Abstract
Background
A National Spina Bifida Patient Registry (NSBPR) was begun in 2009 to help understand the natural history of spina bifida (SB) and the effects of treatments provided by SB clinics. We used the NSBPR to explore the relationship of sociodemographic characteristics with SB outcomes.
Methods
Using NSBPR data collected in 2009 to 2012, we examined the unadjusted association between demographic characteristics and 4 SB outcomes: bowel continence, bladder continence, mobility, and presence of pressure sores. We then developed multivariable logistic models to explore these relationships while controlling for SB clinic, SB type, and level of lesion.
Results
Data were available on 2054 patients <22 years of age from 10 SB clinics. In the multivariable models, older age groups were more likely to have continence and pressure sores and less likely to be community ambulatory. Males and patients without private insurance were less likely to be continent and community ambulatory. Non-Hispanic blacks were less likely to be continent. Level of lesion was associated with all outcomes; SB type was associated with all but pressure sores; and all outcomes except community ambulation showed significant variation across clinic sites.
Conclusions
Sociodemographic attributes are associated with SB outcomes. In particular, males, non-Hispanic blacks, and patients without private insurance have less favorable outcomes, and age has an impact as well. These characteristics need to be considered by clinicians who care for this patient population and factored into case-mix adjustment when evaluating variation in clinical and functional outcomes among different SB clinics.
Advances in medical care and technology have resulted in greater expected longevity for infants born with spina bifida (SB).1 However, knowledge regarding the health status and long-term health outcomes of people with SB is limited. In 2005, the Spina Bifida Association collaborated with the Agency for Healthcare Research and Quality and the Centers for Disease Control and Prevention (CDC) to survey US SB programs regarding clinic operations and services, care processes, and disease outcomes of their patients. Based on this assessment and the experiences of other organizations (such as the Cystic Fibrosis Foundation2), a National SB Patient Registry (NSBPR) was established in 2009 to systematically gather data regarding the natural history of SB in patients attending SB clinics to support SB clinical research and to better understand the effects of treatments provided in SB programs across the United States.3
Clinicians participating in the development of the NSBPR have identified bowel and bladder continence, ambulation, and the occurrence of pressure sores as key clinical outcomes for patients with SB. The manifestations and consequences of SB depend to a great degree on intrinsic characteristics of the congenital defect, particularly lesion type and spinal cord level,1 but initial analyses of the NSBPR have shown significant variation in outcomes among patients even when stratifying by these intrinsic disease features. Socioeconomic and demographic characteristics are significant determinants of health outcomes in a number of chronic medical conditions and are therefore important components of case-mix adjustment when attempting to understand variations in disease outcomes.4–6 We used the NSBPR to determine the impact of sociodemographic and intrinsic lesion characteristics on functional outcomes for SB.
Methods
The NSBPR is a clinic-based registry designed to describe the patient population attending SB clinics and ascertain variations in processes of care that are associated with better health outcomes. Although this approach excludes individuals who do not seek care from multidisciplinary SB clinics, it does offer an opportunity to understand disease characteristics and perform credible analyses of clinical practices and outcomes in the large sample of patients who do attend these clinics. The assumption is that data provided from the clinics are reliable and that, by using the clinic as the unit of analysis, it will eventually be possible to obtain an accurate report of the variety of treatments typically provided to patients by specialized clinics and a clear picture of the relationship between these treatments and health outcomes.
In 2008, the CDC solicited applications from multidisciplinary SB clinics that had participated in earlier exploratory efforts to examine the feasibility of using a standardized tool to collect information on patients with SB attending these clinics.3 Between September 2008 and August 2009, 9 SB clinic sites (1 site included 2 clinics, for a total of 10 clinics), each being multidisciplinary and serving a minimum of 250 patients, were funded to participate in the registry and report longitudinal data on patients having 1 of 4 diagnoses (myelomeningocele, meningocele, lipomyelomeningocele, or fatty filum). Approval was obtained from local institutional review boards, and informed consent (and/or assent, as indicated by age) was obtained from parents and patients. Sites were encouraged but not required to enroll all SB patients; aggregate demographic data on patients not enrolled are collected for comparison with the enrollees. An initial encounter form is used at the patient's enrollment into the registry to collect baseline demographic and diagnostic information as well as a history of selected surgical procedures; an annual visit form, completed at enrollment and at each subsequent visit, collects updated information on time-varying demographic and clinical characteristics and treatments. Data entry uses a web-based electronic medical record that provides a reliable, standardized method for data collection and management for the clinics participating in the registry. Patient data are obtained through medical record abstraction and patient interview, deidentified, and transmitted to the CDC for data management and analysis. A number of systematic procedures are implemented at clinic sites and the CDC Data Management Center to ensure data quality.3
We accessed NSBPR data collected in 2009 to 2012, using information collected at the initial registry visit on each individual patient. We restricted the analysis to patients <22 years of age because the participating SB clinics were primarily pediatric, and only a few followed adult patients.
SB Lesion Characteristics
Registry enrollment forms query the patient's SB type and allow 1 of 4 categories to be chosen: myelomeningocele, meningocele, lipomyelomeningocele, or fatty filum. After an initial examination of the individual diagnostic categories, we grouped patients as having myelomeningocele or nonmyelomeningocele for this analysis. Level of lesion is queried on each annual visit form, and is based on functional neurologic exam rather than the reported anatomic location of the lesion. Five categories are provided in the registry: thoracic (flaccid lower extremities); high-lumbar (hip flexion present); midlumbar (knee extension present); low-lumbar (foot dorsiflexion present); sacral (foot plantar flexion present).
Sociodemographic Characteristics
Patient age was calculated from the birthday and the date of the annual visit from which clinical data were derived. Gender, race, and ethnicity were reported by clinicians; patients were classified by race on the data collection forms as white, black or African American, Asian, American Indian or Alaska Native, Native Hawaiian, or other, and by ethnicity as “Hispanic or Latino” or “not Hispanic or Latino.” These were consolidated for our analysis into 3 categories: Hispanic (of any race), non-Hispanic black, and other (combined owing to the small number of Asians, Native Americans, and Hawaiians and their similarity to whites in the characteristics of interest in this analysis). We were interested in the potential impact of socioeconomic status (SES) on outcomes; the registry contains no information on family income, zip code of residence, or parental education or occupation. Therefore, we used insurance status as a proxy measure of SES. Patients who reported having health insurance for which they or their employer contributed premiums (specifically described as straight commercial insurance, commercial insurance health maintenance organization [HMO], commercial insurance preferred provider organization, or tricare other military) were classified as having private insurance, even if they were also reported to have public assistance (described as straight Medicaid, Medicaid HMO, straight Medicare, Medicare HMO, or insurance related to local/specialty/charity care, financial assistance), and compared with those who were reported as not having any form of private health insurance.
Clinical Outcomes
The registry defines patients as continent of urine if they were reported to be dry, with or without interventions, during the day, and continent of stool if they reported no involuntary stool leakage, with or without interventions, during the day. Our analysis of continence was restricted to patients ≥5 years of age and included patients who achieved continence without intervention (ie, those for whom SB did not affect continence). Four categories of ambulation were reported: community ambulatory (CA) (describing individuals who are ambulatory in the community ie, the individual walks indoors and outdoors for most activities and may need crutches or braces or both and uses a wheelchair only for long trips out of the community); household ambulatory (the individual walks only indoors and with apparatus; is able to get in and out of the chair and bed with little if any assistance; and may use a wheelchair for some indoor activities at home and school and for all activities in the community); therapeutic ambulatory (the individual walks only for therapy sessions, in school or in the hospital, and uses a wheelchair to get from place to place and to satisfy all needs for transportation); and nonambulatory (the individual uses a wheelchair exclusively for mobility but usually can transfer from chair to bed and other surfaces). For purposes of our analysis, a dichotomous classification of ambulation was used, comparing patients who were reported to be CA versus others, and patients <2 years of age were excluded. Pressure sores were reported if any had been present over the previous 12 months or since the last SB clinic visit.
Analysis
Statistical analyses were performed by using SAS version 9.3. Associations in cross tabulations were tested for statistical significance using χ2 tests. Separate multiple logistic regression models were developed to estimate the association of sociodemographic variables with each clinical outcome, controlling for SB type, level of lesion, and SB care center as fixed effects. All reported models incorporated all of these variables to allow us to evaluate their significance in relation to each outcome (and to maintain consistency). Statistical tests were all 2-sided, and P values ≤.05 were considered significant; 95% confidence intervals (CIs) were calculated for all point estimates.
To assess for the presence of selection bias, we compared the distribution of sociodemographic and clinical characteristics between eligible but unenrolled patients and those enrolled at all sites. When we found that some clinics showed differences between those enrolled and those not, we attempted to assess the sensitivity of our findings to selection bias. First, we replicated our analysis excluding the 2 sites that enrolled the smallest proportion of patients they followed, and then we repeated the analysis with just the 5 participating sites that showed no differences in any of the characteristics between the enrolled and the eligible but unenrolled patients.
Results
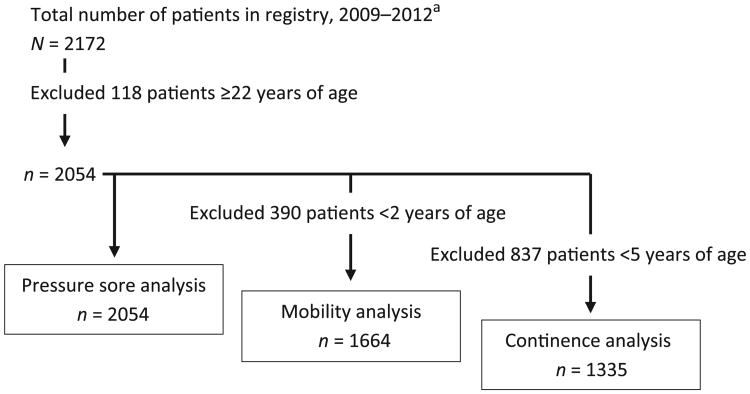
The registry contained data on 2172 patients from 10 SB centers, of whom 2054 were <22 years old (median age 8.3 years, mean 8.9 years, range from newborn to 21.9 years). Table 1 displays the characteristics of this population. Figure 1 shows a flow diagram of the subjects included in each analysis.
Table 1. Distribution of Selected Demographic, Clinical, and Insurance Characteristics Among Participants (N = 2054), Ages Newborn to <22 Years: NSBPR, 2009–2012.
| Characteristic | n (%) |
|---|---|
| Age group, y | |
| <2 | 373 (18.2) |
| 2 to <5 | 346 (16.8) |
| 5 to <10 | 454 (22.1) |
| 10 to <13 | 252 (12.3) |
| 13 to <18 | 419 (20.4) |
| 18 to <22 | 210 (10.2) |
| Gender | |
| Male | 979 (47.7) |
| Female | 1075 (52.3) |
| Race/ethnicitya | |
| Hispanic | 509 (24.8) |
| Non-Hispanic black | 159 (7.7) |
| Other | 1384 (67.4) |
| Health insuranceb | |
| Any private | 963 (46.9) |
| No private | 1090 (53.1) |
| Functional level of lesion | |
| Thoracic | 289 (14.1) |
| High-lumbar | 201 (9.8) |
| Midlumbar | 550 (26.8) |
| Low-lumbar | 379 (18.5) |
| Sacral | 635 (30.9) |
| Spina bifida type | |
| Myelomeningocele | 1657 (80.7) |
| Nonmyelomeningocele | 397 (19.3) |
| Bowel continence, age 5+c | 569 (42.6) |
| Bladder continence, age 5+c | 507 (38.0) |
| Mobility status, age 2+d | |
| CA | 920 (55.3) |
| Household ambulatory | 137 (8.2) |
| Nonfunctional ambulatory | 139 (8.4) |
| Nonambulatory | 468 (28.1) |
| Pressure sore | 283 (13.8) |
| Care center | |
| Alabama | 381 (18.5) |
| California | 271 (13.2) |
| Colorado | 228 (11.1) |
| Connecticut | 74 (3.6) |
| Indiana | 242 (11.8) |
| Massachusetts | 72 (3.5) |
| Ohio | 246 (12.0) |
| Oregon | 172 (8.4) |
| Washington | 196 (9.5) |
| Wisconsin | 172 (8.4) |
N = 2052.
N = 2053.
N = 1335.
N = 1664.
Figure 1.
Participant flow diagram. aThe total number of patients followed at the participating SB clinics during the time period covered by this report is unknown. In 2012, the total number of patients seen by the clinics was 1913, and the total number reported in the registry was 1602 (84.2%).
Table 2 shows simple associations between outcomes and demographic and clinical variables. As expected, all outcomes had a statistically significant association with SB type and level of lesion.
Table 2. Unadjusted Associations Between Outcomes and Sociodemographic and Clinical Variables for Patients Included in this Study: NSBPR, 2009–2012.
| Variable | Bowel Continence (N = 1335)a | Urinary Continence (N = 1335)a | CA (N = 1664)b | Pressure Sores (N = 2054) | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Yes, % | P | Yes, % | P | Yes, % | P | Any, % | P | |
| Overall | 42.6 | 38.0 | 55.3 | 13.8 | ||||
| Age, y | <.0001 | <.0001 | <.0001 | < 0001 | ||||
| <2 | 1.6 | |||||||
| 2 to <5 | 63.0 | 7.8 | ||||||
| 5 to <10 | 33.5 | 30.0 | 63.7 | 13.2 | ||||
| 10 to <13 | 44.4 | 35.7 | 55.6 | 19.0 | ||||
| 13 to <18 | 48.4 | 45.1 | 46.4 | 22.7 | ||||
| 18 to <22 | 48.6 | 43.8 | 42.4 | 22.4 | ||||
| Gender | .0092 | .0277 | .0757 | .5200 | ||||
| Male | 38.8 | 34.9 | 53.0 | 14.3 | ||||
| Female | 46.0 | 40.8 | 57.3 | 13.3 | ||||
| Race/ethnicity | <.0001 | .0022 | .8300 | .1108 | ||||
| Hispanic | 36.6 | 34.1 | 55.9 | 11.8 | ||||
| Non-Hispanic black | 25.5 | 25.5 | 57.3 | 18.2 | ||||
| Other | 46.9 | 40.8 | 54.8 | 13.9 | ||||
| Private insurance | <.0001 | <.0001 | <.0001 | .0467 | ||||
| Any | 52.2 | 45.4 | 61.3 | 12.1 | ||||
| None | 34.8 | 31.8 | 50.1 | 15.2 | ||||
| Level of lesion | <.0001 | <.0001 | <.0001 | <.0001 | ||||
| Thoracic | 33.3 | 31.4 | 0.8 | 23.9 | ||||
| High-lumbar | 42.2 | 34.4 | 6.6 | 17.9 | ||||
| Midlumbar | 34.7 | 33.1 | 42.2 | 19.1 | ||||
| Low-lumbar | 42.5 | 35.5 | 81.3 | 10.3 | ||||
| Sacral | 55.8 | 49.0 | 96.0 | 5.4 | ||||
| SB type | <.0001 | <.0001 | <.0001 | <.0001 | ||||
| Myelomeningocele | 38.4 | 34.6 | 46.3 | 15.6 | ||||
| Non-myelomeningocele | 61.7 | 53.1 | 92.6 | 6.3 | ||||
Continence analyses were limited to patients ≥5 y old.
Limited to patients ≥2 y old.
CA - Community Ambulation.
Our cross-sectional comparison of patients in different age groups showed a stepwise increase in continence and the prevalence of pressure sores with age, leveling off to be similar in adolescents and young adults. In contrast, the prevalence of community ambulation was similar in younger compared with older children in the first decade of life, but then progressively decreased in the later childhood, adolescent, and young adult age groups.
Females were more likely to have bowel and urinary continence and were borderline more likely to be CA, but were no different from males in the prevalence of pressure sores. Non-Hispanic black patients with SB were least likely to have bladder and bowel continence, and Hispanics were less likely than non-Hispanics. There was no association of race/ethnicity with mobility status or prevalence of pressure sores. Patients with private insurance were more likely to be continent and to be CA and less likely to have reported any pressure sores.
In the multivariable logistic models (Fig 2 A-D), most of the bivariate associations remained statistically significant. Age showed a statistically significant relationship with continence and pressure sores and with CA, which peaked in middle childhood. Females were more likely than males to have bowel continence (adjusted odds ratio [aOR] 1.34, 95% CI 1.08–1.67) or urinary continence (aOR 1.29, 95% CI 1.03–1.61) and be CA (aOR 1.54, 95% CI 1.14–2.08). Patients without private insurance were less likely than those with private insurance to have bowel continence (aOR 0.49, 95% CI 0.39–0.61) or urinary continence (aOR 0.56, 95% CI 0.45–0.70), less likely to be CA (aOR 0.68, 95% CI 0.49–0.95), and borderline more likely to have pressure sores (aOR 1.27, 95% CI 0.95–1.71). Non-Hispanic blacks were less likely than others to have bowel continence (aOR 0.37, 95% CI 0.22–0.60) and urinary continence (aOR 0.50, 95% CI 0.31–0.78). Level of lesion was significantly associated with all outcomes; SB type was significantly associated with all outcomes except pressure sores; and all outcomes except community ambulation showed significant variation across clinic sites (data not shown).
Figure 2.
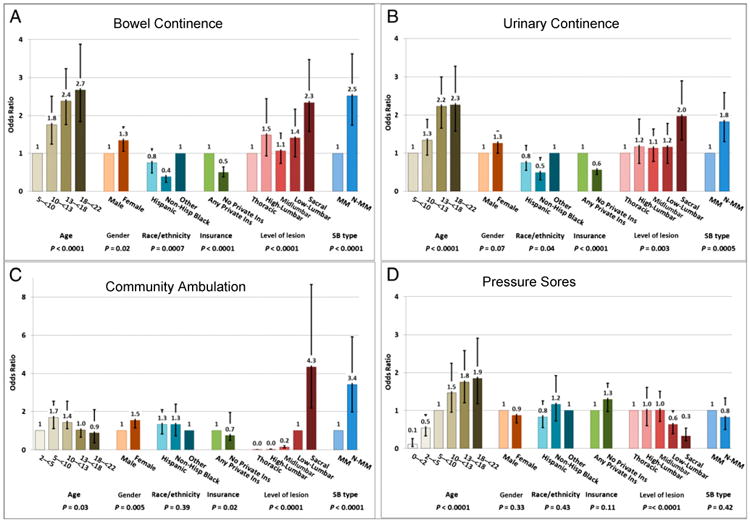
Odds ratio (with CIs) of outcomes associated with sociodemographic and SB characteristics from the multivariable logistic model. For purposes of clarity in the figures, the age reference group for the continence and pressure sore models was 5 to <10 years, and for the community ambulation model, 2-<5 years. The level of lesion reference group for the continence and pressure sores models was thoracic, and for the community ambulation model, low lumbar. For all models, the reference group for gender was male; for race/ethnicity, other; for insurance, any private; and for SB type, myelomeningocele. Hisp, Hispanic; Ins, insurance; MM, myelomeningocele; N-MM, nonmyelomeningocele.
The overall percentage of eligible individuals enrolled in the 2012 NSBPR was 83.7% and ranged, by site, from 63.2% to 99.1%. When the 2 sites with the lowest percentages of enrollment were excluded from the analysis, 1541 eligible individuals remained. When the analysis was limited to the 5 sites that showed no statistically significant differences between enrolled and eligible but unenrolled for any of the characteristics we analyzed, 945 eligible individuals remained. There was no substantive difference in the results of any of the analyses using either restricted group rather than the entire group. The results of these sensitivity analyses are shown in Supplemental Table 3.
Discussion
It is well appreciated that functional outcomes of SB depend in large part on intrinsic characteristics of the congenital defect, specifically the type and spinal level of the lesion.1 This analysis of the NSBPR confirms the preeminent importance of these characteristics, but also shows that after controlling for them, there is still variation in outcomes that is associated with demographic characteristics (age, gender, race, and ethnicity) and health insurance status. Females with SB are more likely than males to be continent and ambulatory; patients with private insurance are also more likely to be continent and ambulatory; and (after controlling for insurance status as a proxy measure of SES) patients with SB who are non-Hispanic black appear less likely to be continent. The incidence of pressure sores is primarily dependent on age and level of lesion, although there is a borderline increased propensity to develop pressure sores in patients without private insurance. There also appears to be significant variation in these outcomes by SB care site, but because of differences in enrollment that may be a source of bias, we are not currently confident in our ability to accurately quantify that variation.
People with SB experience a host of potentially modifiable condition-specific medical complications and functional abnormalities, but current knowledge regarding the health status and long-term health outcomes of people with SB is limited. Prior attempts to collect SB-related patient information have used small convenience or clinic samples, which limit generalizability. The NSBPR was created to describe the patient population attending SB clinics, to help understand the natural history of the condition and risk factors associated with adverse outcomes, and to seek out variations in health outcomes and the processes of care that are associated with these outcomes.3 Our analysis represents an initial attempt to understand the causes of variation in outcomes that are seen in people with SB. The role and relative impact of these risk factors on health outcomes are important to counsel patients regarding expectations and treatment, and also to make the proper case-mix adjustments when comparing outcomes across care sites and evaluating the effect of new treatments before introducing them into practice.
There are important potential limitations to our analysis. The NSBPR is relatively new, and although a host of safeguards have been incorporated into its data collection process, it continues to undergo improvements and modifications to ensure the validity of its data.3 Whereas clear definitions are provided for the functional outcomes that we have analyzed, these are still potentially subject to variation in their interpretation and reporting by different individuals at different care sites. This raises particular caveats when attempting to compare outcomes from different centers. Furthermore, selection bias may be a threat to external validity: our registry is clinic based, so it may not be representative of SB patients who do not attend SB clinics. It is likely, for example, that more severely involved SB patients continue to be followed at regional SB centers on a more regular basis than those with milder involvement. It is also possible that the clinics participating in the registry are not representative of SB clinics in general. We made no attempt to ensure representativeness in choosing centers for participation in the registry, and in fact our insistence that they be multidisciplinary in structure and function and show a history of interest in this effort may limit the generalizability of our findings beyond clinics based at a university medical center with an active interest in spina bifida. However, we believe that this probably characterizes the majority of spina bifida clinics in the United States.
In addition, selection bias may be a threat to internal validity: participating clinics enrolled most but not all of their eligible patients, raising concerns that those who are eligible but not contributing data may be somehow different from those who are.7 In an attempt to evaluate the possible impact of this bias, we reran our analysis omitting the 2 sites that had the lowest proportion of enrolled eligible patients, and again reran it to include only the 5 sites that showed no suggestion of any selection bias in patient enrollment, and we found no substantive difference in the results. Our concerns about differential information and selection bias among the different sites led to a decision to delay direct quantitative comparisons across care sites until we have more information regarding consistency of data reporting and the reasons for variation in recruitment of patients into the registry.
SES of the parents has been reported in a number of studies to be associated with the likelihood of having a child with SB;8,9 there is one report of an association of ethnicity and SES on postnatal cognitive achievement in children with SB.10 We used insurance status as a proxy measure of SES, as no direct measures of SES such as family income are available in the NSBPR. Specifically, we believe that the disparities we found between patients with and without private insurance were a reflection of income, resources, or employment that distinguished families holding private insurance from those who did not, rather than differences in services, equipment, or medication made available by payers. The most appropriate measure of SES has not been settled and is dependent on context,11 but public versus private insurance status has been successfully used as a proxy measure to determine the health impact of SES in other chronic health conditions.12,13 The impact of SES on health is well established; an understanding of the mechanism of this relationship has developed gradually,6 but does appear to be specific to particular populations. For example, the linkage of SES and ethnicity to maternal dietary folate is an important explanation of disparities in the incidence of SB14 but is likely not an important explanation for differences in continence and ambulation in SB. Compromised access to care is an important explanation for health disparities in patients with asthma15 but not in those with cystic fibrosis;16 the relative importance of access to care needs to be explored in the SB population. Most importantly, SES-related gradients in health behaviors17 and disease self-management skills due to differences in health literacy18 exposure to and experience of stress,19 availability of community and family resources,20 and other “social determinants of health”21 contribute to and are likely influential as a cause of health disparities in the SB population.22 The apparent racial/ethnic disparities we found in our analysis need further investigation; they may be due to residual confounding from SES, given that our insurance variable is probably an incomplete proxy for SES.5
The explanation for our finding that females are more likely than males to be continent and ambulatory is unclear. It may be explained by biology (eg, hormonal and/or anatomic differences), by differing cultural norms and social expectations of girls versus boys in regard to these functions, or by a combination of the two.23,24
Finally, the variation in outcomes that appears to exist among SB care centers is an expected but critically important finding, mirroring what has been found across the health care spectrum.25 The causes of this variation need to be explored in more detail, which is one of the motivations for this work. There is heterogeneity in the distribution of risk factors, and this analysis will allow us to begin to develop a reliable case-mix adjustment. As previously noted, selection bias, imprecision in data collection, and any center-related differences in data reporting need to be minimized to ensure that our comparisons will be valid. Once that is accomplished, we believe that analysis of the NBSPR will allow the ascertainment of better outcomes at some SB care centers that will lead to the suggestion of preferred approaches to care.
Conclusions
Sociodemographic attributes are associated with SB functional outcomes. In particular, males and non-Hispanic blacks have less favorable outcomes, and those with any private insurance appear to have better outcomes. The association with insurance status is likely a reflection of socioeconomic disparities overall, and the potential explanations for this, such as barriers in access to care or deficiencies in health literacy and disease self-management, need further investigation. Sociodemographic factors need to be considered by clinicians who care for this patient population and by researchers who consider new interventions to improve outcomes. In addition, they need to be factored into case-mix adjustment when evaluating variation in disease outcomes among different SB clinics.
Supplementary Material
Supplemental Table 3 Comparison of Results of Models Incorporating All 10 Sites Contributing Data to the SB Registry and Either the 8 sites With the Highest Enrollment Percentage or the 5 sites With No Statistical Evidence of Enrollment Bias
What's Known on this Subject
Functional capabilities in patients with spina bifida depend on the spinal level of the lesion and its type. Sociodemographic characteristics have been shown in other conditions to be an important additional influence on outcomes, making them important for risk adjustment.
What this Study Adds
Males, non-Hispanic blacks, and patients without private insurance have less favorable functional outcomes in spina bifida, and age also has an impact. These attributes need to be considered by clinicians and researchers and used in comparing care outcomes across clinic settings.
Acknowledgments
Funding: Funded by grant #1UO1DDD000744.01, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention.
Footnotes
Dr. Schechter conceptualized and designed the analysis and drafted the initial manuscript; Dr Liu contributed to design and performed the analysis; Drs Soe and Swanson contributed to the interpretation of data; Drs Ward and Thibadeau contributed to the acquisition and interpretation of data; all authors revised the manuscript critically for important intellectual content, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Data from the National Spina Bifida Patient Registry used in this analysis were alluded to in the following publication: Thibadeau JK, Ward EA, Soe MM, Liu T, Swanson M, Sawin KJ, Freeman KA, Castillo H, Rauen K, Schechter MS. Testing the feasibility of a National Spina Bifida Patient Registry.
Financial Disclosure: The authors have indicated they have no financial relationships relevant to this article to disclose.
Potential Conflict of Interest: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA. Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg. 2001;34(3):114–120. doi: 10.1159/000056005. [DOI] [PubMed] [Google Scholar]
- 2.Schechter MS, Gutierrez HH. Improving the quality of care for patients with cystic fibrosis. Curr Opin Pediatr. 2010;22(3):296–301. doi: 10.1097/MOP.0b013e328339550e. [DOI] [PubMed] [Google Scholar]
- 3.Thibadeau JK, Ward EA, Soe MM, et al. Testing the feasibility of a National Spina Bifida Patient Registry. Birth Defects Res A Clin Mol Teratol. 2013;97(1):36–41. doi: 10.1002/bdra.23094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 5.LaVeist TA. Disentangling race and socioeconomic status: a key to understanding health inequalities. J Urban Health. 2005;82(2 suppl 3):iii26–iii34. doi: 10.1093/jurban/jti061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adler NE, Stewart J. Health disparities across the lifespan: meaning, methods, and mechanisms. Ann N Y Acad Sci. 2010;1186:5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- 7.Schechter MS. Patient registry analyses: seize the data, but caveat lector. J Pediatr. 2008;153(6):733–735. doi: 10.1016/j.jpeds.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 8.Wasserman CR, Shaw GM, Selvin S, Gould JB, Syme SL. Socioeconomic status, neighborhood social conditions, and neural tube defects. Am J Public Health. 1998;88(11):1674–1680. doi: 10.2105/ajph.88.11.1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang J, Carmichael SL, Canfield M, Song J, Shaw GM National Birth Defects Prevention Study. Socioeconomic status in relation to selected birth defects in a large multicentered US case-control study. Am J Epidemiol. 2008;167(2):145–154. doi: 10.1093/aje/kwm283. [DOI] [PubMed] [Google Scholar]
- 10.Swartwout MD, Garnaat SL, Myszka KA, Fletcher JM, Dennis M. Associations of ethnicity and SES with IQ and achievement in spina bifida meningomyelocele. J Pediatr Psychol. 2010;35(9):927–936. doi: 10.1093/jpepsy/jsq001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 12.Joshi S, Gaynor JJ, Bayers S, et al. Disparities among Blacks, Hispanics, and Whites in time from starting dialysis to kidney transplant waitlisting. Transplantation. 2013;95(2):309–318. doi: 10.1097/TP.0b013e31827191d4. [DOI] [PubMed] [Google Scholar]
- 13.Schechter MS, Shelton BJ, Margolis PA, Fitzsimmons SC. The association of socioeconomic status with outcomes in cystic fibrosis patients in the United States. Am J Respir Crit Care Med. 2001;163(6):1331–1337. doi: 10.1164/ajrccm.163.6.9912100. [DOI] [PubMed] [Google Scholar]
- 14.Agha MM, Glazier RH, Moineddin R, Moore AM, Guttmann A. Food fortification and decline in the prevalence of neural tube defects: does public intervention reduce the socioeconomic gap in prevalence? Int J Environ Res Public Health. 2013;10(4):1312–1323. doi: 10.3390/ijerph10041312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halfon N, Newacheck PW. Childhood asthma and poverty: differential impacts and utilization of health services. Pediatrics. 1993;91(1):56–61. [PubMed] [Google Scholar]
- 16.Schechter MS, McColley SA, Silva S, Haselkorn T, Konstan MW, Wagener JS Investigators and Coordinators of the Epidemiologic Study of Cystic Fibrosis; North American Scientific Advisory Group for ESCF. Association of socioeconomic status with the use of chronic therapies and healthcare utilization in children with cystic fibrosis. J Pediatr. 2009;155(5):634–639. e1–e4. doi: 10.1016/j.jpeds.2009.04.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gazmararian JA, Adams MM, Pamuk ER. Associations between measures of socioeconomic status and maternal health behavior. Am J Prev Med. 1996;12(2):108–115. [PubMed] [Google Scholar]
- 18.Yin HS, Dreyer BP, Vivar KL, MacFarland S, van Schaick L, Mendelsohn AL. Perceived barriers to care and attitudes towards shared decision-making among low socioeconomic status parents: roleof health literacy. Acad Pediatr. 2012;12(2):117–124. doi: 10.1016/j.acap.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson SB, Riley AW, Granger DA, Riis J. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics. 2013;131(2):319–327. doi: 10.1542/peds.2012-0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organization; 2008. [Google Scholar]
- 22.Pincus T, Esther R, DeWalt DA, Callahan LF. Social conditions and self-management are more powerful determinants of health than access to care. Ann Intern Med. 1998;129(5):406–411. doi: 10.7326/0003-4819-129-5-199809010-00011. [DOI] [PubMed] [Google Scholar]
- 23.Bird CE, Rieker PP. Gender matters: an integrated model for understanding men's and women's health. Soc Sci Med. 1999;48(6):745–755. doi: 10.1016/s0277-9536(98)00402-x. [DOI] [PubMed] [Google Scholar]
- 24.Willis E, Miller R, Wyn J. Gendered embodiment and survival for young people with cystic fibrosis. Soc Sci Med. 2001;53(9):1163–1174. doi: 10.1016/s0277-9536(00)00416-0. [DOI] [PubMed] [Google Scholar]
- 25.Goodman DC. Unwarranted variation in pediatric medical care. Pediatr Clin North Am. 2009;56(4):745–755. doi: 10.1016/j.pcl.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 3 Comparison of Results of Models Incorporating All 10 Sites Contributing Data to the SB Registry and Either the 8 sites With the Highest Enrollment Percentage or the 5 sites With No Statistical Evidence of Enrollment Bias