Abstract
Purpose:
Total hip arthroplasty (THA) is a common and effective treatment of hip osteoarthritis. Activity restrictions known as hip precautions are widely practiced in rehabilitation post THA, aiming to foster healing and prevent hip dislocation. The focused clinical question was: Does the application of hip precautions in patients post THA versus unrestricted activities significantly decrease the risk of prosthetic dislocation?
Methods:
A comprehensive literature search was conducted for randomized controlled trials or cohort studies with a comparative group and minimum 6 months follow-up, with dislocation as an end point. Retrieved titles were assessed independently by 2 reviewers for inclusion and underwent standardized data extraction.
Results:
Title search produced 80 potentially relevant articles. Five articles were retrieved for data extraction of which 2 met a prior eligibility criteria. No eligible studies were found that concerned posterior approaches to hip arthroplasty, so the results of this review concern only anterolateral approaches. Neither included study showed any benefit of hip precautions in preventing dislocation.
Conclusion:
The rate of dislocation after anterolateral THA is low and is not improved by hip precautions. Hip precautions are associated with a slower return to activities, significant expense, and decreased patient satisfaction. Existing studies risk being compromised by a type II error, but a definitive study may be prohibitively large and expensive.
Keywords: hip dislocation, postoperative complication, hip replacement
Introduction
Osteoarthritis (OA) is the most common type of arthritis affecting 9.6% of men and 18.0% of women aged older than 60 years worldwide.1 The main symptoms are pain, stiffness, and limited movement of the affected joint.2 Osteoarthritis is a major cause of disability, psychological distress, and poor quality of life. Management objectives include reducing pain, improving quality of life, preserving or improving joint function, and maintaining independence.3 Involvement of the knee and hip is common, leading to reduced mobility, pain, and loss of amenity. Joint replacement surgery is generally indicated when a person no longer responds to conservative management and where the symptoms are so severe as to be unacceptable. Total hip arthroplasty (THA) is a commonly performed major surgical procedure for the treatment of hip OA that is a widely recognized effective and efficient intervention.4 In 2012, the Australian Orthopaedic Association National Joint Replacement Registry identified over 38 200 hip replacement surgeries were performed in Australian hospitals.5 Since 1993 to 1994, the number of total hip replacements per 100 000 persons has increased by 92%, reflecting the success as an intervention and the aging population, and it is anticipated that rates will increase further.6
As with all interventions, THA can be complicated by adverse events. A recognized complication of THA is dislocation of the prosthesis. This can require further surgery and can cause vascular, neurological injury or result in infection.7 In the period from 1999 to 2011 in Australia, dislocation (22.9%) was the second most common reason for revision surgery in those with a primary total conventional hip replacement, superseded only by loosening and lysis (29%).4 The management of hip dislocation post-THA is difficult, with a Cochrane review finding no appropriate operative versus nonoperative studies to guide which produces better outcomes.8 Strategies that may prevent hip dislocation post-THA are therefore important. Dislocation rates may be reduced by prosthesis selection and design, choice of surgical approach, and technical intraoperative factors.9 Postoperative factors have also been identified as playing a role and the focus of this review is the application of postoperative behavioral and biomechanical restrictions known as hip precautions.
Hip precautions are a common component of standard postoperative care following THA.10 The precautions are prescribed for 6 weeks postoperatively to foster proper healing and prevent hip dislocation. Hip precautions encourage patients to avoid bending at the hip past 90°, twisting their leg in or out, and crossing their legs. Patients are also encouraged to sit with their hips higher than their knees, sit in a chair with armrests, and sleep on their back with a pillow between their legs. Hip precautions may also include avoiding riding in a car or any low seat. Occupational therapists and nurses in conjunction with surgeons are the usual health practitioners who reinforce such education to the patient in the perioperative period.11,12 This education will often include an illustrated handout, verbal instruction, and supervised mobility training on the ward.
Hip precautions focus on limiting the internal rotation, external rotation, adduction, and flexion of the hip. These actions place the hip in positions of risk postsurgery, before capsular and other soft tissue elements around the replaced joint have healed in the early postoperative period. When modeled, these maneuvers led to a high rate of dislocation, lending theoretical support to hip precautions.13 Although the theoretical evidence behind hip precautions is sound, there is limited empirical or clinical evidence to support their findings. Moreover, although prescribing hip precautions may appear an innocuous intervention, adverse effects such as delaying return to normal activity, difficulty in nursing care, falls risk, loss of condition, and joint range of motion need to be considered.
The focused clinical question was: In patients who have had a THA does the application of hip precautions versus unrestricted activities significantly decrease the risk of prosthetic dislocation.
Methods
Despite the routine prescription of hip precautions post-THA across Australia, there have been no Australian randomized controlled trials (RCTs), systematic reviews, or meta-analyses to review their efficacy in practice, prompting a need for evaluation of the current data. No systematic reviews concerning this intervention were identified in a search of Database of Abstracts of Reviews of Effects (DARE), the Cochrane Database of Systematic Reviews (CDSR), the National Institute for Health and Clinical Excellence (NICE), and MEDLINE over the previous 12 months. In this study, we sought to systematically review the available clinical evidence concerning the benefits of hip precautions to patients and their role in preventing hip dislocation post THA.
Eligibility Criteria
Studies that were included in the systematic review comprised of randomized controlled trials or cohort studies with a comparative group. Studies had to have follow-up of at least 6 months, allow the independent effect of hip precautions to be evaluated, and include specific information concerning dislocation and reoperation. Case series and case reports are excluded from the review owing to the high potential for bias in these study designs. Case–control studies (except where nested as part of a cohort study) and economic evaluations were also excluded. Studies were considered from the year 2000 onward to reflect contemporary practice and prosthesis design. Language was restricted to those in English and the search included published work and conference abstracts. Where only abstract information was available, a sensitivity analysis was performed.
Information Sources
The following databases were searched: MEDLINE, EMBASE, CINAHL, AMED, Cochrane library, and Google Scholar. The last search took place on the April 3, 2013.
Search Strategy
The following terms were searched: “hip” AND “arthroplasty” AND “education” AND “dislocation” OR “hip precautions”.
Study Selection
All titles and abstracts retrieved by this search were considered independently by 2 authors for eligibility. Where studies suggested that they might meet the eligibility criteria, the full text of the study was obtained. The full-text articles were then assessed for eligibility again by 2 independent reviewers. All studies were assessed for quality using the Jadad criteria.14
Data Collection
Data extraction was performed by all 3 authors using a piloted data extraction form primarily addressing the number of patients in the study, the type of precautions advised, the nature of the control group, and the frequency of dislocation and reoperation in each group. Where differences emerged in the data extraction, they were resolved by consensus. We evaluated risk of bias at study level. In the data synthesis, studies were assessed on a quality basis and a sensitivity analysis was performed to explore the effect of quality on outcome.
Summary Measures
The principle summary measure was the risk ratio between the treatment and the comparator groups at 6 months.
Results
From 80 articles in our initial search, 5 articles were retrieved15,16 for data extraction (Figure 1). Of those 5, 2 RCTs met our eligibility criteria.16,17 The details of the articles retrieved are given in Tables 1 and 2.
Figure 1.
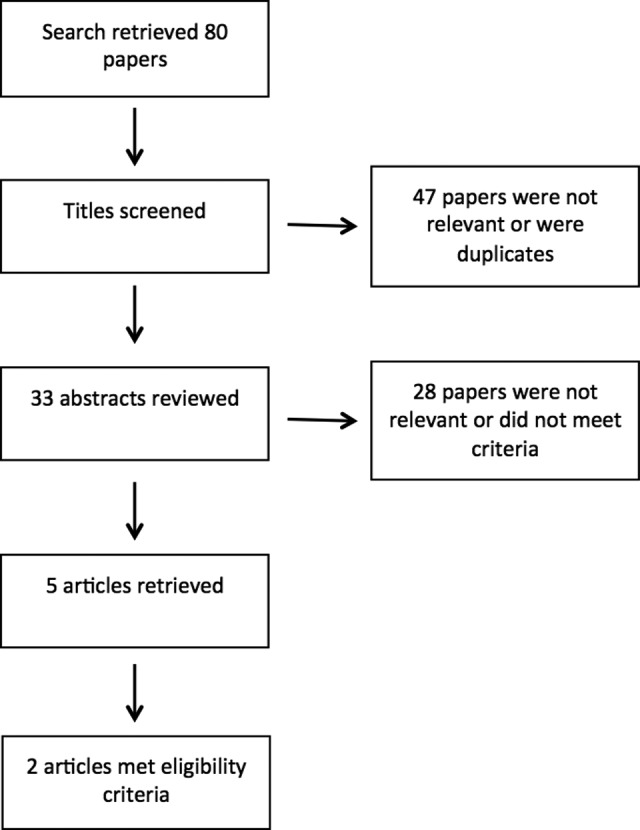
Flow chart for selection of papers.
Table 1.
Summary of Included Studies.
| Ververeli et al16 | Peak et al17 | |
|---|---|---|
| Setting | Single center private practice affiliated with local hospital | Single center University Hospital |
| Type of study | Unblinded prospective randomized controlled trial | Prospective randomized controlled trial Surgeons were blinded until would closure |
| Number of patients included | 81 | 265 |
| Percentage of follow-up | 100% | 100% |
| Duration of follow-up | 1 year | 6 months |
| Intervention and comparative group | Standard versus early rehabilitation Standard: Hip precautions Early: Not to cross legs at thighs, otherwise no restrictions | Restricted versus unrestricted All patients: Limit hip flexion to <90°, hip internal/external rotation <45°, adduction (crossing legs) Restricted group (additional precautions): abduction pillow postoperative, pillows to maintain abduction when in bed, elevated toilet seats, elevated chairs, prevented from sleeping on their side, prevented from driving, and being a passenger |
| Surgical technique | Anterolateral procedure | Anterolateral procedure |
| Dislocations and consequences | No dislocations reported for either group | 1 dislocation in the restricted group Managed with closed reduction and no need for reoperation |
| Conclusions from the study | Faster return to function in early rehabilitation group. Postoperative restrictions provide no additional benefit and limit patients from activities they are capable of completing | Faster recovery and greater satisfaction in unrestricted group, earlier return to activities of daily living, estimated savings of US$655 per patient in unrestricted group. Imposition of restrictions other than the limitations of extreme motions did not influence prevalence of dislocation in this group |
| Limitations | Small numbers, study ended before it was fully enrolled | Low incidence of dislocations suggest a possible type II error. Noted compliance of about 70% with restrictions |
Table 2.
Summary of Excluded Studies.
| Restrepo et al19 | Lubbeke et al15 | Talbot et al20 | |
|---|---|---|---|
| Setting | Single center University Hospital | Single center University Hospital | Single center district hospital |
| Type of study | Prospective cohort of sequential patients | Prospective series with nonparticipant controls—voluntary basis of selection for intervention | Prospective cohort study |
| Number of patients included | 2532 | 2238 | 483 |
| Percentage of follow-up | 94 | 99.3 | 100 |
| Duration of follow-up | 6 Months | 6 Months | 6 Weeks |
| Intervention and comparative group | No comparative group No restrictions on movement | Voluntary preoperative multidisciplinary education program including <90° flexion, <20° internal and external rotation. Instruction on using car seats, raised equipment, explanation of dislocation and surgical procedure | No comparative group No restrictions on movement |
| Surgical Technique | Anterolateral | Anterolateral | Anterolateral Procedure |
| Dislocations and consequences | 4 Dislocations | 46 Dislocations 5 in participants and 41 in non-participants | 3 Dislocations Managed with closed reduction and no need for re-operation |
| Conclusions from the study | Low rate of dislocations without restrictions | Educational session helped decrease rate of dislocation | Restrictions not justified when using an anterolateral approach. |
| Limitations/exclusion basis | Large number of sequentially enrolled patients and no control group | Non-randomized, no systematic ascertainment of dislocation rate, underpowered to detect difference in contemporaneous control and volunteer bias | No control group and brief follow up |
This systematic review yielded few primary studies concerning the effectiveness of hip precautions post-THA. Two RCTs were found.16,17 Neither was blinded beyond the surgery itself. Randomization appeared to be correctly conducted, and all patients were accounted for at follow-up. Both of these studies therefore score 2 out of a possible 3 on the Jadad criteria.14 The interventions and control conditions were different between these studies (Table 1), with more liberal activities permitted in the trial of Ververeli et al. This heterogeneity precludes pooling of data between the reviews. Neither study found any benefit from hip precautions, but only 1 dislocation occurred in 346 patients so there is a high probability of a type II error, which is an error that occurs when one accepts a null hypothesis that is actually false.18
One further study with a comparison group was identified.15 This complex study used prospectively collected data on patient demographics, comorbidities, and operative parameters. The ascertainment of the primary outcome of concern, prosthesis dislocation, was not collected systematically but relied upon reporting and database screening of the individual surgical practices as well as presentations to the hospital where the study had been conducted. The intervention was a multidisciplinary preoperative education session delivered to patients over 3 hours, which included recommendations about restricting movements and advice on seats and cars. The session also incorporated other components including a description of dislocation, a detailed explanation of the prosthesis, and direct contact with a senior surgeon. It is therefore impossible to dissect any one component that may be responsible for any effect. Participation in the program was voluntary, attracting 46.7% of the cohort to partake in the education sessions. These selection criteria may have introduced volunteer bias, and no assessment of actual behavior or concurrent interventions such as advice from other sources during the admission was performed. The comparison groups were those not volunteering to participate and a historical group being those who were operated on prior to the availability of the educational program. It was felt that these methodological issues introduced sufficient bias that the results not be valid for inclusion in this systematic review.
In considering these results, it is important to assess any adverse effects from applying hip precautions. Both the included studies considered the benefits of not applying hip precautions. Peak et al noted a faster return to activities of daily living (ADLs), lower costs, and a higher degree of patient satisfaction in the unrestricted group. Similarly, Ververeli et al found a faster pace of recovery and an earlier return to driving in the unrestricted group.
The 2 other studies retrieved were prospective case series with no comparison group and therefore failed to meet our a priori inclusion criteria.19,20 Nevertheless, they provide an estimate of the rates of dislocation in patients who did not receive a full suite of hip precautions (Table 2).
All retrieved studies concerned only anterolateral approaches to THA, and these results can only pertain to patients who are managed with this technique.
Discussion
This systematic review found no evidence to support the use of hip precautions following anterolateral THA for the prevention of hip dislocation. Moreover, patients assigned to hip precautions had slower rehabilitation and return to usual ADLs.
The strength of this review is the application of an explicit clinical question, a predefined search, inclusion strategy, and multiple assessors of articles to be included. These serve to enhance the reliability of the conclusions and offer important advantages over narrative reviews, which risk including biased studies that may distort the true effect.
The weaknesses of this review are that the number of included studies is small but this is a failing of the existing literature. These results only pertain to anterolateral approaches to THA and cannot be applied to posterior approaches, where the baseline rate of dislocation is higher and the beneficial effects of hip precautions are unknown. We did not perform a sensitivity analysis including results from non-RCT studies. There was only 1 study that included a comparison group but the intervention was not specifically hip precautions, follow-up was not systematic, and participation was voluntary. In those studies where the outcomes of the dislocations were reported, they were benign events usually not requiring surgery and not associated with morbidity. Total hip arthroplasty dislocation is common in patients older than 80 years of age. Those with poor muscular tone, femoral neck fractures, acetabular dysplasia, cerebral palsy, muscular dystrophy, and intellectual impairment are all associated with an increased dislocation rate.21 Unfortunately, no comment can be made on the long-term effects of hip precautions, as one cannot extrapolate beyond the available studies.
The 5 retrieved studies15–17,19,20 covered a total of THA 5816 patients, with a total of 54 dislocations reported. This represents a dislocation rate of 0.9%. Taking this as a crude estimate, it is possible to calculate the size of a study needed to demonstrate a clinically meaningful decrease in hip dislocation. Arbitrarily, decreasing the rate of dislocation by 50% would seem a reasonable goal. This would mean that one hip dislocation would be prevented by 222 patients having precautions. The study involved to reliably demonstrate this incremental benefit would be large, requiring over 5000 patients in each arm.22 It seems unlikely that such a study will ever be logistically feasible.
Conclusion
The available evidence would suggest that the rate of dislocation after anterolateral approach to THA is low and is not improved by hip precautions. At the same time, hip precautions are associated with a slower return to ADLs, significant expense, and less patient satisfaction. Existing studies risk being compromised by type II statistical error, but a definitive study would be prohibitively large and expensive.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. World Health Organization. Chronic diseases and health promotion 2015 4th April 2015. Web site http://www.who.int/chp/topics/rheumatic/en/. Accessed April 4, 2015.
- 2. Felson D. Osteoarthritis In: Longo D, Fauci A, Kasper D, Hauser S, Jameson J, Loscalzo J, eds. Harrison’s Principles of Internal Medicine. 18th ed New York: McGraw-Hill; 2012. [Google Scholar]
- 3. Australian Institute of Health and Welfare. A picture of osteoarthritis in Australia. Canberra Australian Institute of Health and Welfare, 2007 Contract No.: Cat. no. PHE 93.
- 4. Australian Orthopaedic Association National Joint Replacement Registry. Annual Report Adelaide: AOA, 2012. [Google Scholar]
- 5. National Joint Replacement Registry. Australian Orthopaedic Association National Joint Replacement Registry Annual Report 2013. Web site https://aoanjrr.dmac.adelaide.edu.au/documents/10180/127202/Annual%20Report%202013?version=1.2&t=1385685288617. Accessed April 4, 2015.
- 6. Australian Institute of Health and Welfare. Arthritis and osteoporosis in Australia 2008 Canberra: Australian Institute of Health and Welfare, 2008 Contract No.: Cat. no. PHE 106. [Google Scholar]
- 7. Chandler R, Dorr L, Perry J. The functional cost of dislocation following total hip arthroplasty. Clin Orthop Relat Res. 1982;(168):168–172. [PubMed] [Google Scholar]
- 8. Khan RJK, Carey Smith RL, Alakeson R, Fick DP, Wood D. Operative and non-operative treatment options for dislocation of the hip following total hip arthroplasty. Cochrane Database Syst Rev. 2006;(4):CD005320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. 2006;447:19–23. [DOI] [PubMed] [Google Scholar]
- 10. Tran P, Fraval A. Total hip replacement. Recovery and rehabilitation: Western Health; 2013. Web site http://www.orthoanswer.org/hip/total-hip-replacement/recovery.html. Accessed August 13, 2013.
- 11. Stewart LSP, McMillan IR. How necessary are hip restrictions for avoiding dislocation following hemiarthroplasty or total hip arthroplasty in older patients with a hip fracture? Br J Occup Ther. 2011;74(3):110–118. [Google Scholar]
- 12. College of Occupational Therapists. Occupational therapy for adults undergoing total hip replacement. Practice guideline College of Occupational Therapists 2012. Web site http://www.cot.co.uk/sites/default/files/general/public/P171-Total-Hip-Replacement.pdf. Accessed May 10, 2015.
- 13. Nadzadia ME, Pedersena DR, Yackc HJ, Callaghana JJ, Browna TD. Kinematics, kinetics, and finite element analysis of commonplace maneuvers at risk for total hip dislocation. J Biomech. 2003;36(4):577–591. [DOI] [PubMed] [Google Scholar]
- 14. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17(1):1–12. [DOI] [PubMed] [Google Scholar]
- 15. Lubbeke A, Suva D, Perneger T, Hoffmeyer P. Influence of preoperative patient education on the risk of dislocation after primary total hip arthroplasty. Arthritis Rheum. 2009;61(4):552–558. [DOI] [PubMed] [Google Scholar]
- 16. Ververeli PA, Lebby EB, Tyler C, Fouad C. Evaluation of reducing postoperative hip precautions in total hip replacement: A randomized prospective study. Orthopedics. 2009;32(12):889–893. [DOI] [PubMed] [Google Scholar]
- 17. Peak EL, Parvizi J, Ciminiello M, et al. The role of patient restrictions in reducing the prevalence of early dislocation following total hip arthroplasty: A randomized, prospective study. J Bone Joint Surg. 2005;87(2):247–253. [DOI] [PubMed] [Google Scholar]
- 18. Swinscow TDV. In: Campbell MJ, ed. Statistics at square one. 9th ed London: BMJ Publishing Group; 1997. Web site http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/5-differences-between-means-type-i-an. Accessed May 5, 2015. [Google Scholar]
- 19. Restrepo C, Mortazavi SMJ, Brothers J, Parvizi J, Rothman RH. Hip dislocation. Are hip precautions necessary in anterior approaches? Clin Orthop Relat Res. 2011;469(2):417–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Talbot NJ, Brown JHM, Treble NJ. Early dislocation after total hip arthroplasty: Are postoperative restrictions necessary? J Arthroplasty. 2002;17(8):1006–1008. [DOI] [PubMed] [Google Scholar]
- 21. Crawford RW, Murray DW. Total hip replacement: indications for surgery and risk factors for failure. Ann Rheumat Dis. 1997;56(8):455–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brant R. Inference for proportions: comparing two independent samples: The University of British Columbia, Department of Statistics. Web site http://www.stat.ubc.ca/∼rollin/stats/ssize/b2.html. Accessed August 6, 2013.


