Abstract
Purpose
Electrographic seizures (ES) and electrographic status epilepticus (ESE) are common in children in the pediatric intensive care unit (PICU) with acute neurologic conditions, and ESE is associated with worse functional and quality of life outcomes. As an exploratory study, we aimed to determine if ESE was associated with worse outcomes using more detailed neurobehavioral measures.
Methods
Three hundred children with an acute neurologic condition and altered mental status underwent clinically indicated EEG monitoring and were enrolled in a prospective observational study. We obtained follow-up data from subjects who were neurodevelopmentally normal prior to PICU admission. We evaluated for associations between ESE and adaptive behavior (Adaptive Behavior Assessment System-II, ABAS-II), behavioral and emotional problems (Child Behavior Checklist, CBCL), and executive function (Behavior Rating Inventory of Executive Function, BRIEF) using linear regression analyses. A p-value of <0.05 was considered significant.
Results
137 of 300 subjects were neurodevelopmentally normal prior to PICU admission. We obtained follow-up data from 36 subjects for CBCL, 32 subjects for ABAS, and 20 subjects for BRIEF. The median duration from admission to follow-up was 2.6 years (IQR 1.2–3.8). There were no differences in the acute care variables (age, sex, mental status category, intubation status, paralysis status, acute neurologic diagnosis category, seizure category, EEG background category, or short-term outcome) between subjects with and without follow-up data for any of the outcome measures. On univariate analysis, significant differences were not identified for CBCL total problem (ES coefficient −4.1, p=0.48; ESE coefficient 8.9, p=0.13) or BRIEF global executive function scores (ES coefficient 2.1, p=0.78; ESE coefficient 14.1, p=0.06), although there were trends towards worse scores in subjects with ESE. On univariate analysis, ES was not associated with worse scores (coefficient −21.5, p=0.051) while ESE (coefficient −29.7, p=0.013) was associated with worse ABAS adaptive behavioral global composite scores. On multivariate analysis, when compared to subjects with no seizures, both ES (coefficient −28, p=0.014) and ESE (coefficient −36, p=0.003) were associated with worse adaptive behavioral global composite scores.
Discussion
Among previously normal children with acute neurologic disorders, ES and ESE were associated worse adaptive behavior and trends toward worse behavioral-emotional and executive problems. This was a small exploratory study, and the impact of ES and ESE on these neurobehavioral measures may be clarified by subsequent larger studies.
Keywords: EEG Monitoring, Seizure, Status Epilepticus, Pediatric, Outcome, Non-Convulsive Seizure
Introduction
Electrographic seizures (ES) and electrographic status epilepticus (ESE) have been reported in 10–40% of children in pediatric intensive care units (PICU) who underwent clinically indicated continuous EEG monitoring (cEEG).[1–14] Although cEEG is resource-intense,[15] cEEG data often impact clinical management[16] and the costs to identify a child experiencing electrographic seizures are modest.[17] In the context of these data, physicians report rapidly increasing cEEG use in PICUs[18,19] and recent guidelines advocate for cEEG in many critically ill children with acute encephalopathy.[20–22]
In addition to serving as biomarkers of brain injury and dysfunction, ES and ESE may also contribute to secondary brain injury, and they are associated with worse short-term outcome.[1,9,10,12,23–27] Based on a prospective observational study of critically ill children who underwent cEEG, we previously reported that compared to subjects without seizures, subjects with ESE had worse long-term functional outcome scores, lower quality of life, and were more likely to develop epilepsy even after adjusting for variables related to acute encephalopathy etiology and severity.[27] In the current exploratory study, we aimed to describe the relationship between ES or ESE and more detailed neurobehavioral long-term outcome measures including adaptive behavior, problem behaviors, and executive function.
Methods
Standard Protocol Approvals, Registrations and Patient Consents
Parents/guardians provided informed written consent for enrollment in the initial observational database and subsequently provided informed verbal consent for enrollment in the follow-up study. Both studies were approved by the Children’s Hospital of Philadelphia’s Institutional Review Board.
Prospective Observational Database
We have previously described our prospective observational database.[14,25,27] Infants and children treated in the PICU of our quaternary care hospital between July 2008 and September 2011 who underwent cEEG were enrolled in a prospective observational study. Neonates (age <1 month) were excluded. Clinical practice at our institution was to perform cEEG in patients with acute encephalopathy to identify ES and/or to determine whether abnormal movements or vital sign fluctuations of unknown etiology were seizures. We used a Grass-Telefactor (West Warwick, RI) video-EEG system with 21 gold-over-silver scalp surface electrodes positioned according to the international 10–20 system. EEGs were interpreted by the EEG service and patients were managed by pediatric intensivists and the neurology consult service. cEEG duration was at least 24 hours when screening for ES or ESE. Prophylactic anticonvulsants were not routinely administered. Although no formal institutional management pathway was in place, our clinical services aimed to terminate ES and ESE when identified, most commonly using phenobarbital, phenytoin-fosphenytoin, and levetiracetam.[28]
Prospectively collected clinical data included age, sex, acute neurologic disorders, prior neurodevelopmental status, medications, intubation status, cEEG indication, hospital and PICU admission and discharge dates, and short-term outcome. Acute neurologic disorders were categorized as: (1) epilepsy-related, (2) acute structural (stroke, central nervous system inflammation or autoimmune disorder, traumatic brain injury, central nervous system infection, brain malformation, tumor/oncologic, and hypoxic-ischemic encephalopathy), and (3) acute non-structural (sepsis, metabolic, pharmacologic sedation, toxin, paralytic administration). Short-term functional outcome was assessed by assigning a Pediatric Cerebral Performance Category (PCPC) score.[29]
As part of this study, after clinical use the cEEG tracings were reinterpreted by one pediatric encephalographer (N.S.A.) to define EEG background categories and seizure categories, as reported by previous studies.[1,25,27] EEG background categories were: (1) normal or sedated sleep, (2) slow and disorganized, (3) discontinuous or burst-suppression, and (4) attenuated and featureless. Seizure categories were: (1) none, (2) ES, or (3) ESE. An ES was defined as an abnormal paroxysmal event that was different from the background, lasting longer than ten seconds (or shorter if associated with a clinical change) with a temporal-spatial evolution in morphology, frequency, and amplitude, and with a plausible electrographic field. ESE was defined as either a single thirty minute ES or a series of recurrent independent ES totaling more than thirty minutes in any one hour period (50% seizure burden). Patients were scored as ESE if ESE occurred at any point during the recording.
Long-Term Outcome Study
Three hundred subjects were enrolled in the prospective cEEG observational study. We attempted to contact the parents/guardians of all subjects who survived to PICU discharge. This study only included subjects who were reported to be neurodevelopmentally normal prior to PICU admission by parents and any available prior medical records. This avoided having to retrospectively establish baseline scores with analyses evaluating for any interval change. We performed at least five contact attempts to all phone numbers included in the institutional medical record, including weekend and evening calls. A trained caller performed structured phone interviews which included the Glasgow Outcome Scale (Extended Pediatric Version), the Pediatric Quality of Life Inventory, and an epilepsy questionnaire. These data were reported previously.[27] Subjects were then mailed additional neurobehavioral outcome measures to complete and return. If we did not receive the mailed measures back in three weeks, then we performed at least three additional phone contact attempts to remind parents/guardians, and we mailed additional copies of the outcome measures when requested by parents/guardians.
Three outcome measures were assessed. All used the age-appropriate parent/guardian report versions of the forms. As this was an exploratory study with a small number of subjects, we determined a priori that our main analyses would only involve the global scores for each outcome measure and not the various subscales.
The Adaptive Behavior Assessment System-II (ABAS-II) is a comprehensive norm-referenced measure of adaptive and daily living skills.[30] The ABAS-II assesses adaptive functioning using three domains: conceptual (communication and academic skills), social (interpersonal and social competence skills), and practical (independent living and daily living skills). Together, these provide a General Adaptive Composite Score. For each item, the respondent chooses either 0 (not able), 1 (never or almost never when needed), 2 (sometimes when needed), or 3 (always or almost always when needed). The parent/primary caregiver form (ages 0–5, 241 items) or parent form (ages 5–21 years, 232 items) were used as appropriate by follow-up age. Completion takes about 20 minutes. The Global Adaptive Composite Scores were used in our main analysis, and it has been classified as very superior (≥130 score, ≥98th percentile), superior (120–129 score, 91–97th percentile), above average (110–119 score, 75–90th percentile), average (90–109 score, 25–74th percentile), below average (80–89 score, 9–24th percentile), borderline (71–79 score, 3–8th percentile), and extremely low (≤70 score, ≤2nd percentile).
The Child Behavior Checklist (CBCL) assesses behavioral-emotional problems and competencies.[31,32] The CBCL is made up of eight syndrome scales (anxious/depressed, depressed, somatic complaints, social problems, thought problems, attention problems, rule breaking behavior, and aggressive behavior) which lead to two higher order factors (internalizing and externalizing) and the Total Problem Score. For each item, the respondent chooses either 0 (absent), 1 (occurs sometimes), or 2 (occurs often) over the last 2 months (preschool form) or 6 months (school-age form). The school-age form (ages 6–18 years, 112 items) or the pre-school form (ages 1.5–5 years, 99 items) were used as appropriate by follow-up age. Completion takes about 20 minutes. The Total Problem Score was used in our main analysis, and it has been classified as normal range (<60 score), borderline (60–63 score, 84–90th percentile) and clinical (>63 score, >90th percentile).
The Behavior Rating Inventory of Executive Function (BRIEF) is a standardized rating scale assessing real-world behavioral manifestations of executive skills.[33] It assesses eight interrelated subdomains of executive function and provides scores for behavioral regulation and metacognition which together produce a Global Executive Composite score. For each item, the respondent chooses never, sometimes, or often based on the prior 6 months. Completion takes about 15 minutes. The BRIEF was only administered to subjects who were ≥5 years old at the time of follow-up. Our analysis used the Global Executive Composite Score, and scores >65 are considered potentially clinical significant.
Analyses
Summary statistics are reported as medians and interquartile ranges (IQR) for continuous data and counts and proportions for categorical data. Comparisons between subjects with and without follow-up data were examined using the chi-square test for categorical variables and the Wilcoxon’s rank-sum or Kruskal Wallis tests for continuous variables. Linear regression was used to test the association between seizure category and neurobehavioral outcome scores. Variables with p ≤0.2 in univariable analyses were eligible for inclusion in the multivariable models. All statistics were performed on Stata 10.0 (College Station, TX).
Results
We enrolled 300 encephalopathic children in the acute-care component of the study. One-hundred and thirty-seven subjects were reported to be neurodevelopmentally normal at PICU admission by parents/guardian report and survived to PICU discharge. Sixty study participants were enrolled by phone in the long-term outcome study while 73 could not be contacted and 4 declined participation. Figure 1 provides a flowchart of study enrollment.
Figure 1.
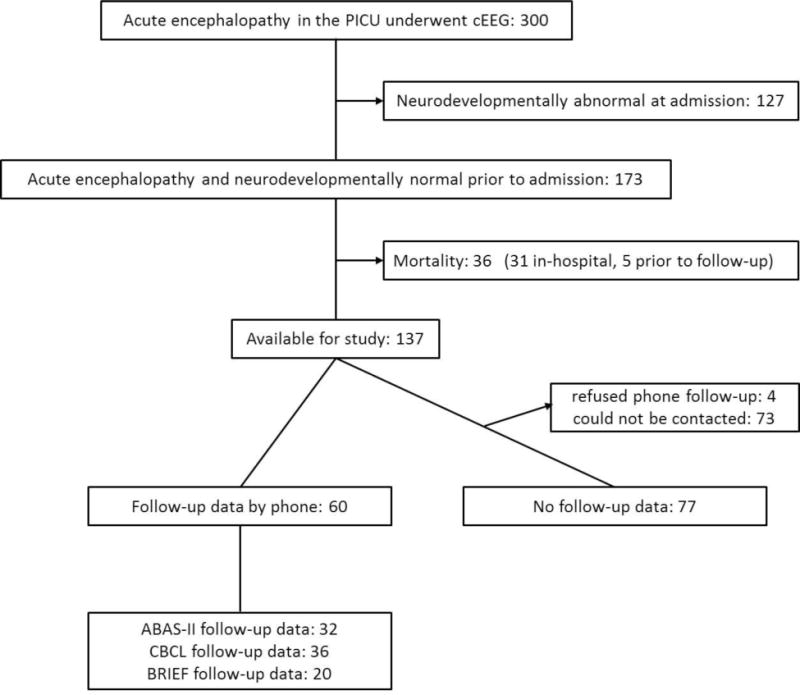
Study flowchart.
We compared subjects with and without follow-up data. For the ABAS-II and CBCL, there were 137 eligible subjects (neuro-developmentally normal on PICU admission and alive at PICU discharge). For the ABAS-II, we identified no significant differences in the acute care variables between the 32 subjects with outcome data and the 105 subjects without outcome data (Table 1). For the CBCL, we identified no significant differences in the acute care variables between the 36 subjects with outcome data and the 101 subjects without outcome data, except that a higher proportion of subjects without CBCL data had convulsions preceding cEEG (Table 1). For the BRIEF, there were 67 eligible subjects (neuro-developmentally normal on PICU admission, alive at PICU discharge, and greater than 5 years old at the time of follow-up). Fewer subjects were eligible for the BRIEF than the ABAS or CBCL since subjects had to be older than 5 years at the time of follow-up to complete the BRIEF. Follow-up data were obtained over about 6 months and among subjects who could be contacted, the median duration to follow-up was 2.6 years. To compare subjects with and without follow-up data for the BRIEF, we needed to determine which subjects would have been eligible. We added 2.6 years, the median duration to follow-up in subjects with follow-up data available, to the ICU discharge age of subjects without follow-up data to determine whether they would have been eligible for the BRIEF. For the BRIEF, we identified no significant differences in the acute care variables between the 20 subjects with outcome data and the 47 subjects without outcome data (Table 1).
Table 1.
Comparison of subjects with and without follow-up data.
| Variables | Adaptive Behavior Assessment System II (ABAS-II) | Child Behavior Checklist (CBCL) | Behavior Rating Inventory of Executive Function (BRIEF) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Follow-Up Data N = 32 (23%) | No Follow-Up Data N = 105 (77%) | p-value | Follow-Up Data N = 36 (26%) | No Follow-Up Data N = 101 (74%) | p-value | Follow-Up Data N = 20 (30%) | No Follow-Up Data N = 47 (70%) | p-value | |
| Age at PICU Admission (median, IQR%) | 4.1 (2.0, 9.8) | 1.6 (0.4, 8.9) | 0.07 | 3.8 (1.3, 8.8) | 2.0 (0.4, 9.5) | 0.37 | 10.6 (6.7, 15.4) | 7.0 (4.4, 14.3) | 0.17 |
|
Sex Male Female |
23 (72%) 9 (28%) |
63 (60%) 42 (40%) |
0.22 |
26 (72%) 10 (28%) |
60 (59%) 41 (41%) |
0.17 |
15 (75%) 5 (25%) |
29 (62%) 18 (38%) |
0.29 |
|
Acute Neurologic Disorder Epilepsy Acute Structural Acute Non-Structural |
3 (9%) 23 (72%) 6 (19%) |
8 (8%) 75 (71%) 22 (21%) |
0.93 |
8 (8%) 72 (71%) 21 (21%) |
3 (8%) 26 (72%) 7 (19%) |
0.98 |
2 (10%) 12 (60%) 6 (30%) |
4 (9%) 35 (74%) 8 (17%) |
0.45 |
|
Comatose Yes No |
18 (56%) 14 (44%) |
61 (58%) 44 (42%) |
0.85 |
17 (47%) 19 (53%) |
41 (41%) 60 (59%) |
0.49 |
13 (65%) 7 (35%) |
23 (49%) 24 (51%) |
0.23 |
|
Intubated Yes No |
25 (78%) 7 (22%) |
81 (77%) 24 (23%) |
0.91 |
79 (78%) 22 (22%) |
27 (75%) 9 (25%) |
0.69 |
15 (75%) 5 (25%) |
34 (72%) 13 (28%) |
0.82 |
|
Paralyzed Yes No |
7 (22%) 25 (78%) |
17 (16%) 88 (84%) |
0.50 |
18 (18%) 83 (82%) |
6 (17%) 30 (83%) |
0.88 |
5 (25%) 15 (75%) |
9 (19%) 38 (81%) |
0.59 |
|
Convulsions Preceding cEEG Yes No |
15 (47%) 17 (53%) |
61 (58%) 44 (42%) |
0.26 |
13 (36%) 23 (64%) |
63 (62%) 38 (38%) |
0.006 |
10 (50%) 10 (50%) |
20 (43%) 27 (57%) |
0.58 |
|
EEG Background Sedated Sleep – Slow Disorganized Discontinuous – Burst Suppression – Attenuated |
30 (94%) 2 (6%) |
95 (90%) 10 (10%) |
0.57 |
34 (94%) 2 (6%) |
91 (90%) 10 (10%) |
0.43 |
19 (95%) 1 (5%) |
42 (89%) 5 (11%) |
0.46 |
|
Seizure Category No Seizure Electrographic Seizures Electrographic Status Epilepticus |
19 (59%) 7 (22%) 6 (19%) |
59 (56%) 25 (24%) 21 (20%) |
0.95 |
22 (61%) 7 (19%) 7 (19%) |
56 (55%) 25 (25%) 20 (20%) |
0.79 |
11 (55%) 4 (20%) 5 (25%) |
34 (72%) 8 (17%) 6 (11%) |
0.27 |
| PICU Length of Stay (median, IQR) | 7 (3, 11) | 6 (3, 11) | 0.79 | 6 (3, 12) | 6 (3, 11) | 0.92 | 7 (3, 18) | 8 (6, 12) | 0.62 |
|
Discharge PCPC 1 (normal) 2 (mild disability) 3 (moderate disability) 4 (severe disability) 5 (coma and vegetative state) |
15 (47%) 6 (19%) 7 (22%) 4 (13%) 0 (0%) |
46 (44%) 27 (26%) 13 (12%) 18 (17%) 1 (1%) |
0.61 |
45 (45%) 26 (26%) 13 (13%) 16 (16%) 1 (1%) |
16 (44%) 7 (19%) 7 (19%) 6 (17%) 0 (0%) |
0.81 |
9 (45%) 6 (30%) 2 (10%) 3 (15%) 0 (0%) |
23 (49%) 12 (26%) 4 (9%) 7 (15%) 1 (2%) |
0.96 |
Among the 32 subjects with ABAS-II data, 19 (59%) had no seizures, 7 (22%) had ES, and 6 (19%) had ESE. The most common acute etiologies were hypoxic-ischemic encephalopathy (6, 19%), traumatic brain injury (6, 19%), stroke (4, 13%), CNS infection (4, 13%), and systemic medical (4, 13%). Median ABAS-II Global Adaptive Composite Scores were significantly different based on seizure category (Table 2). The median (IQR) scores were 105 (100, 118) for subjects with no seizures, 92 (47, 106) for subjects with ES, and 73 (48, 102) for subjects with ESE (p=0.04). On univariate analysis, compared to patients without any seizures, ES and ESE were associated with worse ABAS-II adaptive behavioral global composite scores (ES coefficient −21.5, p=0.05; ESE coefficient −29.7, p=0.01). EEG background category and comatose category were also significantly associated with ABAS-II scores (see Table 4) and therefore were included in the multi-variate analysis. On multi-variate analysis seizure category (ES coefficient −28, p=0.01, ESE coefficient −36, p=0.003) and EEG background category (discontinuous or burst suppression EEG background coefficient −47, p=0.008) were significantly associated with worse ABAS-II scores, while comatose category was not associated with worse ABAS-II scores (comatose coefficient 3, p=0.74) (Table 3).
Table 2.
Univariate analysis of adaptive behavior, behavior and emotional problems, and executive function.
| Variable | Adaptive Behavior Assessment System II (ABAS-II) Global Adaptive Composite Scoresa Median (IQR) N=32 |
p-value | Child Behavior Checklist (CBCL) Total Problems Scoresb Median (IQR) N=36 |
p-value | Behavior Rating Inventory of Executive Function (BRIEF) Global Executive Composite Scoresc Median (IQR) N=20 |
p-value |
|---|---|---|---|---|---|---|
|
Seizure Category No Seizure Electrographic Seizures Electrographic Status Epilepticus |
105 (100, 118) 92 (47, 106) 73 (48, 102) |
0.04 |
43 (37, 54) 37 (34, 52) 61 (34, 65) |
0.26 |
54 (42, 63) 57 (46, 65) 73 (59, 79) |
0.13 |
|
EEG Background Sedated Sleep – Slow Disorganized Discontinuous – Burst Suppression-Attenuated |
105 (80, 108) 62 (40, 83) |
0.09 |
43 (36, 54) 49 (34, 64) |
0.94 |
56 (43, 65) 68 (68, 68) |
0.34 |
|
Acute Neurologic Disorder Epilepsy Acute Structural Acute Non-Structural |
92 (70, 105) 105 (72, 111) 104 (91, 106) |
0.77 |
41 (37, 52) 42 (34, 54) 54 (36, 65) |
0.42 |
57 (49, 64) 50 (42, 71) 61 (56, 65) |
0.60 |
|
Age at PICU Admission <2 years ≥2 years |
107 (74, 117) 103 (76, 106) |
0.35 |
40 (32, 47) 44 (38, 57) |
0.20 | * | * |
| PICU Duration (linear regression coefficient) | −0.29 | 0.23 | 0.04 | 0.75 | −0.02 | 0.91 |
|
Sex Male Female |
105 (72, 108) 102 (91, 108) |
0.90 |
41 (36, 60) 46 (41, 54) |
0.57 |
63 (42, 73) 54 (49, 56) |
0.54 |
|
Comatose Yes No |
97 (70, 105) 105 (100 118) |
0.18 |
45 (37, 60) 42 (34, 51) |
0.65 |
54 (46, 65) 63 (42, 77) |
0.60 |
|
Intubated Yes No |
105 (70, 108) 102 (100, 105) |
0.96 |
41 (34, 54) 51 (42, 65) |
0.15 |
54 (43, 68) 63 (59, 64) |
0.48 |
|
Paralyzed Yes No |
104 (80, 106) 105 (65, 118) |
0.70 |
42 (36, 54) 50 (40, 54) |
0.45 |
59 (43, 68) 54 (46, 56) |
0.73 |
|
Convulsions Preceding cEEG Yes No |
102 (70, 108) 105 (83, 108) |
0.83 |
41 (36, 52) 45 (37, 54) |
0.63 |
58 (46, 65) 56 (42, 68) |
0.82 |
| Follow-up Duration in years (linear regression coefficient) | −1.19 | 0.81 | 1.27 | 0.59 | 3.71 | 0.29 |
ABAS-II Global Adaptive Composite Scores classified as very superior (≥130 score), superior (120–129 score), above average (110–119 score), average (90–109 score), below average (80–89 score), borderline (71–79 score), and extremely low (≤70 score).
CBCL Total Problem Scores classified as normal range (<60 score), borderline (60–63 score) and clinical (>63 score).
BRIEF Global Executive Composite scores > 65 are considered potentially clinically significant.
BRIEF was only administered for subjects >5 years old at the time of follow-up, so all had been ≥2 years old at PICU admission.
Table 3.
Multivariate analysis of ABAS-II Global Adaptive Composite Scores.
| Variable | Linear Coefficient | 95% Confidence Interval | p-value |
|---|---|---|---|
|
Seizure Category No Seizure Electrographic Seizures Electrographic Status Epilepticus |
– −28 −36 |
– −50 – −6 −58 – −13 |
– 0.014 0.003 |
|
EEG Background Sedated Sleep – Slow Disorganized Discontinuous – Burst Suppression – Attenuated |
– −47 |
– −80 – −14 |
– 0.008 |
|
Comatose Category Not Comatose Comatose |
– 3 |
– −15 −21 |
– 0.34 |
Among the 36 subjects with CBCL data, 22 (61%) had no seizures, 7 (19%) had ES, and 7 (19%) had ESE. The most common acute etiologies were traumatic brain injury (8, 22%), hypoxic-ischemic encephalopathy (7, 19%), systemic-medical (5, 14%), CNS infection (4, 11%), and stroke (4, 11%). The median (IQR) scores were 43 (37, 54) for subjects with no seizures, 37 (34, 52) for subjects with ES, and 61 (34, 65) for subjects with ESE (p=0.26) (Table 4). On univariate analysis, compared to patients without any seizures, ES and ESE were not associated with significantly worse CBCL total problem scores (ES coefficient −4.1, p=0.48; ESE coefficient 8.9, p=0.13). Multi-variate analysis was not performed.
Among the 20 subjects with BRIEF data, 11 (55%) had no seizures, 4 (20%) had ES, and 5 (25%) had ESE. The most common acute etiologies were systemic-medical (5, 25%), hypoxic-ischemic encephalopathy (3, 15%), traumatic brain injury (3, 15%), CNS infection (3, 15%), and epilepsy (2, 10%). The median and IQR scores were 54 (42, 63) for subjects with no seizures, 57 (46, 65) for subjects with ES, and 73 (59, 79) for subjects with ESE (p=0.13) (Table 4). On univariate analysis, compared to patients without any seizures, ES and ESE were not associated with significantly worse BRIEF global executive function scores (ES coefficient 2.1, p=0.78; ESE coefficient 14.1, p=0.06). Multi-variate analysis was not performed.
Discussion
ES have been reported in 10–40% of children in PICUs who underwent cEEG.[1–14,26,34–37] Since identifying and managing ES and ESE could reduce secondary brain injury and thereby improve patient outcomes, cEEG use in critically ill children is increasing,[19] guidelines mandate cEEG use in many critically ill patients to identify and manage ESE,[20–22] and anti-seizure medications are generally administered when ES or ESE are identified.[18,28]
Several studies have suggested mechanisms by which ES could produce secondary brain injury, including elevated intracranial pressure and lactate/pyruvate ratios during ES in adults with traumatic brain injury,[38] hippocampal atrophy ipsilateral to ES in adults with traumatic brain injury,[39] and regional hyper-perfusion concordant with ES in adults with epilepsy.[40] In critically ill children, prior studies evaluating short-term outcomes have reported associations between ES or ESE and worse short-term outcome[1,9,10,12,23–25] even after adjusting for potential confounders related to acute encephalopathy etiology and critical illness severity.[1,10,25] We have previously reported that in a 60 subject cohort with a median follow-up duration of 2.6 years, ESE was associated with unfavorable global outcome, lower health-related quality of life, and an increased risk of developing subsequent epilepsy after controlling for age, acute neurologic disorder category, and EEG background category.[27]
The current exploratory work extends the prior observations using more detailed neurobehavioral outcome measures in a small subset of patients. Similar to the previously reported broader outcome measures, patients with ESE had worse adaptive behavior scores compared to patients without seizures, and despite the small sample size there were trends towards worse problem behavior and worse executive function scores. Score variations were substantial with less favorable scores (lower ABAS-II, higher CBCL, and higher BRIEF) in subjects with ESE, although only the less favorable ABAS-II score was significantly worse. For example, an ABAS-II Global Adaptive Composite score of 73 with ESE is at the 3–7th percentile (within the borderline range), a CBCL Total Problems score of 63 with ESE is at the 84–90th percentile (within the borderline range), and a BRIEF Global Executive Composite score of 73 is at the 99th percentile (within the clinically significant range).
The association between ESE and worse outcomes persists in analyses adjusting for brain injury etiology and severity. This suggests that ESE might be producing secondary brain injury and that identifying and managing ESE might reduce secondary brain injury, thereby serving as a neuroprotective strategy. However, to date, studies have not evaluated whether specific ESE identification and management strategies are associated with better outcomes. Our prior work has indicated that subsequent studies comparing various identification and management strategies might include assessments of differences in global functional, quality of life, and epilepsy outcomes. However, in addition to these larger scope outcome measures, such studies might be enhanced by additional neurobehavioral outcome measures. The current data indicate that the ABAS-II, CBCL and BRIEF may be sensitive to differences across seizure burdens. Therefore, these validated measures may be sensitive to outcome differences in future studies aiming to compare outcomes in subjects managed with varied ESE identification and management strategies.
This study has multiple limitations. First, follow-up data was only obtained for a small proportion of subjects from the original cohort so biases related to differential follow-up acquisition are possible. However, acute care data was available for all subjects, and no differences could be identified between subjects with and without follow-up data, suggesting the small cohort might be representative of the entire cohort. The current data were derived from an observational study intended to address acute care questions, such as the incidence and risk factors for ES[14] and short-term outcome.[25] The component related to long-term outcome assessment was subsequently added to the study, but efforts were not made during the intervening years to keep track of subjects. Future studies designed to evaluate long-term outcome would include efforts to track subjects over time, leading to a higher proportion of subjects with follow-up data available. Second, cEEG was initiated only when considered clinically indicated by the critical care or neurology consult services, and this determination may have varied among clinicians. Future studies will benefit from ensuring specific inclusion criteria for cEEG. Third, we stratified seizure burden as ES and ESE, and ESE could involve prolonged or multiple brief seizures. The optimal method for stratifying seizure burden is unknown, and future studies may benefit from a continuous rather than categorical measure of seizure burden, as has been done in other studies.[26] Fourth, we only included subjects who were neurodevelopmentally normal upon PICU admission. This design avoided needing to assess for changes in neurodevelopmental trajectory among patients who were neurodevelopmentally abnormal on admission, but this limits generalization of these data. Fifth, while we used established neurobehavioral outcome measures, we did not perform full neuropsychological evaluations which may have identified additional differences between seizure category groups. Sixth, more robust methods of adjusting for brain injury etiology and severity may yield differing results. The occurrence of ESE indicates more severe brain injury and thus predicts worse outcome, but ESE may also produce some secondary brain injury and contribute to worse outcomes. Future studies in more homogeneous etiology cohorts that include additional variables related to critical illness and brain injury severity may help clarify this central issue. Given all these limitations, a larger prospective longitudinal study including protocoled cEEG indications, standardized cEEG durations, active methods of subject retention, and formal neuropsychological assessments could yield an improved understanding of long-term outcome.
Conclusions
Among previously normal children with acute neurologic disorders in the PICU, ES and ESE were associated with worse adaptive behavior scores and trends toward worse behavioral-emotional and executive function problem scores. In future studies comparing various ESE identification and management strategies, these measures may be sensitive to outcome differences.
Supplementary Material
Highlights.
We aimed to determine if ESE was associated with worse outcomes using neurobehavioral measures.
We evaluated for associations between ESE and adaptive behavior, behavioral and emotional problems, and executive function.
On multivariate analysis, when compared to subjects with no seizures, both electrographic seizures and electrographic status epilepticus were associated with worse adaptive behavioral global composite scores.
Acknowledgments
Study Funding:
The study was supported by NIH (K23NS076550) to Dr. Abend.
J. Radcliffe receives funding from the NIH Penn/CHOP Clinical and Translational Service Award (Grant UL1RR024134), Utility of Nasal Steroids for Treatment of Sleep Disorders, and Adolescent Trials Network Mentorship Program, and DHHS FDA, Polyethylene glycol safety in children. She receives payment for consultation to the City of Philadelphia.
R. Berg reports no disclosures.
D. Dlugos receives research funding from NIH (1R01NS053998, 2U01NS045911,1R01LM011124, and U01NS077276) and has received payment for medical-legal review work.
A. Topjian receives research funding from NIH (K12HD047349 and U01HL094345)
N. Abend receives research funding from NIH (K23NS076550), receives royalties from Demos Medical Publishing, and has received payment for medical-legal review work.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions
Katherine Wagenman – Acquisition of data, critical revision of the manuscript.
Taylor Blake – Study concept and design, analysis and interpretation, critical revision of the manuscript.
Sarah Sanchez – Acquisition of data, critical revision of the manuscript.
Dr. Schultheis – Study concept and design, analysis and interpretation, critical revision of the manuscript.
Dr. Radcliffe – Study concept and design, analysis and interpretation, critical revision of the manuscript.
Dr. Berg – Study concept and design, analysis and interpretation, critical revision of the manuscript.
Dr. Dlugos – Study concept and design, analysis and interpretation, critical revision of the manuscript.
Dr. Topjian – Study concept and design, acquisition of data, analysis and interpretation, critical revision of the manuscript.
Dr. Abend – Study concept and design, acquisition of data, analysis and interpretation, drafting of initial version of the manuscript, critical revision of the manuscript, study supervision.
Disclosures
K. Wagenman reports no disclosures.
T. Blake reports no disclosures.
S. Sanchez reports no disclosures.
M. Schultheis reports no disclosures.
Contributor Information
Nicholas S. Abend, Division of Neurology, The Children’s Hospital of Philadelphia (Philadelphia, PA); Department of Neurology and Pediatrics, Perelman School of Medicine at the University of Pennsylvania (Philadelphia, PA).
Katherine L. Wagenman, Division of Neurology, The Children’s Hospital of Philadelphia (Philadelphia, PA).
Taylor P. Blake, Psychology Department, Drexel University (Philadelphia, PA).
Maria T. Schultheis, Psychology Department, Drexel University (Philadelphia, PA).
Jerilynn Radcliffe, Department of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, The Children’s Hospital of Philadelphia (Philadelphia, PA).
Robert A. Berg, Department of Anesthesia and Critical Care Medicine, The Children’s Hospital of Philadelphia and Perelman School of Medicine at the University of Pennsylvania (Philadelphia, PA).
Alexis A. Topjian, Department of Anesthesia and Critical Care Medicine, The Children’s Hospital of Philadelphia and Perelman School of Medicine at the University of Pennsylvania (Philadelphia, PA).
Dennis J. Dlugos, Division of Neurology, The Children’s Hospital of Philadelphia (Philadelphia, PA); Department of Neurology and Pediatrics, Perelman School of Medicine at the University of Pennsylvania (Philadelphia, PA).
References
- 1.Abend NS, Arndt DH, Carpenter JL, Chapman KE, Cornett KM, Gallentine WB, et al. Electrographic seizures in pediatric ICU patients: Cohort study of risk factors and mortality. Neurology. 2013:383–91. doi: 10.1212/WNL.0b013e31829c5cfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hosain SA, Solomon GE, Kobylarz EJ. Electroencephalographic patterns in unresponsive pediatric patients. Pediatr Neurol. 2005:162–5. doi: 10.1016/j.pediatrneurol.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Jette N, Claassen J, Emerson RG, Hirsch LJ. Frequency and predictors of nonconvulsive seizures during continuous electroencephalographic monitoring in critically ill children. Arch Neurol. 2006:1750–5. doi: 10.1001/archneur.63.12.1750. [DOI] [PubMed] [Google Scholar]
- 4.Abend NS, Dlugos DJ. Nonconvulsive status epilepticus in a pediatric intensive care unit. Pediatr Neurol. 2007:165–70. doi: 10.1016/j.pediatrneurol.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 5.Tay SK, Hirsch LJ, Leary L, Jette N, Wittman J, Akman CI. Nonconvulsive status epilepticus in children: clinical and EEG characteristics. Epilepsia. 2006:1504–9. doi: 10.1111/j.1528-1167.2006.00623.x. [DOI] [PubMed] [Google Scholar]
- 6.Shahwan A, Bailey C, Shekerdemian L, Harvey AS. The prevalence of seizures in comatose children in the pediatric intensive care unit: A prospective video-EEG study. Epilepsia. 2010:1198–204. doi: 10.1111/j.1528-1167.2009.02517.x. [DOI] [PubMed] [Google Scholar]
- 7.Abend NS, Topjian A, Ichord R, Herman ST, Helfaer M, Donnelly M, et al. Electroencephalographic monitoring during hypothermia after pediatric cardiac arrest. Neurology. 2009:1931–40. doi: 10.1212/WNL.0b013e3181a82687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams K, Jarrar R, Buchhalter J. Continuous video-EEG monitoring in pediatric intensive care units. Epilepsia. 2011:1130–6. doi: 10.1111/j.1528-1167.2011.03070.x. [DOI] [PubMed] [Google Scholar]
- 9.Greiner HM, Holland K, Leach JL, Horn PS, Hershey AD, Rose DF. Nonconvulsive status epilepticus: the encephalopathic pediatric patient. Pediatrics. 2012:e748–55. doi: 10.1542/peds.2011-2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kirkham FJ, Wade AM, McElduff F, Boyd SG, Tasker RC, Edwards M, et al. Seizures in 204 comatose children: incidence and outcome. Intensive Care Med. 2012:853–62. doi: 10.1007/s00134-012-2529-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arango JI, Deibert CP, Brown D, Bell M, Dvorchik I, Adelson PD. Posttraumatic seizures in children with severe traumatic brain injury. Childs Nerv Syst. 2012:1925–9. doi: 10.1007/s00381-012-1863-0. [DOI] [PubMed] [Google Scholar]
- 12.Schreiber JM, Zelleke T, Gaillard WD, Kaulas H, Dean N, Carpenter JL. Continuous video EEG for patients with acute encephalopathy in a pediatric intensive care unit. Neurocrit Care. 2012:31–8. doi: 10.1007/s12028-012-9715-z. [DOI] [PubMed] [Google Scholar]
- 13.McCoy B, Sharma R, Ochi A, Go C, Otsubo H, Hutchison JS, et al. Predictors of nonconvulsive seizures among critically ill children. Epilepsia. 2011:1973–8. doi: 10.1111/j.1528-1167.2011.03291.x. [DOI] [PubMed] [Google Scholar]
- 14.Abend NS, Gutierrez-Colina AM, Topjian AA, Zhao H, Guo R, Donnelly M, et al. Nonconvulsive seizures are common in critically ill children. Neurology. 2011:1071–7. doi: 10.1212/WNL.0b013e318211c19e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gutierrez-Colina AM, Topjian AA, Dlugos DJ, Abend NS. EEG Monitoring in Critically Ill Children: Indications and Strategies. Pediatric Neurology. 2012:158–61. doi: 10.1016/j.pediatrneurol.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abend NS, Topjian AA, Gutierrez-Colina AM, Donnelly M, Clancy RR, Dlugos DJ. Impact of continuous EEG monitoring on clinical management in critically ill children. Neurocrit Care. 2011:70–5. doi: 10.1007/s12028-010-9380-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abend NS, Topjian AA, Williams S. How much does it cost to identify a critically ill child experiencing electrographic seizures? Journal of Clinical Neurophysiology. doi: 10.1097/WNP.0000000000000170. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abend NS, Dlugos DJ, Hahn CD, Hirsch LJ, Herman ST. Use of EEG monitoring and management of non-convulsive seizures in critically ill patients: a survey of neurologists. Neurocrit Care. 2010:382–9. doi: 10.1007/s12028-010-9337-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanchez SM, Carpenter J, Chapman KE, Dlugos DJ, Gallentine W, Giza CC, et al. Pediatric ICU EEG Monitoring: Current Resources and Practice in the United States and Canada. Journal of Clinical Neurophysiology. 2013:156–60. doi: 10.1097/WNP.0b013e31827eda27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012:3–23. doi: 10.1007/s12028-012-9695-z. [DOI] [PubMed] [Google Scholar]
- 21.Herman ST, Abend NS, Bleck TP, Chapman KE, Drislane FW, Emerson RG, et al. Consensus Statement on Continuous EEG in Critically Ill Adults and Children, Part I: Indications. J Clin Neurophysiol. 2015 doi: 10.1097/WNP.0000000000000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herman ST, Abend NS, Bleck TP, Chapman KE, Drislane FW, Emerson RG, et al. Consensus Statement on Continuous EEG in Critically Ill Adults and Children, Part II: Personnel, Technical Specifications and Clinical Practice. J Clin Neurophysiol. 2015 doi: 10.1097/WNP.0000000000000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lambrechtsen FA, Buchhalter JR. Aborted and refractory status epilepticus in children: a comparative analysis. Epilepsia. 2008:615–25. doi: 10.1111/j.1528-1167.2007.01465.x. [DOI] [PubMed] [Google Scholar]
- 24.Gwer S, Idro R, Fegan G, Chengo E, Garrashi H, White S, et al. Continuous EEG monitoring in Kenyan children with non-traumatic coma. Arch Dis Child. 2012:343–9. doi: 10.1136/archdischild-2011-300935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Topjian AA, Gutierrez-Colina AM, Sanchez SM, Berg RA, Friess SH, Dlugos DJ, et al. Electrographic Status Epilepticus is Associated with Mortality and Worse Short-Term Outcome in Critically Ill Children. Critical Care Medicine. 2013:215–23. doi: 10.1097/CCM.0b013e3182668035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Payne ET, Zhao XY, Frndova H, McBain K, Sharma R, Hutchison JS, et al. Seizure burden is independently associated with short term outcome in critically ill children. Brain. 2014:1429–38. doi: 10.1093/brain/awu042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wagenman KL, Blake TP, Sanchez SM, Schultheis MT, Radcliffe J, Berg RA, et al. Electrographic status epilepticus and long-term outcome in critically ill children. Neurology. 2014:396–404. doi: 10.1212/WNL.0000000000000082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abend NS, Sanchez SM, Berg RA, Dlugos DJ, Topjian AA. Treatment of electrographic seizures and status epilepticus in critically ill children: A single center experience. Seizure. 2013:467–71. doi: 10.1016/j.seizure.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fiser DH, Long N, Roberson PK, Hefley G, Zolten K, Brodie-Fowler M. Relationship of pediatric overall performance category and pediatric cerebral performance category scores at pediatric intensive care unit discharge with outcome measures collected at hospital discharge and 1- and 6-month follow-up assessments. Crit Care Med. 2000:2616–20. doi: 10.1097/00003246-200007000-00072. [DOI] [PubMed] [Google Scholar]
- 30.Harrison P, Oakland T. Adaptive Behavior Assessment System 2nd Edition) Manual. Western Psychological Services; U.S.A: 2003. [Google Scholar]
- 31.Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms and Profiles. University of Vermont Research Center for Children, Youth, and Families; Burlington, VT: 2000. [Google Scholar]
- 32.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. University of Vermont Research Center for Children, Youth, and Families; Burlington, VT: 2001. [Google Scholar]
- 33.Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function. PAR; Lutz, FL: 2000. [Google Scholar]
- 34.Abend NS, Wusthoff CJ, Goldberg EM, Dlugos DJ. Electrographic seizures and status epilepticus in critically ill children and neonates with encephalopathy. Lancet Neurol. 2013:1170–9. doi: 10.1016/S1474-4422(13)70246-1. [DOI] [PubMed] [Google Scholar]
- 35.Piantino JA, Wainwright MS, Grimason M, Smith CM, Hussain E, Byron D, et al. Nonconvulsive Seizures Are Common in Children Treated With Extracorporeal Cardiac Life Support. Pediatr Crit Care Med. 2013:601–9. doi: 10.1097/PCC.0b013e318291755a. [DOI] [PubMed] [Google Scholar]
- 36.Arndt DH, Lerner JT, Matsumoto JH, Madikians A, Yudovin S, Valino H, et al. Subclinical early posttraumatic seizures detected by continuous EEG monitoring in a consecutive pediatric cohort. Epilepsia. 2013:1780–8. doi: 10.1111/epi.12369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gold JJ, Crawford JR, Glaser C, Sheriff H, Wang S, Nespeca M. The role of continuous electroencephalography in childhood encephalitis. Pediatr Neurol. 2014:318–23. doi: 10.1016/j.pediatrneurol.2013.12.014. [DOI] [PubMed] [Google Scholar]
- 38.Vespa PM, Miller C, McArthur D, Eliseo M, Etchepare M, Hirt D, et al. Nonconvulsive electrographic seizures after traumatic brain injury result in a delayed, prolonged increase in intracranial pressure and metabolic crisis. Crit Care Med. 2007:2830–6. [PMC free article] [PubMed] [Google Scholar]
- 39.Vespa PM, McArthur DL, Xu Y, Eliseo M, Etchepare M, Dinov I, et al. Nonconvulsive seizures after traumatic brain injury are associated with hippocampal atrophy. Neurology. 2010:792–8. doi: 10.1212/WNL.0b013e3181f07334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hauf M, Slotboom J, Nirkko A, von Bredow F, Ozdoba C, Wiest R. Cortical Regional Hyperperfusion in Nonconvulsive Status Epilepticus Measured by Dynamic Brain Perfusion CT. AJNR Am J Neuroradiol. 2009:693–8. doi: 10.3174/ajnr.A1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


