Abstract
Introduction:
Femoral neck fractures in elderly patients result in significant reduction in mobility. Deconditioning takes place quickly without early ambulation postsurgery. A recent Cochrane review found inconclusive evidence on the rehabilitation protocol required to effectively restore patients’ prefracture mobility status. This study was conducted to determine the effects of different rehabilitation approaches on the functional and mobility outcomes of elderly patients after hip hemiarthroplasty for femoral neck fractures.
Materials and Methods:
We enrolled consecutive patients aged >65 years, admitted into a tertiary orthopedic unit from January to December 2010, who had undergone hip hemiarthroplasty. They were divided into 3 cohorts: (a) home with outpatient rehabilitation, (b) intensive short rehabilitation, and (c) extended slow-stream rehabilitation. Clinical variables were collected along with outcome variables of Modified Harris Hip Score, Parker Mobility Score (PMS), and the return to near premorbid ambulatory status at 1 year (PMS decrease of ≤2).
Results:
A total of 133 patients were recruited and followed up for a year. The 3 cohorts were found to be comparable for prefall cardiovascular diseases, PMS, and Katz Index, although it was found that in the slow-stream cohort, there was a greater percentage of patients with previous cerebrovascular accidents. Patients in the intensive short rehabilitation cohort were found to have a higher proportion of patients returning to prefracture mobility, with the odds ratio of 2.3478 (95% confidence interval: 1.0667 to 5.1674; P = .042) after multivariate analysis.
Conclusions:
Elderly patients >65 years who had undergone hemiarthroplasty would likely benefit most from an intensive inpatient rehabilitation program.
Keywords: fragility hip fractures, osteoporosis, hemiarthroplasty, rehabilitation, ambulatory status
Introduction
Hip fractures in elderly patients pose a complex clinical problem, which can have a potentially devastating impact on the ability of the elderly patient remaining independent. Currently, about 1 in 3 who survive a hip fracture return to their previous level of independence, 50% require long-term help with routine activities and cannot walk unaided and 25% require full-time nursing home care.1
Early ambulation accelerates functional recovery and is associated with more discharges home and less discharges to high-level care in previously community-dwelling individuals.2 No particular mobilization strategies have been proven to be superior over others, but studies have shown that weight-bearing home exercises improve balance and functional ability among older people who have completed usual care after a hip fracture.3
A coordinated multidisciplinary rehabilitation program with the specific aim of regaining sufficient function to return to their prefracture living arrangements has been the thrust of the hip fracture programs in our institution. Early multidisciplinary daily geriatric care reduces in-hospital mortality and medical complications in older patients with hip fracture but has not been shown to reduce length of stay or functional recovery.4,5 Previous studies have shown that accelerated discharge and home-based rehabilitation is associated with functional improvement, greater confidence in avoiding subsequent falls, improvements in health-related quality of life, and less caregiver burden.6
Figure 1.

Radiographs of a Patient with Femoral Neck Fracture treated with Hemiarthroplasty.
In our institution, the patients are assessed clinically on their degree of independence and fall risks, taking into considerations the need, availability, and competence of the caregiver before being assigned to the various rehabilitation programs. A large majority of our patients are discharged to inpatient rehabilitative facilities. This study was conducted to determine the effects of the different rehabilitation approaches on functional and mobility outcomes of elderly patients after hip hemiarthroplasty for femoral neck fractures.
Materials and Methods
Study Design
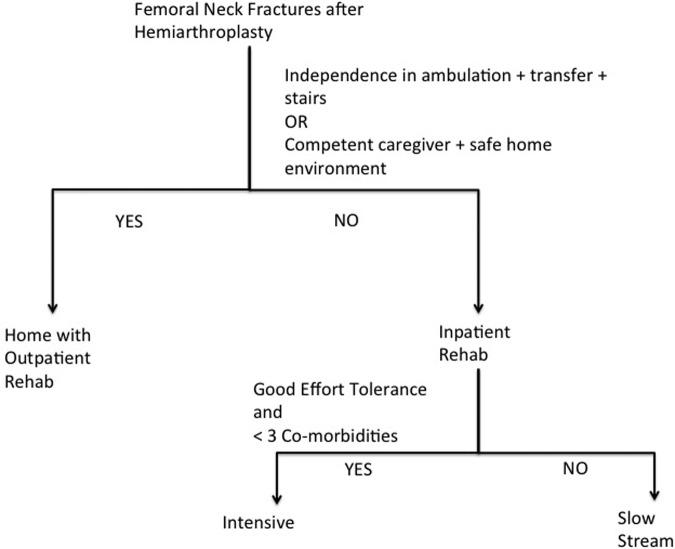
We carried out a prospective cohort study of consecutive patients equal to or more than 65 years old who underwent hip hemiarthroplasty at a tertiary orthopedic unit from January to December 2010. They were divided into 3 groups based on their discharge destination: (1) home with outpatient rehabilitation, (2) short intensive subacute rehabilitation (<3weeks), and (3) extended slow-stream subacute rehabilitation (4-8 weeks). The subacute programs are all within ward-based inpatient facilities known as community hospitals. Prescription of the different rehabilitation programs was made according to the protocol shown in Figure 2.
Figure 2.
Protocol of selection criteria for rehabilitation program.
Patient Selection
All patients were followed up for a year and clinical variables and outcomes were assessed and compared between the cohorts. Patients were excluded if they had the following criteria: (1) Mortality within 1 year from the date of surgery, (2) pathological fractures, (3) premorbid nonambulant mobility status, (4) inability to perform assisted standing at bedside predischarge, (5) cognitive impairment, or (6) concurrent acute fractures affecting ambulation and rehabilitation.
Data Collection
Data were collected from the medical records of the study population for variables that may impact upon ambulatory outcomes. These included age, race, American Society of Anesthesiologists (ASA) score, previous event affecting prefracture mobility, Katz Index, route of anesthesia, cemented/uncemented techniques, total duration of nonambulation after fall, quality of ambulation on postoperative day (POD) 1 as well as postoperative anterior thigh pain. The variables were evaluated against outcome measures such as the Modified Harris Hip Score (MHHS) and Parker Mobility Score (PMS) at 3 months, 6 months, and 1 year after surgery as well as the change in PMS from prefracture to 1 year postsurgery. One team member collected the functional and mobility data through a telephone interview and another team member, both blinded to either side, collected the variables through a review of existing medical records.
Statistical Analysis
The 3 groups were analyzed to identify variables that were significantly different between them. Multivariate regression analysis was done to examine the relationship between the outcomes and the variables identified. Categorical variables are presented as numbers and compared using Fisher exact test. Continuous variables are presented using the median (± standard deviation), utilizing the Kruskal Wallis test—the null hypothesis being that there were no associations between the tested variable and PMS, MHHS, or change in PMS scores. Statistical significance was assumed if P < .05.
Results
A total of 191 consecutive patients were eligible for inclusion into the study. The total number of recruited study participants comprised 133 patients, of which 109 were females and 24 were males. Of the excluded 58 patients, 39 died within 1 year of operation, 6 patients declined participation, and 13 patients were ineligible according to the exclusion criteria. The 3 cohorts are shown in Table 1. The cohorts were comparable based on prefracture PMS and Katz Index. With regard to comorbidities, there were a higher percentage of patients within the slow-stream rehabilitation group with old cerebrovascular accidents (CVAs), but the groups did not show statistical significant differences for cardiovascular (CVS) disease. Mean age and ASA scores were slightly higher in the slow-stream rehabilitation group.
Table 1.
Comparison of the 3 Cohorts.
| Total (N = 133) | Home with outpatient rehab (n = 18) | Intensive short rehab (n = 39) | Extended slow-stream rehab (n = 76) | P values |
|---|---|---|---|---|
| Age, mean ± SD | 75.06 ± 8.171 | 73.41 ± 5.816 | 79.89 ± 7.905 | <.001 |
| ASA, mean ± SD | 2.33 ± 0.485 | 2.26 ± 0.498 | 2.55 ± 0.526 | .011 |
| Significant CVS disease, n (%) | 3(16.7) | 4(10.3) | 18(23.7) | .212 |
| Old CVA, n (%) | 2(11.1) | 3(7.7) | 21(27.6) | .024 |
| Katz Index, mean ± SD | 5.33 ± 1.572 | 5.9 ± 1.021 | 5.41 ± 1.568 | .181 |
| Pre-Fall PMS, mean ± SD | 7.83 ± 2.007 | 8.38 ± 1.388 | 7.59 ± 1.805 | .069 |
Abbreviations: ASA, American Society of Anesthesiologists; CVA, cerebrovascular accident; CVS, cardiovascular; PMS, Parker Mobility Score; SD, standard deviation.
The outcomes of PMS and MHHS measured at 3, 6, and 12 months are shown in Table 2. The proportion of patients who returned to near prefracture mobility at 1-year follow-up was significantly highest in the group with short intensive rehabilitation, with the odds ratio of 2.3478 (95% confidence interval [CI]: 1.0667-5.1674; P =0.042) after multivariate analysis. The median PMS and MHHS scores at the 3 time intervals were significantly better for the cohort that received the short intensive program compared to the other 2 cohorts.
Table 2.
Outcome Measures.
| Home with outpatient rehab | Intensive short rehab | Extended slow-stream rehab | P value | |
|---|---|---|---|---|
| Decrease in Parker mobility scores <2, n (%) | ||||
| Yes | 8 (47.06) | 30 (77.5) | 43 (57.33) | .042a |
| No | 10 (52.94) | 9 (22.5) | 33 (42.67) | |
| Parker mobility score, median (SD) | ||||
| 3 months | 4 (1) | 4.5 (2) | 4 (2) | .0353b |
| 6 months | 5 (2) | 6 (1) | 4 (2) | .0009b |
| 1 year | 5 (1) | 6 (1) | 5 (3) | .0015b |
| Modified Harris Hip Score, median (SD) | ||||
| 3 months | 70 (12) | 72.5 (17) | 67 (19) | .0076b |
| 6 months | 78 (12) | 77.5 (14.5) | 69 (19) | .0009b |
| 1 year | 77 (12) | 80 (17.5) | 70 (19) | .0018b |
Abbreviations: rehab, rehabilitation; SD, standard deviation.
a Fischer Exact test.
b Kruskal Wallis test.
Comparing the patients who received only outpatient rehabilitation with those who received the extended slow-stream program, the former was found to have better functional outcomes. On the other hand, a greater proportion of the patients who received the extended slow-stream program had a return to near prefracture PMS compared to the patients with only outpatient rehabilitation as shown in Table 2.
The above-mentioned results were further analyzed and age, ASA scores, comorbidities, previous event affecting prefracture mobility, time to surgery, type of anesthesia, duration of operation, cemented/uncemented techniques, blood loss, blood transfusion, duration of nonambulation, quality of ambulation on POD 1, anterior thigh/hip pain, and full-time caregiver were found to not significantly affect the ambulatory outcomes measured in Table 2. However, our analysis found that for patients readmitted within 1 month (2 due to pneumonia, 1 due to deep implant infection, and 2 for other comorbidities), they recorded poorer outcome scores measured with PMS at 6 months by 1.95 (95% CI: −2.91 to −0.98; P < .001) and at 1 year by 3.78 (95% CI: −2.89 to −0.89; P < .001).
We investigated further to assess whether previous CVA or significant CVS disease predicted poorer outcomes among those who received the extended slow-stream rehabilitation program. Of those with previous CVA, 42.86% did not have a near return to prefracture mobility compared to the 21.42% in the patients without (P = .0848). Similar findings were noted for CVS disease. 54.54%of those who had significant CVS diseases did not have a near return to prefracture mobility, compared to the 20.01% in those without significant CVS diseases (P = .1717). Although the differences in the proportions compared were not statistically significant, the results for the group with previous CVA were noted by the authors to be approaching significance.
Discussion
It has been established that rehabilitation improves ambulatory outcomes, confidence in avoiding subsequent falls, and health-related quality of life and reduces caregiver burden.2,6,7 However, rehabilitation ranges from subacute ward-based programs to home-based programs. Cultural and social factors have also influenced the use of rehabilitation facilities beyond what was initially intended. Functional independence of elderly individuals after femoral neck fractures is inversely proportional to the socioeconomic costs incurred, hence the need to determine which rehabilitation strategy is most effective in returning mobility to prefall levels.18,19
Previous studies have shown that muscle strength, Katz Index, in-hospital complications, and discharge destinations affect gait ability and quality in one way or another.7,8 Perioperative strategies to improve outcomes have been optimized through multidisciplinary orthogeriatric teams. Postoperative measures in improving ambulatory outcomes consist of outpatient rehabilitation, intensive short inpatient rehabilitation, and extended slow-stream inpatient rehabilitation.9–11 The purported belief that the elderly patients require long rehabilitation programs to improve functional and mobility status may not be true. An increased level of physical activity is needed to prevent the decline in strength gained early in rehabilitation. The overall increased level of physical activity upon returning home encourages one to relearn independent functioning without the supervision of health care workers round the clock.12,13 A short intensive inpatient rehabilitation may be the better solution compared to prolonged subacute care. Notwithstanding the above, certain groups of elderly patients should be identified to receive longer programs if required.
In the 2011 Cochrane Review,14 the authors concluded that there is insufficient evidence to determine the effects of any particular mobilization strategy or program, whether it is in the early or later rehabilitation periods after hip fracture surgery. While the most successful programs evaluated to date have involved supervised ongoing exercises, the optimal format and resource implications for these strategies have not been established.15 The length and intensity of the rehabilitation programs in subacute facilities should be tailored to maximize functional and mobility outcomes in the elderly patients.
Our study team followed up the 3 cohorts with comparable prefracture PMS and Katz Index for 1 year, and it was revealed that the short intensive program cohort achieved the best ambulatory outcomes. This was reflected in the mobility scores measured, supporting the opinion that short intensive rehabilitation allows the patients to be restored to prefracture mobility levels better than leaving these patients without any ward-based program or having an extended program that incurs high socioeconomic costs. Similar to previous findings,2,7 the short-term supervised exercises likely improved mobility outcomes of the elderly patients through the targeted approach of a formal program. It is also known that ward-based programs for an extended period breed dependence through the prolonged lack of an environment that promotes functional independence, explaining the poorer results seen in the mobility outcomes of the extended program.
Among the patients within the extended slow-stream program, patients with a previous CVA had lower proportions of a return to near premorbid mobility, and this was noted to be approaching statistical significance. This finding coupled with the earlier results could be utilized to guide rehabilitation pathways. Multidisciplinary teams in charge of rehabilitation dispositions could consider those patients with good or moderate effort tolerance and more than 3 comorbidities but have no history of CVAs for a short intensive program. This could possibly improve mobility outcomes.
Our study results are limited to the short follow-up period of 1 year, with longer term effects of the rehabilitation programs remaining unknown. In the methodologies used, randomization was not possible, hence separate analyses were done to conclude that the 3 cohorts were comparable in terms of the variables such as prefracture PMS and Katz Index.16,17 Patients with better effort tolerance immediately postsurgery and those with less than or equal to 3 comorbidities were selected for the short intensive program. This could have created a degree of selection bias. However, for those who went for the extended program, they had decent rehabilitation potential, having fulfilled short-term rehabilitation goals such as sitting over the edge of the bed and standing at bedside at the time of disposition. Acute issues that could have affected the effort tolerance immediately postsurgery would have been resolved within the long rehabilitation period, allowing them to possibly catch up on the rehabilitation goals toward the end of their slow-stream program. However, during the follow-up of 1 year, the outcomes of this cohort were not observed to approach that achieved in the cohort who received short intensive rehabilitation—shown to achieve significantly higher mobility scores. Furthermore, the 3 cohorts had comparable prefracture functional and mobility statuses. Based on the findings, the authors are of the opinion that a ward-based short intensive rehabilitation would be the ideal rehabilitation approach for patients similar to our study population to achieve maximal mobility outcomes. Future studies could endeavor to broaden the selection criteria for patients who would benefit from a short and intensive program.
In conclusion, in our study, the intensity and length of rehabilitation programs played a crucial role in the mobility outcomes of the patients recovering from femoral neck fractures after hemiarthroplasty. The data suggest that short intensive inpatient rehabilitation programs (<3 weeks) would most likely yield best functional mobility outcomes, with the highest probability of enabling the patient to achieve prefracture mobility levels.
Footnotes
Authors’ Note: This study was done in compliance with the guidelines set forth for Geriatric Orthopaedic Surgery & Rehabilitation, including Institutional Review Board (IRB) and/or Ethics Committee (EC) approval.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Pasco JA, Sanders KM, Hoekstra FM, Henry MJ, Nicholson GC, Kotowicz MA. The human cost of fracture. Osteoporos Int. 2005;16(12):2046–2052. [DOI] [PubMed] [Google Scholar]
- 2. Oldmeadow LB, Edwards ER, Kimmel LA, et al. No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ J Surg. 2006;76(7):607–611. [DOI] [PubMed] [Google Scholar]
- 3. Sherrington C, Lord SR, Herbert RD. A randomized controlled trial of weight-bearing versus non-weight-bearing exercise for improving physical ability after usual care for hip fracture. Arch Phys Med Rehabil. 2004;85(5):710–716. [DOI] [PubMed] [Google Scholar]
- 4. Vidan M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc. 2005;53(9):1476–1482. [DOI] [PubMed] [Google Scholar]
- 5. Naglie G, Tansey C, Kirkland JL, et al. Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. CMAJ. 2002;167(1):25–32. [PMC free article] [PubMed] [Google Scholar]
- 6. Crotty M, Whitehead CH, Gray S, Finucane PM. Early discharge and home rehabilitation after hip fracture achieves functional improvements: a randomized controlled trial. Clin Rehabil. 2002;16(4):406–413. [DOI] [PubMed] [Google Scholar]
- 7. Eiki Tsushima, Ryukichi Hada, Manabu Iwata, Hitoshi Tsushim. Early prediction of gait ability in patients with hip fracture. Environ Health Prev Med. 2009;14(3):188–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Visser M, Harris TB, Fox KM, et al. Change in muscle mass and muscle strength after a hip fracture: relationship to mobility recovery. J Gerontol A Biol Sci Med Sci. 2000;55(8):M434–M440. [DOI] [PubMed] [Google Scholar]
- 9. Binder EF, Brown M, Sinacore DR, Steger-May K, Yarasheski KE, Schechtman KB. Effects of extended outpatient rehabilitation after hip fracture. a randomized controlled trial. JAMA. 2004;292(7):837–846. [DOI] [PubMed] [Google Scholar]
- 10. Hauer K, Specht N, Schuler M, Bärtsch P, Oster P. Intensive physical training in geriatric patients after severe falls and hip surgery. Age Ageing. 2002;31(1):49–57. [DOI] [PubMed] [Google Scholar]
- 11. Tsauo JY, Leu WS, Chen YT, Yang RS. Effects on function and quality of life of postoperative home-based physical therapy for patients with hip fracture. Arch Phys Med Rehabil. 2005;86(10):1953–1957. [DOI] [PubMed] [Google Scholar]
- 12. Ganz SB, Peterson MG, Russo PW, Guccione A. Functional recovery after hip fracture in the subacute setting. HSS J. 2007;3(1):50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hauer K, Pfisterer M, Schuler M, Bärtsch P, Oster P. Two years later: a prospective long-term follow-up of a training intervention in geriatric patients with a history of severe falls. Arch Phys Med Rehabil. 2003;84(10):1426–1432. [DOI] [PubMed] [Google Scholar]
- 14. Handoll HHG, Sherrington C, Mak JCS. Interventions for improving mobility after hip fracture surgery in adults (Review). Cochrane Database Syst Rev. 2011;(3):CD001704. [DOI] [PubMed] [Google Scholar]
- 15. Parker MJ, Palmer CR. A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br. 1993;75(5):797–798. [DOI] [PubMed] [Google Scholar]
- 16. Kristensen MT, Bandholm T, Foss NB, Ekdahl C, Kehlet H. High inter-tester reliability of the new mobility score in patients with hip fracture. J Rehabil Med. 2008;40(7):589–591. [DOI] [PubMed] [Google Scholar]
- 17. Parker MI, Pryor G, Gurusamy K. Cemented versus uncemented hemiarthroplasty for intracapsular hip fractures. J Bone Joint Surg Br. 2010;92(1):116–122. [DOI] [PubMed] [Google Scholar]
- 18. Lee AY, Chua BS, Howe TS. One-year outcome of hip fracture patients admitted to a Singapore hospital: quality of life post-treatment. Singapore Med J. 2007;48(11):996–999. [PubMed] [Google Scholar]
- 19. Lavini F, Renzi-Brivio L, Aulisa R, et al. The treatment of stable and unstable proximal femoral fractures with a new trochanteric nail: results of a multicentre study with the Veronail. Strat Traum Limb Recon. 2008;3(1):15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]