Abstract
Past studies have shown successful outcomes regarding the use of various interventional education methods in improving patient compliance. At our institution, different educational resources are offered and encouraged, including a 2-hour–long educational class, to prepare patients who are undergoing total joint arthroplasty procedures. Given the significant impact that patient compliance with preoperative instruction can have on overall outcomes of these procedures, this study was intended to assess the effects that the educational classes can have on patient compliance with this institution’s 6-point preoperative total joint arthroplasty protocol. The study analyzed 2 groups, those who did and did not attend the preoperative classes, and compliance rates were compared between the 2. It was hypothesized that patients who did attend the classes would be more compliant to the protocol compared to those who did not. Although results from the study showed that there were no significant differences in adherence between the 2 groups, future quality assessment studies can build off this in order to move toward achieving optimal patient compliance with preoperative instructions.
Keywords: adult reconstructive surgery, physical medicine and rehabilitation, geriatric medicine, systems of care, physical therapy
Introduction
Optimal patient outcomes after total joint arthroplasty rely heavily on the cooperative efforts by patients, just as it does on the performance of the medical team. Without the proper patient education and adherence to different perioperative instruction, ideal care may not be achieved and outcomes of surgery may be compromised. Some factors measuring outcome that may be affected include length of hospitalization, postoperative pain management, patient recovery, and quality of life, among other factors. The preoperative stage is particularly important in that growing evidence supports that simple measures taken during this time, that is, patient education, patient adherence to preoperative treatments, physical therapy, and nutrition, directly result in better patient postoperative outcomes.1–3 A meta-analysis of 13 randomized clinical trials showed that the use of preoperative nonsteroidal anti-inflammatory drugs (NSAIDs) as an adjunct in a multimodal regimen decreased early postoperative pain, opioid-sparing effects, nausea, vomiting, and pruritus in patients undergoing total joint arthroplasty.4 Similarly, other studies investigating the use of NSAIDs in preoperative pain management programs found that hospital stay was shortened and the likelihood of discharge to a skilled nursing facility was decreased.5–7
Given the importance of patient adherence during the preoperative stage, it is important to look into the different factors that can potentially improve compliance rates to a preoperative treatment protocol. One possible method to improving adherence to preoperative instructions is the provision of adequate patient educational resources on the topic of a patient’s illness, treatments, and rehabilitation plans whether it be through educational classes, pamphlets, digital media, consults with physicians, or visual aids. Past studies have shown favorable results regarding the relationship between educational intervention and improved patient compliance. In a study comparing the compliance between patients with rheumatoid arthritis who did and did not receive monthly patient education, Hill et al found that 85% of the education group compared to 55% of the control group remained compliant.8 In another related study by Peveler et al, a difference of 63% to 39% in patients with depression who received and did not received counseling, respectively, complied with their tricyclic medications.9 Cuddihy et al found that successful osteoporosis intervention increased from 16% to 45% in patients with forearm fractures after the implementation of an educational program.10
Patient adherence to a preoperative medication protocol is not exactly the same as long-term medication regimens mentioned in the studies described earlier. One major difference includes a larger window of opportunity for medical services to intervene with patients undergoing long-term medication treatment versus in patients who are given a 1-time preoperative regimen. However, this is not to say that a lot cannot be learned from the success of these previous studies and that similar results can be met in regard to adherence.
After extensive review of the literature, there is minimal to no evidence of past investigations into how educational resources can specifically affect patient adherence to a preoperative protocol. Thus, the goal of our report is to look into how a total joint arthroplasty educational class affects compliance rates to the established 6-point preoperative protocol at a university-based medical center. Our hypothesis is that attendance at a preoperative educational class would increase patient compliance with preoperative instructions. By improving our understanding of this relationship, a better assessment of the quality of the educational resources used to prepare patients for surgery can be made.
Materials and Methods
Design and Patients
This study was approved by our institutional review board as well as being part of a quality improvement initiative. Our study was a retrospective analysis of prospectively collected data of a consecutive cohort of patients, as part of a quality control initiative, undergoing total hip and total knee arthroplasty at a university-based medical center. We specifically looked into 2 groups of patients, those who attended the offered preoperative educational classes and those who did not. Attendance was analyzed by reviewing the class attendance roster, which was taken at the beginning of each class. These classes were nonmandatory sessions taught by the orthopedic department’s nurse manager and physical therapist but were highly encouraged to attend. The class agenda outlined a short book detailing what would happen before, during, and after surgery. It also reviewed different ways for patients to prepare during the days preceding the surgery, including reminders to carry out the preoperative treatment regimens and what the recovery process would look like. Finally, the instructors reviewed the exercises the patients were scheduled to do after surgery and encouraged patients to begin practicing the exercises before the actual date of the surgery. The class followed a developed script, thus to make sure it is the same every time and that no portions are missed. The class included a review and reminder of the preoperative protocol. The classes were offered every first and third Monday every month and lasted for 2 hours. As part of our preoperative evaluation and preparation prior to surgery, all patients attended a preoperative clinic visit where they were evaluated by a nurse practitioner (NP). During this clinic visit, the NP reviewed the preoperative protocol, and patients received an educational booklet, and were referred to our Web site where a digital copy of the booklet as well as other educational material is available.
We examined patient adherence rates to the preoperative protocol between those who did and did not attend the educational classes. Patient adherence to the protocol was measured using a “yes” or “no” 6-question questionnaire regarding the 6 points of the protocol. A registered nurse administered the questionnaire on the day of the surgery. The preoperative protocol included warfarin to be taken the night before surgery, celecoxib to be taken for 2 consecutive nights before surgery, nasal mupirocin application twice a day for 5 days before surgery (if needed for preoperative decolonization of a positive culture of methicillin-resistant Staphylococcus aureus or methicillin-sensitive S aureus in the nares), chlorhexidine body wash for 3 consecutive days before surgery, abstaining from shaving the surgical site, and abstaining from marking the surgical site before arrival the day of the surgery.
The inclusion criteria consisted of patients who were undergoing total knee or hip joint arthroplasty and were part of the total joint replacement surgical home prior to surgery (ie, were given instructions on the protocol during a structured preoperative visit). Those who did not meet the criteria included patients who were not part of the joint replacement surgical home project (eg, emergency department admissions, patients with cancer, and inpatient consults).
Statistical Analysis
Patient adherence rates were measured using simple percentages and averages of the data collected from the questionnaires. These values were calculated for each treatment of the 6-point preoperative protocol. The statistical significance of adherence rates based on whether patients attended the educational class was calculated using Fisher exact test. A logistic regression model was used to calculate odds ratios of likelihood to be adherent based on the number of days in between attendance of the educational class and date of surgery.
Results
In the cohort, there were a total of 244 patients who met the inclusion criteria, 88 males and 156 females. The average age of the patients was 63.7 years old (range of 19-93 years). Prior to surgery, 212 patients took their Coumadin medication, which resulted in an 86.9% adherence rate. Two hundred patients adhered to their Celebrex medications, which resulted in an 81.2% compliance rate. Of the 52 patients who were prescribed Mupirocin, 46 were adherent, resulting in an 88.5% compliance rate. Of the 244 patients, 240 adhered to Chlorhexidine treatment, which showed a 98.4% adherence rate. Of the patients, 90.2% and 99.2% were adherent to shave and marking instruction prior to surgery, respectively.
Of the 244 patients involved, 104 attended the class and 140 did not, which showed an attendance rate of 42.6%. When we examined demographic characteristics between patients who attended class (average age 64.33 years and 35% male) and patients who did not attend class (average age 63.54 years and 36% male), no statistical significance was observed between patient gender and class attendance (P = 1) as well as no relationship between increasing age and increased likeliness to attend class. The following adherence averages were found for each drug based on whether patients attended or didn’t attend a class, respectively: Coumadin, 85.6% to 87.9%; Celebrex, 81.7% to 82.1%; Mupirocin, 87.0% to 90.0%; Chlorhexidine, 99.0% to 97.9%; Shave, 88.5% to 91.4%; and Mark, 99.0% to 99.3% (Figure 1).
Figure 1.
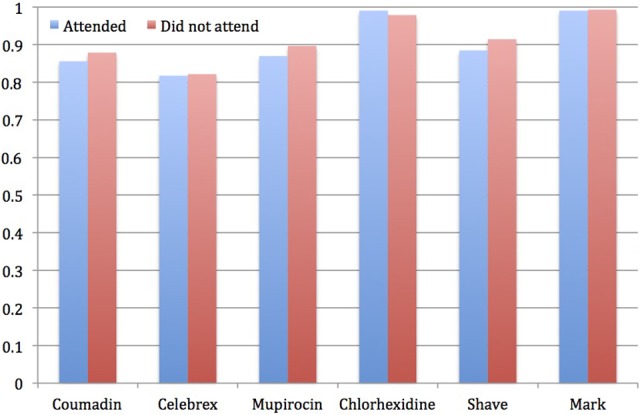
Compliance based on class attendance.
A Fisher exact test of the 2 groups’ adherence rates based on attendance to the educational class did not reveal any statistical difference between the groups for any of the medications. This indicated that attending the educational class did not have a statistically significant effect on patient compliance rates (Table 1).
Table 1.
Patient Compliance With Preoperative Treatment Protocol Based on Patient Class Attendance.a
| Medication | Odds Ratio | Confidence Interval | P Value |
|---|---|---|---|
| Warfarin | 0.772 | 0.364-1.643 | .314 |
| Celecoxib | 0.934 | 0.481-1.814 | .485 |
| Mupirocin | 0.769 | 0.140-4.224 | .547 |
| Chlorhexidine | 2.256 | 0.231-21.998 | .430 |
| Site shave | 0.719 | 0.309-1.671 | .289 |
| Site mark | 0.741 | 0.046-11.987 | .672 |
a P values were based on Fisher exact test.
A logistic regression model analyzing whether patient adherence rates to any of the protocol points correlated with the increasing amount of days between class attendance and surgery date did not show any statistical significance (Table 2).
Table 2.
Logistic Regression Model Based on Days Between Patient Educational Class and Surgery Day.
| Medication | Odds Ratio | Confidence Interval | P Value |
|---|---|---|---|
| Warfarin | 1.007 | 0.944-1.073 | .841 |
| Celecoxib | 1.010 | 0.954-1.069 | .739 |
| Mupirocin | 1.037 | 0.890-1.208 | .628 |
| Chlorhexidine | 1.061 | 0.847-1.329 | .573 |
| Site shave | 1.003 | 0.947-1.062 | .927 |
| Site mark | 1.147 | 0.954-1.379 | .107 |
Discussion
One of the goals of a clinical pathway is to standardize surgical education to patients in order to reduce confusion or conflict from the preoperative to the operative and to the postoperative outpatient stages.11–13 Not only is the standardization of care essential, but also understanding the most effective modes of patient education is just as important. This report was a step in that direction by assessing whether the attendance of an optional preoperative educational class had an effect on patient adherence to a preoperative treatment protocol. In this work, it was found that when comparing the two groups of patients who did and did not attend the educational class, attending the class did not have any effect on patient adherence rates to the preoperative treatment protocol. Our results showed that adherence to each of the 6 treatments in the 6-point protocol was found to be similar between both the groups. Further analysis of the data also indicated that there was no correlation between adherence levels to any of the 6 treatments in regard to increasing number of days between class attendance and the date of surgery.
Other similar studies in the literature have shown varying results regarding the relationship between educational intervention and patient compliance. Cuddihy et al found an increase of successful osteoporosis intervention from 16% to 45% in patients after the implementation of an educational program.10 The program included educational materials on osteoporosis and consultation with a primary care physician. Peveler et al found a 39% to 63% increase in medication compliance in patients with depression who received counseling throughout their course of treatment.9 The counseling courses included educational resources and advice that covered the importance of drug treatment, its potential side effects, the need for treatment continuation for up to 6 months, and the use of reminders and cues for therapy. In a study by Hill et al, a difference of 85% and 55% was observed between patients with rheumatoid arthritis who did and did not receive monthly patient education through regular appointments, respectively.8 The educational appointments consisted of monthly 30-minute sessions with nurse practitioners and covered topics including the types of medication used for rheumatoid arthritis, the disease process, physical exercise, joint protection, pain control, and coping strategies. In a past study specifically looking into the utility of written and audio educational materials, without any other intervention by a health care provider, there was a small, but significant, evidence found suggesting improved compliance. The study by Schaffer and Tian investigated patients with asthma who were randomly assigned to an experimental educational audiotape, a standard asthma management booklet, both tape and written material, or no intervention. Compliance increased from 15% to 19% in all 3 experimental groups and decreased by 22% in the nonintervention group.14 Although all these studies dealt with long-term medication regimens, which contrasted from our short-course protocol, parallels can be drawn from these success stories and could potentially be used as a model to improve compliance rates.
In addition to the possibility of looking at other institutions’ intervention models, improved compliance rates may possibly be achieved by evaluating the utility of educational resources used at our institution. Currently, patient attendance to educational classes is not mandatory as it is at some other institutions. Instead, it is recognized that people learn best through different modes whether it be group classes or more individual styles of learning such as reading papers or watching educational videos, both of which are equally encouraged. As a quality assessment measure and attempt to determine which educational resources are indeed the most effective, it may be beneficial to carry out future prospective studies, looking into the efficacy of the other educational options offered.
These data were part of a quality improvement initiative to increase patient attendance with a preoperative educational class and assess patient compliance with preoperative treatment protocol. However, the work did encounter some limitations. It did not control for any other educational resources outside class attendance that the patient may have utilized. These resources may have come in the form of extra reading material or educational videos and other online resources that were offered by the joint replacement service and may have influenced how likely patients were to follow protocol instructions. Also, one surgeon performed all of the surgeries included in this study. In normal health care settings, differences in education styles between surgeons and care providers may influence the adherence of patients in ways that this work did not account for. The patients themselves could have introduced another source of bias, by reporting a higher rate of compliance than what was actually true in order to impress or seem compliant in the eyes of the surgical team. Finally, we did not consider the possibility of patients who had previous experiences undergoing a total joint arthroplasty. Prior experience with this procedure could potentially have affected their likeliness to adhere to the protocol as well as their decision to attend the educational class.
In conclusion, we found that there seems to be no correlation between educational class attendance and adherence rates to the total joint arthroplasty preoperative treatment protocol. Based on other similar studies, it is reasonable to believe that educational intervention can potentially improve patient adherence rates. However, pinpointing which modifications need to be made to the established patient educational resources, in order to increase patient attendance in the educational class and adherence to preoperative treatment protocol, still needs to be determined. At the same time, considering the relatively high baseline adherence rates measured for both groups, the possibility that an increase in adherence rates not having any measurable clinical significance should also be considered.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Berend KR, Lombardi AV, Mallory TH. Rapid recovery protocol for peri-operative care of total hip and total knee arthroplasty patients. Surg Technol Int. 2004;13:239–247. [PubMed] [Google Scholar]
- 2. Hansen TB, Bredtoft HK, Larsen K. Preoperative physical optimization in fast-track hip and knee arthroplasty. Dan Med J. 2012;59(2):A4381. [PubMed] [Google Scholar]
- 3. Parker MJ, Gurusamy K, Stoker M. Surgery in elderly patients. Curr Orthop. 2004;18(5):333–344. [Google Scholar]
- 4. De Oliveira GS, Jr, Agarwal D, Benzon HT. Perioperative single dose ketorolac to prevent postoperative pain: a meta-analysis of randomized trials. Anesth Analg. 2012;114(2):424–433. [DOI] [PubMed] [Google Scholar]
- 5. Bergeron SG, Kardash KJ, Huk OL, Zukor DJ, Antoniou J. Perioperative Dexamethasone does not affect functional outcome in total hip arthroplasty. Clin Orthop Relat Res. 2009;467(6):1463–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Buvanendran A, Kroin JS, Tuman KJ, et al. Effects of perioperative administration of a selective cyclooxygenase 2 inhibitor on pain management and recovery of function after knee replacement: a randomized controlled trial. J Amer Med Assoc. 2003;290(18):2411–2418. [DOI] [PubMed] [Google Scholar]
- 7. Duellman TJ, Gaffigan C, Milbrandt JC, Allan DG. Multi-modal, pre-emptive analgesia decreases the length of hospital stay following total joint arthroplasty. Orthopedics. 2009;32(3):167. [PubMed] [Google Scholar]
- 8. Hill J, Bird H, Johnson S. Effect of patient education on adherence to drug treatment for rheumatoid arthritis: a randomized controlled trial. Ann Rheum Dis. 2001;60(9):869–875. [PMC free article] [PubMed] [Google Scholar]
- 9. Peveler R, George C, Kinmonth AL, Campbell M, Thompson C. Effect of antidepressant drug counseling and information leaflets on adherence to drug treatment in primary care: randomized controlled trial. Brit Med J. 1999;319(7210):612–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cuddihy MT, Amadio PC, Gabriel SE, Pankratz VS, Kurland RL, Melton LJ., III A prospective clinical practice intervention to improve osteoporosis management following distal forearm fracture. Osteoporosis Int. 2004;15(9):695–700. [DOI] [PubMed] [Google Scholar]
- 11. Raphael DR, Cannesson M, Schwarzkopf R, et al. Total joint perioperative surgical home: an observational financial review. Perioper Med (Lond). 2014;3:6 doi:10.1186/2047-0525-3-6. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Garson L, Schwarzkopf R, Vakharia S, et al. Implementation of a total joint replacement-focused perioperative surgical home: a management case report. Anesth Analg. 2014;118(5):1081–1089. doi:10.1213/ANE.0000000000000191. [DOI] [PubMed] [Google Scholar]
- 13. Kain ZN, Vakharia S, Garson L, et al. The perioperative surgical home as a future perioperative practice model. Anesth Analg. 2014;118(5):1126–1130. Copyright: © 2014 International Anesthesia Research Society [DOI] [PubMed] [Google Scholar]
- 14. Schaffer SD, Tian L. Promoting adherence: effects of theory-based asthma education. Clin Nurs Res. 2004;13(1):69–89. [DOI] [PubMed] [Google Scholar]


