Abstract
Objective. Previous studies have shown that receiving diabetes self-management education (DSME) is associated with increased care utilization. However, the relationship between DSME duration and care utilization patterns remains largely unexamined. Our purpose is to characterize DSME duration and examine the relationship between DSME duration and clinical- and self-care utilization patterns.
Methods. The study sample included 1,446 adults who were ≥18 years of age, had diabetes, and had participated in the 2008 Florida Behavioral Risk Factor Surveillance System survey. Clinical- and self-care outcomes were derived using responses to the survey’s diabetes module and were based on minimum standards of care established by the American Diabetes Association. The outcomes examined included self-monitoring of blood glucose at least once per day; receiving at least one eye exam, one foot exam, A1C tests, and an influenza vaccination in the past year; and ever receiving a pneumococcal vaccination. DSME duration was categorized as no DSME, >0 to <4 hours, 4–10 hours, and >10 hours.
Results. After adjusting for sociodemographic variables, compared to those who did not receive DSME, those who had 4–10 or 10+ hours of DSME were more likely to receive two A1C tests (odds ratio [95% CI] 2.69 [1.30–5.58] and 2.63 [1.10–6.31], respectively) and have a pneumococcal vaccination (1.98 [1.03–3.80] and 1.92 [1.01–3.64], respectively). Those receiving 10+ hours of DSME were 2.2 times (95% CI 1.18–4.09) as likely to have an influenza vaccination.
Conclusion. These data reveal a positive relationship between DSME duration and utilization of some diabetes clinical care services.
Diabetes has many debilitating and lethal consequences, including kidney failure, nontraumatic lower-extremity amputations, blindness, heart disease, and stroke. According to data from the National Health Interview Survey from January to June 2013, the prevalence of diagnosed diabetes was 9.3% among U.S. adults ≥18 years of age (1). Because of the increasing prevalence of diabetes, disease management is becoming increasingly important to improve the health and well-being of people with diabetes and to minimize the disease’s impact on the health care system. Diabetes-related costs are enormous. In 2012, direct medical costs associated with diabetes in the United States were $176 billion and indirect costs were $69 billion. Overall, the direct medical costs for people with diagnosed diabetes are more than twice those of people without diabetes (2).
In response to this national epidemic, Healthy People 2020’s strategic framework for improving the nation’s health includes diabetes self-management education (DSME) as one of its diabetes-related objectives (3,4). DSME is a collaborative effort between people with or at risk for diabetes and diabetes educators. The goal is to increase the knowledge and skills of people with diabetes to help them successfully self-manage the disease (5). In 2011, a joint American Association of Diabetes Educators/American Diabetes Association task force convened to update the National Standards for Diabetes Self-Management Education. Much of the work of this task force involved updating infrastructure, data collection, evaluation, and program coordination standards. Standard 6 addresses DSME curriculum content, but DSME duration recommendations are not included in the recommendations outlined by this standard (6).
Studies show that effective diabetes self-management significantly reduces both complications and health care costs (4,7–9). In a Florida-specific study, the authors found that receiving DSME is positively associated with receiving more comprehensive diabetes clinical care (10).
Whereas DSME has been repeatedly shown to increase awareness of recommended diabetes services and is associated with receiving higher levels of comprehensive clinical care, much less is known about the association between time spent receiving DSME (DSME duration) and diabetes self-management and clinical service utilization outcomes (11,12). A few articles have been published examining the relationship between DSME duration and diabetes-related outcomes. One study of insurance billing records showed a dose-response relationship between the number of DSME encounters (0–2 or more) and the proportion of patients complying with A1C and lipid panel testing recommendations (11). This study did not use a representative sample and only examined those receiving DSME from accredited programs versus those who did not receive DSME. In a meta-analysis of randomized clinical trials, the authors found that additional contact time between a participant and an educator resulted in a greater decrease in A1C (13). The meta-analysis did not examine health care utilization patterns stratified by patient-educator contact time.
The aim of this study was to examine clinical- and self-care utilization patterns among those receiving varying numbers of hours of DSME, using data from a population-based, representative sample of Florida adults with diagnosed diabetes.
Methods
This study used data from the 2008 Florida Behavioral Risk Factor Surveillance System (BRFSS). The BRFSS is an ongoing, telephone-based survey of noninstitutionalized adults in households in the United States and its territories. The BRFSS was established in 1984 and designed to monitor behavioral risks in the sampled population. The BRFSS is funded by the Centers for Disease Control and Prevention and administered by state-based health departments. A sample of telephone numbers within each state is randomly selected using a disproportionate stratified sample design to obtain a probability sample (14,15). Each state uses trained interviewers to collect data, which, when weighted, are representative of the state’s noninstitutionalized adult population ≥18 years of age (14). In addition to socioeconomic questions, the BRFSS survey instrument contains questions about a variety of health topics, including overall health status, chronic health conditions (including diabetes), disability, oral health, cancer screening, physical activity, nutrition, immunization, and mental health. State health departments are allowed to include state-added questions in response to emerging issues and to collect additional data on a specific topic. This study used answers to the diabetes-related BRFSS questions listed in Table 1 (16).
TABLE 1.
Diabetes-Related Questions From the 2008 Florida BRFSS That Were Used in This Study*
| Question | Response Options | Who Was Asked? |
| Have you ever been told by a doctor that you have diabetes? | 1 = yes; 2 = yes, during pregnancy; 3 = no; 4 = no, prediabetes/borderline; “don’t know/not sure” and “refused” responses were considered missing data | All respondents |
| Are you now taking insulin? | 1 = yes; 2 = no; “don’t know/not sure” and “refused” responses were considered missing data | All respondents with diagnosed diabetes |
| About how often do you check your blood for glucose or sugar? | Respondents indicated the number of times per day, week, month, or year; average per day was calculated based on responses; “don’t know/not sure” and “refused” responses were considered missing data | All respondents with diagnosed diabetes |
| About how many times in the past 12 months has a doctor, nurse, or other health professional checked you for “A one C?” | Respondents indicated the number of times in the past 12 months; “don’t know/not sure” and “refused” responses were considered missing data | All respondents with diagnosed diabetes |
| About how many times in the past 12 months has a health professional checked your feet for any sores or irritations? | Respondents indicated the number of times in the past 12 months; “don’t know/not sure” and “refused” responses were considered missing data | All respondents with diagnosed diabetes |
| When was the last time you had an eye exam in which the pupils were dilated? | 1 = within the past month; 2 = within the past year; 3 = within the past 2 years; 4 = ≥2 years ago; 8 = never; “don’t know/not sure” and “refused” responses were considered missing data | All respondents with diagnosed diabetes |
| Have you ever taken a course or class in how to manage your diabetes yourself? | 1 = yes; 2 = no; “don’t know/not sure” and “refused” responses were considered missing data | All respondents with diagnosed diabetes |
| During the past 12 months, have you had a flu shot? Had the flu vaccine sprayed in the nose? | 1 = yes; 2 = no; “don’t know/not sure” and “refused” responses were considered missing data | All respondents |
| Have you ever had a pneumonia shot? | 1 = yes; 2 = no; “don’t know/not sure” and “refused” responses were considered missing data | All respondents |
| State-added: About how long did the course or class you took in how to manage your diabetes yourself last? | 1 = <1 hour; 2 = >1 but <4 hours; 3 = >4 but <8 hours; 4 = 8–10 hours; 5 = >10 hours; “don’t know/not sure” and “refused” responses were considered missing data | All respondents with diagnosed diabetes who indicated they had taken a self-management course |
Additional verbiage that appeared before or after questions to define specific terms has been omitted.
The single question ascertaining whether respondents had ever taken a class or course in how to manage their diabetes allows public health systems to monitor the percentage of adults with diabetes who receive DSME on a state and national level. There are two significant problems with using this question: first, one cannot determine the quality of and setting for DSME delivery; and, second, one cannot quantify DSME duration for each respondent. A state-added question included in the 2008 Florida BRFSS survey attempted to quantify DSME duration but did not attempt to ascertain DSME quality and setting. Respondents who indicated they had ever taken a course or class in how to manage diabetes were asked to respond to the state-added question listed in Table 1 (17). Of the 1,446 respondents with diagnosed diabetes, 1,445 (99.9%) had valid responses to the diabetes module’s DSME question, and 1,335 (92.3%) had valid responses to the state-added DSME duration question. To our knowledge, Florida is the only state that has used this state-added question.
From the responses to this added question, the independent variable of interest, DSME duration, was categorized in the following manner: no DSME, >0 to <4 hours, 4–10 hours, and >10 hours. Several dichotomous (yes/no) dependent variables were examined using data from corresponding questions listed in Table 1: engaged in self-monitoring of blood glucose (SMBG) at least once per day on average (engaged in SMBG); received at least one dilated retinal exam in the past year (annual eye exam); received at least one foot exam by a health care professional in the past year (annual foot exam); received at least two A1C tests in the past year (two HbA1c tests); received an influenza vaccination either by injection or spray in the past year (annual flu shot); ever received a pneumococcal vaccination (one-time pneumococcal); and uses insulin. For each of the dependent variable questions, “don’t know” and “refused” were response options on the survey that were treated as missing data in the analyses. The data were weighted to account for nonresponse and were managed using SAS version 9.2 (SAS, Cary, N.C.). Descriptive, χ2, and logistic regression analyses were conducted using SUDAAN version 11.0 (SUDAAN, Research Triangle Park, NC).
The University of North Florida institutional review board approved the use of the 2008 Florida BRFSS data.
Results
The results of the analyses indicate that there are a number of statistically significant associations between DSME duration and the outcomes of interest. Because of the cross-sectional study design, causal relationships can-not be inferred.
Table 2 shows the number of respondents with diagnosed diabetes, the prevalence of diabetes by sociodemographic characteristics, and the percentage of each sociodemographic characteristic among those with diabetes. In addition, the table shows the percentage of adults with diabetes in each DSME duration category (among those with valid DSME duration responses). In Florida in 2008, the prevalence of diabetes was statistically significantly higher among those in the following subpopulations: non-Hispanic blacks, those ≥45 years of age, those with a high school education or less, those earning <$50,000 per year, and those with health insurance. Among those with valid DSME duration responses, 52.1% received no DSME, 22% had <4 hours of DSME, 14.8% had 4–10 hours of DSME, and 11.6% had >10 hours of DSME. The percentage receiving each level of the DSME duration did not vary significantly by sex, race/ethnicity, age-group, education level, income, or marital status (data not shown).
TABLE 2.
Diabetes Prevalence Among Adults by Sociodemographic Covariates and Distribution of Each Covariate Among Diagnosed Adults, Florida BRFSS 2008
| Covariate | n | Diabetes prevalence (%) | Within covariate P | Percentage among those with diagnosed diabetes |
| Had diagnosed diabetes | 1,446 | 9.5 | 100 | |
| Sex | 0.07 | |||
| Male | 600 | 10.4 | 52.5 | |
| Female | 846 | 8.7 | 47.5 | |
| Race/ethnicity | 0.01 | |||
| Non-Hispanic white | 1,103 | 9.0 | 63.7 | |
| Non-Hispanic black | 178 | 14.6 | 19.6 | |
| Hispanic | 85 | 7.9 | 16.7 | |
| Age-group (years) | <0.01 | |||
| 18–44 | 93 | 2.1 | 10.0 | |
| 45–64 | 586 | 13.5 | 45.7 | |
| ≥65 | 766 | 19.3 | 44.3 | |
| Education Level | <0.01 | |||
| Less than high school | 244 | 12.7 | 13.8 | |
| High school | 553 | 11.9 | 34.4 | |
| More than high school | 640 | 7.9 | 51.8 | |
| Annual income ($) | <0.01 | |||
| <25,000 | 604 | 14.5 | 41.7 | |
| 25,000 to <50,000 | 362 | 10.5 | 29.5 | |
| ≥50,000 | 316 | 6.2 | 28.8 | |
| Married or cohabiting | 0.33 | |||
| Yes | 750 | 9.2 | 61.1 | |
| No | 691 | 10.1 | 38.9 | |
| Has health insurance | <0.01 | |||
| Yes | 1,301 | 10.2 | 88.1 | |
| No | 141 | 6.5 | 11.9 | |
| Uses insulin | ||||
| Yes | 390 | NA | NA | 24.9 |
| No | 1,055 | NA | NA | 75.1 |
| DSME duration among valid responses (hours) | ||||
| 0 | 705 | NA | NA | 52.1 |
| >0 to <4 | 259 | NA | NA | 22.0 |
| 4–10 | 202 | NA | NA | 14.8 |
| >10 | 169 | NA | NA | 11.6 |
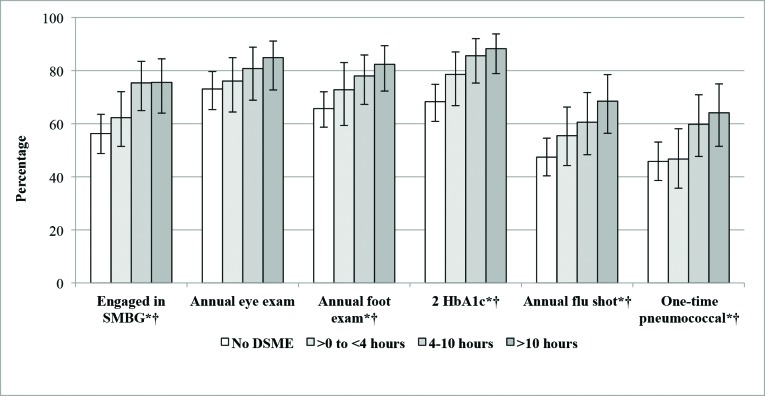
Figure 1 shows the percentage of adults who received services or engaged in self-management practices by DSME duration category.The percentage who engaged in SMBG varied significantly by DSME duration category (P <0.05). The percentage engaging in SMBG was highest among those who received ≥4 hours of DSME. Although the percentage who had an annual eye exam increased with increasing DSME duration, the differences were not statistically significant. The percentages of individuals who had an annual foot exam, had at least two A1C tests in the past year, and had received an annual influenza vaccination had positive dose-response relationships with DSME duration (all P <0.05). The percentages of individuals who received a one-time pneumococcal vaccination varied significantly by DSME duration category (P <0.05). The percentage receiving this vaccination was highest among those who received ≥4 hours of DSME. Each of the dependent variables was statistically significant for trend, with the exception of annual eye exams, suggesting a dose-response relationship between DSME duration and these dependent variables.
FIGURE 1.
Percentage of Florida adults with diagnosed diabetes who received services or engaged in self-management practices by DSME duration category, Florida BRFSS 2008.
*Statistically significant differences between categories within variables (P <0.05). †Statistically significant trend (P <0.05).
Table 3 shows the adjusted odd ratios (ORs) for receiving services or engaging in self-management practices by DSME duration category from logistic regression models adjusted for sex, race/ethnicity, age-group, education level, marital status, health insurance status, and insulin use status. Education level was used as a proxy for socioeconomic status, and annual income was not included in the logistic regression models because these two indicators are highly correlated (18). Compared to those who did not receive DSME, the adjusted odds of performing SMBG, having had an annual eye exam, and having had an annual foot exam did not vary significantly by DSME duration category. The adjusted odds of having had at least two A1C tests in the past year was 2.69 (95% CI 1.30–5.58) times higher among those who received 4–10 hours of DSME and 2.63 (95% CI 1.10–6.31) times higher among those who received >10 hours of DSME compared to those receiving 0 hours. The adjusted odds of having an annual flu shot was 2.20 (95% CI 1.18–4.09) times higher among those who received >10 hours of DSME compared to those who received no DSME. Finally, the adjusted odds of ever receiving a pneumococcal vaccination was almost twice as high among those who received 4–10 hours (OR 1.98, 95% CI 1.03–3.80) and >10 hours of DSME (OR 1.92, 95% CI 1.01–3.64) compared to those who did not receive DSME.
TABLE 3.
Results From Logistic Regression Models for Clinical Services or Self-Management Practices, Florida BRFSS 2008
| Covariate (Referent*) | Engaged in SMBG |
Annual Eye Exam |
Annual Foot Exam |
Two A1C Tests |
Annual Flu Shot |
One-Time Pneumococcal |
||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Female (male) | 1.51 | 0.94–2.43 | 1.19 | 0.67–2.12 | 0.88 | 0.55–1.40 | 0.75 | 0.44–1.29 | 1.28 | 0.82–2.00 | 1.50 | 0.94–2.41 |
| Race/ethnicity (non-Hispanic white) | ||||||||||||
| Non-Hispanic black | 1.08 | 0.49–2.38 | 1.12 | 0.40–3.14 | 2.87 | 1.26–6.52 | 2.06 | 0.88–4.80 | 0.49 | 0.26–0.95 | 0.61 | 0.28–1.34 |
| Hispanic | 0.92 | 0.44–1.90 | 1.25 | 0.54–2.90 | 0.44 | 0.22–0.87 | 0.38 | 0.18–0.80 | 0.38 | 0.19–0.75 | 0.32 | 0.13–0.76 |
| Age-group (18–44 years) | ||||||||||||
| 45–64 years | 0.62 | 0.24–1.60 | 2.98 | 1.34–6.63 | 6.12 | 2.52–14.87 | 1.38 | 0.54–3.49 | 1.88 | 0.81–4.34 | 0.82 | 0.31–2.22 |
| ≥65 years | 0.63 | 0.24–1.63 | 6.63 | 2.90–15.17 | 4.22 | 1.73–10.32 | 1.03 | 0.41–2.58 | 4.79 | 2.10–10.92 | 2.35 | 0.92–6.04 |
| Education level (less than high school) | ||||||||||||
| High school | 0.43 | 0.20–0.92 | 0.83 | 0.34–2.03 | 1.09 | 0.55–2.14 | 0.71 | 0.27–1.91 | 0.96 | 0.49–1.90 | 0.83 | 0.43–1.62 |
| More than high school | 0.42 | 0.19–0.91 | 0.77 | 0.30–1.99 | 1.13 | 0.58–2.21 | 0.55 | 0.21–1.46 | 1.20 | 0.62–2.32 | 1.28 | 0.63–2.62 |
| Not married or cohabitating (Yes) | 1.46 | 0.95–2.26 | 1.08 | 0.61–1.90 | 0.92 | 0.58–1.47 | 1.09 | 0.67–1.77 | 1.05 | 0.67–1.64 | 0.81 | 0.51–1.29 |
| Has health insurance (No) | 0.71 | 0.30–1.70 | 2.60 | 1.16–5.85 | 1.27 | 0.54–2.99 | 5.52 | 2.49–12.24 | 0.80 | 0.35–1.81 | 0.86 | 0.35–2.14 |
| Uses insulin (No) | 14.72 | 7.88–27.49 | 1.12 | 0.60–2.08 | 2.77 | 1.54–5.00 | 1.06 | 0.57–1.97 | 0.94 | 0.59–1.49 | 1.17 | 0.73–1.88 |
| DSME duration (No DSME) | ||||||||||||
| >0 to <4 hours | 0.84 | 0.47–1.52 | 1.69 | 0.86–3.31 | 1.74 | 0.95–3.21 | 1.87 | 0.96–3.64 | 1.74 | 0.99–3.03 | 1.16 | 0.63–2.12 |
| 4–10 hours | 1.61 | 0.82–3.16 | 1.56 | 0.70–3.44 | 1.57 | 0.81–3.04 | 2.69 | 1.30–5.58 | 1.76 | 0.99–3.24 | 1.98 | 1.03–3.80 |
| >10 hours | 1.45 | 0.76–2.75 | 1.72 | 0.74–4.02 | 1.45 | 0.70–2.99 | 2.63 | 1.10–6.31 | 2.20 | 1.18–4.09 | 1.92 | 1.01–3.64 |
All referent categories have an OR of 1.00.
Discussion
Existing literature documents the benefits of engaging in self-management practices and receiving clinical services for those with diabetes (10,19–22). Likewise, the literature documents positive associations between receiving DSME and clinical and self-care (10,20,22). What remains less understood is the association between DSME duration and receiving clinical care or engaging in self-care practices. A review of existing literature did not reveal any large, population-based studies examining the relationship between DSME duration and clinical- or self-care outcomes. This study helps to fill this gap in the literature.
The results of this study show that, among those with diagnosed diabetes who received DSME, a positive association exists between DSME duration and a number of clinical-care utilization patterns. In particular, having received at least 4 hours of DSME had the greatest impact on clinical-care utilization, specifically A1C testing and influenza and pneumococcal vaccinations. The results also indicate that those who use insulin have significantly higher odds of performing SMBG and having an annual foot examination.
A number of potential confounding variables are associated with the patient behaviors and outcomes of interest in this study but were not well recorded in the available data (23–30). These variables can be broadly grouped into provider behaviors, social support, and access to care issues. Provider behaviors include providing patients with the care outlined in clinical practice guidelines, providing necessary referrals to specialty care such as podiatrists and ophthalmologists, and effectively communicating with patients to ensure they understand examination outcomes and the importance of receiving the recommended care. Social support includes settings such as home, community, and worksites. The ability to quantify social support variables was very limited in the data used for this study. Finally, although the data presented controls for having health insurance, insurance is only part of the overall access-to-care construct. Variables such as the inability to access the health care system because of monetary, transportation, geographic isolation, and psychosocial issues were not included.
Finding the balance between DSME duration and best health outcomes is crucial for people with diabetes. It is imperative to determine the most effective dose of DSME necessary to decrease the prevalence of the debilitating consequences of poor diabetes outcomes while also containing costs and making the best use of limited resources. Although the results of this study help to inform this endeavor, more research is needed.
In addition to examining the effects of DSME duration, further qualifying the nature of DSME delivery is another area that needs more study (11,12). Important topics to consider in future studies include determining the most effective length for a single session of DSME, the most beneficial time lapse between individual sessions, and the optimal total number of sessions that a person with diabetes should receive. In addition, studies comparing health outcomes of individual- versus group-based DSME would help guide health educators to the most prudent, cost-effective approach. The combined results of studies such as these would provide a more complete, evidence-based picture of what constitutes a successful DSME program.
There are a number of limitations to consider when examining the results of this analysis. The BRFSS is a cross-sectional study, and one cannot infer causal relationships from the results. The 2008 Florida BRFSS was a telephone-based questionnaire administered to a sample of individuals living in households with landlines. Given the sampling methodology, those without landline telephones in the household and those who do not reside in households (e.g., homeless individuals and those who reside in institutional settings) were not eligible for participation, increasing the chances of exclusion bias. The BRFSS collects self-reported data, which may introduce recall and interviewer bias. In addition, the DSME duration question was a state-added question unique to the 2008 Florida BRFSS, and the means to verify the information provided by respondents did not exist. Therefore, the authors cannot evaluate the accuracy and precision of the question using the study data. Moreover, although the state-added DSME duration question provides a means to quantify the estimated number of hours of DSME a respondent received, it does not collect data for the following important considerations: educational setting, curriculum quality, course sequence, and spacing of DSME hours over time (i.e., days, weeks, or months). Finally, the outcome behaviors examined are potentially influenced by health care provider behaviors and referral practices. The effects of provider behavior on the outcomes studied cannot be assessed using these data. However, this line of inquiry is a logical next step in research on this topic.
Given the ever-increasing magnitude of diabetes incidence and prevalence, the potential for devastating health complications, and the skyrocketing costs associated with diabetes, the urgent need for effective DSME is clear. The results of this study can be used as an important segue for future studies that strive to hone and refine best practices in DSME delivery. It is already widely accepted that DSME is associated with improved clinical/self-care and diabetes-related health outcomes (4,7–9). Further elucidating the parameters of what constitutes the most effective form and dosage of DSME will help improve evidence-based strategies for preventing complications and maintaining a good quality of life among people with diabetes.
Acknowledgments
The authors thank the staff of the Florida Department of Health, Division of Disease Control, Bureau of Epidemiology, for collecting and sharing Florida-specific BRFSS data. They also thank Sara McDowell (graduate research assistant, University of North Florida Department of Public Health) for her editorial contribution. Preliminary findings from this study were presented at two meetings and published in abstracts: the Centers for Disease Control and Prevention Division of Diabetes Translation Diabetes Prevention and Control Program Directors Meeting in October 2010 and the American Public Health Association 140th Annual Meeting in October 2012.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Schiller JS, Ward BW, Freeman G. Early release of selected estimates based on data from the January–June 2013 National Health Interview Survey. National Center for Health Statistics. December 2013. Available from http://www.cdc.gov/hchs/nhis.htm. Accessed 13 February 2014
- 2.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033–1046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burke RE, O’Grady ET. Group visits hold great potential for improving diabetes care and outcomes, but best practices must be developed. Health Aff (Millwood) 2012;31:103–109 [DOI] [PubMed] [Google Scholar]
- 4.Caspersen CJ, Thomas GD, Boseman LA, Albright AL. Aging, diabetes, and the public health system in the United States. Am J Public Health 2012;102:1482–1497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Association of Diabetes Educators AADE guidelines for the practice of diabetes self-management education and training (DSME/T). Diabetes Educ 2009;35:85S–107S [Google Scholar]
- 6.Haas L, Maryniuk M, Beck J, et al. National standards for diabetes self-management education and support. Diabetes Care 2013;36:S100–S108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stetson B, Schlundt D, Rothschild C, Floyd JE, Rogers W, Mokshagundam SP. Development and validation of the Personal Diabetes Questionnaire (PDQ): a measure of diabetes self-care behaviors, perceptions and barriers. Diabetes Res Clin Pract 2011;91:321–332 [DOI] [PubMed] [Google Scholar]
- 8.Sürücü HA, Kizilci S. Use of Orem’s Self-Care Deficit Nursing Theory in the self-management education of patients with type 2: a case study. Self Care Depend Care Nurs 2012;19:53–59 [Google Scholar]
- 9.Thorpe KE. The Affordable Care Act lays the groundwork for a national diabetes prevention and treatment strategy. Health Affairs (Millwood) 2012;31:61–66 [DOI] [PubMed] [Google Scholar]
- 10.Johnson TM, Murray MR, Huang Y. Associations between self-management education and comprehensive diabetes clinical care. Diabetes Spectrum 2010;23:41–46 [Google Scholar]
- 11.Duncan I, Ahmed T, Li Q, et al. Assessing the value of the diabetes educator. Diabetes Educ 2011;37:638–657 [DOI] [PubMed] [Google Scholar]
- 12.Steinsbekk A, Rygg LØ, Lisulo M, Rise MB, Fretheim F. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus a systematic review with meta-analysis. BMC Health Serv Res 2012;12:213–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002;25:1159–1171 [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention About BRFSS: Behavioral Risk Factor Surveillance System. Available from http://www.cdc.gov/brfss/about/about_brfss.htm. Accessed 8 January 2014
- 15.Centers for Disease Control and Prevention The BRFSS Data User Guide. Available from http://www.cdc.gov/brfss/data_documentation/PDF/UserguideJune2013.pdf. Accessed 14 December 2013
- 16.Centers for Disease Control and Prevention 2008 Behavioral Risk Factor Surveillance System questionnaire. Available from http://www.cdc.gov/brfss/annual_data/pdf-ques/2008brfss.pdf. Accessed 23 January 2014
- 17.Florida Department of Health Florida 2008 BRFSS questionnaire. Available from http://www.floridahealth.gov/reports-and-data/survey-data/behavioral-risk-factor-surveillance-system/survey-instruments/_documents/2008_BRFSS_questionnaire.pdf. Accessed 23 January 2014
- 18.U.S. Bureau of Labor Statistics Earnings and unemployment rates by educational attainment. Available from http://www.bls.gov/emp/ep_chart_001.htm. Accessed 3 June 2013
- 19.Balamurugan A, Ohsfeldt R, Hughes T, Phillips M. Diabetes self-management education program for Medicaid recipients: a continuous quality improvement process. Diabetes Educ 2006;32:893–900 [DOI] [PubMed] [Google Scholar]
- 20.Gumbs JM. Relationship between diabetes self-management education and self-care behaviors among African American women with type 2 diabetes. J Cult Divers 2012;19:18–22 [PubMed] [Google Scholar]
- 21.Rygg L, Rise MB, Grønning K, Steinsbekk A. Efficacy of ongoing group based diabetes self-management education for patients with type 2 diabetes mellitus: a randomised controlled trial. Patient Educ Couns 2012;86:98–105 [DOI] [PubMed] [Google Scholar]
- 22.Strine TW, Okora CA, Chapman DP, Beckles GLA, Balluz L, Mokdad AH. The impact of formal diabetes education on the preventive health practices and behaviors of persons with type 2 diabetes. Prev Med 2005;41:79–84 [DOI] [PubMed] [Google Scholar]
- 23.Bundesmann R, Kaplowitz SA. Provider communication and patient participation in diabetes self-care. Patient Educ Couns 2011;85:143–147 [DOI] [PubMed] [Google Scholar]
- 24.Hudelson P, Dominié Dao M, Perron NJ, Bischoff A. Interpreter-mediated diabetes consultations: a qualitative analysis of physician communication practices. BMC Fam Pract 2013;14:163–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferrara A, Hedderson MM, Ching J, Kim C, Peng T, Crites YM. Referral to telephonic nurse management improves outcomes in women with gestational diabetes. Am J Obstet Gynecol 2012;206:491.e1–491.e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jianzhen Z, Burridge L, Baxter KA, et al. A new model of integrated primary-secondary care for complex diabetes in the community: study protocol for a randomised controlled trial. Trials 2013;14:1–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scott C. Care planning: supporting self-management in diabetes care. Practice Nurse 2013;43:28–30 [Google Scholar]
- 28.Stopford Rrskau, Winkley K, Ismail K. Social support and glycemic control in type 2 diabetes: a systematic review of observational studies. Patient Educ Couns 2013;93:549–558 [DOI] [PubMed] [Google Scholar]
- 29.Chou C-F, Sherrod CE, Zhang X, et al. Barriers to eye care among people aged 40 years and older with diagnosed diabetes, 2006–2010. Diabetes Care 2014;37:180–188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilkinson A, Whitehead L, Ritchie L. Factors influencing the ability to self-manage diabetes for adults living with type 1 or 2 diabetes. Int J Nurs Studies 2014;51:111–122 [DOI] [PubMed] [Google Scholar]