Abstract
In an effort to explore opportunities for cancer prevention during preadolescence and adolescence, the Cancer Prevention Across the Lifespan workgroup within the Division of Cancer Prevention and Control at the Centers for Disease Control and Prevention (CDC) convened an informal panel of experts for a 2-day workshop August 9–10, 2011. In this report, we provide highlights from the workshop. A central theme of the workshop was that preadolescence and adolescence are times of unique susceptibility and vulnerability within the lifespan. Participants discussed the evidence linking exposures during adolescence (e.g., risky behaviors, chemicals, medical imaging procedures) and subsequent cancer risk during adulthood. Participants also discussed potential opportunities to intervene on risk factors for cancer at multiple levels during adolescence, the importance of more focused approaches to adequately address health disparities, and the ongoing need for transdisciplinary and translational prevention research. Future opportunities for the CDC include further leveraging surveillance data from sources such as the National Health and Nutrition Examination Survey, the Youth Risk Behavior Surveillance System, and the National Children's Study and continuing to build on collaborations with other federal agencies and with national, state, and local organizations. Many ideas and insights generated during the workshop will be put into action as CDC continues to explore opportunities for cancer prevention during youth and across the lifespan.
Keywords: Cancer prevention, Adolescent health, Translational research
Despite advances in cancer research during the past 40 years, U.S. cancer incidence and death rates have shown only small declines, and incidence rates for some cancers have increased in recent years [1–6]. Cancer has emerged as a leading cause of death, and the number of adults with cancer is expected to grow as the U.S. population ages [7]. New public health approaches to cancer prevention are needed [7–9]. Staff within the Division of Cancer Prevention and Control at the Centers for Disease Control and Prevention (CDC) organized the Cancer Prevention Across the Lifespan (CPAL) workgroup in an effort to foster innovative, public health approaches to cancer prevention. The workgroup is exploring the following overarching questions:
Where is the evidence linking specific risk factors with cancer causation the strongest?
Which of these cancer causes or risk factors could be modified through environmental changes, health policies, systems change, or other social or public health interventions?
What specific public health activities have been demonstrated to be effective or to show promise at the community level to address these cancer risk factors?
How do the answers to these questions differ across the lifespan?
The CPAL workgroup decided to use the Action Model to Achieve Healthy People 2020 Goals as the framework for its efforts (Figure 1). This model illustrates the determinants of health across the lifespan and the need for intervention at multiple levels to improve health outcomes [10]. In addition, the workgroup used the four Strategic Directions of the National Prevention Strategy (healthy and safe community environments, clinical and community preventive services, empowered people, and elimination of health disparities) as a guide to identifying the most effective and achievable strategies for prevention [11].
Figure 1.
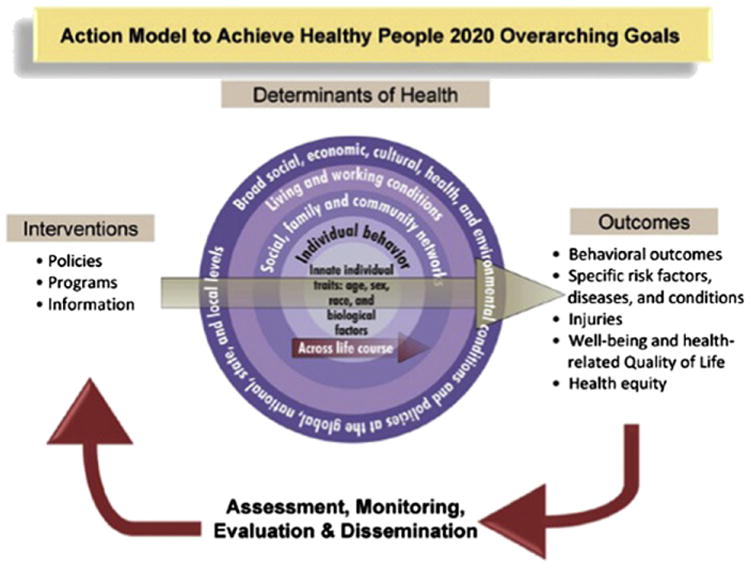
The action model to achieve Healthy People 2020's overarching goals [10].
The CPAL workgroup began addressing the overarching questions listed here by focusing first on preadolescents and adolescents (roughly ages 8–18). We recognize this phase of life could potentially begin and end at other ages as well. This is an age group already targeted by the CDC for cancer prevention efforts with regard to tobacco use, ultraviolet radiation, and the human papillomavirus (HPV) vaccine [3,12–20]. Over time, the CPAL workgroup plans to address cancer prevention at every age, from the prenatal period through late adulthood. The workgroup reviewed the current literature to identify evidence linking exposures and risk factors during preadolescence and adolescence and cancer risk during adulthood. In addition, the workgroup asked experts in a variety of fields to weigh in on relevant research findings and discussion topics.
On August 9–10, 2011, the CPAL workgroup convened an informal panel of experts representing a diverse range of disciplines for a 2-day workshop. The workshop's purpose was to discuss opportunities for cancer prevention during preadolescence and adolescence and to consider where the scientific evidence may be strongest and where public health could have the largest impact. Discussions during the workshop focused on factors during youth that could impact cancer risk during adulthood. Workshop participants included Kimberly Applegate, Frank Biro, Bruce Blumberg, David Carpenter, Frank Chaloupka, Julianna Deardorff, Shanta Dube, Suzanne Fenton, Lindsay Frazier, Sarah Gehlert, Bill Kapogiannis, Lawrence Kushi, DeAnn Lazovich, Somdat Mahabir, Daisy Morales-Campos, Linda Morse, John Santelli, Lee Strunin, and Tami Thomas. These participants contributed knowledge from various fields: adolescent medicine, pediatric oncology, pediatric radiology, developmental biology, endocrinology, toxicology, nutrition, epidemiology, behavioral science, health psychology, social determinants of health, anthropology, nursing, health education, school health, health economics, health policy, and translational science. In addition, staff from various divisions at the CDC also participated in the workshop. The full list of participants can be found in the Acknowledgments section.
The workshop agenda was structured so that participants could share their perspectives through individual presentations and engage in facilitated discussion. The first day focused on the “state of the science” and on discussing factors during preadolescence and adolescence that affect cancer risk during adulthood. The second day was devoted to discussions about translating the current scientific evidence into public health action and exploring promising strategies to reduce harmful exposures and risk factors. Highlights from the workshop discussions and opportunities for the future are described in the following section.
Discussion Highlights
A central theme of the workshop was that preadolescence and adolescence is a time of unique susceptibility and vulnerability within the lifespan [8,21–23]. As children transition from childhood into near-adulthood, they experience many physical, biologic, social, and cultural changes. These changes make preadolescence and adolescence critical times to intervene on both exposures and behaviors that could have a lasting effect on their cancer risk during adulthood. Frank Biro described the sequence of pubertal events that occur during adolescence and explained that the timing of these events is related to both exposures during youth and health outcomes (including risk of certain cancers) during adulthood [23–25]. For example, factors associated with the onset of puberty (e.g., hormonal changes, changes in body composition) may also be associated with later risk of breast cancer [25]. As Biro described these associations, he helped the group to understand why the developing adolescent body is particularly susceptible to the effects of harmful exposures. The diversity of the workshop participants further enriched the subsequent discussions on the various types of exposures during adolescence that may affect cancer risk during adulthood, including behavioral risk factors, chemical exposures, and medical imaging procedures.
Behavioral factors that may affect cancer risk include physical inactivity, poor dietary habits, alcohol and tobacco use, poor sun protection, indoor tanning, and risky sexual activity [26–31]. As described by Lindsay Frazier, Larry Kushi, Julianna Deardorff, and John Santelli, risky behaviors often begin during adolescence and can affect adult health and cancer risk [32]. Sometimes, risky behaviors become habits and are continued into adulthood. For example, many long-term smokers begin smoking before age 18 [33]. However, even exposures that occur solely during youth (e.g., multiple severe sunburns, exposure to a sexually transmitted infection) can have a lasting impact on adult health [22,34]. In either case, adolescence is a key time to intervene on behavioral risk factors in order to optimize lifetime health and decrease cancer risk [32].
Adolescents are also regularly exposed to a number of different chemicals, many of which are known or suspected to increase cancer risk [35]. As explained by David Carpenter, traditional cancer prevention messages that emphasize lifestyle do not adequately address the risks associated with chemical exposures. Endocrine disruptors, exogenous chemicals that interfere with the normal functions of the endocrine system, were of particular interest during workshop discussions. Such chemicals are ubiquitous in our environment and can enter our bodies in many ways. Experts suggest that exposure to endocrine-disrupting chemicals may contribute to chronic morbidities, including obesity, diabetes, and cancer [36]. Sue Fenton and Bruce Blumberg highlighted suspected endocrine disruptors such as perfluorooctanoic acid, bisphenol A, phthalates, and tributyltin. These industrial chemicals are pervasive in the environment, and biomonitoring data from the National Health and Nutrition Examination Survey indicate widespread exposure among the civilian, noninstitutionalized U.S. population, including children and teenagers [37].
Exposure to ionizing radiation during medical imaging procedures may also increase cancer risk. In particular, repeated exposure from procedures such as computed tomography scans and scoliosis radiographs during adolescence may increase lifetime cancer risk [38]. Kimberly Applegate shared not only background information on the evidence that links medical radiation exposure to cancer risk, but also described the Image Gently campaign, a campaign designed to reduce childhood exposure to medical radiation by educating and raising awareness among radiologists, physicians, and parents about the importance of limiting childhood exposure to medical radiation as much as possible [39,40].
The school environment is particularly important to consider when addressing child health and has great potential as a venue for intervention. Linda Morse's presentation, “Let Schools Do It!,” stimulated much discussion about the formidable challenges of public health efforts targeting schools [41]. Most states require less than one credit on health-related topics during 4 years of high school, generally equaling about 27 hours of instruction during the 4 years [42]. During this limited amount of time, many states require that specific subjects (e.g., tobacco use) be covered, which limits addressing other health-related topics. In addition, although national health education standards exist, these standards are voluntary and schools often consider them of lower priority than core subjects (e.g., reading, mathematics, science) that are measured on standardized tests [43]. Some suggest including health-related topics in science courses, but current practices seem to emphasize the engineering and mathematical aspects of science rather than the health-related topics. In addition, few schools have the resources to provide students with preventive care (e.g., funding for school nurses or vaccine administration). Using a whole-child approach to teach children and adolescents to make healthy life choices as part of learning overall life skills may be a way to empower them to make healthy decisions.
Some of the most successful public health efforts have created macro-level change through legislative and environmental changes. Frank Chaloupka and Shanta Dube shared examples from tobacco prevention and control initiatives that have been effective in reducing tobacco use by adolescents, such as product pricing, smoke-free laws, limits on adolescents' access to tobacco, and countermarketing [44–48]. Chaloupka also gave examples of how pricing affects consumption of nontobacco products, such as alcohol and sugar-sweetened beverages [49,50].
Although workshop participants suggested that broad, macro-level changes can have powerful effects, they also recognized the need for more focused approaches to effectively address health disparities. Economic disadvantage is strongly associated with corresponding disparities in education, income, occupation, employment, and housing [51]. Financial constraints also create barriers to engaging in healthful behaviors. For example, a child living in poverty may have poor access to high-quality, nutritious food options and may have higher exposures to dietary contaminants compared with those with greater financial resources. In addition, economic disadvantage leads to disparities in access to medical care, with predictable consequences: people at the lowest level of the socioeconomic scale have less access to healthy communities and quality medical care and thus have the poorest health outcomes [52]. Furthermore, racial and ethnic minorities are more likely to live in communities at the lowest end of the socioeconomic scale [53].
Implementing cancer prevention strategies among disadvantaged and underserved populations demands new, more focused approaches. Workshop participants, including Lee Strunin, Daisy Morales-Campos, Julianna Deardorff, and Tami Thomas, described their approaches to addressing this important charge. Deardorff described a framework that illustrates the causes and consequences of early puberty among U.S. girls and proposed a model that links a lifecourse approach to reducing cancer risk with the underlying mechanisms of individual responses to stress [54]. In this model, psychosocial factors such as low socioeconomic status and family dysfunction can lead to early tobacco and alcohol use, early initiation of sexual activity, overweight, and depression, all of which contribute to one's risk of certain cancers (e.g., breast, lung, cervical) later in life.
Another focused approach to cancer prevention is through community-based participatory research, as described by Lee Strunin. She described lessons learned through collaboration between a community-based organization and a public housing authority [55]. Through this collaboration, young people engaged in competitive recreational sports to reduce violence and substance use. Strunin invited us to view violence and substance use not as individual pathologies, but as consequences of social structural factors such as poverty, limited access to health care, and aggressive tobacco and alcohol marketing.
Morales-Campos advocated for the use of community-based participatory research as an approach to addressing the problem of economic disadvantage. She used two studies conducted in two Hispanic communities as examples. The first study involved exploring barriers to physical activity using participatory photo mapping. This project used photography, narrative interviews with participants, and global positioning units to describe the physical environment and safety in a San Antonio, Texas, neighborhood. The second study also used qualitative research methods to examine Hispanic girls' and their parents' perspectives on the HPV vaccine [56]. Learning that girls want to be informed about decisions regarding their health and that they want to participate in decision-making with their parents provided valuable insights into factors that influence HPV vaccine success.
The importance of community-based approaches to cancer prevention, specifically community engagement with parents, local schools, and churches, was highlighted by Tami Thomas. She described results from her research focused on correlates of HPV vaccination in children ages 9 to 13 in three rural counties in Georgia [57]. These findings demonstrated the unique challenges of cancer prevention in rural areas. Future cancer prevention efforts must consider a “triad” of social determinants: culture, geography, and economy to make sustainable changes in reducing HPV-related cancers.
All workshop participants shared two characteristics: (1) they recognized adolescence as a period of vulnerability to exposures that affect health across the lifespan; and (2) they were open to the viewpoints, concepts, and frameworks of the other disciplines at the table. Participants also recognized the need for transdisciplinary efforts aligned across multiple levels of influence. More than simply bringing together experts who would each address cancer prevention from his or her particular area of interest, a transdisciplinary approach to cancer prevention requires the integration of biological, clinical, environmental, social, and behavioral sciences into collaborative efforts. Of particular note were discussions led by DeAnn Lazovich and Sarah Gehlert. Using indoor tanning as an example, Lazovich described a range of potential interventions to reduce indoor tanning that included price manipulation, regulatory efforts, school policies, provider education, advertising restrictions, and media campaigns. Lazovich challenged the workgroup to consider whether aligning interventions at multiple levels would be more effective than individual efforts at a single level. How could such an approach be designed and how would the effectiveness of a multilevel intervention be evaluated? An additional challenge would be to fund and implement an approach that is likely to be time- and resource-intensive. Gehlert also emphasized the importance of transdisciplinary research efforts that create a new, shared intellectual space with the potential for solving problems that are beyond the scope of any one discipline [58]. Because cancer risk is influenced by multiple factors — genes, individual behaviors, family relationships, demographic factors, environmental carcinogens, and social conditions and policies—a transdisciplinary approach would work by encouraging mutually informative research projects at multiple levels. For example, to understand the aggressiveness of breast cancer in young African-American women, Gehlert described a shared multilevel and multidisciplinary model that considers the effects of community characteristics, housing, social support, behavior patterns, hormones, and genes [59]. In fact, aligning biology and society may create novel opportunities for intervention at many levels, from the cellular to the community.
In addition to emphasizing transdisciplinary research, Gehlert reminded workshop participants of the importance of planning for translation early in intervention development. Translating the scientific findings into public health action is necessary for creating meaningful impact at a population level. Implementation and dissemination are complex sciences in and of themselves and should not be simply be afterthoughts following initial studies of efficacy.
The CDC is not alone in exploring strategies for cancer prevention across the lifespan and the importance of trans-disciplinary research and public health practice. Somdat Mahabir shared highlights from a workshop convened by the National Cancer Institute (NCI) to examine the relationship between early life events and cancer risk in adulthood [60]. Although the age range discussed at the NCI workshop was broader than that discussed during the CPAL workshop, some information presented at the NCI workshop did pertain specifically to preadolescents and adolescents. For example, evidence was presented from animal models to illustrate that factors early in life (e.g., nutritional factors, exposure to radiation) can impact lifetime cancer risk and that puberty is a unique window of vulnerability to the negative effects of harmful exposures.
In addition, Frank Biro, Suzanne Fenton, Larry Kushi, and Julianna Deardorff shared information about and findings from the research conducted through the Breast Cancer and the Environment Research Program, a joint effort co-funded by the National Institute of Environmental Health Sciences and NCI. The Breast Cancer and the Environment Research Program supports a multidisciplinary network of scientists, clinicians, and community partners to examine the effects of environmental exposures that may predispose a woman to breast cancer throughout her life. This network engages both laboratory and population-based research to study puberty and other specific periods when the developing breast may be more vulnerable to environmental exposures.
Opportunities for the Future
The ultimate goal of the workshop was to explore opportunities for cancer prevention efforts targeting youth. Areas of prevention in which the CDC may be able to contribute include reducing exposure to radiation from medical imaging, reducing exposure to harmful environmental chemicals, and promoting and facilitating healthy, protective behaviors (e.g., physical activity, healthful eating, avoidance of tobacco, alcohol, and excessive exposure to ultraviolet radiation). The CDC can address these areas through continued surveillance efforts, collaborations with national, state, and local partners, and through translation and implementation of community programs and policies.
The CDC continues to collect valuable surveillance data, and expanding the capacity of current national surveillance systems to monitor adolescents' exposures and risky behaviors could help move prevention research forward. For example, the CDC continues to improve and expand its measurement of adolescent exposure to environmental chemicals through National Health and Nutrition Examination Survey and adolescent behaviors through the Youth Risk Behavior Surveillance System and the National Children's Study. Some cancer registry data are available to the public via the Research Data Centers [61], and the CDC has ongoing collaborations with state cancer registries to make such data even more accessible to researchers and policy makers.
Emphasizing the value of interventions across multiple levels is particularly important when discussing next steps. Continued collaboration with national, state, and local partners will facilitate working with communities, schools, families, and parents and educating them about risk, exposures, and healthy behaviors. In addition, such collaborations will be important as we work to address structural barriers and the special needs of vulnerable populations in new and innovative ways. Ensuring that prevention efforts at the state and local level align with and complement national efforts will maximize the return we get on our investments in prevention.
CDC is also in a unique position to further inform cancer prevention research and programs through its ability to act as a vehicle for the translation of scientific findings into public health action and the implementation of community programs and policies. For example, the CDC works with the Community Guide Task Force to provide evidence-based recommendations about which intervention strategies work to improve public health [21]. In addition, the CDC conducts research to inform key stakeholders such as policy makers and state cancer control programs. Using the discussions with experts during and after the workshop to inform these efforts could ultimately lead to changes in the cancer prevention paradigm.
The workshop succeeded in providing a neutral space where multiple perspectives and disciplines could learn from each other. Cancer prevention is an enormously complex problem that is beyond the scope of any one discipline. A recurrent theme emerging from the discussions was the need to change how we approach cancer prevention, including creating a more trans-disciplinary approach that integrates actions across multiple levels. Attention is needed not only on carcinogens, but also on factors that modify risk, such as early puberty and obesity, and the interaction of multiple risk factors. Some of the new insights and perspectives generated at the workshop are reflected in the articles within this supplemental issue of the Journal of Adolescent Health.
Among federal agencies, the CDC is unique in having health promotion and disease prevention as a central mission. Several workshop participants encouraged the CDC to exercise its leadership role to continue to pull people together in similar meetings to break down silos and further develop innovative approaches to prevention. Most determinants of health occur outside the health care system, in schools and in communities where people live. Existing networks and partnerships could be leveraged to promote community-based action. In disadvantaged communities where people are challenged to meet the basic needs of life, the focus should be placed on structural changes that facilitate healthy choices and behaviors.
Although the CDC is not a major funder of research, it is a science-based agency and can facilitate public health research and take action as the research shifts. There is a need for research on (1) policy development, especially around pricing; (2) methods to monitor and evaluate the effect of multilevel interventions; and (3) interventions that include dissemination plans from the outset. Because the CDC is the source of considerable data from its surveillance systems, it is important that it make these data more accessible to researchers and others and continue to expand biomonitoring activities, with a particular emphasis on measuring adolescent exposures to endocrine-disrupting chemicals.
As we recognize that different disciplines have different ways of interpreting data, the question becomes, “When do we know enough to take action?” Many workshop participants recommended that we consider a new paradigm for prevention that places a greater emphasis on precaution. To reduce the burden of cancer, we must communicate and act on the basis of what we know. One example could be unnecessary exposure to medical radiation.
Compiling articles from workshop participants into a journal supplement is just one of several tangible actions that we are taking to follow up on the many energizing ideas generated at this workshop. Going forward, we are committed to exploring these suggestions and applying these different ways of thinking to identify new opportunities for cancer prevention across the lifespan.
Acknowledgments
The members of the Cancer Prevention Across the Lifespan (CPAL) workgroup were instrumental in the preparations for the workshop. Workgroup members included Jennifer E. Boehm, Natasha Buchanan, Donatus Ekwueme, Jeffrey D. Glenn, Jane Henley, Dawn Holman, T'Ronda Joseph, Chunyu Li, Jun Li, Antonio Neri, Brandy Peaker, Lucy Peipins, Juan L. Rodriguez, Katherine B. Roland, Sherri L. Stewart, Katrina F. Trivers, Meg Watson, Hannah Weir, Mary C. White, and Susan White. Workshop participants included Kimberly Applegate, Frank Biro, Bruce Blumberg, David Carpenter, Frank Chaloupka, Julianna Deardorff, Suzanne Fenton, Lindsay Frazier, Sarah Gehlert, Bill Kapogiannis, Lawrence Kushi, DeAnn Lazovich, Somdat Mahabir, Daisy Morales-Campos, Linda Morse, John Santelli, Lee Strunin, and Tami Thomas. In addition to CPAL workgroup members, the following CDC staff participated in the workshop: Shanta Dube (CDC, Office on Smoking and Health), Dafna Kanny (CDC, Alcohol Program, Division of Adult and Community Health), Ann Malarcher (CDC, Office on Smoking and Health), Marion Nadel (CDC, Division of Cancer Prevention and Control), Marcus Plescia (CDC, Division of Cancer Prevention and Control), Bettylou Sherry (CDC, Division of Nutrition, Physical Activity, and Obesity), and Heather Strosnider (CDC, Environmental Health Tracking). The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Publication of this article was supported by the Centers for Disease Control and Prevention.
All authors are federal employees and have no conflicts of interest to disclose.
References
- 1.Holman DM, Soman A, Watson M, et al. Examination of the increase in thyroid cancer incidence among younger women in the United States by age, race, geography, and tumor size, 1999-2007. J Adolesc Young Adult Oncol. 2011;1:95–102. doi: 10.1089/jayao.2011.0014. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Saraiya M, Patel P, et al. Recent trends in cutaneous melanoma incidence and death rates in the United States, 1992-2006. J Am Acad Dermatol. 2011;65:S17–25. doi: 10.1016/j.jaad.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 3.Jemal A, Simard EP, Dorell C, et al. Annual report to the nation on the status of cancer, 1975-2009, featuring the burden and trends in human papillomavirus (HPV)-associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. 2013;105:175–201. doi: 10.1093/jnci/djs491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li J, German R, King J, et al. Recent trends in prostate cancer testing and incidence among men under age of 50. Cancer Epidemiol. 2012;36:122–7. doi: 10.1016/j.canep.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 5.Simard EP, Ward EM, Siegel R, et al. Cancers with increasing incidence trends in the United States: 1999 through 2008. CA Cancer J Clin. 2012;62:118–28. doi: 10.3322/caac.20141. [DOI] [PubMed] [Google Scholar]
- 6.Trivers KF, Sabatino SA, Stewart SL. Trends in esophageal cancer incidence by histology, United States, 1998-2003. Int J Cancer. 2008;123:1422–8. doi: 10.1002/ijc.23691. [DOI] [PubMed] [Google Scholar]
- 7.Smith BD, Smith GL, Hurria A, et al. Future of cancer incidence in the United States: Burdens upon an aging, changing nation. J Clin Oncol. 2009;27:2758–65. doi: 10.1200/JCO.2008.20.8983. [DOI] [PubMed] [Google Scholar]
- 8.National Cancer Institute (NCI) Annual Report. Washington, DC: NCI; 2010. President's Cancer Panel. Reducing environmental cancer risk: What we can do now: 2008-2009. [Google Scholar]
- 9.White MC, Peipins LA, Watson M, et al. Cancer prevention for the next generation. J Adolesc Health. 2013;52(suppl 5):S1–7. doi: 10.1016/j.jadohealth.2013.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.U.S. Department of Health and Human Services (DHHS), Office of Disease Prevention and Health Promotion. Phase I report: Recommendations for the framework and format of Healthy People 2020. Washington, DC; DHHS; 2008. Available at: http://healthypeople.gov/2020/about/advisory/PhaseI.pdf. [Google Scholar]
- 11.National Prevention Council. National Prevention Strategy. Washington, DC: Office of the Surgeon General; 2011. [Accessed February 19, 2013]. Available at: http://www.healthcare.gov/prevention/nphpphc/strategy/report.pdf. [Google Scholar]
- 12.Centers for Disease Control and Prevention. The guide to community preventive services: What works to promote health. Restricting minors' access to tobacco products. Available at: http://www.thecommunityguide.org/tobacco/restrictingaccess/index.html.
- 13.U.S. Department of Health and Human Services. Preventing tobacco use among youth and young adults: A report of the Surgeon General. Rockville, MD: Office of the Surgeon General; 2012. [Google Scholar]
- 14.Farrelly MC, Loomis BR, Han B, et al. A comprehensive examination of the influence of state tobacco control programs and policies on youth smoking. Am J Pub Health. 2013;103:549–55. doi: 10.2105/AJPH.2012.300948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kepka D, Berkowitz Z, Yabroff KR, et al. Human papillomavirus vaccine practices in the USA: Do primary care providers use sexual history and cervical cancer screening results to make HPV vaccine recommendations? Sex Transm Infect. 2012;88:433–5. doi: 10.1136/sextrans-2011-050437. [DOI] [PubMed] [Google Scholar]
- 16.Jim CC, Lee JW, Groom AV, et al. Human papillomavirus vaccination practices among providers in Indian health service, tribal and urban Indian healthcare facilities. J Womens Health (Larchmt) 2012;21:372–8. doi: 10.1089/jwh.2011.3417. [DOI] [PubMed] [Google Scholar]
- 17.Guy GP, Jr, Tai E, Richardson LC. Use of indoor tanning devices by high school students in the United States, 2009. Prev Chronic Dis. 2011;8:A116. Available at: http://www.cdc.gov/pcd/issues/2011/sep/pdf/10_0261.pdf. [PMC free article] [PubMed] [Google Scholar]
- 18.Miyamoto J, Berkowitz Z, Jones SE, Saraiya M. Indoor tanning device use among male high school students in the United States. J Adolesc Health. 2012;50:308–10. doi: 10.1016/j.jadohealth.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 19.Weir HK, Marrett LD, Cokkinides V, et al. Melanoma in adolescents and young adults (ages 15-39 years): United States, 1999-2006. J Am Acad Dermatol. 2011;65:S38e1–S38e3. doi: 10.1016/j.jaad.2011.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. The guide to community preventive services: What works to promote health. Cancer. Available at: http://www.thecommunityguide.org/cancer/index.html.
- 21.Biro FM, Wolff MS. Puberty as a window of susceptibility. In: Russo J, editor. Environment and Breast Cancer. New York: Springer; 2011. pp. 29–41. [Google Scholar]
- 22.Casey BJ, Jones RM. Neurobiology of the adolescent brain and behavior: Implications for substance use disorders. J Am Acad Child Adolesc Psychiatry. 2010;49:1189–201. doi: 10.1016/j.jaac.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Linos E, Willett WC, Cho E. Red meat consumption during adolescence among premenopausal women and risk of breast cancer. Cancer Epidemiol Biomarkers Prev. 2008;17:2146–51. doi: 10.1158/1055-9965.EPI-08-0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Biro FM, Deardorff J. Identifying opportunities for cancer prevention during preadolescence and adolescence: Puberty as a window of susceptibility. J Adolesc Health. 2013;52:S15–20. doi: 10.1016/j.jadohealth.2012.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010;91(Suppl):1499S–505S. doi: 10.3945/ajcn.2010.28701B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fuemmeler BF, Pendzich MK, Tercyak KP. Weight, dietary behavior, and physical activity in childhood and adolescence: Implications for adult cancer risk. Obes Facts. 2009;3:179–86. doi: 10.1159/000220605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Cancer Research Fund/American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: A global perspective. Washington DC: AICR; 2007. [Google Scholar]
- 28.U.S. Department of Health and Human Services. How tobacco smoke causes disease: The biology and behavioral basis for smoking-attributable disease: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [PubMed] [Google Scholar]
- 29.World Health Organization. International Agency for Research on Cancer. Exposure to artificial UV radiation and skin cancer. Lyon: France; 2006. [Google Scholar]
- 30.World Health Organization. International Agency for Research on Cancer. Solar and ultraviolet radiation. Vol. 55. Lyon, France; 1992. IARC monographs on the evaluation of carcinogenic risks to humans. [Google Scholar]
- 31.World Health Organization. International Agency for Research on Cancer. Human papillomaviruses. Vol. 90. Lyon, France; 2007. IARC monographs on the evaluation of carcinogenic risks to humans. [Google Scholar]
- 32.Santelli JS. Adolescent risk taking, cancer risk and lifecourse approaches to prevention. J Adolesc Health. 2013;52(suppl 5):S41–4. doi: 10.1016/j.jadohealth.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 33.Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health: National findings. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration; 2009. Available at: http://www.oas.samhsa.gov/nsduh/2k8nsduh/2k8results.pdf. [Google Scholar]
- 34.Karagas MR, Weinstock MA, Nelson HH. Keratinocyte carcinomas (basal and squamous cell carcinomas of the skin) In: Schottenfeld D, Fraumeni JF, editors. Cancer Epidemiology and Prevention. 3rd. New York: Oxford University Press; 2006. pp. 1230–50. [Google Scholar]
- 35.Bushkin-Bedient S, Carpenter DO. Exposure to chemicals and radiation during childhood and risk for cancer later in life. J Adolesc Health. 2013;52(suppl 5):S21–9. doi: 10.1016/j.jadohealth.2013.01.027. [DOI] [PubMed] [Google Scholar]
- 36.Grun F, Blumberg B. Endocrine disruptors as obesogens. Mol Cell Endocrin. 2009;304:19–29. doi: 10.1016/j.mce.2009.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention (CDC) Fourth National Report on Human Exposure to Environmental Chemicals. Atlanta, GA: CDC; 2009. Available at: http://www.cdc.gov/exposurereport/pdf/FourthReport.pdf. [Google Scholar]
- 38.Brenner DJ, Elliston CD, Hall EJ, Berdon WE. Estimated risks of radiation induced fatal cancer from pediatric CT. Am J Roentgenol. 2001;176:289–96. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 39.Alliance for Radiation Safety in Pediatric Imaging. Image Gently campaign. Available at: http://www.pedrad.org/associations/5364/ig/
- 40.Cost NG, Applegate KE. Image Gently: A campaign to reduce children's and adolescents' risk for cancer during adulthood. J Adolesc Health. 2013;52(suppl 5):S93–7. doi: 10.1016/j.jadohealth.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 41.Morse LL. Let schools do it! Helping schools find a role in cancer prevention. J Adolesc Health. 2013;52(suppl 5):S89–92. doi: 10.1016/j.jadohealth.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention (CDC) School Health Profiles 2010. Atlanta, GA: CDC; 2011. Available at: http://www.cdc.gov/HealthyYouth/profiles/ [Google Scholar]
- 43.Joint Committee on National Health Education Standards. National Health Education Standards. 2nd. Atlanta, GA: American Cancer Society; 2007. [Google Scholar]
- 44.Chaloupka FJ, Straif K, Leon ME. Effectiveness of tax and price policies in tobacco control. Tob Control. 2011;20:235–8. doi: 10.1136/tc.2010.039982. [DOI] [PubMed] [Google Scholar]
- 45.Friend KB, Lipperman-Kreda S, Grube J. The impact of local US tobacco policies on youth tobacco use: A critical review. Open J Prev Med. 2011;1:34–43. doi: 10.4236/ojpm.2011.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Siegel M, Albers AB, Cheng DM, et al. Effects of local restaurant smoking regulations on progression to established smoking among youths. Tobacco Control. 2005;14:300–6. doi: 10.1136/tc.2005.012302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Terry-McElrath YM, Wakefield MA, Emery S, et al. State anti-tobacco advertising and smoking outcomes by gender and race/ethnicity. Ethnicity Health. 2007;12:339–62. doi: 10.1080/13557850701300723. [DOI] [PubMed] [Google Scholar]
- 48.Tworek C, Yamaguchi R, Kloska DD, et al. State-level tobacco control policies and youth smoking cessation measures. Health Pol. 2010;97:136–44. doi: 10.1016/j.healthpol.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brownell KD, Farley T, Willett WC, et al. The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med. 2009;361:1599–605. doi: 10.1056/NEJMhpr0905723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wagenaar AC, Salois MJ, Komro KA. Effects of beverage alcohol price and tax levels on drinking: A meta-analysis of 1003 estimates from 112 studies. Addiction. 2009;104:179–90. doi: 10.1111/j.1360-0443.2008.02438.x. [DOI] [PubMed] [Google Scholar]
- 51.Graham H. Building an inter-disciplinary science of health inequalities: The example of lifecourse research. Soc Sci Med. 2002;55:2005–16. doi: 10.1016/s0277-9536(01)00343-4. [DOI] [PubMed] [Google Scholar]
- 52.Graham H, Power C. Childhood disadvantage and adult health: A life-course framework. London, UK: Health Development Agency; 2004. Available at: http://www.gserve.nice.org.uk/niceMedia/pdf/childhood_disadvantage_health.pdf. [Google Scholar]
- 53.Krieger N, Chen JT, Waterman PD, et al. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: The public health disparities geocoding project. Am J Public Health. 2005;95:312–23. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ellis BJ, Shirtcliff EA, Boyce WT, et al. Quality of early family relationships and the timing and tempo of puberty: Effects depend on biological sensitivity to context. Dev Psychopathol. 2011;23:85–99. doi: 10.1017/S0954579410000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Strunin L, Wulach L, Yang GJ, et al. Preventing cancer: A community-based program for youths in public housing. J Adolesc Health. 2013;52(suppl 5):S83–8. doi: 10.1016/j.jadohealth.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 56.Morales-Campos DY, Markham C, Peskin MF, Fernandez ME. Hispanic mothers' and high school girls' perceptions of cervical cancer, human papilloma virus, and the human papilloma virus vaccine. J Adolesc Health. 2013;52(suppl 5):S69–75. doi: 10.1016/j.jadohealth.2012.09.020. [DOI] [PubMed] [Google Scholar]
- 57.Thomas TL, Strickland O, Diclemente R, Higgins M. An opportunity for cancer prevention during preadolescence and adolescence: Stopping human papillomavirus (HPV)-related cancer through HPV vaccination. J Adolesc Health. 2013;52(suppl 5):S60–8. doi: 10.1016/j.jadohealth.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gehlert S. Turning disciplinary knowledge into solutions. J Adolesc Health. 2013;52(suppl 5):S98–102. doi: 10.1016/j.jadohealth.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gehlert S, Sohmer D, Sacks T, et al. Targeting health disparities: A model linking upstream determinants to downstream interventions. Health Aff. 2008;27:339–49. doi: 10.1377/hlthaff.27.2.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mahabir S, Aagaard K, Anderson LM, et al. Challenges and opportunities in research on early-life events/exposures and cancer development later in life. Cancer Causes Control. 2012;23:983–90. doi: 10.1007/s10552-012-9962-5. [DOI] [PubMed] [Google Scholar]
- 61.Centers for Disease Control and Prevention. Research Data Centers. Available at: http://www.cdc.gov/rdc/index.htm.


