Insulin continues to be the most potent therapeutic option available to reduce hyperglycemia in people with diabetes (1). In 2011, approximately one-third of people diagnosed with diabetes reported taking insulin as part of their therapeutic regimen (2). In the same year, data from a large commercial insurer in the United States showed that ∼80% of individuals with type 2 diabetes who were taking insulin had an A1C ≥7% (3). Clinicians and patients agree that there are numerous obstacles for initiating intensified insulin therapy and adhering to a prescribed regimen. Included in these challenges are interference with daily living, complexity of regimens, injection discomfort, and public embarrassment (4,5).
Addressing such barriers likely would lead to improvement in glycemic control, which has been shown to reduce morbidity and mortality related to uncontrolled diabetes (6–8). This article presents the experiences of three individuals with type 2 diabetes who switched from disposable insulin pens to a new disposable insulin delivery device to address elevated A1C levels or simplify a complicated insulin regimen.
Background
For people with type 2 diabetes, national guidelines support the use of basal insulin first, with the later addition of prandial insulin if needed in patients with limited β-cell secretory capacity who are not achieving glycemic goals (9). However, the prospect of adding injections often is met with reluctance on the part of both patients and clinicians. In a recently published multinational survey (10), 49% of the 600 insulin prescribers surveyed reported lack of experience with insulin and time required to intensify insulin as primary factors hindering escalation of insulin therapy. Furthermore, 39% believed that patients are not able to cope with adding prandial insulin or an additional injection to their current therapy regimen. Research has shown that, as the insulin regimen is intensified to a full basal-bolus regimen, patients’ treatment satisfaction and adherence decrease (11,12).
Based on these challenges, advances in insulin delivery and new tools that simplify the process of intensifying insulin therapy for both clinicians and patients are worth evaluating. Disposable insulin pens provide many advantages over vials and syringes, including ease of use, convenience, and self-containment (13,14). However, with pen devices, patients still must administer multiple injections, remember the pen when they are eating away from home, and potentially face injection anxiety when administering insulin in public.
Disposable Insulin Delivery Devices
A disposable insulin delivery device is an alternative that may lessen the burden of insulin administration. V-Go (Valeritas, Inc., Bridgewater, N.J.), a disposable insulin delivery device, received U.S. Food and Drug Administration (FDA) approval for continuous subcutaneous delivery of insulin in adult patients in December 2010 and is now on the U.S. market. Patients who use V-Go apply a new device every 24 hours for coverage of daily basal and prandial insulin requirements. Three basal dosing options are available (V-Go 20, V-Go 30, and V-Go 40), each delivering insulin at a preset, fixed basal infusion rate over a 24-hour period. In addition, each dosing option offers up to 36 units of insulin (in 2-unit increments) for on-demand prandial insulin coverage (Table 1).
TABLE 1.
V-Go Dosing Options*
| V-Go 20 | V-Go 30 | V-Go 40 | |
| Preset basal dose (units/24 hours) | 20 | 30 | 40 |
| Basal rate (unit/hour) | 0.83 | 1.25 | 1.67 |
| On-demand bolus (units) | Up to 36, delivered in 2-unit increments | ||
| Total available insulin (units/24 hours) | 56 | 66 | 76 |
A U-100 fast-acting insulin should be used with V-Go. Lispro and aspart insulins have been tested by the V-Go manufacturer and found to be safe for use in the device.
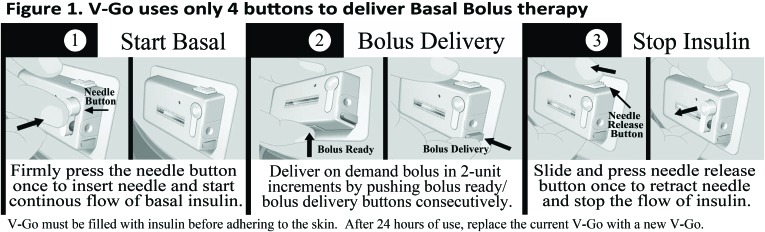
Before applying a V-Go device, patients fill it with U-100 fast-acting insulin via a filling device provided with each 30-day supply (15). V-Go is small, is lightweight, and can be worn under clothing. After filling the device, patients adhere it to their skin in any location insulin can be injected or infused (15). There are only four buttons on the outside of the V-Go device: one to simultaneously insert the 4.6-mm, 30-gauge stainless steel needle and start the basal rate, two for on-demand bolus dosing at mealtimes, and one to retract the needle and stop insulin delivery (Figure 1).
FIGURE 1.
V-Go disposable insulin delivery system.
Case Studies
The following retrospective case series describes three patients who were following an intensified insulin regimen and were switched to V-Go. The information provided was obtained from the patients’ medical charts. The patients received diabetes care from an academic-based diabetes center, and patients had previously received individualized diabetes education. These cases were selected to provide insight for use in people with a variety of demographic and clinical characteristics. Insulin total daily dose (TDD), complexity of the regimen, and patients’ age and duration of diabetes were all considered when searching for cases to describe. Insulin doses and blood glucose goals were based on clinicians’ individual assessment of each patient and may differ from national recommendations.
Case 1: Elevated A1C, Type 2 Diabetes for 1 Year, and a TDD of 33 Units
A 50-year-old working woman with a strong family history of diabetes struggled to control her diabetes as a result of the perceived difficulty and time required to administer multiple insulin injections. At the time of diagnosis, she was started on triple antidiabetic oral therapy. With minimal glycemic improvement after 3 months, her treatment was escalated to a basal-bolus insulin regimen and two of the three oral agents were discontinued. She was provided with pre- and postprandial glucose targets and encouraged to perform self-monitoring of blood glucose (SMBG) to adjust her insulin appropriately.
The patient’s SMBG results continued to show daily elevations, possibly secondary to omission of prandial insulin doses. She compensated for elevated glucose by administering high correction doses of insulin in the evenings, resulting in reported nocturnal hypoglycemia. Her therapeutic regimen before switching to V-Go consisted of metformin 1,000 mg twice daily, 15 units of insulin glargine in the morning, and 6 units of insulin lispro at each meal, for a TDD of 33 units of insulin. Before initiating V-Go, her A1C was 8.6%.
The patient’s clinician discontinued her previous insulin regimen and prescribed a regimen using the V-Go 20 filled with insulin lispro. In addition to the basal rate of 0.83 units/hour, the patient was given guidance to bolus 4–6 units per meal based on her preprandial glucose targets, resulting in an average TDD of 35 units of insulin. Her metformin dose was maintained.
At 3 months, the prescribed regimen remained unchanged, and her A1C had decreased from 8.6 to 7.2%. The patient noted that V-Go improved her adherence to the insulin regimen, particularly prandial dosing secondary to having insulin readily available for prandial coverage. Clinically, the patient benefited from significantly improved glycemic control and a reduction in reported nocturnal hypoglycemia.
Case 2: Elevated A1C, Type 2 Diabetes for 19 Years, and a TDD of 80 Units
A 73-year-old retired man with type 2 diabetes for 19 years presented with a baseline A1C of 8.0%. He was new to the practice and had previously been prescribed metformin 1,000 mg twice daily, sitagliptin 100 mg daily, 60 units of insulin determir daily, and 10 units of insulin lispro at both lunch and dinner.
The clinician provided guidance for administering insulin correction doses based on preprandial SMBG results. Because basal insulin comprised 75% of the patient’s TDD, the clinician redistributed the basal/bolus ratio and prescribed a V-Go 40 and lispro insulin to evaluate whether a different delivery approach would improve that patient’s glycemic control. The patient was instructed to bolus 10 units per meal plus a correction dose if his preprandial blood glucose exceeded 150 mg/dL. This distribution was more in line with the 50% basal/50% bolus ratio commonly recommended (16,17). The patient’s oral medications were maintained as previously prescribed.
After 6 months of V-Go use, the patient’s A1C decreased to 6.7%. The only change in therapy during this time was a 50% reduction in metformin. A 3-lb weight gain was recorded at the 6-month follow-up visit. Secondary to poor insurance coverage, the patient’s monthly cost for V-Go was $150. Given the improved glucose control and convenience, the patient was willing to pay that amount and continue on the therapy. Redistributing the basal-bolus insulin was simplified by using the V-Go device and resulted in the patient achieving his glycemic goals with a reduction in oral medication and TDD and one needle insertion per day.
Case 3: Good Glycemic Control, Type 2 Diabetes for 31 Years, and a Complex Insulin Regimen
A 68-year-old woman with type 2 diabetes for 31 years demonstrated good glycemic control on a combination of 30 units of insulin glargine dosed in the morning, 8 units of NPH at bedtime, and insulin lispro dosed at meals using an insulin-to-carbohydrate ratio of 1:10 plus a correction scale when her preprandial blood glucose exceeded 125 mg/dL. Oral antidiabetic medications were not included in her therapeutic regimen. The patient had an active lifestyle, spending time with grandchildren and serving as a caretaker for both her husband and mother. Her meals were erratic because of her unpredictable schedule, which complicated insulin administration. She had administered insulin for 27 years and was comfortable with injections. However, she said her current therapeutic regimen of five or more injections per day interfered with her lifestyle, and she desired a simplified approach. Her A1C at baseline was 7.1%.
The patient was switched from her previous regimen to a V-Go 30 filled with insulin lispro and given guidance to bolus 8 units with breakfast, 10 units with lunch, 12 units with dinner, and 6 units with a snack. An additional subcutaneous injection of insulin lispro was prescribed if her total bolus requirements exceeded 36 units.
When the patient returned to the clinic after 6 months, her A1C had improved to 6.9% with no reported increase in hypoglycemia. Her weight was unchanged. She felt more in control of her life and enjoyed the flexibility this delivery method provided. V-Go demonstrated durability with regard to her glycemic control, and the simplified approach allowed for a reported improvement in the patient’s quality of life.
Practical Considerations and Perceptions
The new V-Go insulin delivery device offers additional options for patients and clinicians to manage insulin therapy. Experience with this device is limited, and few publications are available to date. In our practice, we wanted to gain familiarity with the device and therefore prescribed V-Go for patients who were already on basal-bolus therapy but not achieving their glycemic goals or who desired a simplified approach to insulin administration.
All three of the patients described above had type 2 diabetes, and two had elevated A1C levels before V-Go initiation. A1C levels were reduced in all three patients because of improved adherence to prandial insulin dosing, redistribution of the basal-bolus insulin ratio, and reduction in the complexity of the insulin regimen, respectively. In addition, patients’ perceptions were positive; they found the V-Go easy to use and less disruptive than administration of multiple daily injections. One patient was even willing to pay more out of pocket for the increased convenience this new delivery device affords.
Our findings are similar to those previously reported in the literature for patients switched to V-Go. A small, prospective study evaluating patient and clinician feedback demonstrated that 84% of clinicians had positive impressions of managing patients using the device. More than 90% of patients ranked V-Go easy to use and found it discreet (18). Recently reported interim results from a prospective, multicenter, observational study, found that, after 9 months of V-Go therapy, the overall population experienced an A1C decrease of 0.7% with a reduction in TDD of 11% compared to previous therapy. The overall population included patients with type 2 diabetes previously treated with oral agents alone, long-acting insulin ± oral agents, multiple daily insulin injections ± oral agents, or premixed insulin ± oral agents. The cohort of patients that experienced the greatest A1C benefit (–1.2%) were those who had been taking long-acting insulin ± oral agents before switching to V-Go (19).
There are limitations with this new device. In our opinion, some patients do not prefer to have a device adhered to their skin for 24 hours, and those with sensitive skin may experience irritation from the adhesive. We have found the use of skin barriers beneficial for the small percentage of patients reporting such irritation. Second, the minimum basal rate with V-Go is 20 units per 24 hours, and the largest TDD available when using V-Go is 76 units (15). This dosing range may limit patient selection. Patients requiring a basal dose of <20 units per 24 hours should not be considered for V-Go. However, we have seen positive results with V-Go in patients who were previously prescribed insulin regimens involving >76 units/day and therefore no longer exclude patients based on higher baseline insulin doses. We attribute the success in these patients to better adherence and the efficient insulin delivery provided by this device.
Other disposable insulin delivery devices designed for people with type 2 diabetes are in development, but none are yet available in the United States. A disposable bolus-only option called Finesse (Calibra Medical Inc., Redwood City, Calif.) that can be worn for up to 3 days for prandial insulin coverage has been approved in the United States, but a timeline for its market availability has not been disclosed (20). A semi-disposable insulin device called PaQ (Cequr SA, Montreux, Switzerland) incorporates an electronic messenger with an infuser unit to alert patients when it is time to replace the device. PaQ, which has been approved in Europe, is designed to administer basal-bolus therapy and is intended to be worn for 3 days (21). The timeline for filing with the FDA to secure approval in the United States is not available.
Conclusion
The patients described in this case series were selected as examples to provide clinical insight into the use of the V-Go insulin delivery system in people with type 2 diabetes. Innovations that address insulin administration challenges increase the possibility of improving glycemic control with insulin therapy. This disposable device is simple to use, and its use has resulted in A1C reductions and other positive benefits perceived by both patients and clinicians.
Acknowledgments
The authors thank Catherine E. Cooke, PharmD, president of PosiHealth, Inc., for editorial assistance.
Funding
Editorial assistance for preparation of this article was provided by Valeritas, Inc.
Duality of Interest
Ms. Knutsen serves as a speaker for Valeritas, Inc., which manufactures the V-Go, and is on an advisory board for Sanofi, which manufactures insulin glargine. Ms. Nikkel is an employee of and holds stock options for Valeritas, Inc. No other potential conflicts of interest relevant to this article were reported.
References
- 1.Nathan DM, Buse JB, Davidson MB, et al. . Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2009;32:193–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Percentage using diabetes medications by type of medication, 2011 [article online]. Available from www.cdc.gov/diabetes/statistics/meduse/fig2.htm. Accessed 7 March 2014
- 3.Chen Y, Grabner M, Nguyen M, Abbott S, Quimbo R. Using observational data to inform the design of a prospective effectiveness study for a novel insulin delivery device [Poster]. American Association of Colleges of Pharmacy Annual Meeting, Hollywood, Fla., 21–24 October 2012 [Google Scholar]
- 4.Peyrot M, Barnett AH, Meneghini LF, Schumm-Draeger PM. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabet Med 2012;29:682–689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peyrot M, Rubin RR, Kruger DF, Travis LB. Correlates of insulin injection omission. Diabetes Care 2010;33:240–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cramer JA, Pugh MJ. The influence of insulin use on glycemic control: how well do adults follow prescriptions for insulin? Diabetes Care 2005;28:78–83 [DOI] [PubMed] [Google Scholar]
- 7.Ho PM, Rumsfeld JS, Masoudi FA, et al. . Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med 2006;166:1836–1841 [DOI] [PubMed] [Google Scholar]
- 8.Rhee MK, Cook CB, El-Kebbi I, et al. . Barriers to diabetes education in urban patients: perceptions, patterns, and associated factors. Diabetes Educ 2005;31:410–417 [DOI] [PubMed] [Google Scholar]
- 9.Inzucchi SE, Bergenstal RM, Buse JB, et al. . Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012;35:1364–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cuddihy RM, Philis-Tsimikas A, Nazeri A. Type 2 diabetes care and insulin intensification: is a more multidisciplinary approach needed? Results from the MODIFY survey. Diabetes Educ 2011;37:111–123 [DOI] [PubMed] [Google Scholar]
- 11.Rodbard H, Visco V, Anderson H, Hiort LC, Shu DH. Treatment intensification with stepwise addition of prandial insulin aspart boluses compared with full basal-bolus therapy (FullSTEP Study): a randomised, treat-to-target clinical trial. Lancet 2014;2:30–37 [DOI] [PubMed] [Google Scholar]
- 12.Meneghini L. Intensifying insulin therapy: what options are available to patients with type 2 diabetes? Am J Med 2013;126 (9 Suppl. 1):S28–S37 [DOI] [PubMed] [Google Scholar]
- 13.Asamoah E. Insulin pen: the “iPod” for insulin delivery (why pen wins over syringe). J Diabetes Sci Techol 2008;2:292–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Selam JL. Evolution of diabetes insulin delivery devices. J Diabetes Sci Technol 2010;4:505–513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Valeritas Inc V-Go disposable insulin delivery device: instructions for patient use. Valeritas, Inc; Bridgewater, N.J, 2011 [Google Scholar]
- 16.Abrahamson M, Peters A. Intensification of insulin therapy in patients with type 2 diabetes mellitus: an algorithm or basal-bolus therapy. Ann Med 2012;44:836–846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hamaty M. Insulin treatment for type 2 diabetes: when to start, which to use. Cleve Clin J Med 2011;78:332–342 [DOI] [PubMed] [Google Scholar]
- 18.Rosenfeld CR, Bohannon NJ, Bode B, et al. . The V-Go insulin delivery device used in clinical practice: patient perception and retrospective analysis of glycemic control. Endocr Pract 2012;18:660–667 [DOI] [PubMed] [Google Scholar]
- 19.Grunberger G, Bode B, Rosenfeld C, Strange P, Hershon K. Effectiveness of switching to V-Go in patients with type 2 diabetes: long-term follow-up from the SIMPLE study [Abstract]. Diabetes 2014;63(Suppl. 1). Available from http://app.core-apps.com/tristar_ada14/abstract/a15eac091139f735f9383a1ce14148b5. Accessed 13 June 2014 [Google Scholar]
- 20.Ramchandani N, Heptulla R. New technologies for diabetes: a review of the present and future. Int J Pediatr Endocrinol 2012;28:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mader JK, Lilly LC, Aberer F, et al. . A feasibility study of a 3-day basal-bolus insulin delivery device in individuals with type 2 diabetes. Diabetes Care 2014;37:1476–1479 [DOI] [PubMed] [Google Scholar]