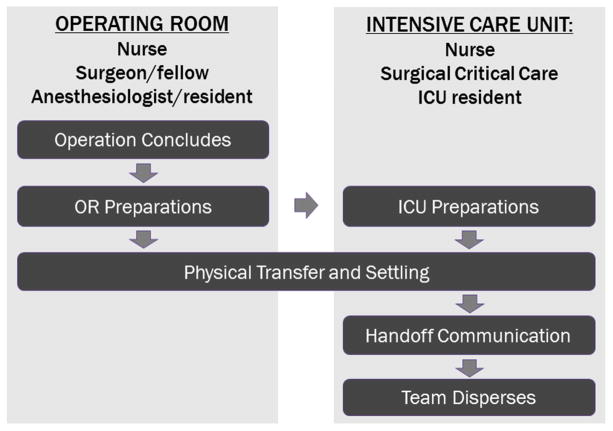
Prior to beginning the FMECA, two members of the research team (LM, RK) conducted ethnographic observations of five OR to ICU handoffs to initially identify key steps and all relevant clinical personnel (e.g., transplant surgeon, scrub nurse, anesthesiology fellow) involved in the handoff. As a result, a schema of the OR to ICU handoff process was created (Figure 1). Any safeguards against process failure or patient harm observed by the researchers were also noted.
Figure 1. The OR to ICU Handoff Process In-brief.
Figure 1 shows the basic steps in an operating room to intensive care unit handoff
FMECA Process
The FMECA was performed by engaging all relevant clinicians with knowledge and experience in the process of interest, identified by the ethnographic observations. The overall FMECA process is shown in Figure 2.
Figure 2. FMECA Process In-brief.

Figure 2 shows a shema of the failure modes effects and criticality analysis process
All sessions were audio-recorded and then transcribed verbatim by a professional transcription service specializing in medical transcription. Clinicians began by describing, in their own words, the steps in the systems and processes of care involved in the handoff, their specific role and specific tasks performed. This description was graphically depicted as a process map. Clinicians were asked to provide further clarification until consensus was reached. Individual interviews were arranged to fill in any gaps in process, as necessary. Following each session, the process map was updated.
After confirming the accuracy of the process map, clinicians were asked to examine each step in the process and to identify any weaknesses that could lead to a failure (failure mode). Then, clinicians were asked, for each failure, to assign a frequency of occurrence, the impact of the failure on a patient (effect), and any safeguards in place to mitigate the failure. A ten-point scale was used to assign frequency, impact, and safeguard. For each scale, a low score of 1 indicates minimal risk to the process or the patient (e.g., minor delay) and a high score of 10 indicating maximum risk of patient harm (e.g., death, permanent disability) (Figure 3).
Figure 3. FMECA 10-point scoring scales.
Figure 3 shows the 10-point failure modes effects and criticality analysis scoring system customized for the operating room to Intensive care unit handoff
Finally, in order to prioritize the failures, a Risk Priority Number was (RPN) was calculated as the “criticality” for each failure. The RPN is product of the frequency by the impact. RPNs can range from 1 (lowest risk) to 1,000 (highest risk) and are ordinal. An RPN of 300 is considered as a threshold above which a failure would be designated as “critical.”13,14 In addition, the complete list of process failures was reviewed by a clinician panel to prevent omission of a clinically critical process failure due to low RPN.
Results
The FMECA involved sixteen (16) individual and small group sessions with transplant and critical care surgeons, anesthesiologists, OR and ICU nurses, and trainees. Failures identified during the FMECA were verified with the ethnographic observation notes.
The ethnographic observations revealed that the OR to ICU handoff process has multiple simultaneous workflows performed by as many as 12 clinicians who interact during the OR to ICU handoff. Thirty-seven (37) major steps were identified in the OR to ICU handoff process (SDC 1). Most steps were vulnerable to multiple failures. Sixteen failures were not scored as they were based solely on performance of individual practitioners unrelated to handoff activities (e.g., incorrect fascia closure, incorrect instrument counts, incomplete skin closure, patient incorrectly gowned, ventilator attached incorrectly). Of the 37 steps, 22 had a failure with an RPN > 300 that was considered to be critical (Table 1).
Table 1.
Critical Failures
| Process step | Critical Process Failures | RPN |
|---|---|---|
| Preliminary call to ICU | No call placed | 504 |
| Incorrect callee | 504 | |
| Inadequate information exchange | 441 | |
|
| ||
| Verify ICU room prepared | No verification | 441 |
|
| ||
| Inadequate verification | 441 | |
|
| ||
| Notify of need for ventilator | No notification | 448 |
|
| ||
| Vent into ICU room | No placement into room | 448 |
|
| ||
| ICU bed assessment | Incorrect assessment | 448 |
| No assessment | 448 | |
| Incomplete/inadequate assessment | 448 | |
|
| ||
| Final departure call to ICU | No call placed | 360 |
| Incorrect callee | 360 | |
|
| ||
| Service fellow at ICU bedside | No arrival | 432 |
|
| ||
| ICU resident at ICU bedside | No arrival | 480 |
| Late arrival | 480 | |
|
| ||
| Transplant surgery handoff | Incorrect information/plan given | 343 |
|
| ||
| Surgical drain documentation | No documentation | 378 |
| Incomplete documentation | 336 | |
| Incorrect documentation | 336 | |
|
| ||
| Postoperative labs drawn | No labs drawn | 360 |
| Incorrect labs drawn | 320 | |
| Incomplete labs drawn | 360 | |
|
| ||
| Postoperative orders activated | Orders not activated | 360 |
| Orders incompletely activated | 432 | |
Process Steps in the Operating Room Prior to Physical Transfer
Five steps occurring in the OR prior to physical transfer of the patient were identified as having critical failures including: failure of the OR team to make a preliminary call to the ICU, failure to verify the ICU room readiness for patient arrival, failure to notify ICU team members of the need for a ventilator, failure to transport the ventilator to the ICU room prior to patient arrival, and failure to assess the bed and equipment used for transfer from the OR to ICU.
ICU team members conveyed the importance of advance notification of the impending patient arrival from the OR with an emphasis on the need for early communication regarding the patient’s clinical stability. They also indicated that the advance notice allows the team to assemble, recruit assistance for handoff tasks, and prepare necessary equipment and supplies. Conversely, they articulated how not receiving advance can result in the ICU staff being underprepared for the patient’s care needs and/or not having the proper equipment available (e.g., rapid infuser, ventilator) to immediately provide optimal care of the patient. OR team members attributed these failures to the lack of a designated person responsible for contacting the ICU and for verifying the availability and functionality of transport equipment. All participants recalled occasions where this lack of preparation resulted in patients remaining on a transport ventilator longer than necessary, or delayed the administration of blood and/or medications.
FMECA participants provided preliminary recommendations to mitigate the failures. The main recommendations, prior to physical transfer were:
Create automatic notifications of the handoff for delivery to all relevant team members 1 hour, 30 minutes, and just before leaving the OR;
Designate an OR team member who contacts a similarly designated ICU team member to provide a pre-handoff communication
Create a multidisciplinary workgroup to agree upon essential pre-handoff communication elements, including clinical status of the patient, ICU equipment needs assessment and confirmation of clinician/staff and equipment availability; and
Designate an OR team member responsible for verifying the availability and functionality of transport equipment.
Process Steps in the Intensive Care Unit
Six steps in the ICU were identified as having critical failures including: failure of certain team members (transplant fellow, ICU resident) to be present at the bedside for the transfer of clinical information, failure to accurately record early postoperative surgical drain output, and untimely or inaccurate postoperative orders and/or laboratory orders. Participants offered some preliminary recommendations to mitigate the failures including: increased communication about potential patient risks and complications during the handoff as opposed to communication focused on details of the operative procedure and presentation of data (for example: estimated blood loss, fluid administration), that could be found elsewhere documented in the electronic health record. Several participants recalled specific occasions where absence of a team member during handoff and errors in the postoperative order sets led to delay in diagnosis of postoperative hemorrhage. Participants also articulated that inconsistencies in the handoff process can result from interpersonal dynamics. In particular, they mentioned variation in behavior of surgical team members and how the presence of even one “difficult” team member can discourage communication and compromise patient safety. More specific recommendations include:
Create an automated notification of the handoff for delivery to ICU team members 1 hour, 30 minutes, and at the departure of the patient from the OR;
Designate an ICU team member receive the preliminary call from a similarly designated OR team member with a preliminary report of the patient’s clinical status and to confirm need for a ventilator and need to notify respiratory therapy;
Create an OR summary data sheet for ICU team (print or digital);
Develop handoff communication guidelines; train team members on use of the guidelines; with retraining for team members
Revise postoperative order sets with input from ICU team members; and
Require independent, double entry of critical postoperative data and manual entry of laboratory results during initial 24 post-operative hours.
Discussion
Early postoperative complications are common after liver transplantation, and can have significant consequences. The best way to prevent the majority of postoperative complications is in the operating room with excellent technical and clinical skill. A complimentary step is to ensure there is a complete and effective hand-off between teams. An effective OR to ICU handoff can potentially enhance prompt detection and mitigation of postoperative complications. This study strongly suggests that an effective OR to ICU handoff begins with advance notification of the ICU team by the OR team, includes clearly defined roles and responsibilities for participating team members, leverages information technology, allows for adequate preparatory time for the receiving team, and includes anticipatory guidance, based on clinical judgment beyond information contained in the medical record. A key goal of the handoff should be a shared “mental model” of the patient’s status and potential risks and complications.15
The OR to ICU handoff, like many complex healthcare processes, is vulnerable to failures. It involves both the physical transfer of the patient and a knowledge and information transfer about the patient’s medical status between teams. The physical transfer of the patient depends on technology and equipment by requiring a transfer between stationary and portable life sustaining equipment and switching of tubing and wires for monitoring prior to leaving the OR and again upon arrival in the ICU. The knowledge and information transfer involves specific information for each discipline (e.g., nursing, ICU, surgeon) who have varying levels of authority and experience. Handoffs typically occur in an ICU setting that includes substantial ambient noise, multitasking by clinicians during the handoff, and distractions of clinicians by care needs of other ICU patients.16 This complicated environment results in steps in the handoff process that are at substantial risk for failures that results in compromised patient safety.
The application of FMECA to the OR to ICU handoff process has, however, identified specific steps that are likely to have “critical” failures that substantially impact patients. Pre-transfer ICU notification, designation of handoff team roles and responsibilities, and early postoperative documentation and monitoring are critical elements that may decrease the risk of patient harm by allowing for prompt detection and mitigation of early postoperative complications. These findings echo prior work that has shown how differences in communication style, hierarchical constraints, and a lack of structure contribute to handoff process failures.17 Chang and colleagues reported that although handoff participants thought their report contained “the most important piece of information,” information receivers disagreed 60% of the time. A recent study reported that anesthesiologists failed to transfer all of the essential information in 67% of OR to post-anesthesia care unit handoffs, with a focus on operative details over anticipatory guidance.18
Interventions designed to improve OR to ICU handoffs have seen measurable progress. The majority of studies to date have focused on the pediatric cardiac population and demonstrated an ability to improve process metrics such as information transfer, duration of handoff process, and clinician teamwork.19–21 In addition, Kauffman demonstrated decreased rates of unplanned extubations and decreased mean ventilator time following implementation of a post-handoff protocol, developed by a multidisciplinary team, further supporting the notion that the quality of a handoff quality affects clinical outcomes.22 Although this study provides general recommendations for improving the OR to ICU handoff, the specific logistics for executing an OR to ICU handoff will likely vary somewhat by institution and surgical specialty, clinical discipline, experience, and authority level of participants. Interventions to improve the OR to ICU handoff may be most effective when designed following inter-professional education and consensus building at the specialty, discipline, and institution level. This allows participants to develop a customized protocol that incorporates existing roles and responsibilities, utilizes existing team members, adapts the handoff to the unique sequence of events of the physical settling, and exploits the existing information system. Checklists and other documentation tools are also more likely to be adopted by team members who, collectively, have reconciled differing opinions about handoff process goals and recognized and addressed institution-specific challenges.
Limitations of this study include those inherent to FMECA methodology such as its inherent dependence on the subjective experiences of the individual, clinician participants, in which a failure mode or effect may be missed or exaggerated. The scales used for FMECA scoring are ordinal which has led to criticism of using the numerical product of those scales to calculate the RPN as the primary means of prioritization.23 Finally, this study was conducted at a single institution and there are undoubtedly varying experiences in different institutions.
In conclusion, the OR to ICU handoff includes many steps and a substantial number of the steps include weaknesses that can lead to failures that result in potentially significant outcomes for patients. Clinicians can readily provide preliminary recommendations to mitigate or eliminate these failures. However, engaging frontline clinicians who are involved in the OR to ICU handoff to customize the process, designate roles and responsibilities, and adapt to the institution’s specific environment will likely lead to better acceptance, adoption, and sustainability. Improvements in OR to ICU handoff processes have the potential to mitigate postoperative complications by heightening team awareness, therefore enhancing ability to promptly detect and intervene. Further studies aim to test the recommendations for improvement, evaluate the feasibility of implementation, and finally to quantify the impact of the quality of handoffs on patient outcomes.
Supplementary Material
SDC 1 shows the completed process map for the operating room to Intensive care unit handoff
Acknowledgments
This work is funded by AHRQ and NIDDK T32 Training Grants (McElroy 5T32HS78-15, T32DK77662-7). The authors would like to thank Adela Mizrachi her opinions and suggestions for this work.
Footnotes
“Presented at the 10th Annual Academic Surgical Congress; Las Vegas, NV, February 3–5, 2015”
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Patel G, Huprikar S. Infectious complications after orthotopic liver transplantation. Semin Respir Crit Care Med. 2012;33(1):111–124. doi: 10.1055/s-0032-1301739. [DOI] [PubMed] [Google Scholar]
- 2.Perez-Saborido B, Pacheco-Sanchez D, Barrera-Rebollo A, et al. Incidence, management, and results of vascular complications after liver transplantation. Transplant Proc. 2011;43(3):749–750. doi: 10.1016/j.transproceed.2011.01.104. [DOI] [PubMed] [Google Scholar]
- 3.Khalaf H. Vascular complications after deceased and living donor liver transplantation: a single-center experience. Transplant Proc. 2010;42(3):865–870. doi: 10.1016/j.transproceed.2010.02.037. [DOI] [PubMed] [Google Scholar]
- 4.Nagpal K, Arora S, Abboudi M, et al. Postoperative handover: problems, pitfalls, and prevention of error. Ann Surg. 2010;252(1):171–176. doi: 10.1097/SLA.0b013e3181dc3656. [DOI] [PubMed] [Google Scholar]
- 5.Segall N, Bonifacio AS, Schroeder RA, et al. Can we make postoperative patient handovers safer? A systematic review of the literature. Anesth Analg. 2012;115(1):102–115. doi: 10.1213/ANE.0b013e318253af4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perry SJ, Wears RL, Patterson ES. High-Hanging Fruit: Improving Transitions in Health Care. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 3: Performance and Tools) Rockville (MD): 2008. [Google Scholar]
- 7.Procedures for Performing a Failure Mode, Effects and Criticality Analysis. 1949 MIL-P-1629. [Google Scholar]
- 8.Procedure for Failure Mode, Effects and Criticality Analysis (FMECA) 1966 RA–006–013–1A. [Google Scholar]
- 9.Design Analysis Procedure For Failure Modes, Effects and Criticality Analysis (FMECA. 1967:ARP926. [Google Scholar]
- 10.Aita M, Belvedere O, De Carlo E, et al. Chemotherapy prescribing errors: an observational study on the role of information technology and computerized physician order entry systems. BMC Health Serv Res. 2013;13:522. doi: 10.1186/1472-6963-13-522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khare RK, Nannicelli AP, Powell ES, Seivert NP, Adams JG, Holl JL. Use of risk assessment analysis by failure mode, effects, and criticality to reduce door-to-balloon time. Ann Emerg Med. 2013;62(4):388–398. e312. doi: 10.1016/j.annemergmed.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 12.Hover AR, Sistrunk WW, Cavagnol RM, et al. Effectiveness and Cost of Failure Mode and Effects Analysis Methodology to Reduce Neurosurgical Site Infections. Am J Med Qual. 2013 doi: 10.1177/1062860613505680. [DOI] [PubMed] [Google Scholar]
- 13.Davie JL. An analysis of risk perception and the RPN index within Failure Modes and Effects Analysis. ProQuest. 2008 [Google Scholar]
- 14.An introduction to FMEA. Using failure mode and effects analysis to meet JCAHO’s proactive risk assessment requirement. Failure Modes and Effect Analysis. Health devices. 2002;31(6):223–226. [PubMed] [Google Scholar]
- 15.Mayer CM, Cluff L, Lin WT, et al. Evaluating efforts to optimize TeamSTEPPS implementation in surgical and pediatric intensive care units. Joint Commission journal on quality and patient safety / Joint Commission Resources. 2011;37(8):365–374. doi: 10.1016/s1553-7250(11)37047-x. [DOI] [PubMed] [Google Scholar]
- 16.Bonifacio AS, Segall N, Barbeito A, Taekman J, Schroeder R, Mark JB. Handovers from the OR to the ICU. Int Anesthesiol Clin. 2013;51(1):43–61. doi: 10.1097/AIA.0b013e31826f2b0e. [DOI] [PubMed] [Google Scholar]
- 17.Chang VY, Arora VM, Lev-Ari S, D’Arcy M, Keysar B. Interns overestimate the effectiveness of their hand-off communication. Pediatrics. 2010;125(3):491–496. doi: 10.1542/peds.2009-0351. [DOI] [PubMed] [Google Scholar]
- 18.Anwari JS. Quality of handover to the postanaesthesia care unit nurse. Anaesthesia. 2002;57(5):488–493. doi: 10.1046/j.0003-2409.2001.02406.x. [DOI] [PubMed] [Google Scholar]
- 19.Catchpole KR, de Leval MR, McEwan A, et al. Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. Paediatr Anaesth. 2007;17(5):470–478. doi: 10.1111/j.1460-9592.2006.02239.x. [DOI] [PubMed] [Google Scholar]
- 20.Zavalkoff SR, Razack SI, Lavoie J, Dancea AB. Handover after pediatric heart surgery: a simple tool improves information exchange. Pediatr Crit Care Med. 2011;12(3):309–313. doi: 10.1097/PCC.0b013e3181fe27b6. [DOI] [PubMed] [Google Scholar]
- 21.Joy BF, Elliott E, Hardy C, Sullivan C, Backer CL, Kane JM. Standardized multidisciplinary protocol improves handover of cardiac surgery patients to the intensive care unit. Pediatr Crit Care Med. 2011;12(3):304–308. doi: 10.1097/PCC.0b013e3181fe25a1. [DOI] [PubMed] [Google Scholar]
- 22.Kaufmnan J, Twite M, Barrett C, et al. A handoff protocol from the cardiovascular operating room to cardiac ICU is associated with improvements in care beyond the immediate postoperative period. Joint Commission journal on quality and patient safety / Joint Commission Resources. 2013;39(7):306–311. doi: 10.1016/s1553-7250(13)39043-6. [DOI] [PubMed] [Google Scholar]
- 23.Shebl NA, Franklin BD, Barber N. Failure mode and effects analysis outputs: are they valid? BMC Health Serv Res. 2012;12:150. doi: 10.1186/1472-6963-12-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SDC 1 shows the completed process map for the operating room to Intensive care unit handoff