Abstract
Background
Shoulder instability is an important clinical problem. Arthroscopic surgery is an established treatment modality in shoulder instability, but it continues to be associated with a high rate of recurrences and complications. The purpose of the study was to analyze late outcomes of arthroscopic repair of Bankart lesions in patients with post-traumatic anterior shoulder instability and non-engaging Hill-Sachs lesion, with special focus on the incidence and causes of recurrences and complications.
Material/Methods
We investigated 92 patients (92 shoulders) who underwent surgery on account of post-traumatic anterior shoulder instability. The duration of follow-up ranged from 6 to 12.5 years (mean: 8.2 years). All patients were operated on in the lateral decubitus position using FASTak 2.8-mm suture anchors (FASTak, Arthrex, Naples, Florida). Treatment outcomes were evaluated using the Rowe and University of California at Los Angeles rating system (UCLA).
Results
According to Rowe scores, there were 71 (81.5%) excellent, 12 (12.6%) good, 5 (5.3%) satisfactory, and 2 (2.1%) poor results. Rowe scores improved in a statistically significant manner (p=0.00) post-surgery, to a mean of 90 (range: 25–100). Treatment outcomes measured as UCLA scores improved in a statistically significant manner (p=0.00), reaching post-operative levels of 12–35 (mean: 33.5). There were 9 recurrences, 1 case of axillary nerve praxia, and 1 case of anchor loosening.
Conclusions
With rigorous criteria for qualifying patients for surgery, arthroscopic treatment of post-traumatic anterior shoulder instability produces good outcomes and low recurrence and complication rates irrespective of the number of previous dislocations, age, or sex.
MeSH Keywords: Arthroscopy, Joint Instability, Shoulder Dislocation, Shoulder Joint
Background
Owing to its complex anatomy, the shoulder is the most mobile joint in the human body. It also has to be able to bear heavy loads, especially in athletes and those carrying out heavy manual work. Load resistance is ensured by dynamic and static stabilizers of the shoulder joint [1–3]. A wide range of mobility is, however, hardly compatible with load resistance and the shoulder joint is the most frequently dislocated of all human joints [4,5]. The incidence of shoulder dislocation has been estimated at 11.2/100 000/year, affecting 2% of the general population. Of all shoulder dislocations, 85% are post-traumatic anterior dislocations [1,4–6]. A characteristic of the shoulder joint is a tendency towards repeated dislocations following an initial event. Patients with a history of shoulder dislocation at 20 years of age or earlier have a 66–100% risk of repeat dislocation, with the figure falling to 13–63% for the age range of 21–39 years and 0–16% in those over 40 years of age [7,8]. The most characteristic intraarticular lesions seen on arthroscopy include the Bankart lesion and a compression fracture of the humeral head [9,10]. Open surgery was the gold standard in the operative treatment of shoulder instability for many years [11,12]. Owing to the dynamic development of surgical techniques, arthroscopic methods have been enjoying increasing popularity [13]. The advantages of arthroscopic techniques include low invasiveness, minor tissue damage, good exposure of the joint, minor post-operative pain, and shorter times to resumption of daily activities [14,15]. However, even though arthroscopic procedures have been in use for a number of years and carry many advantages, the rate of recurrences and complications continues to be high [16–24].
Purpose
To analyze late outcomes of arthroscopic repair of Bankart lesions in patients with post-traumatic anterior shoulder instability and non-engaging Hill-Sachs lesion with special regard to the incidence and causes of recurrences and complications.
Material and Methods
This study presents the findings of a retrospective analysis of 92 patients (92 shoulders) with anterior post-traumatic shoulder instability who were operated on at Department VI of the Regional Trauma Hospital in Piekary Slaskie between January 2002 and January 2007. Patients’ age at surgery was 19–40 years, mean 25.6 years. The study group comprised of 18 (19.6%) women and 74 (80.4%) men. The duration of follow-up was 6–12.5 years, mean 8.2 years. Age on the day of injury was 15–37 years, mean 22.5 years.
The time between the initial dislocation and surgery was 0.5–4.8 years, mean 2.5 years. A total of 84 (91.3%) patients were right-handed and 8 (8.7%) were left-handed. The right shoulder was operated on in 81 (88%) cases, the left shoulder in 11 (12%). The basic characteristics of the study group are presented in Table 1.
Table 1.
Basic descriptive characteristics of the study group.
| Number of patients | 92 |
| Number of shoulders | 92 |
| Duration of follow-up | 5–12.5 years, mean 8.2 |
| Males | 74 (80.4%) |
| Females | 18 (19.6%) |
| Right-handed | 84 (91.3%) |
| Left-handed | 8 (8.7%) |
| Ambidextrous | 0 |
| Age at initial dislocation | 15–37 years, mean 22.5 |
| Time from initial dislocation to surgery | 05–4.8 years, mean 2.5 |
| Right shoulder | 81 (88%) |
| Left shoulder | 11 (12%) |
During the examination, a diagnosis of post-traumatic anterior instability of the shoulder joint was made in patients with a documented (medical records, imaging studies) history of at least two shoulder joint dislocations. Recurrences were classified as complications if they had occurred spontaneously after surgery. If a recurrence had been due to another high-energy trauma (e.g., during contact sport practice), it was regarded as a sequela of a new injury rather than a complication.
Preoperative patient assessment
Patients were examined on admission to the department by members of our shoulder team. History taking involved detailed questions about the number of dislocations, date and circumstances of the initial dislocation, circumstances of subsequent dislocations, a sense of apprehension, past treatment and the degree of daily activity: practising sport and the type of occupation. A physical examination included the apprehension test, anterior drawer test, posterior apprehension test, posterior drawer test and sulcus test in all patients [21,22]. All patients enrolled in the study underwent a CT scan in order to assess damage to bone tissue: bony Bankart lesions, Hill-Sachs lesions and an MRI scan to assess damage of soft tissues: rotator cuff tears, Superior Labral Antero-Posterior lesion (SLAP lesion), Humeral Avulsion Glenohumeral Ligament (HAGL), rotator interval lesions.
Surgical technique
All patients were operated on by the same surgeon under general anaesthesia in a lateral decubitus position. The operated limb was placed in 20° flexion and 45° abduction. Traction was achieved with a 5 kg or 2 kg weight. The weight was chosen so as to afford the best possible visualization of the joint. The joint was inspected initially from a posterior portal. The type of Bankart lesion was assessed, and any additional lesions, such as rotator cuff tears, Superior Labral Antero-Posterior lesion (SLAP lesion), Humeral Avulsion of the Glenohumeral Ligament (HAGL), rotator interval lesions, bony Bankart lesions or engaging Hill-Sachs lesions, were identified. The Hill-Sachs lesion was assessed according to the criteria presented by Burkchard and De Beer (engaging/non-engaging) [19]. The working cannula was always positioned in the anterior inferior portal using the inside-in technique [20]. After insertion of a cannula, the glenoid labrum and glenohumeral ligaments were separated from the glenoid and the antero-inferior bony part of the glenoid was scarified with a rasp. The labroligamentous complex was always reconstructed with FASTak 2.8 mm suture anchors (FASTak, Arthrex, Naples, Florida). Two or three implants were used, depending on the extent of injury. In each patient, the most distant implant (at 5:30 in the right shoulder, at 6:30 in the left shoulder) was mounted first, followed by mounting an implant at 3:30 for the right shoulder and 8:30 for the left and, in patients who received 3 implants, at 2:30 and 9: 30 respectively. The anchors were positioned along the bony ridge of the glenoid using a guide. The Dunkan loop knot was used in each case [25].
Inclusion criteria
A diagnosis of anterior post-traumatic shoulder instability based on: a history of 2 or more documented dislocations, a positive apprehension test and anterior drawer test on physical examination, no previous surgery, no bony lesions of the acetabulum as confirmed by a CT scan, presence of a Bankart lesion confirmed by an MRI scan and a non-engaging Hill-Sachs lesion with a definitive diagnosis ascertained intraoperatively [19].
Exclusion criteria
Posterior instability, multidirectional instability, voluntary instability diagnosed on history taking and confirmed by physical testing, glenoid fracture documented by a CT scan, previous surgery for shoulder instability, joint laxity, anatomic variants, neurological symptoms, additional problems: rotator cuff tears, Superior Labral Antero-Posterior lesion (SLAP lesion), Humeral Avulsion Glenohumeral Ligament (HAGL), rotator interval lesions, bony Bankart lesions, engaging Hill-Sachs lesions – diagnosed on the basis of history and physical examination, with a definitive diagnosis ascertained intraoperatively.
Post-operative management
After surgery, the joint was immobilized in adduction and internal rotation for 4 weeks. During this period of immobilization, the patients were instructed to exercise their hand joints and the elbow joint 3–4 times daily for 10 minutes, making extension, flexion and rotatory movements. Gradual rehabilitation began in week 5, with unloaded exercises, improving muscle strength via isometric exercises, and active exercises (elevation and abduction without loading). It was emphasized at that time that patients should avoid exercises in external rotation. External rotation exercises were introduced cautiously after 7 weeks. Safe sports exercises were commenced between weeks 10 and 12. Normal activity was resumed after 2–5 months, mean: 3.5 months, after the surgery.
Postoperative evaluation and outcome measurement
During a post-operative follow-up examination, performed after operation from 6 to 12.5 years, mean 8.2., by members of our shoulder team, patients were asked if they had resumed activities such as sport or employment and if they experienced any pain. Any recurrences of dislocations and/or subluxations were recorded together with the degree of limitation of daily activity. A physical examination involved the apprehension test, the anterior drawer test and range of motion assessment. A precise analysis of treatment outcomes was afforded by comparing pre- and post-operative questionnaires according to the Rowe scale and the University of California at Los Angeles rating system (UCLA) [11,26,27]. The duration of surgery, length of hospital stay and the rate and types of recurrences and complications were also noted.
The statistical analysis to confirm or reject the presence of correlations between the patients’ medical conditions, their causes and surgical treatment outcomes expressed according to the UCLA and Rowe scales employed a number of statistical tests and methods. Correlations between qualitative variables were assessed using the chi-squared test. Pearson’s linear correlation coefficients (r) were calculated for interval variables (age, treatment outcomes, etc.). Multiple regression was also used to evaluate the effect of the test variables on the values of the dependent variables. p<0.05 was assumed as the threshold statistical significance. Means and standard deviations per sample were used as measures of centrality of variables. The t test was also used to evaluate significance of differences if a sample was large enough (n>50). Some results measured according to scales employing different values were unified before they were compared.
Results
All patients had sustained their initial dislocation as a result of an injury. In 56 (60.8%) cases, these were sports injuries, and in 36 (39.2%), the causes were various types of high-energy injuries. The detailed data on the types of injury are presented in Table 2.
Table 2.
Causes of initial dislocation in the study group.
| Number of shoulders | 92 |
| Sport | 56 (60.9%) |
| Contact sports | 40 (71.4%) |
| Non-contact sports | 16 (28.6%) |
| Work accidents | 29 (31.5%) |
| Transportation accidents | 7 (7.6%) |
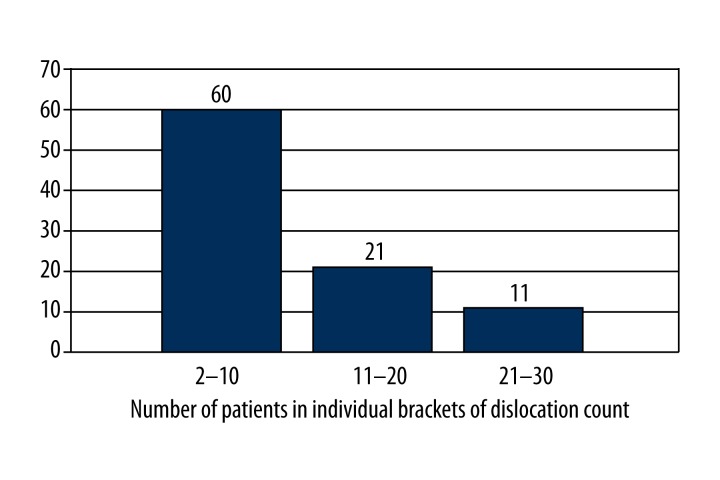
The number of dislocations per patient ranged from 2 to 30 (Figure 1).
Figure 1.
Graphic presentation of dislocation counts.
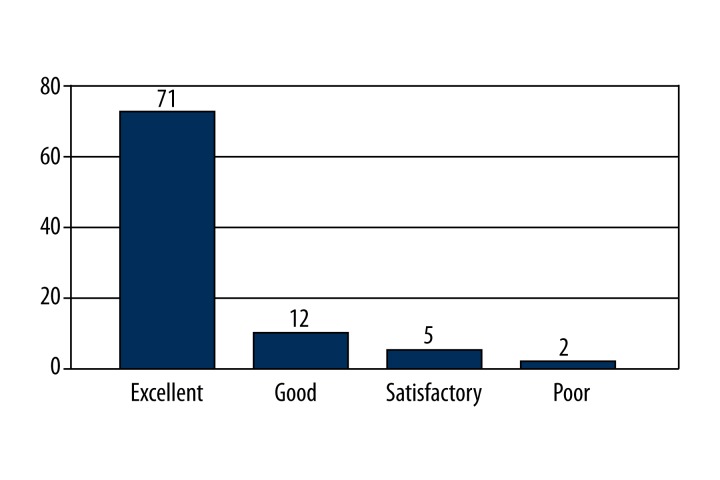
In 49 (53.3%) cases, a labral injury extending from 2 to 6 o’clock was diagnosed intraoperatively. All those patients received three implants. In 43 (46.7%) cases, the zone of injury extended from 3 to 6 o’clock and two implants were used. Based on the 4-level Rowe scale, there were 71 (81.5%) excellent results, 12 (12.6%) good results, 5 (5.3%) satisfactory results and 2 (2.1%) poor results in the study group (Figure 2).
Figure 2.
Treatment outcomes according to the 4-level Rowe scale.
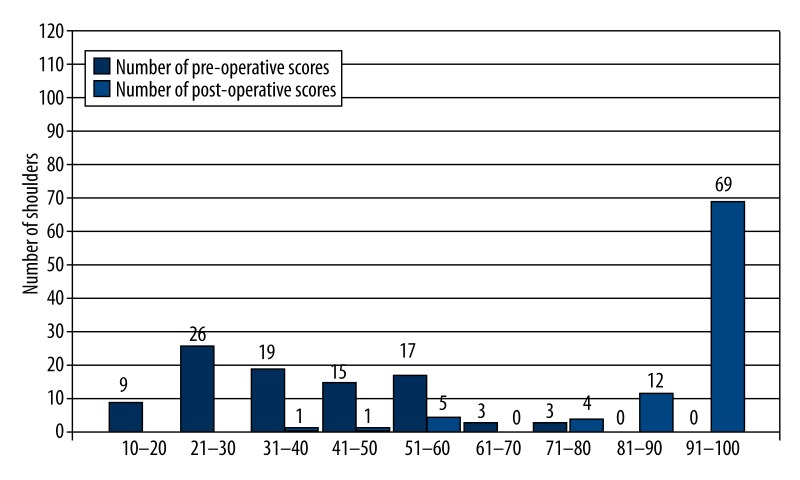
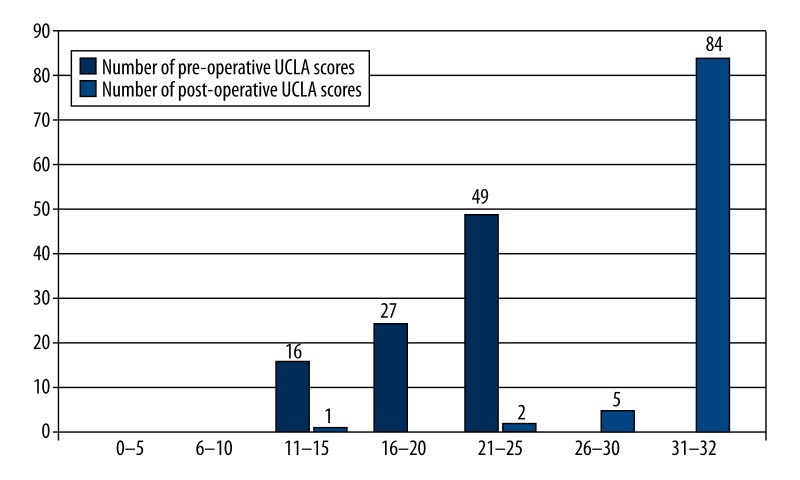
The mean pre-operative Rowe score was 41 (range: 15–80), compared to a mean post-operative score of 90 (range: 25–100). That was a statistically significant improvement (p=0.00) in treatment outcomes according to the Rowe scale post-operatively. Pre-operative UCLA scores were 11–24, mean 19.9, compared to post-operative scores of 12–35, mean 33.5, representing a statistically significant improvement in UCLA scores post-surgery at p=0.00. The pre and post-operative Rowe and UCLA scores are presented in Table 3. For better visibility of the differences, Rowe scores are grouped in 10-point intervals (Figure 3) and UCLA scores are grouped in 5-point intervals (Figure 4).
Table 3.
Pre and postoperative Rowe and UCLA scores.
| Rowe score | UCLA score | |||
|---|---|---|---|---|
| Before surgery | After surgery | Before surgery | After surgery | |
| Min | 15 | 25 | 11 | 12 |
| Max | 80 | 100 | 24 | 35 |
| Mean | 41 | 90 | 19.9 | 33.5 |
Figure 3.
Comparison of pre- and post-operative Rowe scores grouped into 10-point brackets.
Figure 4.
Comparison of pre- and post-operative UCLA scores grouped into 5-point brackets.
An analysis of correlations between the two scores pre and post-surgery revealed a significant (p=0.001) correlation between pre-operative Rowe scores and post-operative UCLA and a significant correlation (p=0.0001) between post-operative Rowe scores and post-operative UCLA (Table 4). No statistically significant correlation was found between age, sex, handedness, age at first dislocation and interval between the first dislocation and surgery and treatment outcomes according to either scale. The outcomes of patients with a labral injury between 2 and 6 o’clock, who received 3 implants, were also compared with those of patients with a labral injury between 3 and 6 o’clock, who received 2 implants. No statistically significant correlations were ascertained in the two groups between the Rowe and UCLA scores as outcome markers vs. extent of injury or number of implants. Post-surgery, 4 (4.3%) patients had a positive apprehension test, and 2 (2.1%) had a positive anterior Drawer test. The observed limitation of external rotation compared to the healthy limb was 0–25°, mean 6°. The duration of hospital stay was from 2 to 5 days, mean 3 days. The duration of the operation was 20–110 minutes, mean 35 minutes. 87 (94.6%) of the patients fully resumed their activities from the period before the initial dislocation, with 5 (5.4%) reporting functional limitation of various severity. In 4 (4.3%) patients, the limitation was due to fear of new dislocation and in 1 (1.1%) it was due to a limited range of motion. There were 9 (9.7%) cases of recurrence in the study group in 6 male and 3 female patients. The mean interval between surgery and re-dislocation was 2 years (range: 0.5–2.5 years). All cases were due to the patient suffering another high-energy injury. In 7 cases, re-dislocation occurred during intensive contact sport practice, including 3 re-dislocations during football practice, 1 during basketball practice, 2 during handball practice, and 1 during judo practice. One re-dislocation occurred while the patient was practising a non-contact sport (snowboarding) and one was the result of an accident at work (fall from a height). Of the patients with a recurrence, 6 required surgery, which was performed as an arthroscopic procedure in 4 patients and as an open procedure (Latarjet procedure) in 2. Three patients with re-dislocation were treated conservatively with 4 weeks of immobilization followed by rehabilitation. In the group of patients with recurrences, there have been no new dislocations to date. The surgical technique was chosen in accordance with the CT evidence. Patients with acetabular defects greater than 25% were qualified for a Latarjet procedure. Patients without bony lesions were treated arthroscopically. Analysis of the causes of recurrences showed a statistically significant correlation between recurrences and the practising of contact sports (p=0.0001).
Table 4.
Statistically significant correlations between pre and post-operative Rowe and UCLA scores.
| n | r | p | |
|---|---|---|---|
| Pre-operative Rowe and post-operative UCLA scores | 92 | 0.33 | P=0.001 |
| Post-operative Rowe and UCLA scores | 92 | 0.39 | P=0.0001 |
n – group size; r – correlation coefficient; p – level of significance.
Apart from the re-dislocations, one cause of a neurological complication (axillary nerve praxia) was noted (1.1%). There was also one case (1.1%) of anchor loosening. No inflammatory or vascular complications were noted.
Discussion
A number of surgical methods are used in the operative treatment of post-traumatic anterior shoulder instability. The main criterion underlying the choice of a particular technique is the predicted risk of subsequent dislocation following surgery. The literature indicates that the risk of recurrence depends on age, sex, number of previous dislocations, everyday activity, the extent of fracture of the glenoid and the presence of a Hill-Sachs lesion [18,28]. Until quite recently, open procedures were regarded as a gold standard in the treatment of shoulder instability, with proponents of open surgery arguing primarily that arthroscopic techniques were associated with a higher rate of recurrences [11,12,16,28,29]. The arthroscopic approach is now gaining in popularity and more and more authors are reporting good treatment outcomes that are not different from those obtained following open surgery [29–31]. At the same time, the recurrence and complication rates continue to be high [16–18]. Our study enrolled a selected group of patients as homogeneous as possible with regard to intraarticular lesions. This made possible the exclusion of patients presenting lesions that could influence treatment outcomes. To this end, we only enrolled patients with the Bankart lesion and the non-engaging Hill Sachs lesion. All patients in our study presented the Bankart lesion and 98% also presented the Hill Sachs lesion. Similar results were obtained by Yiannakopoulos in an investigation of the incidence of intraarticular lesions in patients with post-traumatic anterior shoulder instability in a group of 104 patients, where the Bankart lesion was found in 97% of the study group and the Hill Sachs lesion in 93%. Other authors have reported similar findings [10,32]. The inclusion criteria described above did not involve any limitations with regard to epidemiological data or the level of daily activity. This made possible an evaluation of treatment outcomes in a group of patients with specific patterns of injury while also accounting for the effect on these outcomes of such variables as age, sex, number of previous dislocations or time from the first dislocation to surgery. Existing publications describe late outcomes of post-traumatic anterior shoulder instability, but there still is a scarcity of studies involving large homogeneous samples. The present paper describes treatment outcomes in a group of 92 patients (92 shoulders) followed up for a mean of 8.2 years. An evaluation in terms of Rowe scores yielded 71 (81.5%) excellent, 12 (12.6%) good, 5 (5.3%) satisfactory and 2 (2.1%) poor outcomes. The post-operative Rowe scores (mean: 90, range: 25–100) represented a statistically significant improvement. Our results were compatible with late outcomes presented by other authors: Franceschi (8 years’ follow up) reports Rowe scores of 88, Kim (6.4 years’ follow up) had Rowe scores of 90 and Castagna (10.9 years’ follow up) reported a Rowe score of 80 [16,33,34]. Outcomes according to the UCLA scores were also significantly better post-surgery with a range of 12 to 35 and a mean score of 33.5. These were also not different from those reported by other authors: Ee 32.4 (2 years’ follow up) or Castagna 32 (10.9 years of follow up) [14,35]. Most patients in our study were active people who worked or practised sport. Accordingly, an important aspect of the study was the evaluation of the percentage of patients who were able to resume the level of activity that they had enjoyed prior to the initial dislocation. This rate reached 94.6% in our study, with Garofalo reporting a similar percentage [32]. The patients in our study experienced 9 (9.7%) recurrences, all of which were due to another high-energy trauma (Table 5). Kim et al. reported a recurrence rate of 6%, including two recurrences related to an injury; Castagna recorded a recurrence rate of 23%, where 16% were not related to an injury and 7% were post-traumatic; and Franceschi reported a recurrence rate of 17% [16,33,34]. Of the patients with a recurrence in our study, 6 required repeat surgery, with 4 arthroscopic procedures and 2 open procedures (Latarjet procedure). Three patients did not need repeat surgery. Of the patients who suffered re-dislocations, one experienced re-dislocations following conservative treatment, but he did not agree to have another surgery and his treatment outcome remains poor. The remaining patients, 6–11 (mean 9) years since surgery, have remained free of signs of instability and have resumed their previous activity levels. All recurrences have occurred in those aged 20 to 30 years old. Similar rates have been given by other authors (Porcelinii and Garofalo) [28,32].
Table 5.
Characteristics of patients who experienced a recurrence.
| Number of recurrences | 9 |
| Age | 20–29, mean 24.5 years |
| Males | 6 |
| Females | 3 |
| Limb | |
| R | 8 |
| L | 1 |
| Surgery-to-recurrence time | 0.5–2.5, mean 2 years |
| Sport | 8 |
| Contact sports | 7 |
| Non-contact sports | 1 |
| Accident at work | 1 |
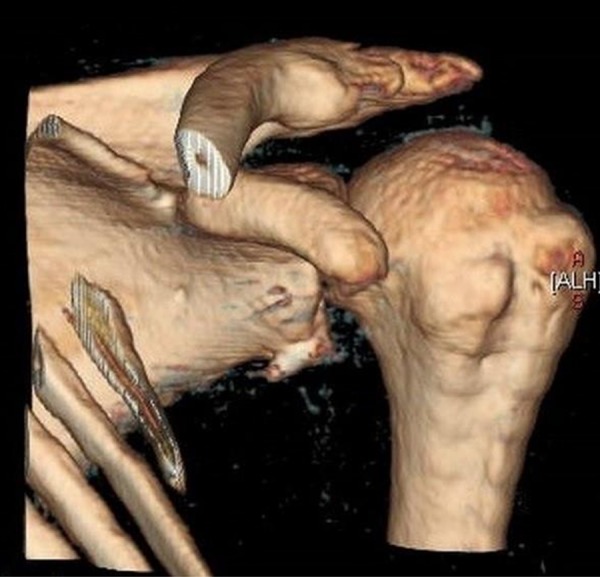
An analysis of treatment outcomes accounting for the effect of epidemiological factors and daily activity on treatment outcomes failed to reveal a statistically significant correlation between age at first dislocation, sex, number of dislocations, time between first dislocation and surgery or the number of implants. Similar data have been obtained by: Boileau et al. and Ee et al. [35,36]. The finding of no correlation between age/sex and treatment outcomes is not consistent with other reports [28]. There was one case of axillary nerve praxia in our sample that was due to malpositioning of an implant (Figure 5). The female patient was re-operated and the implant was removed and a new one was placed at a different location. After the second operation, the symptoms resolved over 4 months. One patient developed anchor loosening. The implant protruded above glenoid surface and over 2 years (during which the patient did not report to the hospital) destroyed the articular surface of the humeral head, which eventually led to extensive damage to the articular surface and deformity of the humeral head (Figure 6). The underlying cause, as in the patients described above, was malpositioning of the implant and also the fact that the patient worked as a security guard. The patient is not being prepared for shoulder joint capoplasty and his treatment outcome, just like the outcome of the patient discussed above who did not agree to undergo another surgery, remains poor.
Figure 5.
Extraosseous implant positioning – 3D reconstruction.
Figure 6.

Loose malpositioned implant causing destruction – 3D reconstruction.
Recapitulating this discussion, it should also be mentioned that many authors will still choose open surgical techniques for shoulder joint instability, basing their decisions mainly on data suggesting a lower incidence of post-operative recurrences. However, the results obtained and presented in this paper contradict the validity of this approach to the treatment of shoulder joint instability. It is our opinion, and it has been corroborated by data from other authors, that arthroscopic treatment using suture anchors is just as effective and is not associated with a higher incidence of recurrences, while its advantages include its low invasiveness and quick resumption of pre-surgery activity levels [14,15,37]. We realize the limitations of our study. First, the study was retrospective and it was not randomized and there was no control group. Our future study will be better documented and standardized for all group of patients.
Conclusions
With rigorous criteria for qualifying patients for surgery, as described in this article, arthroscopic treatment of post-traumatic anterior shoulder instability produces good outcomes and low recurrences and complication rates irrespective of the number of previous dislocations, age, or sex.
Footnotes
Conflicts of interest
We declare that we have no conflicts of interest in the authorship or publication of this work.
Source of support: Departmental sources
References
- 1.Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in United States. J Bone Joint Surg (Am) 2010;92:542–49. doi: 10.2106/JBJS.I.00450. [DOI] [PubMed] [Google Scholar]
- 2.Chant CB, Litchfield R, Griffin S, Thain LM. Humeral head retroversion in competitive baseball players and its relationship to glenohumeral rotation range of motion. J Orthop Sports Phys Ther. 2007;37(9):514–20. doi: 10.2519/jospt.2007.2449. [DOI] [PubMed] [Google Scholar]
- 3.Bergin D. Imaging shoulder instability in the athlete. Magn Reson Imaging Clin N Am. 2009;17(4):595–615. doi: 10.1016/j.mric.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Kroner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg. 1989;108:288–90. doi: 10.1007/BF00932317. [DOI] [PubMed] [Google Scholar]
- 5.Hovelius L. The natural history of primary anterior dislocation of the shoulder in the young. J Orthop Sci. 1999;4:307–17. doi: 10.1007/s007760050109. [DOI] [PubMed] [Google Scholar]
- 6.Simonet WT, Melton LJ, III, Cofield RH, Ilstrup DM. Incidence of anterior shoulder dislocation in Olmsted County, Minnesota. Clin Orthop Relat Res. 1984;(186):186–91. [PubMed] [Google Scholar]
- 7.Rowe CR, Zarins B, Ciullo JV. Recurrent anterior dislocation of the shoulder after surgical repair. Apparent causes of failure and treatment. J Bone Joint Surg (Am) 1984;66:159–68. [PubMed] [Google Scholar]
- 8.Simonet WT, Cofield RH. Prognosis in anterior shoulder dislocation. Am J Sports Med. 1984;12:19–24. doi: 10.1177/036354658401200103. [DOI] [PubMed] [Google Scholar]
- 9.Van der Linde JA, Van Kampen DA, Terwee CB, et al. Long-term results after arthroscopic shoulder stabilization using suture anchors: An 8- to 10-year follow-up. Am J Sports Med. 2011;39(11):2396–403. doi: 10.1177/0363546511415657. [DOI] [PubMed] [Google Scholar]
- 10.Yiannakopoulos CK, Mataragas E, Antonogiannakis E. A comparison of the spectrum of intra-articular lesions in acute and chronic anterior shoulder instability. Arthroscopy. 2007;23(9):985–90. doi: 10.1016/j.arthro.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 11.Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a longterm end result study. J Bone Joint Surg (Am) 1978;60:1–16. [PubMed] [Google Scholar]
- 12.Freedman KB, Smith AP, Romeo AA, et al. Open Bankart repair versus arthroscopic repair with transglenoid sutures or bioabsorbable tacks for recurrent anterior instability of the shoulder: a meta-analysis. Am J Sports Med. 2004;32(6):1520–27. doi: 10.1177/0363546504265188. [DOI] [PubMed] [Google Scholar]
- 13.Zhang AL, Montgomery SR, Nago SS, et al. Arthroscopic versus open shoulder stabilization: current practice patterns in the United States. Arthroscopy. 2014;30(4):436–43. doi: 10.1016/j.arthro.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Green MR, Christensen KP. Arthroscopic versus open Bankart procedures: a comparison of early morbidity and complications. Arthroscopy. 1993;(9):371–74. doi: 10.1016/s0749-8063(05)80308-1. [DOI] [PubMed] [Google Scholar]
- 15.Mazzocca AD, Brown FM, Jr, Carreira DS, et al. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med. 2005;33(1):52–60. doi: 10.1177/0363546504268037. [DOI] [PubMed] [Google Scholar]
- 16.Castagna A, Markopoulos N, Conti M, et al. Arthroscopic Bankart suture-anchor repair: radiological and clinical outcome at minimum 10 years of follow-up. Am J Sports Med. 2010;38:2012–16. doi: 10.1177/0363546510372614. [DOI] [PubMed] [Google Scholar]
- 17.Carreira DS, Mazzocca AD, Oryhon J, et al. A prospective outcome evaluation of arthroscopic Bankart repairs: minimum 2-year follow-up. Am J Sports Med. 2006;34(5):771–77. doi: 10.1177/0363546505283259. [DOI] [PubMed] [Google Scholar]
- 18.Boileau P, Villalba M, Hery JY, et al. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg (Am) 2006;88(8):1755–63. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 19.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–94. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 20.Lo IK, Lind CC, Burkhart SS. Glenohumeral arthroscopy portals established using an outside-in technique: neurovascular anatomy at risk. Arthroscopy. 2004;20(6):596–602. doi: 10.1016/j.arthro.2004.04.057. [DOI] [PubMed] [Google Scholar]
- 21.Jobe F, Kvitne RS. Shoulder pain in the overhand or throwing athlete: the relationship of anterior instability and the rotator cuff impingement. Orthop Rev. 1989;18:963–75. [PubMed] [Google Scholar]
- 22.Magee D. Shoulder. In: Magee D, editor. Orthopedic physical assessment. Philadelphia: WB Saunders; 1992. pp. 90–142. [Google Scholar]
- 23.Dumont GD, Golijanin P, Provencher MT. Shoulder instability in the military. Clin Sport Med. 2014;33(4):707–20. doi: 10.1016/j.csm.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 24.Matsuki K, Sugaya H. Complications after arthroscopiclabral repair for shoulder instability. Curr Rev Musculoskelet Med. 2015;8(1):53–58. doi: 10.1007/s12178-014-9248-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim SH, Yoo JC, Wang JH, et al. Arthroscopic sliding knot: how many additional half-hitches are really needed? Arthroscopy. 2005;21(4):405–11. doi: 10.1016/j.arthro.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 26.Amstutz HC, Sew Hoy AL, Clarke IC. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981;(155):7–20. [PubMed] [Google Scholar]
- 27.Nutton RW, McBirnie JM, Phillips C. Treatment of chronic rotator-cuff impingement by arthroscopic subacromial decompression. J Bone Joint Surg (Br) 1997;79(1):73–76. doi: 10.1302/0301-620x.79b1.7225. [DOI] [PubMed] [Google Scholar]
- 28.Porcellini G, Campi F, Pegreffi F, et al. Predisposing factors for recurrent shoulder dislocation after arthroscopic treatment. J Bone Joint Surg (Am) 2009;91(11):2537–42. doi: 10.2106/JBJS.H.01126. [DOI] [PubMed] [Google Scholar]
- 29.Cole BJ, L’Insalata J, Irrgang J, Warner JJ. Comparison of arthroscopic and open anterior shoulder stabilization: a two to six-year follow-up study. J Bone Joint Surg (Am) 2000;82:1108–114. doi: 10.2106/00004623-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Sperber A, Hamberg P, Karlsson J, et al. Comparison of an arthroscopic and an open procedure for posttraumatic instability of the shoulder: a prospective, randomized multicenter study. J Shoulder Elbow Surg. 2001;10:105–8. doi: 10.1067/mse.2001.112019. [DOI] [PubMed] [Google Scholar]
- 31.Harris JD, Gupta AK, Mall NA, et al. Long-term outcomes after Bankart shoulder stabilization. Arthroscopy. 2013;29(5):920–33. doi: 10.1016/j.arthro.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 32.Garofalo R, Mocci A, Moretti B, et al. Arthroscopic treatment of anterior shoulder instability using knotless suture anchors. Arthroscopy. 2005;21(11):1283–89. doi: 10.1016/j.arthro.2005.08.033. [DOI] [PubMed] [Google Scholar]
- 33.Franceschi F, Papalia R, Del Buono A, et al. Glenohumeral osteoarthritis after arthroscopic Bankart repair for anterior instability. Am J Sports Med. 2011;39(8):1653–59. doi: 10.1177/0363546511404207. [DOI] [PubMed] [Google Scholar]
- 34.Kim SJ, Jung M, Moon HK, et al. Is the transglenoid suture technique recommendable for recurrent shoulder dislocation? A minimum 5-year follow-up in 59 non-athletic shoulders. Knee Surg Sports Traumatol Arthrosc. 2009;17(12):1458–62. doi: 10.1007/s00167-009-0748-6. [DOI] [PubMed] [Google Scholar]
- 35.Ee GW, Mohamed S, Tan AH. Long term results of arthroscopic bankart repair for traumatic anterior shoulder instability. J Orthop Surg Res. 2011;6:28. doi: 10.1186/1749-799X-6-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boileau P, Villalba M, Héry JY, et al. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88(8):1755–63. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 37.Mishra A, Sharma P, Chaudhary D. Analysis of the functional results of arthroscopic Bankart repair in posttraumatic recurrent anterior dislocations of shoulder. Indian J Orthop. 2012;46(6):668–74. doi: 10.4103/0019-5413.104205. [DOI] [PMC free article] [PubMed] [Google Scholar]