Abstract
As part of setting the stage for this supplement to the American Journal of Preventive Medicine, a life-course perspective is presented to assist in understanding the importance of cancer prevention for adults in midlife, a period roughly spanning 20 years between ages 45 and 64 years. Drawing on disciplinary perspectives from the social sciences and public health, several life-course themes are delineated in this article: how specific life transitions present unique opportunities for interventions to inform policy and practice that can improve population health outcomes; how interventions can be focused on those at particular life stages or on the entire life course; and how the onset and progression of chronic conditions such as cancer are dependent on a complex interplay of critical and sensitive periods, and trajectory and accumulation processes. A translational research framework is applied to help promote the movement of applied public health interventions for cancer prevention into practice. Also explored are differences that can affect people at midlife relative to other age cohorts. Specifically, cancer-related risks and care networks are examined, with examples of public health strategies that can be applied to cancer prevention and control. As a conclusion, select methodologic issues and next steps for advancing research and practice are identified.
Introduction
As elaborated in other papers in this supplement, cancer risks are multifaceted and include well-documented genetic, behavioral, social, and environmental factors.1,2 Fortunately, evidence-based cancer prevention strategies for ameliorating such risk factors are growing.3,4 Although less is known about what specific interventions should be targeted to particular age groups to reduce cancer risks, there is growing recognition of the value of combining a life-course perspective with public health frameworks and interventions that can be applied to cancer prevention and control. The purpose of this introductory article is to delineate how a life-course perspective can advance research and practice related to cancer prevention among adults 45–64 years of age.
A Life-Course Perspective
Life-course theory from a social sciences perspective refers to a person’s placement in society (experiences and roles) as well as life stage or age.5–7 In public health, life-course epidemiology8 examines a range of potential processes through which exposures acting at different stages of life can, alone or in combination, influence the timing of disease risks. This provides a way to conceptualize how underlying socio-environmental determinants of health, experienced at different life-course stages, can differentially influence the development of chronic diseases. Applying a life-course perspective can help with identifying the factors earlier in adulthood that may help to delay, minimize, or prevent some of the changes in biological, psychological, and social functioning that occur in later life; help with the identification of key risk factors to reduce onset and exacerbation of chronic diseases and disabilities at each life stage; and support the formulation of interventions to address unique risk factors at specific life stages.
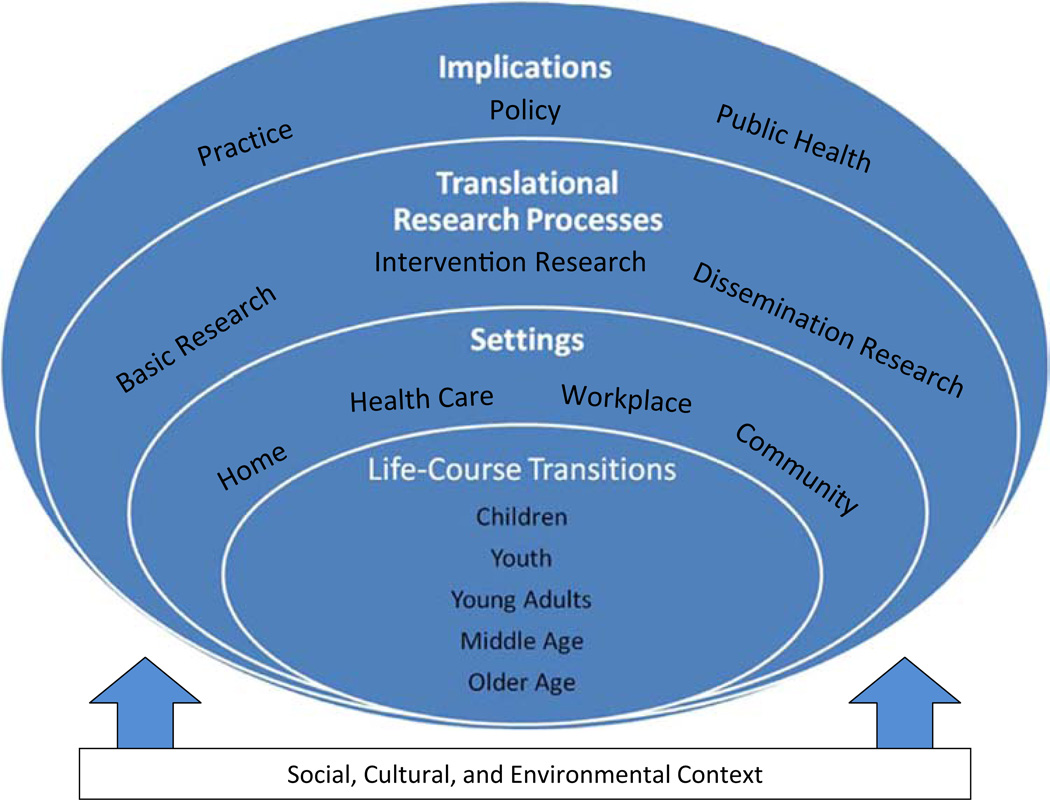
A framework examining the life course through the lens of research translation can help enhance our understanding of cancer prevention at midlife. Figure 1, adapted from the behavioral medicine field,9 has at its core Life-Course Transitions. These transitions are important for a number of reasons. Specific life transitions, such as entering or leaving the workforce, present unique opportunities for interventions to inform policy and practice that can improve health outcomes and quality of life. Additionally, interventions can be focused on those at particular life stages (e.g., course on postretirement planning) or on the entire life course (e.g., age-appropriate educational activity from kindergarten to Elderhostel). Most individual-level interventions tend to be life-course–specific, while those targeting family or community-level populations are more likely to cut across different life-course stages. This is particularly so for interventions focused on intergenerational interactions such as caregiving.
Figure 1.
A life-course perspective for translational cancer-prevention research
The next ring of the figure—Settings—directs attention to the importance of interventions for cancer prevention directed to single or multiple settings (e.g., home, health care, workplace, or community settings). Each of these settings has particular relevance to adults at midlife. For example, workplace may be a particularly important place to intervene for groups of workers at established worksites. Translational Research Processes, the next ring, highlights the importance of translating interventions into practice. A life-course approach recognizes that life transitions or events can result in teachable moments for introducing health-oriented interventions (preparing for a daughter’s or son’s wedding or birth of a grandchild).9
In the most outer ring, a broad range of implications need to be considered in cancer prevention, including improved public health and quality of life. For example, interventions affecting the structural features of the workplace may affect an employee’s ability to make healthy physical activity and nutritional choices while working.10 Chronic conditions, including cancer, likely result from the complex interplay of multiple risk factors operating at critical and sensitive periods, and trajectory and accumulation processes. Such examples illustrate the importance of a life-course perspective for understanding disease risks over time.8 The framework helps delineate how basic cancer prevention processes get translated into applied public health interventions that are influenced by the social, cultural, and environmental context.
Cancer Prevention and Midlife
In recent years, there has been increased attention to midlife as an area worthy of distinct study, especially in the context of a life-course perspective.11–18 Although its definition can vary in terms of age ranges considered, midlife is defined here to mean the age period from 45 to 64 years. Midlife is an important developmental period because it reflects influences from younger years and foreshadows health and well-being in later life. Covering roughly 25% or more of a typical adult’s life expectancy, the salience of mid-life has increased as it has become a growing portion of the American population. Between 2000 and 2010, the population aged 45–64 years grew 31.5%, to 81.5 million, and now makes up 26.4% of the total U.S. population.19 This age group spends a large portion of their income on health expenditures, and this is especially so among individuals with lower incomes. For example, almost one third of those aged 50–64 years spend 10% or more of their income on health services, and the numbers of uninsured have grown.20 From a health perspective, midlife represents a watershed, the period at which host immunity begins to decline and the effects of behavioral, social, and environmental risks for ill health begin to accumulate.21
Although there is much variability among those in midlife, people in this stage of life may be facing unexpected or new responsibilities like changes in their own health or aging family members.22 For example, using 2006–2010 data from the Behavioral Risk Factor Surveillance System (BRFSS), self-reported disability status was 26.4% among respondents aged 45–64 years compared to only 13.0% among those aged 18–44 years.23 This life-stage might be a wake-up call in the form of early health problems experienced by midlife adults themselves or seen in others in their social networks.
Competing obligations may jeopardize the use of preventive services because of time spent juggling multiple roles to achieve a balance of work, family, and personal interests. In terms of career, for many, this age period is a time of career “peaking” and of women returning to the workforce.11 In contrast, using a set of select clinical preventive services recommended by age and gender, about 26% of adults aged 50–64 years in 2009 were up-to-date on select services compared to about 48% of older adults.24,25 Additionally, a study by Lima et al.26 found that adults aged 52–62 years with functional limitations were cared for primarily by spouses, the majority remained in the workforce and typically provided fewer hours of care as compared to that received by older age groups. Moreover, those in midlife, particularly women, are also more likely to be responsible for caring for both dependent adult children as well as older family members, which has serious implications for prevention.26
Cancer-Related Risk Factors Among Adults Aged 45–64 Years
The life experiences of midlife adults can place them at increased risk for cancer, especially for breast, colon, and lung cancers, as well as other leading chronic conditions, which are increasingly being recognized as linked to behaviors (such as smoking, lack of physical activity, and poor eating habits).27–29 The recognition of links between obesity and increased cancer risks28 is another good reason why healthcare professionals should adopt behaviorally based strategies for counseling overweight or obese midlife patients about the importance of physical activity and weight management.30 Additionally, there are suggestions that health disparity gaps in cancer incidence rates related to health behaviors and environmental factors begin to widen in this age group with the accumulation of a lifetime of exposures and risk factors.31,32
Consistent with stresses that might accompany multiple roles, some studies find that caregivers are less likely than noncaregivers to engage in regular exercise and healthy eating.33 Similarly, caring for multiple generations may prevent individuals from taking care of their own health and medical needs, with reduced amount of time available for engaging in healthy behaviors. Conversely, caregivers may be particularly motivated to maintain their own health because others depend on them for care or because they observe the decline in health among those around them.
Life-Course Approach to Cancer Prevention
This paper applies a life-course approach to cancer prevention, with a particular focus, here, on midlife.34 Two types of activities are highlighted that can help identify at earlier stages the onset of chronic diseases such as cancer: promoting clinical preventive services and promoting physical activity and exercise.
Age- and gender-based guidelines focusing on recommended clinical preventive services, often organized around vaccinations, screenings, and counseling, can be a key public health strategy to help ensure early detection of diseases and timely intervention.25 In line with Healthy People 2020 targets,35 a number of indicators for monitoring the use of clinical preventive services among adults aged 50–64 years have been identified, including a set of screening services and risk factors related to cancer detection and prevention.24 Cancer prevention guidelines often include the recommended clinical preventive services (including colorectal cancer screening, mammography, and Pap tests) and also promote a reduction in cancer risk factors such as physical inactivity, smoking, alcohol consumption, and obesity.
Adults in this age group are often unaware of the clinical preventive services recommended for their age, gender, and risk factors—or do not consider themselves to be at risk.36 Systemic referrals between clinical and community providers are not consistently available or fully utilized.37 Ensuring the delivery of essential preventive services requires creative, sustained collaboration between healthcare and community providers. In 2009, it was estimated that approximately 26% of adults in this age range are up to date on the delivery of recommended cancer screenings and influenza vaccination.38 New innovations are also being developed and tested, such as a new “5over50” initiative,39 which is being led by the SPARC program (Sickness Prevention Achieved Through Regional Collaboration) and supported in part by the Robert Wood Johnson Foundation to encourage people aged 50–64 years to know about and obtain recommended preventive services.40 This initiative is part of a larger effort to enhance the use of multiple clinical preventive services through creating and sustaining linkages between community organizations and healthcare entities.24,40
Among the various health behaviors receiving increased attention in cancer prevention, there is strong evidence that engagement in physical activity, from everyday walking to more structured exercise regimens, reduces the incidence of leading forms of cancer, most notably, cancers of the breast and colon.41–43 Although our perspective is that every life stage presents unique opportunities and risks, adults in midlife (ages 45–64 years) are among the most sedentary segment of the population and hence especially vulnerable. According to BRFSS data from 2010,44 middle-aged adults were more sedentary than younger groups (25.5% of adults aged 45–64 years did not report exercising in past 30 days compared to 17.7% for adults aged 18–24 years and 21.8% for adults aged 25–44 years). Midlife adults were more active than older adults, with 31.8% reported not being physically active. Inadequate physical activity at midlife is likely to contribute to weight gain in later life unless preventive action is taken to modify physical activity.2 Further, available data suggest that adult cancer patients/survivors are more sedentary than the general population,45 although estimates of physical activity or sedentary behavior for adult cancer patients/survivors aged 50–64 years compared to other age groups are not readily available.
There are several evidence-based strategies for increasing physical activity. As indicated in The Guide to Community Preventive Services, there is positive support for community-wide campaigns, behavioral and social approaches, and environmental and policy approaches.3 Behavioral change studies confirm that midlife adults can improve their physical activity levels, although maintenance after the intervention ceases remains challenging.46–49 Hence, community programs should build on ongoing initiatives or incentives that enhance opportunities for walking and physical activity as part of everyday life. For example, it has been suggested that walking routes be established in proximity to businesses and worksites and that zoning regulations increase opportunities for mixed-use developments that reduce the distances between residences and places of work.50,51
Because physical activity also reduces the risk of a variety of other chronic conditions, including cardiovascular disease and diabetes, programs to promote physical activity do not typically focus exclusively on cancer prevention. Instead, such programs are often part of broader health and wellness programs directed toward both individuals and communities. An exception that is particularly relevant to adults in midlife is the CEO Gold Standard Program,52 which encourages workplaces to adopt programs and policies that will increase workers’ access to physical activity, healthy nutrition, and smoke-free environments.
Next Steps for Life-Course Cancer-Prevention Research and Practice
This paper has emphasized the importance of a life-course perspective that recognizes the unique risk factors experienced by midlife adults and calls for wider dissemination of evidence-based and other promising interventions for reducing cancer risks. Given the current fragmented disciplinary approaches being used to understand the wide variety of factors affecting people in midlife, there is a need for multidisciplinary perspectives to address cancer-related risk factors in this life stage. For example, there is relevant expertise in life-course perspectives in social sciences and epidemiology, attention to midlife transitions in psychological sciences, a growing evidence base in behavior change/intervention research, and promising theory and applications in cancer prevention and control. What is missing, however, is a transdisciplinary perspective that brings together knowledge from various biological, clinical, behavioral and social sciences, and public health disciplines to accelerate cancer prevention activities for adults aged 45–64 years.
Many questions about midlife are still unanswered. Further research is needed on topics such as (1) the multidisciplinary nature of midlife and the interplay of biomedical, psychological, and social factors during midlife; (2) risks most important to target for cancer prevention and control in midlife; and (3) interventions most effective for the general population aged 45–64 years, as well as the most vulnerable segments who are often the hardest to reach and medically underserved.
There are also opportunities to make positive changes to practice. As midlife can provide a window for a glimpse of later life, this time period should be used to engage in prevention and to ameliorate cancer-related risks in midlife and beyond. Opportunities to improve delivery of preventive services exist in both clinical and community settings. Better linkages and more coordinated activities across these settings could result in more efficiencies and prevention benefits. In an ideal world, individuals in midlife would be aware of cancer risks, know what can be done to reduce these risks, have the skills to engage in healthier behaviors, and live in communities that support healthy living environments that reduce cancer risks.
The life-course perspective offers a valuable framework for identifying cancer risks as well as pinpointing effective cancer prevention strategies that resonate with teachable moments related to midlife transitions and trajectories. This paper provides a context in which the subsequent series of articles that examine genetic, behavioral, social, and environmental factors as well as their interactions with cancer incidence and prevention can be viewed.
Acknowledgments
Publication of this article was supported (in part) by the CDC cooperative agreements to Prevention Research Centers Programs in support of two Networks, the Healthy Aging Research Network, which is funded by CDC’s Healthy Aging Program, and the Cancer Prevention and Control Research Network, which is funded by CDC’s Division of Cancer Prevention and Control. MG Ory was partially supported by Grant 1U48/ DP001924. DB Friedman was partially supported by Grant 1U48/DP001936, the Cancer Prevention and Control Research Network, from the CDC and the National Cancer Institute and Grant 1U48/DP001936, the Healthy Aging Research Network, from the CDC. WA Satariano was partially supported by Grant 1U48/DP001911.
The publication of this supplement was made possible through the CDC and the Association for Prevention Teaching and Research (APTR) Cooperative Agreement No. 1 U360E000005-01. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC or the APTR.
Footnotes
No financial disclosures were reported by the authors of this paper.
References
- 1.Holman DM, Grossman M, Henley SJ, Peipins LA, Tison L, White MC. Opportunities for cancer prevention during midlife: highlights from a meeting of experts. Am J Prev Med. 2014;46(3S1):S73–S80. doi: 10.1016/j.amepre.2013.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.White MC, Holman DM, Boehm JE, Peipins LA, Grossman M, Henley SJ. Age and cancer risk: a potentially modifiable relationship. Am J Prev Med. 2014;46(3S1):S7–S15. doi: 10.1016/j.amepre.2013.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Task Force on Community Preventive Services. The guide to community preventive services: cancer prevention and control. www.thecommunityguide.org/cancer/index.html. [Google Scholar]
- 4.National Cancer Institute. Research-tested intervention programs (RTIPs) doi: 10.1111/j.1746-1561.2009.00426.x. rtips.cancer.gov/rtips/index.do. [DOI] [PMC free article] [PubMed]
- 5.Mortimer JT, Shanahan MJ. Handbook of the life course. New York: Kluwer Academic/Plenum Publishers; 2003. libcat.tamu.edu/vwebv/holdingsInfo?bibId=2164443. [Google Scholar]
- 6.Settersten RA. Lives in time and place: the problems and promises of developmental science. Amityville NY: Baywood Publishing; 1999. p. 318. [Google Scholar]
- 7.Fuller-Iglesias H, Smith J, Antonucci TC. Theories of aging from a lifecourse and life-span perspective. Annu Rev Gerontol Geriatr. 2009;29:3–25. [Google Scholar]
- 8.Lynch J, Smith GD. A life course approach to chronic disease epidemiology. Annu Rev Public Health. 2005;26:1–35. doi: 10.1146/annurev.publhealth.26.021304.144505. [DOI] [PubMed] [Google Scholar]
- 9.Ory MG, Smith ML, Resnick B. Changing behavior throughout the life-course: translating the success of aging research. Transl Behav Med. 2012;2(2):159–162. doi: 10.1007/s13142-012-0129-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sorensen G, Landsbergis P, Hammer L, et al. Preventing chronic disease in the workplace: a workshop report and recommendations. Am J Public Health. 2011;101:S196–S207. doi: 10.2105/AJPH.2010.300075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pruchno R. Not your mother’s old age: baby boomers at age 65. Gerontologist. 2012;52(2):149–152. doi: 10.1093/geront/gns038. [DOI] [PubMed] [Google Scholar]
- 12.Moen P, Wethington E. Midlife development in a life course context. In: Willis S, Reid J, editors. Life in the middle. San Diego CA: Academic Press; 1999. pp. 3–24. [Google Scholar]
- 13.Lachman ME. Development in midlife. Annu Rev Psychol. 2004;55:305–331. doi: 10.1146/annurev.psych.55.090902.141521. [DOI] [PubMed] [Google Scholar]
- 14.Willis S, Martin M, Rocke C. Longitudinal perspectives on midlife development: stability and change. Eur J Ageing. 2010;7(3):131–134. doi: 10.1007/s10433-010-0162-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Toothman EL, Barrett AE. Mapping midlife: an examination of social factors shaping conceptions of the timing of middle age. Adv Life Course Res. 2011;16(3):99–111. [Google Scholar]
- 16.Katz J, Peace S, Spurr S. Adult lives: a life course perspective. Bristol: Policy Press; 2012. [Google Scholar]
- 17.Lynch C, Danely J. Transitions and transformations: cultural perspectives on aging and the life course. New York: Berghahn; 2013. viii, 270 p.: ill., 24 cm. libcat.tamu.edu/vwebv/holdingsInfo?bibId=4552787. [Google Scholar]
- 18.Binstock RH, George LK. Handbook of aging and the social sciences. 7th ed. San Diego CA: Academic Press; 2011. [Google Scholar]
- 19.U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau. Howden L, Meyer J, editors. Age and sex composition: 2010. 2010 Census Briefs. 2011 C2010BR-03. www.census.gov/prod/cen2010/briefs/c2010br-03.pdf.
- 20.Smolka G, Multack M, Figueiredo C. Health costs and coverage for 50–64-year olds. AARP Public Policy Institute. 2012:247. www.aarp.org/content/dam/aarp/research/public_policy_institute/health/Health-In surance-Coverage-for-50-64-year-olds-insight-AARP-ppi-health.pdf. [Google Scholar]
- 21.Satariano WA. Epidemiology of aging: an ecological approach. Sudbury MA: Jones & Bartlett Learning; 2006. [Google Scholar]
- 22.Settersten RA, Angel JL. Handbook of sociology of aging. New York NY: Springer; 2011. [Google Scholar]
- 23.CDC. National center on birth defects and developmental disabilities: disability and health data system. www.cdc.gov/ncbddd/disabilityandhealth/dhds.html.
- 24.CDC, AARP, American Medical Association. Promoting preventive services for adults 50–64: community and clinical partnerships. 2009 www.cdc.gov/aging/pdf/promoting-preventive-services.pdf.
- 25.Shenson D, Anderson L, Slonim A, Benson W. Vaccinations and preventive screening services for older adults: opportunities and challenges in the USA. Perspect Public Health. 2012;132(4):165–170. doi: 10.1177/1757913912444850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lima JC, Allen SM, Goldscheider F, Intrator O. Spousal caregiving in late midlife versus older ages: implications of work and family obligations. J Gerontol B Psychol Sci Soc Sci. 2008;63(4):S229–S238. doi: 10.1093/geronb/63.4.s229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peel JB, Sui X, Matthews CE, et al. Cardiorespiratory fitness and digestive cancer mortality: findings from the aerobics center longitudinal study. Cancer Epidemiol Biomarkers Prev. 2009;18(4):1111–1117. doi: 10.1158/1055-9965.EPI-08-0846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peel JB, Sui X, Adams S, Hebert J, Hardin J, Blair S. A prospective study of cardiorespiratory fitness and breast cancer mortality. Med Sci Sports Exerc. 2009;41(4):742–748. doi: 10.1249/MSS.0b013e31818edac7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.La Vecchia C, Giordano SH, Hortobagyi GN, Chabner B. Overweight, obesity, diabetes, and risk of breast cancer: interlocking pieces of the puzzle. Oncologist. 2011;16(6):726–729. doi: 10.1634/theoncologist.2011-0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American College of Preventive Medicine. Adult obesity: a resource from the American College of Preventive Medicine. 2009 c.ymcdn.com/sites/www.acpm.org/resource/resmgr/timetools-files/adultobesitypatientguide.pdf. [Google Scholar]
- 31.Satariano WA, Swanson GM. Racial differences in cancer incidence: the significance of age-specific patterns. Cancer. 1988;62(12):2640–2653. doi: 10.1002/1097-0142(19881215)62:12<2640::aid-cncr2820621233>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 32.National Cancer Institute. Cancer health disparities. www.gov/cancertopics/factsheet/disparities/cancer-health-disparities.
- 33.Talley RC, Crews JE. Framing the public health of caregiving. Am J Public Health. 2007;97(2):224–228. doi: 10.2105/AJPH.2004.059337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Breslow L, Somers AR. The lifetime health-monitoring program. A practical approach to preventive medicine. N Engl J Med. 1977;296(11):601–608. doi: 10.1056/NEJM197703172961104. [DOI] [PubMed] [Google Scholar]
- 35.USDHHS. Healthy People 2020 topics and objectives. www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=5.
- 36.Friedman DB, Corwin SJ, Dominick GM, Rose ID. African American men’s understanding and perceptions about prostate cancer: why multiple dimensions of health literacy are important in cancer communication. J Community Health. 2009;34(5):449–460. doi: 10.1007/s10900-009-9167-3. [DOI] [PubMed] [Google Scholar]
- 37.IOM. Living well with chronic illness: a call for public health action. 2012 doi: 10.7205/MILMED-D-15-00034. www.iom.edu/Reports/2012/Living-Well-with-Chronic-Illness.aspx. [DOI] [PubMed] [Google Scholar]
- 38.Shenson D, Adams M, Bolen J. Delivery of preventive services to adults aged 50–64: monitoring performance using a composite measure, 1997–2004. J Gen Intern Med. 2008;23(6):733–740. doi: 10.1007/s11606-008-0555-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Change Observer. Aspen design summit report: CDC and healthy aging. changeobserver.designobserver.com/aspen/. [Google Scholar]
- 40.Shenson D, Benson W, Harris AC. Expanding the delivery of clinical preventive services through community collaboration: the SPARC model. Prev Chronic Dis. 2008;5(1):A20–A27. [PMC free article] [PubMed] [Google Scholar]
- 41.Friedenreich CM. Physical activity and cancer prevention: from observational to intervention research. Cancer Epidemiol Biomarkers Prev. 2001;10(4):287–301. [PubMed] [Google Scholar]
- 42.CDC. Physical activity and health. www.cdc.gov/physicalactivity/everyone/health/index.html#ReduceCancer.
- 43.National Cancer Institute. Physical activity and cancer. www.cancer.gov/cancertopics/factsheet/prevention/physicalactivity.
- 44.CDC. BRFSS Crosstabulation 2010 data. apps.nccd.cdc.gov/s_broker/WEATSQL.exe/weat/freq_Year.hsql.
- 45.Courneya KS, Katzmarzyk PT, Bacon E. Physical activity and obesity in Canadian cancer survivors. Cancer. 2008;112(11):2475–2482. doi: 10.1002/cncr.23455. [DOI] [PubMed] [Google Scholar]
- 46.Ory MG, Jordan PJ, Bazzarre T. The behavior change consortium: setting the stage for a new century of health behavior-change research. Health Educ Res. 2002;17(5):500–511. doi: 10.1093/her/17.5.500. http://her.oxfordjournals.org/content/17/5/500.long. [DOI] [PubMed] [Google Scholar]
- 47.Ory MG, Smith ML, Mier N, Wernicke MM. The science of sustaining health behavior change: the health maintenance consortium. Am J Health Behav. 2010;34(6):647–659. doi: 10.5993/ajhb.34.6.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wilbur J, Vassalo A, Chandler P, McDevitt J, Miller AM. Midlife women's adherence to home-based walking during maintenance. Nurs Res. 2005;54(1):33–40. doi: 10.1097/00006199-200501000-00005. [DOI] [PubMed] [Google Scholar]
- 49.Marcus B, Forsyth LH, Stone EJ, Dubbert PM, McKenzie TL. Physical activity behavior change: issues in adoption and maintenance. Health Psychol. 2000;19(1):32–41. doi: 10.1037/0278-6133.19.suppl1.32. doi: http://dx.doi.org/10.1037/0278-6133.19.Suppl1.32. [DOI] [PubMed] [Google Scholar]
- 50.Kahn EB, Ramsey LT, Brownson RC, et al. The effectiveness of interventions to increase physical activity. AmJ Prev Med. 2002;22(4):73–107. doi: 10.1016/s0749-3797(02)00434-8. [DOI] [PubMed] [Google Scholar]
- 51.Heath GW, Brownson RC, Kruger J, Miles R, Powell KE, Ramsey LT. The effectiveness of urban design and land use and transport policies and practices to increase physical activity: a systematic review. J Phys Act Health. 2006;3:S55–S76. doi: 10.1123/jpah.3.s1.s55. [DOI] [PubMed] [Google Scholar]
- 52.CEO Roundtable on Cancer. CEO gold standard. www.cancergoldstandard.org/. [Google Scholar]