Abstract
Proper treatment of hypoxic myoclonic status is not clearly determined. Induced hypothermia is improving prognosis and a more aggressive treatment might be beneficial in some patients. Among the new options of antiepileptic drugs, perampanel (PER) is a drug with a novel mechanism, and it might be a promising drug for myoclonic status or as an antimyoclonic drug. We describe the use of PER in one patient with hypoxic super-refractory myoclonic status.
Description
A 51-year-old patient presented after an out-of-hospital cardiac arrest due to an acute myocardial infarction. The patient was diagnosed with clinical and electrical (EEG) myoclonic status at the rewarming phase. Several treatments were used, starting with clonazepam, valproate, sedation (midazolam, propofol), and subsequently barbiturate-induced coma with persistent myoclonic status. Finally, we decided to try PER (dose: 6–8 mg) through a nasogastric tube, resulting in a marked improvement of EEG activity and myoclonus decrease. The patient had a progressive clinical improvement, with a CPC (Cerebral Performance Category) scale score of 1.
Conclusion
This case shows the potential utility of PER as a therapeutic option in super-refractory hypoxic status and even its potential use before other aggressive alternatives considering their greater morbidity.
Keywords: Hypoxic myoclonic status, Perampanel
1. Introduction
The intensity of treatment of postanoxic myoclonic status is not clearly established: it can be considered that myoclonic status is only a marker of the severity of the initial damage and therefore its treatment does not improve the prognosis; however, other authors point out that status epilepticus (SE) acts actively to increase brain injury and worsen prognosis, so its aggressive treatment could improve prognosis [1].
The introduction of therapeutic hypothermia is improving the prognosis of these patients, and there is an increasing number of new studies and reassessment of concepts in hypoxic encephalopathy. Aggressive treatment could be justified in some patients since they may awaken if their seizures are treated adequately. Treatment in these cases is usually initiated in a similar way to any SE but with particularities: clonazepam, valproate, levetiracetam, or piracetam is preferable to other antiepileptic drugs (AEDs) (especially phenytoin) due to their antimyoclonic action, and, if necessary, the comatose state should be induced pharmacologically, controlling the depth of coma by EEG until epileptiform activity is eliminated.
In many centers, the treatment of postanoxic myoclonic status includes all these options (levetiracetam, valproate, midazolam, and propofol) for a minimum of 24 h, and then between 24 and 72 h, the treatment is reassessed according to the patient's condition based on brainstem reflexes and/or cortical response (N20 wave) to somatosensory-evoked potentials.
Among the new options in AEDs, perampanel (PER) constitutes a drug with a novel mechanism of action that makes it attractive for use in situations of SE. We report the first case, to our knowledge, of a patient with postanoxic myoclonic status super-refractory to all antiepileptic drugs and sedatives used, in whom the efficacy of PER was tested.
2. Case report
A 51-year-old male patient presented after an out-of-hospital cardiorespiratory arrest in the context of an anterolateral acute myocardial infarction (AMI) — Killip class II. The patient's history included only active smoking without other cardiovascular risk factors. Cardiopulmonary resuscitation (CPR) maneuvers were performed for 15 min until resumption of spontaneous circulation (ROSC). On arrival to the hospital, the hypothermia protocol was initiated to target a body temperature of 33 °C. A coronary arteriography was subsequently performed with revascularization of the occluded vessel.
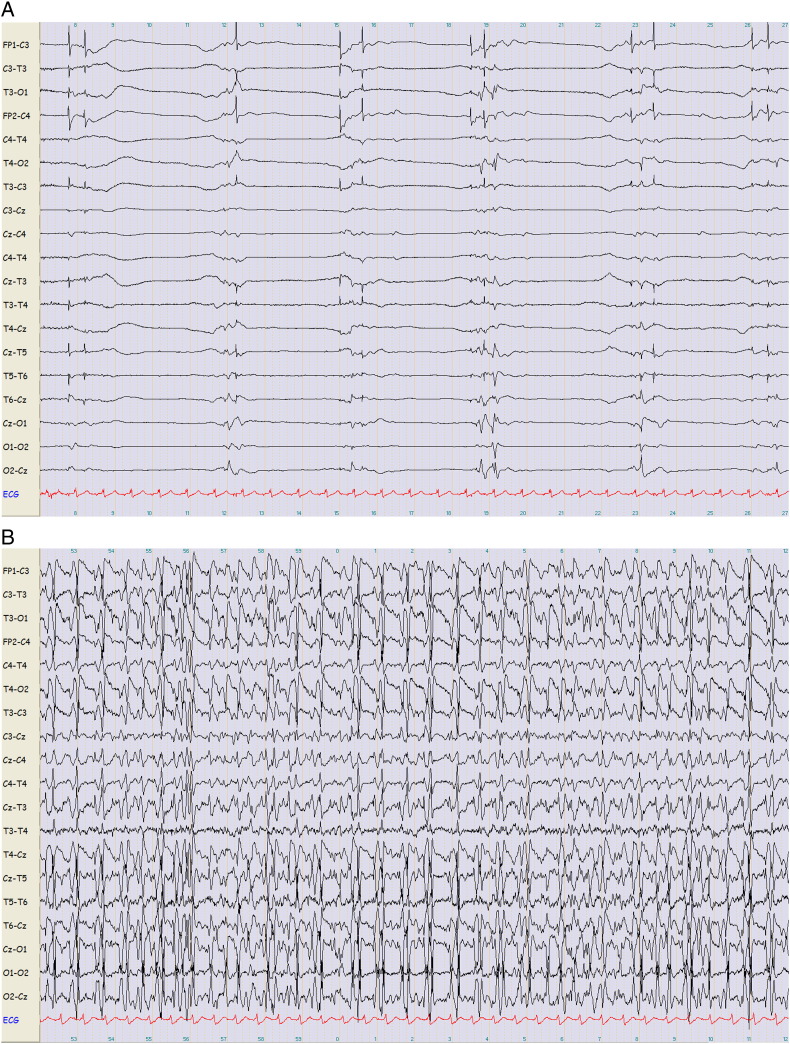
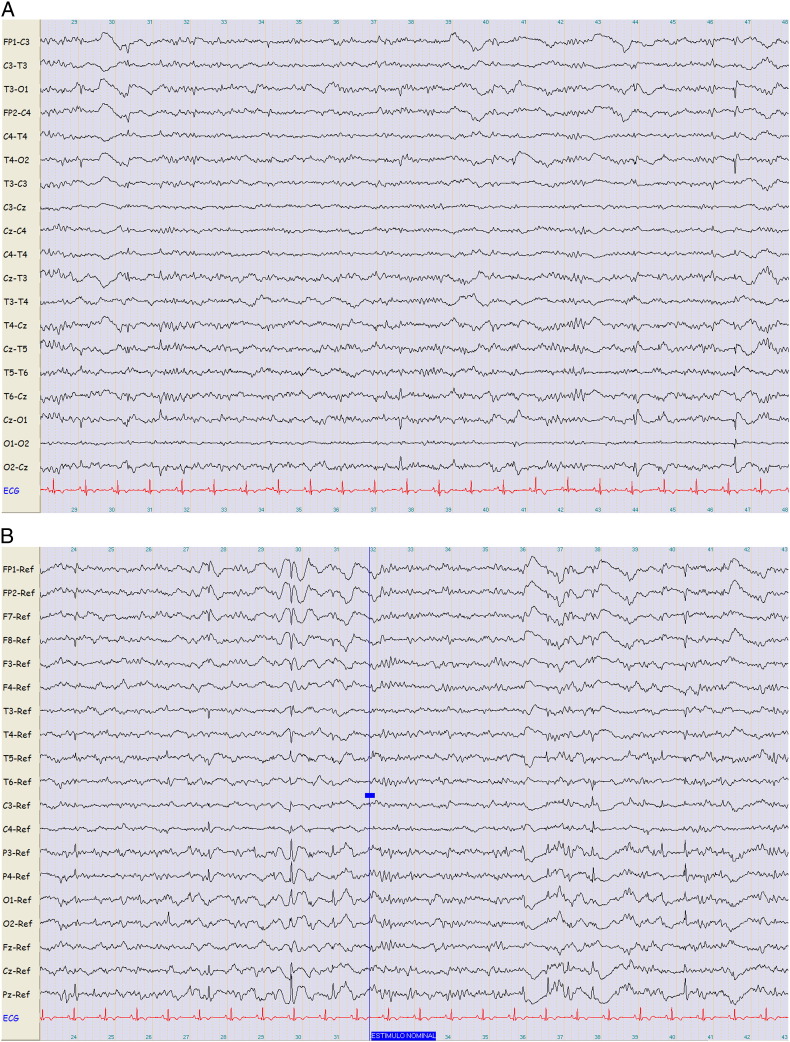
Twelve hours after CPR (still in the hypothermia phase), the patient was observed to have early myoclonic SE with a burst-suppression EEG pattern (Fig. 1a). Despite the introduction of clonazepam and valproic acid (40 mg/kg), electroclinical worsening was observed in the following hours (rewarming phase), with intense spiky bilateral periodic activity on the EEG and increase in myoclonic jerks (Fig. 1b), and levetiracetam (40 mg/kg) was added. The EEG acquired an alternating pattern with persistence of spiky activity and myoclonic jerks (mainly facial), and it was therefore decided to increase the degree of sedation with midazolam and propofol. The patient had brainstem reflexes and response to nociceptive stimulus. Despite high dose sedation, total remission of the myoclonic state was not achieved, and after a week, a barbiturate coma was induced for 48 h. Myoclonic activity recurred after lowering the doses of barbiturate; therefore, we decided to administer perampanel via a nasogastric tube at an initial dose of 6 mg and then 8 mg, with significant clinical and electrical improvement. The EEG showed recovery of background activity with hyporeactive 8-Hz alpha rhythms and isolated spike–waves focalized in the posterior regions of both hemispheres; no myoclonia was identified (Fig. 2a and b). This new situation allowed us to start withdrawal of sedation with clonazepam and to lower the doses of the other AEDs. This was associated clinically with progressive recovery of level of consciousness with the patient connecting to his surroundings and responding to questions coherently. The final CPC (Cerebral Performance Category) scale score was 1.
Fig. 1.
EEG evolution before PER. (a) 12 h post-CPR. Hypothermia (33 °C). Sedation with midazolam and morphine chloride. Burst-suppression pattern. Pectoral and laterocervical myoclonia. (b) 72 h post-CPR. Sedation. AEDs: CZP, VPA. Spiky bilateral periodic discharges.
Bipolar montage (sensitivity: 15 μV/mm; speed: 20 s). CPR: cardiopulmonary resuscitation. AED: antiepileptic drug. CZP: clonazepam. VPA: valproic acid.
Fig. 2.
EEG after administration of PER. No sedation. AEDs: PER, 8 mg/24 h; LEV, 1500 mg/12 h; CZP, 0.5 mg/8 h. (a) 8-Hz alpha rhythms and spike–waves in posterior regions. Bipolar montage (sensitivity: 15 μV/mm; speed: 20 s). (b) Spike–waves in parietal and occipital regions. Reactivity present with greater synchronization of background activity to acoustic stimulation. Referential (common average) montage (sensitivity: 10 μV/mm; speed: 20 s).
AED: antiepileptic drug. PER: perampanel, CZP: clonazepam, LEV: levetiracetam.
The cranial MRI did not show acute or subacute ischemic lesions on the diffusion study nor any other type of signal alterations in cerebral or cerebellar parenchyma.
Treatment with PER was maintained for 10 days with no recurrence of myoclonia, and the other antiepileptic medications (valproate, levetiracetam) were withdrawn without problems.
3. Discussion
To our knowledge, this is the first reported case in the literature of a hypoxic myoclonic SE in which perampanel was used. Few data are available on the possible clinical utility of PER in situations of SE.
AMPA (α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid) receptors play an important role in the initiation and propagation of epileptic activity [2]. In animal models of SE induced by pilocarpine, refractory SE was associated with a selective reduction of surface expression of the GluA2 subunit of the AMPA receptor on hippocampal cell membranes and with increased internalization of this subunit [3]. This results in AMPA receptors with different biophysical characteristics permeable to calcium and, consequently, in continuous neurotransmission. Therefore, inhibition of AMPA receptor activity could be a potential target in the treatment of refractory SE.
Perampanel selectively blocks AMPA receptor-mediated synaptic transmission and thus it appears to be an attractive option for these cases. In addition, PER has shown broad-spectrum antiepileptic activity when administered orally in preclinical animal models, including antimyoclonic activity [4]. These data therefore suggest its potential utility in hypoxic SE.
The aggressive approach to treatment in this patient was based on preservation of brainstem reflexes in the neurological examination and on the presence of early reactivity on EEG recordings followed by a progressive recovery of background activity, as recommended by some authors [1]. The lack of response after administering different AEDs and sedation including barbiturates led us to consider a drug with a different mechanism of action.
It is difficult to demonstrate with a single case the relationship of the drug to cessation of antiepileptic activity, but there seems to be no other explanation in this patient since even the barbiturate had been discontinued before the introduction of PER.
This case shows the potential utility of PER in these dramatic situations and even its potential use before other aggressive alternatives considering their greater morbidity (with prolongation of hospitalization and days requiring intubation).
Disclosures
The authors disclose that there are no known conflicts of interest associated with this publication, and there has been no significant financial support for this work that could have influenced its outcome.
Eisai Farmacéutica financed the translation and adaptation of the present manuscript but did not interfere with the content.
References
- 1.Rossetti A.O., Oddo M., Liaudet L., Kaplan P.W. Predictor of awakening from postanoxic status epilepticus after therapeutic hypothermia. Neurology. 2009;72:744–749. doi: 10.1212/01.wnl.0000343006.60851.62. [DOI] [PubMed] [Google Scholar]
- 2.Rogawski M.A. Revisiting AMPA receptors as an antiepileptic drug target. Epilepsy Curr. 2011;11:56–63. doi: 10.5698/1535-7511-11.2.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rajasekaran K., Todorovic M., Kapur J. Calcium-permeable AMPA receptors are expressed in a rodent model of status epilepticus. Ann Neurol. 2012;72:91–102. doi: 10.1002/ana.23570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanada T., Hashizume Y., Tokuhara N., Takenaka O., Kohmura N., Ogasawara A. Perampanel: a novel, orally active, noncompetitive AMPA-receptor antagonist that reduces seizure activity in rodent models of epilepsy. Epilepsia. 2011;52:1331–1340. doi: 10.1111/j.1528-1167.2011.03109.x. [DOI] [PubMed] [Google Scholar]