Abstract
Hydrogen peroxide (H2O2) acts as a second messenger that can mediate intracellular signal transduction via chemoselective oxidation of cysteine residues in signaling proteins. This Review presents current mechanistic insights into signal-mediated H2O2 production and highlights recent advances in methods to detect reactive oxygen species (ROS) and cysteine oxidation both in vitro and in cells. Selected examples from the recent literature are used to illustrate the diverse mechanisms by which H2O2 can regulate protein function. The continued development of methods to detect and quantify discrete cysteine oxoforms should further our mechanistic understanding of redox regulation of protein function and may lead to the development of new therapeutic strategies.
INTRODUCTION
Reactive oxygen species (ROS) including hydrogen peroxide (H2O2), superoxide (O2•−), and the hydroxyl radical (•OH) are generally deemed toxic consequences of aerobic life that are swiftly eradicated to maintain cellular homeostasis. If left unchecked, ROS can indiscriminately damage biomolecules and contribute to aging and pathologies such as cancer, diabetes, and neurodegenerative disorders (1–3). However, studies performed over the past decade also indicate that a diverse array of external signals (Table 1) stimulate the controlled production of ROS in healthy cells and have uncovered a role for oxidants as essential second messengers in intracellular signaling pathways. An important cellular target or “sensor” of ROS is the thiol (RSH) functional group of the amino acid cysteine, which can exist in a number of oxidation states such as disulfides (RSSR) or sulfenic (SOH), sulfinic (SO2H) and sulfonic (SO3H) acids (4). Such oxidative cysteine modifications can constitute a facile switch for modulating protein function, akin to phosphorylation. In this Review, we present current mechanistic insights into signal-mediated H2O2 production and highlight recent advances in methods to detect ROS and cysteine oxidation both in vitro and in cells. Selected examples from the recent literature of proteins that form disulfides, SOH, and SO2H are discussed, underscoring the variety of mechanisms by which ROS can modulate protein function and signal transduction cascades.
Table 1.
External Stimulants that Induce ROS Production.
| Stimulant | Organisma | ROS Sourceb | Effect of Stimulant | Reference |
|---|---|---|---|---|
| Peptide Growth Factors | ||||
| Epidermal growth factor (EGF) | Hs,M,R | NOXc | Proliferation | (40, 127–129) |
| Platelet-derived growth factor (PDGF) | Hs,M,R | NOX | Proliferation/Migration | (129–132) |
| Basic fibroblast growth factor (bFGF) | B | NOX | Proliferation | (133) |
| Vascular endothelial growth factor (VEGF) | P | L | Angiogenesis/Proliferation | (134) |
| Granulocyte-macrophage colony-stimulating factor (GM-CSF) | H | ND | Proliferation/Migration | (135) |
| Insulin | M,R | NOX | Glucose uptake/transport | (136, 137) |
| Cytokines | ||||
| Lipopolysaccharide (LPS) | M | NOX | Induction of immune response | (39, 42, 138) |
| Interleukin-1β (IL-1β) | Hs,M | NOX,L | Induction of immune response | (129, 139) |
| Interleukin-3 (IL-3) | Hs | ND | Induction of immune response | (135) |
| Interleukin-4 (IL-4) | Hs | NOX | Induction of immune response | (27) |
| CD28 stimulation | Hs | L | Induction of immune response/Proliferation | (140) |
| Tumor necrosis factor α (TNFα) | B,M,Hs | NOX | Apoptosis | (26, 28, 129, 133) |
| Transforming growth factor-β1 (TGF-β1) | M | ND | Cell cycle arrest | (141) |
| Agonists of GPCRsd | ||||
| Angiotensin II (AngII) | R | NOX | Hypertrophy | (22, 142–144) |
| Lysophosphatidic acid (LPA) | Hs | NOX,L | Proliferation | (145, 146) |
| Thrombin | Hs | NOX | Proliferation | (130) |
| Serotonin | Ha | NOX | Proliferation | (147) |
| Other Stimulants | ||||
| Wounding | Z | NOX | Leukocyte recruitment | (9) |
| Oxidative stress | D | MT | Differentiation | (33) |
| Reoxygenation after hypoxia | R | MT | O2•− burst | (43) |
B, bovine; D, Drosophila melanogaster; Ha, hamster; Hs, human; M, mouse; P, pig; R, rat; Z, zebrafish.
NOX, NADPH Oxidase; M, mitochondria; L, lipoxygenase; ND, not determined.
For many of these cases, the specific NOX isoform activated is unknown. Each NOX isoform demonstrates disparate tissue expression and continued studies will be required to elucidate the regulation of each NOX isoform in response to diverse external signals.
Guanosine triphosphate (GTP)-binding protein (G protein)-coupled receptors (GPCRs).
H2O2 AS A SIGNALING MOLECULE
O2•− spontaneously dismutates to H2O2, a process that is enhanced at least 1,000-fold by a class of enzymes known as superoxide dismutases (SOD) (5). In the presence of metal ions (iron or copper), H2O2 can be decomposed through the Fenton reaction to form •OH. Among these, H2O2 is the most abundant ROS (in vivo concentration of 10−7 M) with the longest half life (t1/2 = 10−5 sec) (6, 7). The relative stability and uncharged nature of H2O2 permits its enhanced diffusion across long distances and membranes, though it is likely that this oxidant is less membrane permeant than a gas such as nitric oxide. Interestingly, recent evidence indicates that O2•− may also cross membranes through anion channels (5). Owing to its highly diffusible nature, H2O2 has been shown to act as a paracrine signal both in plant cell differentiation (8) and more recently in the recruitment of immune cells to wound sites in zebrafish larvae (9). As will be discussed below, H2O2 can be quickly generated in cells, selectively perceived by downstream proteins, and undergo degradation by cellular antioxidant defense systems. Collectively, these properties make H2O2 an ideal mediator of signal transduction processes.
SIGNAL-MEDIATED ROS PRODUCTION
The mitochondrial electron transport chain (ETC) funnels electrons from reduced matrix substrates through four protein complexes (I-IV) to molecular oxygen producing water and establishing a proton gradient across the inner mitochondrial membrane. The energy from this gradient is then harnessed to drive the production of the primary cellular energy source, adenosine triphosphate (ATP). The final complex in this pathway, complex IV delivers electrons to molecular oxygen to generate water; however, electrons can leak prematurely from the ETC upstream of complex IV to cause the univalent reduction of oxygen to O2•− (6). The accidental production of O2•− by the ETC is thought to be the primary intracellular source of this oxidant, though cellular signals can also stimulate O2•− generation in the mitochondria. This process is strictly dependent upon the redox enzyme p66Shc, which has been shown to be a genetic determinant of lifespan in mammals (10). In response to signals that include growth factor deprivation, oxidative stress, or UV irradiation, p66Shc translocates to the mitochondria where it generates ROS (either H2O2 or O2•−) by delivering electrons from the ETC to molecular oxygen (Figure 1, panel a) (11, 12).
Figure 1.
Signaling-derived sources of intracellular reactive oxygen species (ROS). a) p66Shc generates pro-apoptotic ROS in the mitochondria. In response to oxidative stress, UV irradiation, or growth factor deprivation, p66Shc localizes to the mitochondria where it generates ROS (O2•− or H2O2). H2O2 ultimately produced can diffuse across the outer mitochondrial membrane to the cytosol where it can modulate the activity of diverse proteins. P66Shc-derived H2O2 also stimulates the opening of the permeability transition pore causing mitochondrial swelling and apoptosis. b) NOX enzymes assemble at discrete locations in the cell such as the plasma membrane and at focal adhesions to generate ROS in response to diverse extracellular signals. The catalytic subunit of each NOX isoform (NOX1-5, DUOX1-2) has a conserved domain structure of six transmembrane α-helices and binding sites for two heme prosthetic groups. The C-terminal intracellular domain binds the FAD and NADPH cofactors and electrons from NADPH are translocated across the membrane through the heme prosthetic groups to generate O2•− (NOX1-5) or H2O2 (DUOX1-2). Full enzymatic activity of these enzymes requires the association of co-activator proteins (NOX1-4) or Ca2+ (NOX5, DUOX1-2) to the N-terminal intracellular domain. The O2•− produced is dismutated by SOD to H2O2, which can freely diffuse across the membrane to the cytosol to regulate protein activity and signaling cascades.
P66Shc-derived ROS can diffuse into the cytoplasm where it down-regulates the activity of FoxO3, a transcription factor implicated in the expression of mitochondrial antioxidant enzymes including manganese SOD (MnSOD) and catalase (13, 14). The resulting decrease in the mitochondrial antioxidant capacity renders the organelle more susceptible to oxidative stress. This may enhance the pro-apoptotic effect of p66Shc through increased permeability of the mitochondrial inner membrane, ultimately resulting in apoptosis (15). Mice lacking p66Shc accumulate significantly less ROS over time, exhibit extended life spans and reduced incidence of aging-associated degenerative diseases without an increase in tumor frequency (10, 11, 16–18). Therefore, p66Shc has recently been deemed a potential therapeutic target for treating diseases such as neurodegenerative disorders that are associated with ROS accumulation and induction of apoptosis (6, 19, 20).
A variety of extracellular signals have also been shown to stimulate ROS production by activating NADPH oxidase (NOX) enzymes, which translocate an electron from reduced nicotinamide adenine dinucleotide phosphate (NAPDH) across the cell membrane to generate H2O2 (Table 1) (6, 9, 21–23). ROS production by these enzymes requires a catalytic subunit, of which there are seven known human isoforms (Nox1–5, Duox1 and Duox2) that show disparate cell- and tissue-specific expression patterns. Full activity of these multi-component enzymes also requires the binding of flavin adenine dinucleotide (FAD) and the association of either a distinct set of cytoplasmic coactivator proteins or calcium to the intracellular domain (Figure 1, panel b) (24). Recent work indicates that receptor-mediated NOX activation occurs through the recruitment of these additional proteins (25–27) and cofactors (27), though the precise mechanistic details appear to be pathway- and isoform-specific. For example, NOX1 and NOX2 activation by tumor necrosis factor (TNF) requires riboflavin kinase (RFK). This association may promote enzyme activation by increasing local levels of the FAD prosthetic group (28). Future studies on the mechanism of NOX activation are likely to reveal additional biochemical features that could conceivably lead to the identification of potential therapeutic targets. Lastly, it is important to note that intracellular and extracellular signals can also initiate ROS production through p66Shc- and NOX-independent mechanisms (Table 1) (29–31).
Regardless of the specific cellular source, the H2O2 signal diffuses into the cytoplasm where it can induce distinct physiological responses including proliferation, differentiation and apoptosis/necrosis (6, 32–34). However, the high diffusability of H2O2 also raises the specter of aberrant signaling. To circumvent this problem, NOX complexes appear to be targeted to distinct regions of the plasma membrane via lipid rafts (24) and assemble at focal adhesions (35) to direct H2O2 production to specific cellular microdomains. The precise mechanisms that prevent H2O2 diffusion from such microenvironments are unknown (36, 37). One possibility is that antioxidant enzymes including glutathione peroxidases, catalase, and peroxiredoxins co-localize with NOX complexes to limit extraneous ROS dissemination (24).
CELLULAR ROS DETECTION
The subcellular location and relative ROS concentration produced in response to external signals can have a dramatic impact on the cellular outcome (e.g. proliferation or apoptosis). Chemical probes for oxidant detection have emerged as essential tools to probe signal-mediated ROS production in cells (38). Compounds such as dihydrodichlorofluorescin (DCFH), dihydrorhodamine-123 (DHR), and more recently, dihydrocyanines (39) are routinely used to visualize intracellular ROS. Often times, however, these reagents exhibit high background fluorescence resulting from auto- and photo-oxidation. An innovative, new generation of reagents employs a caged boronate switch and provides chemoselective detection of cellular H2O2 (40). Ratiometric sensors (41), nanoparticles (42), and protein-based (43) systems have also been developed for ROS detection. Continued improvement in the reaction kinetics and dynamic range of these reagents should facilitate detection of intracellular ROS at subcellular resolution (44).
SENSING H2O2 THROUGH CYSTEINE OXIDATION
The reaction of H2O2 with biomolecules provides a mechanism for how cells can “sense” changes in redox balance. In proteins, the thiol side chain of the amino acid cysteine is particularly sensitive to oxidation (45). Some cysteines are more susceptible to oxidation than others and this provides a basis for specificity in ROS-mediated signaling. Thiolate anions (RS−) are intrinsically better nucleophiles and show enhanced reactivity with H2O2, compared to the thiol form (46). Thus, the pKa value of the thiol group can modulate cysteine reactivity. In proteins, a typical cysteine residue has a pKa of ~8.5. However, the presence of polar or positively charged amino acids can stabilize the thiolate form through electrostatic interactions and decrease the pKa to as low as 3.5 (45, 47).
Other determinants of cysteine reactivity toward H2O2 include access of the oxidant to its target and the presence of specific binding sites. For example, peroxiredoxins have low pKa catalytic cysteines (4.5–5.9) (48–50) that react with H2O2 with second-order rate constants of 105-108 M−1 sec−1 (51, 52). The catalytic cysteine of protein tyrosine phosphatases (PTPs) is also characterized by a low pKa value (4.6–5.5) (53, 54). However, H2O2 reacts with PTPs at second-order rate constants between 10–160 M−1 sec−1 (46, 55, 56). This difference in reactivity is likely due to the unique architecture of the peroxiredoxin active site and facilitates rapid reaction with low, endogenous levels of H2O2 (57). Importantly, the decreased reactivity of non-peroxiredoxin thiolates with H2O2 provides a potential mechanism to modulate protein activity only after robust changes in oxidant concentration (e.g., in response to external signals).
The initial reaction of a cysteine thiolate with H2O2 yields a sulfenic acid (SOH), which is implicated in a number of important biochemical transformations. Once formed, a SOH lies at a crossroad and can lead to formation of additional posttranslational modifications (PTMs) (Figure 2). The stability of a SOH is influenced, in part, by the presence of nearby cysteine residues and by the accessibility of the modification site to the low molecular weight thiol, glutathione (GSH) (4). The reaction of SOH with either a neighboring cysteine or GSH will generate a disulfide bond that, in the case of GSH, is known as S-glutathiolation (58). Both disulfide products can be reduced back to the thiol by the action of either the GSH/glutathione reductase (GSH/GSR) or the thioredoxin/thioredoxin reductase (Trx/TrxR) systems (59). Cysteine thiolates can also react with reactive nitrogen species (RNS) including nitric oxide (NO) to generate S-nitrosothiols (S-NO) that can hydrolyze to form SOH or react with a second cysteine to form a disulfide (60, 61).
Figure 2.
Oxidative modifications of protein cysteine residues. Low pKa cysteines are present in the cell as thiolates and form a sulfenic acid (SOH) upon reaction with H2O2. Once formed, the SOH can react with a second cysteine either in the same or a second protein yields a disulfide. Alternatively, a SOH can react with the low molecular weight thiol glutathione (GSH) (pink circle) to form a special disulfide known as S-glutathiolation. In the event that a neighboring cysteine or glutathione are absent, the amide nitrogen of the neighboring residue can attack the SOH to form a sulfenamide. Each of these oxoforms can be reduced by the GSH/glutathione reductase or thioredoxin/thioredoxin reductase systems to regenerate the thiols (not depicted). The SOH can also further react with H2O2 to generate the irreversible SO2H and SO3H oxoforms.
SOH can undergo further reaction with H2O2 to generate the SO2H and SO3H oxoforms (Figure 2), though the rate of these reactions is slower than observed for a thiolate (49). With the exception of one protein family, both the SO2H and SO3H modifications are considered irreversible and the latter is deemed a hallmark of diseases such as cancer, diabetes, and neurodegenerative disorders that are associated with oxidative stress (1–3). To prevent over-oxidation of critical cysteine residues, SOH may be converted to a disulfide or be S-glutathiolated. Sulfenamide (62–65) and hypervalent sulfur (66) species also form through SOH intermediates and may also safeguard against over-oxidation (Figure 2).
The switch-like nature of the disulfide and SOH highlights their ability to function as a reversible means to regulate protein function, analogous to phosphorylation. The SO2H oxoform has also emerged as an important PTM. For these reasons, efforts have been aimed at identifying proteins with redox-active cysteine residues and to elucidate the biological roles of these cysteine oxoforms. To highlight the progress in this area over the past few years, the remainder of this Review will focus on recent examples from the literature that demonstrate the diverse ways in which these PTMs regulate vital cellular processes.
DISULFIDE BONDS
Disulfide bond formation in proteins is a widely recognized cysteine modification and, under normal conditions, occurs predominately in the endoplasmic reticulum (ER). This organelle provides an oxidizing environment to facilitate disulfide bond formation in nascent proteins destined for export to the extracellular milieu (67). By contrast, the cytoplasm, nucleus, and mitochondrial matrix are reducing environments. In these compartments, cysteines are maintained in their thiol form by the combined activity of the GSH/GSR and Trx/TrxR systems (59, 67), though protein disulfides can be generated by the action of the Erv family of sulfhydryl oxidases (68). In response to external signals and under stress conditions the cytoplasm becomes more oxidizing, which allows protein disulfides to accumulate until redox balance is restored.
Disulfide bond formation can influence the catalytic activity, protein-protein interactions, and subcellular localization. Underscoring the importance of this oxoform, a number of methods have been developed to identify proteins that undergo this modification (69, 70). These approaches are typically based on loss of reactivity with thiol-modifying reagents or restoration of labeling by reducing agents such as dithiothreitol (DTT) with subsequent analysis by mass spectrometry (MS). To enable quantitative analysis of redox-sensitive cysteines, Cohen and colleagues have employed isotope-coded affinity tag (ICAT) methodology (71). This differential isotopic labeling method uses a subtractive approach to monitor fluctuations in levels of reduced protein thiols under different conditions (e.g. +/− oxidant). Jakob and coworkers have expanded the application of ICAT to develop a ratiometric labeling approach, termed OxICAT (72). This approach permits direct identification and quantitative evaluation of proteins that form disulfides under different cellular conditions.
Global studies to identify proteins that undergo disulfide bond formation implicate this modification in the regulation of numerous biological processes including redox homeostasis, chaperone activity, metabolism, transcriptional regulation, and protein translation (Table 2) (72, 73). Once formed, a disulfide can have divergent effects on protein function, which are central to the ability of H2O2 to orchestrate cellular signaling events, which can lead to diverse biological outcomes (Table 2). For example, starvation-induced autophagy is associated with a temporary increase in ROS production that inactivates a key cysteine protease, Atg4 by forming a disulfide bond involving the catalytic cysteine (74). In contrast, survival of bacteria such as Escherichia coli under conditions of both oxidative and heat stresses requires activation of the molecular chaperone Hsp33 via intramolecular disulfide bond formation (75).
Table 2.
Examples of Redox-Regulated Proteins and Complexes.
| Protein | Oxoforma,b | Effect of Oxidation on Protein | Reference |
|---|---|---|---|
| Phosphatases | |||
| LMW-PTPs | A,B | Inactivates | (90) |
| PTEN | A,B | Inactivates | (92, 95) |
| Cdc25 | A,B | Inactivates | (56, 91) |
| PTP1B | A,B,C | Inactivates | (63, 64) |
| PTP2α | A,B,C | Inactivates | (65) |
| SHP-1/SHP-2 | A,B | Inactivates | (94) |
| Kinases | |||
| Sty1/Tpx1 | A | Activates | (148) |
| PKA RI | A | Activates | (149) |
| Src tyrosine kinase | A | Activates/Inactivates | (150, 151) |
| PKG-1α | A | Enhances affinity for substrates | (76) |
| ASK1 | A | Initiates oligomerization/Activates | (123) |
| Transcription factors | |||
| AP-1 (Fos/Jun) | A | Inhibits DNA binding | (77) |
| Hsf1 | A | Activates | (152, 153) |
| Nrf-2/Keap-1 | A | Enhances Nrf-2 stability | (121) |
| FoxO4/p300/CBP | A | Acetylates/Inactivates | (82) |
| OxyR | A,B | Activates | (78, 79) |
| Yap1/Gpx3 | A,B | Activates | (106, 126, 154) |
| OhrR | A,B | Inhibits DNA binding | (62, 155) |
| SarZ | A,B | Inhibits DNA binding | (86) |
| Other | |||
| Hsp33 | A | Activates | (75) |
| HDAC4/DnaJb5 | A | Inactivates/Inhibits complex formation | (80) |
| GDE2 | A | Inactivates | (96) |
| DJ-1 | D | Locates to mitochondria/Active as a cytoprotectant | (114, 115) |
| MMP-7 | D | Activates | (113) |
The significance of oxidation for many of these proteins in live cells remains to be determined.
A, inter/intramolecular disulfide; B, sulfenic acid; C, sulfenamide; D, sulfinic acid.
H2O2 can also regulate the activity of protein tyrosine phosphatases (PTPs) by inducing intramolecular disulfide bond formation, which inactivates the phosphatases to permit prolonged flux through the corresponding signaling pathways (Table 2). Protein kinases are also believed to undergo redox control; however, the evidence for this is less direct since increased activity may also be attributed to inhibition of the opposing phosphatase. Recently, the serine/threonine kinase, PKGIα was shown to undergo intermolecular disulfide formation between monomers and this modification appears to enhance its affinity for target proteins (76).
The terminal targets of signal transduction cascades are transcription factors that regulate gene expression. Some transcription factors, such as AP-1 (77) and OxyR (78, 79) appear to be regulated by direct oxidative modification (Table 2). The activity of transcription factors can also be regulated by changes in the accessibility of their target genes, for example, by PTM of histones. The class II histone deacetylases (HDACs) function as transcriptional corepressors of various developmental and differentiation processes. The activity of one isoform, HDAC4 is regulated by its interaction with the small molecular chaperone DnaJb5 (80). This chaperone forms a multiprotein complex with thioredoxin (Trx1) and importin α (Imp), a component of the nuclear import machinery, through the adapter protein Trx binding protein-2 (TBP-2) (Figure 3) (81). In a recent study, Sadoshima and colleagues demonstrated that cysteine residues in DnaJb5 can form a disulfide preventing its interaction with HDAC4. Dissociation from the DnaJb5 multiprotein complex coupled with disulfide bond formation in HDAC4 exposed the nuclear export signal (NES) resulting in cytoplasmic localization of HDAC4 and derepression of its target genes (80). Sadoshima and coworkers proposed a model whereby Trx1 reduces intramolecular disulfides in DnaJb5 and HDAC to restore complex formation and nuclear accumulation (Figure 3). This model presents a mechanism for how signal-mediated H2O2 production may promote developmental defects such as cardiac hypertrophy and highlights this pathway as a potential target for therapeutic intervention.
Figure 3.
Model for redox-regulation of cardiac hypertrophy by HDAC4. The type-II histone deacetylase, HDAC4 normally modifies histones to repress the expression of genes involved in hypertrophy. Nuclear localization of HDAC4 is mediated by its association with importin α (Imp) through a multiprotein complex consisting of the molecular chaperone DnaJb5, TBP-2, and Trx1. In the presence of H2O2, intramolecular disulfide bonds form within HDCA4 and DnaJb5, which stimulates dissociation and nuclear export of the complex. Upon removal of H2O2, Trx1 reduces the disulfides in both HDAC4 and DnaJb5 to restore formation and nuclear localization of the complex.
Disulfide bond formation can also lead to additional PTM of oxidized proteins and represents another important mechanism to modulate activity. An example of such a regulatory mechanism was recently demonstrated for the FoxO4 transcription factor, which is inactivated by forming an intermolecular disulfide with either the p300 or CREB-binding protein (CBP) acetyltransferases (82). Caspase-9, the initial caspase in the mitochondrial apoptotic cascade also appears to be regulated in this manner since formation of an intermolecular disulfide with apoptotic protease-activating factor 1 (Apaf-1) stimulates auto-cleavage of caspase-9 and initiation of the apoptotic cascade (83).
SULFENIC ACIDS
Sulfenic acids are relatively unstable and reactive groups, which have traditionally been viewed as intermediates en route to other oxidation states (Figure 2). In recent years, however, stable SOH have been identified in a growing list of proteins and received intense interest for their roles in cell signaling (Table 2) (4, 36, 84). Indeed, the appropriate protein microenvironment can lead to stable SOH formation. For example, SOH modification of human serum albumin can persist for hours (85) and has been observed in more than 40 crystal structures (47, 86).
The PTP family of phosphatases is another commonly cited example of SOH-mediated regulation of activity (87–89). In these enzymes, the low pKa catalytic cysteine can oxidize to SOH with concomitant inactivation. Crystal structures of PTP1B and PTPα demonstrate that the SOH modification can react with the backbone amide nitrogen of a neighboring amino acid to form a cyclic sulfenamide (63–65). However, the rate of sulfenamide formation is slow relative to reaction of the SOH intermediate with thiols such as GSH or cysteine (62). Alternatively, the SOH intermediate in PTPs can condense with a proximal “backdoor” cysteine to generate an intramolecular disulfide, as has been observed for low molecular weight (LMW) (90), Cdc25 (56, 91), and PTEN phosphatases (92). Two members of the tandem Src homology 2 (SH2) domain-containing PTPs (SHPs) also undergo oxidative modification in activated T cells (93). Interestingly, SHPs possess two “backdoor” cysteines that comprise a unique regulatory mechanism (94). Sequential reaction of these proximal cysteines with the SOH intermediate and subsequent disulfide exchange generates a disulfide between the “backdoor” cysteines that inactivates the enzyme.
Peroxidases and peroxiredoxins also form SOH intermediates as part of their catalytic cycle (36). The primary role of these enzymes is to metabolize peroxides and maintain the reducing environment of the cell. Recent studies, however, reveal additional regulatory functions for these antioxidant enzymes. For example, peroxiredoxin 1 (Prdx1) was shown to promote PTEN tumor suppressor activity by protecting against oxidative inactivation (95). A molecular mechanism was not provided in this study, however, it is possible that Prdx1 either neutralizes local H2O2 to prevent PTEN oxidation or acts as a reductase to reduce the PTEN disulfide. The latter activity is analogous to the newly elucidated role for Prdx1 in promoting neuronal cell differentiation (96).
Small molecule probes that recognize specific cysteine oxoforms over similar species represent promising new tools for elucidating signaling pathways and regulatory mechanisms that involve redox signaling and thiol oxidation. To this end, approaches have been developed that allow for the detection of sulfenic acid modifications on proteins that exploit the unique chemical reactivity of this species (97–102). Although SOH are often metastable species, the direct detection of SOH formation has several advantages including the identification of the reactive site where the oxidation chemistry was initiated (36).
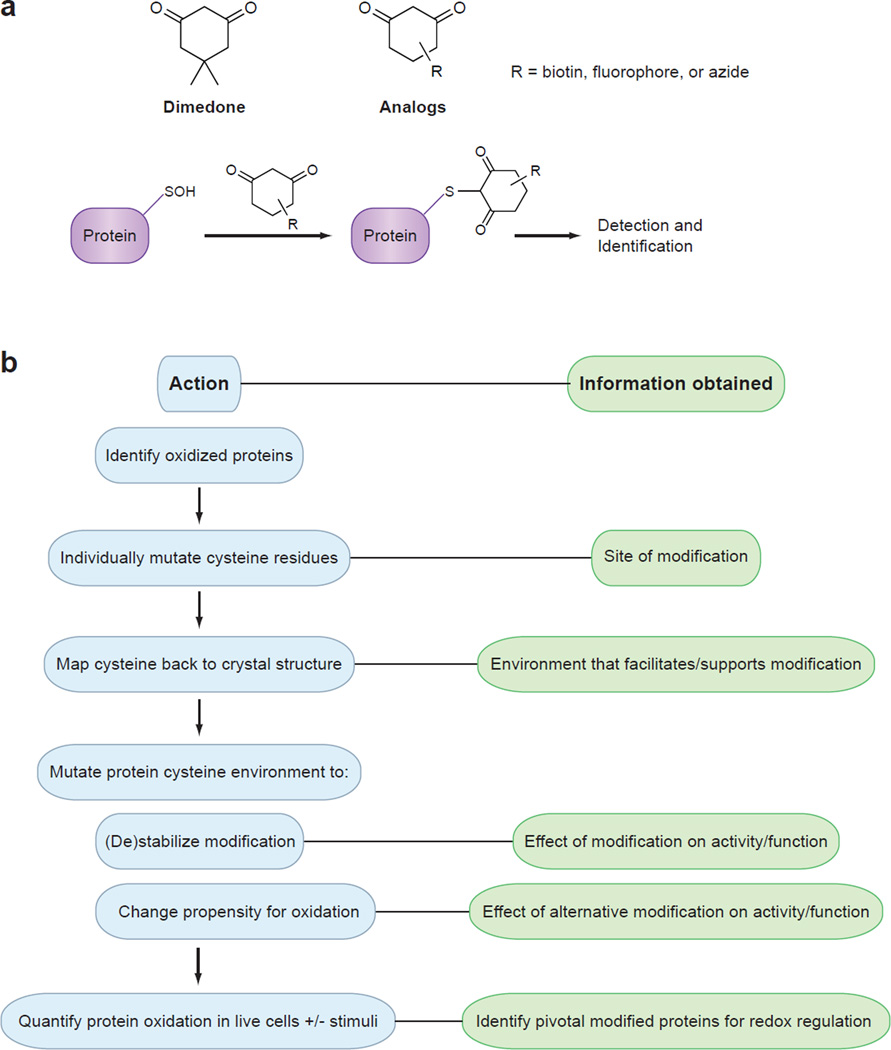
All recently developed reagents for sulfenic acid detection are based on 5,5-dimethyl-1,3-cyclohexanedione, also known as dimedone (Figure 4, panel a). The chemoselective reaction between dimedone and a protein SOH was first reported by Benitez and Allison in 1974 (103, 104). Since then, this reaction has been exploited to detect SOH modifications by MS and through direct conjugation to fluorophores and biotin (97, 99). More recently, azide analogs of dimedone known as DAz-1 (100, 101) and DAz-2 (98) have been developed that can be used to label sulfenic acid-containing proteins in live cells, thereby minimizing the potential for oxidative artifacts during cell lysis. Proteins tagged by the azidodimedone analogs can be conjugated to biotin or fluorophores via chemical ligation techniques such as the Staudinger ligation or click chemistry (Figure 4, panel a) (101, 105). Application of azidodimedone probes to discover protein targets of oxidation in human cell lines has shown that as many as 200 different cellular proteins undergo SOH modification (98). The newly identified proteins have roles in signal transduction, DNA repair, metabolism, protein synthesis, redox homeostasis, nuclear transport, vesicle trafficking, and ER quality control. Azidodimedone probes have also been used to identify a functional role for SOH modifications in the yeast peroxide-sensing system comprising the peroxidase Gpx3 and the transcription factor Yap1 (106).
Figure 4.
Detection and characterization of oxidized proteins. a) Structures and reaction scheme for chemoselective tools used to detect protein SOH in vitro and in vivo. b) Flowchart of steps that can be undertaken and the corresponding information obtained to elucidate the significance and prevalence of protein oxidation in vivo.
SULFINIC ACIDS
The SO2H modification has been best characterized in peroxiredoxins and forms through reaction of H2O2 with the SOH intermediate. Notably, only the eukaryotic homologues of the peroxiredoxins are susceptible to SO2H formation (107, 108). For a subset of eukaryotic peroxiredoxins, the SO2H modification can be reversed by an enzyme termed, sulfiredoxin (109). Recent studies indicate that SO2H repair proceeds through a sulfinic acid phosphoryl ester intermediate formed by the direct transfer of the γ-phosphate from ATP to peroxiredoxin (110–112). The reversibility of SO2H in peroxiredoxins suggests that this modification may also function as a controllable redox switch in proteins. Indeed, Poole and coworkers have proposed the floodgate model of signaling, which posits that SO2H modification of peroxiredoxin permits a temporary increase in cellular H2O2 (108). In addition to peroxiredoxins, important biological functions for SO2H modifications have been demonstrated in matrix metalloproteases (113) and the Parkinson’s disease protein DJ-1 (114, 115). Although oxidation of cysteine to SO2H is gaining acceptance as an important regulatory mechanism as well as a marker of protein damage, the full scope of these modifications remain unknown. The development of chemical tools for SO2H detection may afford new opportunities to elucidate the role of this modification in human health and disease.
REGULATION OF PROTEIN SIGNALING COMPLEXES
H2O2 can also influence protein activity through oxidative modification of regulatory protein complexes, as illustrated by the mammalian NRF2/KEAP1 system. NRF2 is a basic leucine zipper (bZIP) transcription factor that regulates the expression of enzymes involved in oxidant and xenobiotic detoxification (116). This transcription factor has a nuclear localization sequence (NLS), however, it is held in the cytoplasm under non-stress conditions by KEAP1, which functions as a homodimer and interacts with the DLG and ETGE sites of NRF2 (Figure 5, panel a) (117, 118). KEAP1 serves as an adaptor for an ubiquitin ligase complex and binding of KEAP1 to both the DLG and ETGE sites optimally orients NRF2 lysine residues for ubiquitination, which targets it for degradation (119). Nuclear accumulation and activation of NRF2 in response to oxidative stress is associated with increased NRF2 stability and is dependent upon oxidative modification of three cysteine residues in KEAP1, which weakens its interaction with the DLG motif in NRF2 (117–120). Until recently, it was not clear how KEAP1 oxidation enhances the stability of NRF2 since oxidized KEAP1 still interacts fully with the ETGE site and weakly with the DLG site. A new study demonstrated that p21Cip1/WAF1, a protein involved in numerous cellular processes including cell-cycle arrest and apoptosis, could compete with KEAP1 for binding to the DLG site of NRF2. Displacement of KEAP1 by p21CIP1/WAF1 inhibits KEAP1-mediated ubiquitination of NRF2 and provides a unique regulatory role for p21Cip1/WAF1 (Figure 5, panel a) (121).
Figure 5.
Redox-regulation of protein complexes influences gene transcription and signaling cascades. a) Proposed mechanism for redox-regulation of NRF2 stability and activity by KEAP1 and p21CIP1/WAF1. Binding of KEAP1 to the DLG and ETGE sites in NRF2 optimally orients lysine residues in NRF2 for ubiquitination (black circles) leading to degradation. In the presence of H2O2, three cysteine residues in KEAP1 are oxidatively modified (oxoform unknown, S*), which induces a conformational change in KEAP1 that decreases its affinity for the DLG site. Additionally, KEAP1 oxidation may mask its NES leading to nuclear accumulation of the complex and activation of NRF2. p21CIP1/WAF1 can compete with oxidized KEAP1 for binding to the NRF2 DLG site to enhance the stability of the transcription factor. b) Two proposed models for H2O2-mediated activation of ASK1. ASK1 assembles into multimers in the cell that interact with Trx1. Association of Trx1 with ASK1 sequesters the kinase in an inactive conformation. Upon oxidation of Trx1 by H2O2, ASK1 is released to interact with additional proteins forming the active signaling complex (Trx1-oxidation model). Alternatively, H2O2 induces intermolecular disulfide bond formation between ASK1 monomers to facilitate the interaction with additional proteins forming the activate kinase complex (ASK1-oxidation model). In this second model, Trx1 negatively regulates ASK1 by maintaining the kinase in a reduced and inactivate state.
The apoptosis signal-regulating kinase (ASK1)/Trx1 system represents another H2O2-sensitive protein complex (Figure 5b). Two models have been proposed to explain H2O2-mediated activation of ASK1. One model posits that Trx1 sequesters ASK1 in an inactive complex and, upon treatment of cells with TNF or H2O2, undergoes intramolecular disulfide formation. In subsequent steps, ASK1 is released, which permits oligomerization to form the active kinase complex (Figure 5, panel b, left) (122). A recent study, however, demonstrated that stable ASK1 oligomerization and activation in response to H2O2 is mediated by disulfide bond formation between ASK1 monomers (123). Hence, an alternative regulatory model was presented whereby Trx1 negatively regulates ASK1 signaling under resting conditions by maintaining it in a reduced state (Figure 5, panel b, right). This alternative model is attractive since it is consistent with the known disulfide reductase activity of Trx1.
Prolonged activation of ASK1 by TNF signaling induces apoptosis, which is also associated with ROS production from the NOX1 complex (26). ASK1 activates the Jun N-terminal kinase (JNK) and p38MAPK-signaling pathways. The latter is required for induction of mitochondrial apoptosis during oxidative stress by enhancing the stability of p53 (124). Interestingly, p53 regulates the expression of p66Shc, which is required for stress-activated p53 to stimulate mitochondrial ROS production and apoptosis (19). This apoptotic signaling pathway provides an attractive mechanistic link between NOX activation and the initiation of p66Shc-dependent mitochondrial ROS production, though further studies will be required to evaluate this potential connection.
CYSTEINE OXIDATION IN DISEASE
To date, a number of proteins have been identified wherein chemoselective oxidation of cysteine residues serves as a mechanism to regulate normal cellular functions (Table 2). It is important to note, however, that excessive H2O2 production, either through aberrant receptor activation or mitochondrial dysfunction can lead to spurious modification and hyper-oxidation of cysteines. This would be expected, for example, in disease states that are associated with excessive ROS production such as cancer, diabetes, or neurodegenerative disorders (1–3). Consistent with this proposal, a recent study found that SOH modification of proteins is enhanced in malignant breast cell lines using an antibody that recognizes the protein-dimedone adduct (102). Although Trx/TrxR, GSH/GSR and the recently identified bacterial sulfenate reductase (125) can repair reversible forms of thiol oxidation, persistent oxidative stress can overpower these systems can lead to aberrant protein oxidation that may contribute to disease pathogenesis.
FUTURE PERSPECTIVES
The recent development of chemical tools to detect cellular ROS as well as mechanistic studies into NOX enzymes activation and p66Shc have greatly expanded our understanding of how ROS are produced in response to diverse external signals. Continued development of ROS-sensing reagents should facilitate the temporal and spatial resolution of signal-mediated ROS production. Once formed, ROS can modulate the activity of proteins and regulate signaling pathways involved in cell proliferation, cell differentiation, and apoptosis via chemoselective oxidation of cysteine residues. The recent development of methods to detect disulfides and SOH has expanded the inventory of protein cysteine residues known to undergo oxidation modifications, though probes for SO2H are lacking. Such proteins targets of oxidation are implicated in a wide array of cellular processes including signal transduction, DNA repair, metabolism, protein synthesis, redox homeostasis, nuclear transport, vesicle trafficking, and ER quality control. Though some reactive cysteines are susceptible to numerous modifications, the majority of thiols appear to undergo specific oxidative PTMs, which suggests that there are fundamental differences in the chemical and biological basis for target specificity (98).
Profiling oxidized proteins (i.e., inventory mapping) serves as the first step to elucidating the biological roles of these cysteine PTMs (Figure 4, panel b). Mapping sites of cysteine modification can be used to expand our understanding of features within a protein microenvironment that facilitate the oxidation process. The transition from inventory mapping to the mapping of functional cellular context will be greatly facilitated by genetic and biochemical experiments. For example, site-directed mutagenesis can be employed to remove the modified cysteine or alter the protein environment in order to influence the redox sensitivity, as in DJ-1 (114) and Gpx3 (126). Another important step toward evaluating the physiological significance of oxidative cysteine modifications will be to quantify redox-dependent changes in the extent of protein oxidation. To this end, the OxICAT method (72) should facilitate such analysis for disulfide bond formation. Since increased H2O2 concentrations can lead to aberrant SOH formation (102), similar ratiometric methods should be developed for SOH to hone in on the modified proteins that are pivotal for regulation of cellular signaling.
Studies reported in the last three years have expanded our knowledge regarding mechanisms of signal-mediated ROS production and the means by which ROS regulate cellular signaling networks. The continued emergence of methods to detect and quantify discrete cysteine oxoforms should further our mechanistic understanding of redox regulation of protein function and could lead to the development of new therapeutics.
Supplementary Material
ACKNOWLEDGEMENTS
We thank the CBI Training Program T32-GM-008597-13 to C.E.P. and the Life Sciences Institute and the American Heart Association Scientist Development Grant #0835419N to K.S.C. for support of this work.
REFERENCES
- 1.Andersen JK. Oxidative stress in neurodegeneration: cause or consequence? Nat. Med. 2004;10(Suppl):S18–S25. doi: 10.1038/nrn1434. [DOI] [PubMed] [Google Scholar]
- 2.Klaunig JE, Kamendulis LM. The role of oxidative stress in carcinogenesis. Annu. Rev. Pharmacol. Toxicol. 2004;44:239–267. doi: 10.1146/annurev.pharmtox.44.101802.121851. [DOI] [PubMed] [Google Scholar]
- 3.Lowell BB, Shulman GI. Mitochondrial dysfunction and type 2 diabetes. Science. 2005;307:384–387. doi: 10.1126/science.1104343. [DOI] [PubMed] [Google Scholar]
- 4.Reddie KG, Carroll KS. Expanding the functional diversity of proteins through cysteine oxidation. Curr. Opin. Chem. Biol. 2008;12:746–754. doi: 10.1016/j.cbpa.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 5.Mumbengegwi DR, Li Q, Li C, Bear CE, Engelhardt JF. Evidence for a superoxide permeability pathway in endosomal membranes. Mol. Cell. Biol. 2008;28:3700–3712. doi: 10.1128/MCB.02038-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giorgio M, Trinei M, Migliaccio E, Pelicci PG. Hydrogen peroxide: a metabolic by-product or a common mediator of ageing signals? Nat. Rev. Mol. Cell. Biol. 2007;8:722–728. doi: 10.1038/nrm2240. [DOI] [PubMed] [Google Scholar]
- 7.Halliwell B, Gutteridge JMC. Free Radicals in Biology and Medicine. Oxford: Oxford University Press; 1999. [Google Scholar]
- 8.Bienert GP, Schjoerring JK, Jahn TP. Membrane transport of hydrogen peroxide. Biochim. Biophys. Acta. 2006;1758:994–1003. doi: 10.1016/j.bbamem.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 9.Niethammer P, Grabher C, Look AT, Mitchison TJ. A tissue-scale gradient of hydrogen peroxide mediates rapid wound detection in zebrafish. Nature. 2009;459:996–999. doi: 10.1038/nature08119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Migliaccio E, Giorgio M, Mele S, Pelicci G, Reboldi P, Pandolfi PP, Lanfrancone L, Pelicci PG. The p66shc adaptor protein controls oxidative stress response and life span in mammals. Nature. 1999;402:309–313. doi: 10.1038/46311. [DOI] [PubMed] [Google Scholar]
- 11.Giorgio M, Migliaccio E, Orsini F, Paolucci D, Moroni M, Contursi C, Pelliccia G, Luzi L, Minucci S, Marcaccio M, Pinton P, Rizzuto R, Bernardi P, Paolucci F, Pelicci PG. Electron transfer between cytochrome c and p66Shc generates reactive oxygen species that trigger mitochondrial apoptosis. Cell. 2005;122:221–233. doi: 10.1016/j.cell.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 12.Orsini F, Migliaccio E, Moroni M, Contursi C, Raker VA, Piccini D, Martin-Padura I, Pelliccia G, Trinei M, Bono M, Puri C, Tacchetti C, Ferrini M, Mannucci R, Nicoletti I, Lanfrancone L, Giorgio M, Pelicci PG. The life span determinant p66Shc localizes to mitochondria where it associates with mitochondrial heat shock protein 70 and regulates trans-membrane potential. J. Biol. Chem. 2004;279:25689–25695. doi: 10.1074/jbc.M401844200. [DOI] [PubMed] [Google Scholar]
- 13.Guo J, Gertsberg Z, Ozgen N, Steinberg SF. p66Shc links alpha1-adrenergic receptors to a reactive oxygen species-dependent AKT-FOXO3A phosphorylation pathway in cardiomyocytes. Circ. Res. 2009;104:660–669. doi: 10.1161/CIRCRESAHA.108.186288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nemoto S, Finkel T. Redox regulation of forkhead proteins through a p66shc-dependent signaling pathway. Science. 2002;295:2450–2452. doi: 10.1126/science.1069004. [DOI] [PubMed] [Google Scholar]
- 15.Bernardi P, Petronilli V, Di Lisa F, Forte M. A mitochondrial perspective on cell death. Trends Biochem. Sci. 2001;26:112–117. doi: 10.1016/s0968-0004(00)01745-x. [DOI] [PubMed] [Google Scholar]
- 16.Francia P, delli Gatti C, Bachschmid M, Martin-Padura I, Savoia C, Migliaccio E, Pelicci PG, Schiavoni M, Luscher TF, Volpe M, Cosentino F. Deletion of p66shc gene protects against age-related endothelial dysfunction. Circulation. 2004;110:2889–2895. doi: 10.1161/01.CIR.0000147731.24444.4D. [DOI] [PubMed] [Google Scholar]
- 17.Menini S, Amadio L, Oddi G, Ricci C, Pesce C, Pugliese F, Giorgio M, Migliaccio E, Pelicci P, Iacobini C, Pugliese G. Deletion of p66Shc longevity gene protects against experimental diabetic glomerulopathy by preventing diabetes-induced oxidative stress. Diabetes. 2006;55:1642–1650. doi: 10.2337/db05-1477. [DOI] [PubMed] [Google Scholar]
- 18.Rota M, LeCapitaine N, Hosoda T, Boni A, De Angelis A, Padin-Iruegas ME, Esposito G, Vitale S, Urbanek K, Casarsa C, Giorgio M, Luscher TF, Pelicci PG, Anversa P, Leri A, Kajstura J. Diabetes promotes cardiac stem cell aging and heart failure, which are prevented by deletion of the p66shc gene. Circ. Res. 2006;99:42–52. doi: 10.1161/01.RES.0000231289.63468.08. [DOI] [PubMed] [Google Scholar]
- 19.Pani G, Koch OR, Galeotti T. The p53-p66shc-manganese superoxide dismutase (MnSOD) network: a mitochondrial intrigue to generate reactive oxygen species. Int. J. Biochem. Cell Biol. 2009;41:1002–1005. doi: 10.1016/j.biocel.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 20.Pinton P, Rizzuto R. p66Shc, oxidative stress and aging: importing a lifespan determinant into mitochondria. Cell Cycle. 2008;7:304–308. doi: 10.4161/cc.7.3.5360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ameziane-El-Hassani R, Morand S, Boucher JL, Frapart YM, Apostolou D, Agnandji D, Gnidehou S, Ohayon R, Noel-Hudson MS, Francon J, Lalaoui K, Virion A, Dupuy C. Dual oxidase-2 has an intrinsic Ca2+-dependent H2O2-generating activity. J. Biol. Chem. 2005;280:30046–30054. doi: 10.1074/jbc.M500516200. [DOI] [PubMed] [Google Scholar]
- 22.Block K, Eid A, Griendling KK, Lee DY, Wittrant Y, Gorin Y. Nox4 NAD(P)H oxidase mediates Src-dependent tyrosine phosphorylation of PDK-1 in response to angiotensin II: role in mesangial cell hypertrophy and fibronectin expression. J. Biol. Chem. 2008;283:24061–24076. doi: 10.1074/jbc.M803964200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garrido AM, Griendling KK. NADPH oxidases and angiotensin II receptor signaling. Mol. Cell. Endocrinol. 2009;302:148–158. doi: 10.1016/j.mce.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen K, Craige SE, Keaney JF., Jr Downstream targets and intracellular compartmentalization in Nox signaling. Antioxid. Redox Signal. 2009;11:2467–2480. doi: 10.1089/ars.2009.2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choi H, Leto TL, Hunyady L, Catt KJ, Bae YS, Rhee SG. Mechanism of angiotensin II-induced superoxide production in cells reconstituted with angiotensin type 1 receptor and the components of NADPH oxidase. J. Biol. Chem. 2008;283:255–267. doi: 10.1074/jbc.M708000200. [DOI] [PubMed] [Google Scholar]
- 26.Kim YS, Morgan MJ, Choksi S, Liu ZG. TNF-induced activation of the Nox1 NADPH oxidase and its role in the induction of necrotic cell death. Mol. Cell. 2007;26:675–687. doi: 10.1016/j.molcel.2007.04.021. [DOI] [PubMed] [Google Scholar]
- 27.Sharma P, Chakraborty R, Wang L, Min B, Tremblay ML, Kawahara T, Lambeth JD, Haque SJ. Redox regulation of interleukin-4 signaling. Immunity. 2008;29:551–564. doi: 10.1016/j.immuni.2008.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yazdanpanah B, Wiegmann K, Tchikov V, Krut O, Pongratz C, Schramm M, Kleinridders A, Wunderlich T, Kashkar H, Utermohlen O, Bruning JC, Schutze S, Kronke M. Riboflavin kinase couples TNF receptor 1 to NADPH oxidase. Nature. 2009;460:1159–1163. doi: 10.1038/nature08206. [DOI] [PubMed] [Google Scholar]
- 29.Ali MH, Mungai PT, Schumacker PT. Stretch-induced phosphorylation of focal adhesion kinase in endothelial cells: role of mitochondrial oxidants. Am. J. Physiol. 2006;291:L38–L45. doi: 10.1152/ajplung.00287.2004. [DOI] [PubMed] [Google Scholar]
- 30.Fay AJ, Qian X, Jan YN, Jan LY. SK channels mediate NADPH oxidase-independent reactive oxygen species production and apoptosis in granulocytes. Proc. Natl. Acad. Sci. U.S.A. 2006;103:17548–17553. doi: 10.1073/pnas.0607914103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Handy DE, Lubos E, Yang Y, Galbraith JD, Kelly N, Zhang YY, Leopold JA, Loscalzo J. Glutathione peroxidase-1 regulates mitochondrial function to modulate redox-dependent cellular responses. J. Biol. Chem. 2009;284:11913–11921. doi: 10.1074/jbc.M900392200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kwon SH, Pimentel DR, Remondino A, Sawyer DB, Colucci WS. H(2)O(2) regulates cardiac myocyte phenotype via concentration-dependent activation of distinct kinase pathways. J. Mol. Cell. Cardiol. 2003;35:615–621. doi: 10.1016/s0022-2828(03)00084-1. [DOI] [PubMed] [Google Scholar]
- 33.Owusu-Ansah E, Banerjee U. Reactive oxygen species prime Drosophila haematopoietic progenitors for differentiation. Nature. 2009;461:537–541. doi: 10.1038/nature08313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Veal EA, Day AM, Morgan BA. Hydrogen peroxide sensing and signaling. Mol. Cell. 2007;26:1–14. doi: 10.1016/j.molcel.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 35.Wu RF, Xu YC, Ma Z, Nwariaku FE, Sarosi GA, Jr, Terada LS. Subcellular targeting of oxidants during endothelial cell migration. J. Cell Biol. 2005;171:893–904. doi: 10.1083/jcb.200507004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Poole LB, Nelson KJ. Discovering mechanisms of signaling-mediated cysteine oxidation. Curr. Opin. Chem. Biol. 2008;12:18–24. doi: 10.1016/j.cbpa.2008.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ushio-Fukai M. Localizing NADPH oxidase-derived ROS. Sci. STKE 2006. 2006:re8. doi: 10.1126/stke.3492006re8. [DOI] [PubMed] [Google Scholar]
- 38.Miller EW, Chang CJ. Fluorescent probes for nitric oxide and hydrogen peroxide in cell signaling. Curr. Opin. Chem. Biol. 2007;11:620–625. doi: 10.1016/j.cbpa.2007.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kundu K, Knight SF, Willett N, Lee S, Taylor WR, Murthy N. Hydrocyanines: a class of fluorescent sensors that can image reactive oxygen species in cell culture, tissue, and in vivo. Angew. Chem., Int. Ed. 2009;48:299–303. doi: 10.1002/anie.200804851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miller EW, Tulyathan O, Isacoff EY, Chang CJ. Molecular imaging of hydrogen peroxide produced for cell signaling. Nat. Chem. Biol. 2007;3:263–267. doi: 10.1038/nchembio871. [DOI] [PubMed] [Google Scholar]
- 41.Srikun D, Miller EW, Domaille DW, Chang CJ. An ICT-based approach to ratiometric fluorescence imaging of hydrogen peroxide produced in living cells. J. Am. Chem. Soc. 2008;130:4596–4597. doi: 10.1021/ja711480f. [DOI] [PubMed] [Google Scholar]
- 42.Lee D, Khaja S, Velasquez-Castano JC, Dasari M, Sun C, Petros J, Taylor WR, Murthy N. In vivo imaging of hydrogen peroxide with chemiluminescent nanoparticles. Nat. Mat. 2007;6:765–769. doi: 10.1038/nmat1983. [DOI] [PubMed] [Google Scholar]
- 43.Wang W, Fang H, Groom L, Cheng A, Zhang W, Liu J, Wang X, Li K, Han P, Zheng M, Yin J, Wang W, Mattson MP, Kao JP, Lakatta EG, Sheu SS, Ouyang K, Chen J, Dirksen RT, Cheng H. Superoxide flashes in single mitochondria. Cell. 2008;134:279–290. doi: 10.1016/j.cell.2008.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dickinson BC, Chang CJ. A targetable fluorescent probe for imaging hydrogen peroxide in the mitochondria of living cells. J. Am. Chem. Soc. 2008;130:9638–9639. doi: 10.1021/ja802355u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Banerjee R, editor. Redox Biochemistry. New Jersey: John Wiley & Sons; 2008. [Google Scholar]
- 46.Winterbourn CC, Metodiewa D. Reactivity of biologically important thiol compounds with superoxide and hydrogen peroxide. Free Radic. Biol. Med. 1999;27:322–328. doi: 10.1016/s0891-5849(99)00051-9. [DOI] [PubMed] [Google Scholar]
- 47.Salsbury FR, Jr, Knutson ST, Poole LB, Fetrow JS. Functional site profiling and electrostatic analysis of cysteines modifiable to cysteine sulfenic acid. Protein Sci. 2008;17:299–312. doi: 10.1110/ps.073096508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bryk R, Griffin P, Nathan C. Peroxynitrite reductase activity of bacterial peroxiredoxins. Nature. 2000;407:211–215. doi: 10.1038/35025109. [DOI] [PubMed] [Google Scholar]
- 49.Hugo M, Turell L, Manta B, Botti H, Monteiro G, Netto LE, Alvarez B, Radi R, Trujillo M. Thiol and sulfenic acid oxidation of AhpE, the one-cysteine peroxiredoxin from mycobacterium tuberculosis: kinetics, acidity constants, and conformational dynamics. Biochemistry. 2009;48:9416–9426. doi: 10.1021/bi901221s. [DOI] [PubMed] [Google Scholar]
- 50.Nelson KJ, Parsonage D, Hall A, Karplus PA, Poole LB. Cysteine pK(a) values for the bacterial peroxiredoxin AhpC. Biochemistry. 2008;47:12860–12868. doi: 10.1021/bi801718d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Parsonage D, Karplus PA, Poole LB. Substrate specificity and redox potential of AhpC, a bacterial peroxiredoxin. Proc. Natl. Acad. Sci. U.S.A. 2008;105:8209–8214. doi: 10.1073/pnas.0708308105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Peskin AV, Low FM, Paton LN, Maghzal GJ, Hampton MB, Winterbourn CC. The high reactivity of peroxiredoxin 2 with H(2)O(2) is not reflected in its reaction with other oxidants and thiol reagents. J. Biol. Chem. 2007;282:11885–11892. doi: 10.1074/jbc.M700339200. [DOI] [PubMed] [Google Scholar]
- 53.Lohse DL, Denu JM, Santoro N, Dixon JE. Roles of aspartic acid-181 and serine-222 in intermediate formation and hydrolysis of the mammalian protein-tyrosine-phosphatase PTP1. Biochemistry. 1997;36:4568–4575. doi: 10.1021/bi963094r. [DOI] [PubMed] [Google Scholar]
- 54.Zhang ZY, Dixon JE. Active site labeling of the Yersinia protein tyrosine phosphatase: the determination of the pKa of the active site cysteine and the function of the conserved histidine 402. Biochemistry. 1993;32:9340–9345. doi: 10.1021/bi00087a012. [DOI] [PubMed] [Google Scholar]
- 55.Denu JM, Tanner KG. Specific and reversible inactivation of protein tyrosine phosphatases by hydrogen peroxide: evidence for a sulfenic acid intermediate and implications for redox regulation. Biochemistry. 1998;37:5633–5642. doi: 10.1021/bi973035t. [DOI] [PubMed] [Google Scholar]
- 56.Sohn J, Rudolph J. Catalytic and chemical competence of regulation of cdc25 phosphatase by oxidation/reduction. Biochemistry. 2003;42:10060–10070. doi: 10.1021/bi0345081. [DOI] [PubMed] [Google Scholar]
- 57.Stone JR, Yang S. Hydrogen peroxide: a signaling messenger. Antioxid. Redox Signal. 2006;8:243–270. doi: 10.1089/ars.2006.8.243. [DOI] [PubMed] [Google Scholar]
- 58.Mieyal JJ, Gallogly MM, Qanungo S, Sabens EA, Shelton MD. Molecular mechanisms and clinical implications of reversible protein S-glutathionylation. Antioxid. Redox Signal. 2008;10:1941–1988. doi: 10.1089/ars.2008.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Berndt C, Lillig CH, Holmgren A. Thiol-based mechanisms of the thioredoxin and glutaredoxin systems: implications for diseases in the cardiovascular system. Am. J. Physiol. Heart Circ. Physiol. 2007;292:H1227–H1236. doi: 10.1152/ajpheart.01162.2006. [DOI] [PubMed] [Google Scholar]
- 60.Forrester MT, Foster MW, Benhar M, Stamler JS. Detection of protein S-nitrosylation with the biotin-switch technique. Free Radic. Biol. Med. 2009;46:119–126. doi: 10.1016/j.freeradbiomed.2008.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hess DT, Matsumoto A, Kim SO, Marshall HE, Stamler JS. Protein S-nitrosylation: purview and parameters. Nat. Rev. Mol. Cell. Biol. 2005;6:150–166. doi: 10.1038/nrm1569. [DOI] [PubMed] [Google Scholar]
- 62.Lee JW, Soonsanga S, Helmann JD. A complex thiolate switch regulates the Bacillus subtilis organic peroxide sensor OhrR. Proc. Natl. Acad. Sci. U.S.A. 2007;104:8743–8748. doi: 10.1073/pnas.0702081104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Salmeen A, Andersen JN, Myers MP, Meng TC, Hinks JA, Tonks NK, Barford D. Redox regulation of protein tyrosine phosphatase 1B involves a sulphenyl-amide intermediate. Nature. 2003;423:769–773. doi: 10.1038/nature01680. [DOI] [PubMed] [Google Scholar]
- 64.van Montfort RL, Congreve M, Tisi D, Carr R, Jhoti H. Oxidation state of the active-site cysteine in protein tyrosine phosphatase 1B. Nature. 2003;423:773–777. doi: 10.1038/nature01681. [DOI] [PubMed] [Google Scholar]
- 65.Yang J, Groen A, Lemeer S, Jans A, Slijper M, Roe SM, den Hertog J, Barford D. Reversible oxidation of the membrane distal domain of receptor PTPalpha is mediated by a cyclic sulfenamide. Biochemistry. 2007;46:709–719. doi: 10.1021/bi061546m. [DOI] [PubMed] [Google Scholar]
- 66.Nakamura T, Yamamoto T, Abe M, Matsumura H, Hagihara Y, Goto T, Yamaguchi T, Inoue T. Oxidation of archaeal peroxiredoxin involves a hypervalent sulfur intermediate. Proc. Natl. Acad. Sci. U.S.A. 2008;105:6238–6242. doi: 10.1073/pnas.0709822105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Go YM, Jones DP. Redox compartmentalization in eukaryotic cells. Biochim. Biophys. Acta. 2008;1780:1273–1290. doi: 10.1016/j.bbagen.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fass D. The Erv family of sulfhydryl oxidases. Biochim. Biophys. Acta. 2008;1783:557–566. doi: 10.1016/j.bbamcr.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 69.Hansen RE, Roth D, Winther JR. Quantifying the global cellular thiol-disulfide status. Proc. Natl. Acad. Sci. U.S.A. 2009;106:422–427. doi: 10.1073/pnas.0812149106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Leichert LI, Jakob U. Global methods to monitor the thiol-disulfide state of proteins in vivo. Antioxid. Redox Signal. 2006;8:763–772. doi: 10.1089/ars.2006.8.763. [DOI] [PubMed] [Google Scholar]
- 71.Sethuraman M, McComb ME, Heibeck T, Costello CE, Cohen RA. Isotope-coded affinity tag approach to identify and quantify oxidant-sensitive protein thiols. Mol. Cell. Proteomics. 2004;3:273–278. doi: 10.1074/mcp.T300011-MCP200. [DOI] [PubMed] [Google Scholar]
- 72.Leichert LI, Gehrke F, Gudiseva HV, Blackwell T, Ilbert M, Walker AK, Strahler JR, Andrews PC, Jakob U. Quantifying changes in the thiol redox proteome upon oxidative stress in vivo. Proc. Natl. Acad. Sci. U.S.A. 2008;105:8197–8202. doi: 10.1073/pnas.0707723105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Le Moan N, Clement G, Le Maout S, Tacnet F, Toledano MB. The Saccharomyces cerevisiae proteome of oxidized protein thiols: contrasted functions for the thioredoxin and glutathione pathways. J. Biol. Chem. 2006;281:10420–10430. doi: 10.1074/jbc.M513346200. [DOI] [PubMed] [Google Scholar]
- 74.Scherz-Shouval R, Shvets E, Fass E, Shorer H, Gil L, Elazar Z. Reactive oxygen species are essential for autophagy and specifically regulate the activity of Atg4. EMBO J. 2007;26:1749–1760. doi: 10.1038/sj.emboj.7601623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ilbert M, Horst J, Ahrens S, Winter J, Graf PC, Lilie H, Jakob U. The redox-switch domain of Hsp33 functions as dual stress sensor. Nat. Struct. Mol. Biol. 2007;14:556–563. doi: 10.1038/nsmb1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Burgoyne JR, Madhani M, Cuello F, Charles RL, Brennan JP, Schroder E, Browning DD, Eaton P. Cysteine redox sensor in PKGIa enables oxidant-induced activation. Science. 2007;317:1393–1397. doi: 10.1126/science.1144318. [DOI] [PubMed] [Google Scholar]
- 77.Abate C, Patel L, Rauscher FJ, 3rd, Curran T. Redox regulation of fos and jun DNA-binding activity in vitro. Science. 1990;249:1157–1161. doi: 10.1126/science.2118682. [DOI] [PubMed] [Google Scholar]
- 78.Saurin AT, Neubert H, Brennan JP, Eaton P. Widespread sulfenic acid formation in tissues in response to hydrogen peroxide. Proc. Natl. Acad. Sci. U.S.A. 2004;101:17982–17987. doi: 10.1073/pnas.0404762101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Storz G, Tartaglia LA, Ames BN. Transcriptional regulator of oxidative stress-inducible genes: direct activation by oxidation. Science. 1990;248:189–194. doi: 10.1126/science.2183352. [DOI] [PubMed] [Google Scholar]
- 80.Ago T, Liu T, Zhai P, Chen W, Li H, Molkentin JD, Vatner SF, Sadoshima J. A redox-dependent pathway for regulating class II HDACs and cardiac hypertrophy. Cell. 2008;133:978–993. doi: 10.1016/j.cell.2008.04.041. [DOI] [PubMed] [Google Scholar]
- 81.Nishinaka Y, Masutani H, Oka S, Matsuo Y, Yamaguchi Y, Nishio K, Ishii Y, Yodoi J. Importin alpha1 (Rch1) mediates nuclear translocation of thioredoxin-binding protein-2/vitamin D(3)-up-regulated protein 1. J. Biol. Chem. 2004;279:37559–37565. doi: 10.1074/jbc.M405473200. [DOI] [PubMed] [Google Scholar]
- 82.Dansen TB, Smits LM, van Triest MH, de Keizer PL, van Leenen D, Koerkamp MG, Szypowska A, Meppelink A, Brenkman AB, Yodoi J, Holstege FC, Burgering BM. Redox-sensitive cysteines bridge p300/CBP-mediated acetylation and FoxO4 activity. Nat. Chem. Biol. 2009;5:664–672. doi: 10.1038/nchembio.194. [DOI] [PubMed] [Google Scholar]
- 83.Zuo Y, Xiang B, Yang J, Sun X, Wang Y, Cang H, Yi J. Oxidative modification of caspase-9 facilitates its activation via disulfide-mediated interaction with Apaf-1. Cell Res. 2009;19:449–457. doi: 10.1038/cr.2009.19. [DOI] [PubMed] [Google Scholar]
- 84.D'Autreaux B, Toledano MB. ROS as signalling molecules: mechanisms that generate specificity in ROS homeostasis. Nat. Rev. Mol. Cell Biol. 2007;8:813–824. doi: 10.1038/nrm2256. [DOI] [PubMed] [Google Scholar]
- 85.Turell L, Botti H, Carballal S, Ferrer-Sueta G, Souza JM, Duran R, Freeman BA, Radi R, Alvarez B. Reactivity of sulfenic acid in human serum albumin. Biochemistry. 2008;47:358–367. doi: 10.1021/bi701520y. [DOI] [PubMed] [Google Scholar]
- 86.Poor CB, Chen PR, Duguid E, Rice PA, He C. Crystal structures of the reduced, sulfenic acid, and mixed disulfide forms of SarZ, a redox active global regulator in Staphylococcus aureus. J. Biol. Chem. 2009;284:23517–23524. doi: 10.1074/jbc.M109.015826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tonks NK. Redox redux: revisiting PTPs and the control of cell signaling. Cell. 2005;121:667–670. doi: 10.1016/j.cell.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 88.Tonks NK. Protein tyrosine phosphatases: from genes, to function, to disease. Nat. Rev. Mol. Cell. Biol. 2006;7:833–846. doi: 10.1038/nrm2039. [DOI] [PubMed] [Google Scholar]
- 89.Xu D, Rovira II, Finkel T. Oxidants painting the cysteine chapel: redox regulation of PTPs. Dev. Cell. 2002;2:251–252. doi: 10.1016/s1534-5807(02)00132-6. [DOI] [PubMed] [Google Scholar]
- 90.Chiarugi P. The redox regulation of LMW-PTP during cell proliferation or growth inhibition. IUBMB Life. 2001;52:55–59. doi: 10.1080/15216540252774775. [DOI] [PubMed] [Google Scholar]
- 91.Savitsky PA, Finkel T. Redox regulation of Cdc25C. J. Biol. Chem. 2002;277:20535–20540. doi: 10.1074/jbc.M201589200. [DOI] [PubMed] [Google Scholar]
- 92.Kwon J, Lee SR, Yang KS, Ahn Y, Kim YJ, Stadtman ER, Rhee SG. Reversible oxidation and inactivation of the tumor suppressor PTEN in cells stimulated with peptide growth factors. Proc. Natl. Acad. Sci. U.S.A. 2004;101:16419–16424. doi: 10.1073/pnas.0407396101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Michalek RD, Nelson KJ, Holbrook BC, Yi JS, Stridiron D, Daniel LW, Fetrow JS, King SB, Poole LB, Grayson JM. The requirement of reversible cysteine sulfenic acid formation for T cell activation and function. J. Immunol. 2007;179:6456–6467. doi: 10.4049/jimmunol.179.10.6456. [DOI] [PubMed] [Google Scholar]
- 94.Chen CY, Willard D, Rudolph J. Redox regulation of SH2-domain-containing protein tyrosine phosphatases by two backdoor cysteines. Biochemistry. 2009;48:1399–1409. doi: 10.1021/bi801973z. [DOI] [PubMed] [Google Scholar]
- 95.Cao J, Schulte J, Knight A, Leslie NR, Zagozdzon A, Bronson R, Manevich Y, Beeson C, Neumann CA. Prdx1 inhibits tumorigenesis via regulating PTEN/AKT activity. EMBO J. 2009;28:1505–1517. doi: 10.1038/emboj.2009.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yan Y, Sabharwal P, Rao M, Sockanathan S. The antioxidant enzyme Prdx1 controls neuronal differentiation by thiol-redox-dependent activation of GDE2. Cell. 2009;138:1209–1221. doi: 10.1016/j.cell.2009.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Charles RL, Schroder E, May G, Free P, Gaffney PR, Wait R, Begum S, Heads RJ, Eaton P. Protein sulfenation as a redox sensor: proteomics studies using a novel biotinylated dimedone analogue. Mol. Cell. Proteomics. 2007;6:1473–1484. doi: 10.1074/mcp.M700065-MCP200. [DOI] [PubMed] [Google Scholar]
- 98.Leonard SE, Reddie KG, Carroll KS. Mining the thiol proteome for sulfenic acid modifications reveals new targets for oxidation in cells. ACS Chem. Biol. 2009;4:783–799. doi: 10.1021/cb900105q. [DOI] [PubMed] [Google Scholar]
- 99.Poole LB, Klomsiri C, Knaggs SA, Furdui CM, Nelson KJ, Thomas MJ, Fetrow JS, Daniel LW, King SB. Fluorescent and affinity-based tools to detect cysteine sulfenic acid formation in proteins. Bioconugate Chem. 2007;18:2004–2017. doi: 10.1021/bc700257a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Reddie KG, Seo YH, Muse WB, III, Leonard SE, Carroll KS. A chemical approach for detecting sulfenic acid-modified proteins in living cells. Mol. Biosyst. 2008;4:521–531. doi: 10.1039/b719986d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Seo YH, Carroll KS. Facile synthesis and biological evaluation of a cell-permeable probe to detect redox-regulated proteins. Bioorg. Med. Chem. Lett. 2009;19:356–359. doi: 10.1016/j.bmcl.2008.11.073. [DOI] [PubMed] [Google Scholar]
- 102.Seo YH, Carroll KS. Profiling protein thiol oxidation in tumor cells using sulfenic acid-specific antibodies. Proc. Natl. Acad. Sci. U.S.A. 2009;106:16163–16168. doi: 10.1073/pnas.0903015106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Allison WS. Formation and reactions of sulfenic acids in proteins. Acc. Chem. Res. 1976;9:293–299. [Google Scholar]
- 104.Benitez LV, Allison WS. The inactivation of the acyl phosphatase activity catalyzed by the sulfenic acid form of glyceraldehyde 3-phosphate dehydrogenase by dimedone and olefins. J. Biol. Chem. 1974;249:6234–6243. [PubMed] [Google Scholar]
- 105.Agard NJ, Baskin JM, Prescher JA, Lo A, Bertozzi CR. A comparative study of bioorthogonal reactions with azides. ACS Chem. Biol. 2006;1:644–648. doi: 10.1021/cb6003228. [DOI] [PubMed] [Google Scholar]
- 106.Paulsen CE, Carroll KS. Chemical dissection of an essential redox switch in yeast. Chem. Biol. 2009;16:217–225. doi: 10.1016/j.chembiol.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 107.Karplus PA, Hall A. Structural survey of the peroxiredoxins. Subcell. Biochem. 2007;44:41–60. doi: 10.1007/978-1-4020-6051-9_3. [DOI] [PubMed] [Google Scholar]
- 108.Wood ZA, Poole LB, Karplus PA. Peroxiredoxin evolution and the regulation of hydrogen peroxide signaling. Science. 2003;300:650–653. doi: 10.1126/science.1080405. [DOI] [PubMed] [Google Scholar]
- 109.Biteau B, Labarre J, Toledano MB. ATP-dependent reduction of cysteine-sulphinic acid by S. cerevisiae sulphiredoxin. Nature. 2003;425:980–984. doi: 10.1038/nature02075. [DOI] [PubMed] [Google Scholar]
- 110.Jonsson TJ, Johnson LC, Lowther WT. Structure of the sulphiredoxin-peroxiredoxin complex reveals an essential repair embrace. Nature. 2008;451:98–101. doi: 10.1038/nature06415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jonsson TJ, Johnson LC, Lowther WT. Protein engineering of the quaternary sulfiredoxin-peroxiredoxin enzyme-substrate complex reveals the molecular basis for cysteine sulfinic acid phosphorylation. J. Biol. Chem. 2009;284:33305–33310. doi: 10.1074/jbc.M109.036400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Roussel X, Kriznik A, Richard C, Rahuel-Clermont S, Branlant G. The catalytic mechanism of Sulfiredoxin from Saccharomyces cerevisiae passes through an oxidized disulfide Sulfiredoxin intermediate that is reduced by thioredoxin. J. Biol. Chem. 2009;284:33048–33055. doi: 10.1074/jbc.M109.035352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fu X, Kassim SY, Parks WC, Heinecke JW. Hypochlorous acid oxygenates the cysteine switch domain of pro-matrilysin (MMP-7). A mechanism for matrix metalloproteinase activation and atherosclerotic plaque rupture by myeloperoxidase. J. Biol. Chem. 2001;276:41279–41287. doi: 10.1074/jbc.M106958200. [DOI] [PubMed] [Google Scholar]
- 114.Blackinton J, Lakshminarasimhan M, Thomas KJ, Ahmad R, Greggio E, Raza AS, Cookson MR, Wilson MA. Formation of a stabilized cysteine sulfinic acid is critical for the mitochondrial function of the parkinsonism protein DJ-1. J. Biol. Chem. 2009;284:6476–6485. doi: 10.1074/jbc.M806599200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Canet-Aviles RM, Wilson MA, Miller DW, Ahmad R, McLendon C, Bandyopadhyay S, Baptista MJ, Ringe D, Petsko GA, Cookson MR. The Parkinson's disease protein DJ-1 is neuroprotective due to cysteine-sulfinic acid-driven mitochondrial localization. Proc. Natl. Acad. Sci. U.S.A. 2004;101:9103–9108. doi: 10.1073/pnas.0402959101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kensler TW, Wakabayashi N, Biswal S. Cell survival responses to environmental stresses via the Keap1-Nrf2-ARE pathway. Annu. Rev. Pharmacol. Toxicol. 2007;47:89–116. doi: 10.1146/annurev.pharmtox.46.120604.141046. [DOI] [PubMed] [Google Scholar]
- 117.Tong KI, Katoh Y, Kusunoki H, Itoh K, Tanaka T, Yamamoto M. Keap1 recruits Neh2 through binding to ETGE and DLG motifs: characterization of the two-site molecular recognition model. Mol. Cell. Biol. 2006;26:2887–2900. doi: 10.1128/MCB.26.8.2887-2900.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tong KI, Padmanabhan B, Kobayashi A, Shang C, Hirotsu Y, Yokoyama S, Yamamoto M. Different electrostatic potentials define ETGE and DLG motifs as hinge and latch in oxidative stress response. Mol. Cell. Biol. 2007;27:7511–7521. doi: 10.1128/MCB.00753-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.McMahon M, Thomas N, Itoh K, Yamamoto M, Hayes JD. Dimerization of substrate adaptors can facilitate cullin-mediated ubiquitylation of proteins by a "tethering" mechanism: a two-site interaction model for the Nrf2-Keap1 complex. J. Biol. Chem. 2006;281:24756–24768. doi: 10.1074/jbc.M601119200. [DOI] [PubMed] [Google Scholar]
- 120.Velichkova M, Hasson T. Keap1 regulates the oxidation-sensitive shuttling of Nrf2 into and out of the nucleus via a Crm1-dependent nuclear export mechanism. Mol. Cell. Biol. 2005;25:4501–4513. doi: 10.1128/MCB.25.11.4501-4513.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chen W, Sun Z, Wang XJ, Jiang T, Huang Z, Fang D, Zhang DD. Direct interaction between Nrf2 and p21(Cip1/WAF1) upregulates the Nrf2-mediated antioxidant response. Mol. Cell. 2009;34:663–673. doi: 10.1016/j.molcel.2009.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Matsuzawa A, Ichijo H. Redox control of cell fate by MAP kinase: physiological roles of ASK1-MAP kinase pathway in stress signaling. Biochim. Biophys. Acta. 2008;1780:1325–1336. doi: 10.1016/j.bbagen.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 123.Nadeau PJ, Charette SJ, Toledano MB, Landry J. Disulfide Bond-mediated multimerization of Ask1 and its reduction by thioredoxin-1 regulate H(2)O(2)-induced c-Jun NH(2)-terminal kinase activation and apoptosis. Mol. Biol. Cell. 2007;18:3903–3913. doi: 10.1091/mbc.E07-05-0491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Piccirillo S, Filomeni G, Brune B, Rotilio G, Ciriolo MR. Redox mechanisms involved in the selective activation of Nrf2-mediated resistance versus p53-dependent apoptosis in adenocarcinoma cells. J. Biol. Chem. 2009;284:27721–27733. doi: 10.1074/jbc.M109.014837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Depuydt M, Leonard SE, Vertommen D, Denoncin K, Morsomme P, Wahni K, Messens J, Carroll KS, Collet J-F. A periplasmic reducing system protects single cysteine residues from oxidation. Science. 2009;326:1109–1111. doi: 10.1126/science.1179557. [DOI] [PubMed] [Google Scholar]
- 126.Ma LH, Takanishi CL, Wood MJ. Molecular mechanism of oxidative stress perception by the Orp1 protein. J. Biol. Chem. 2007;282:31429–31436. doi: 10.1074/jbc.M705953200. [DOI] [PubMed] [Google Scholar]
- 127.Bae YS, Kang SW, Seo MS, Baines IC, Tekle E, Chock PB, Rhee SG. Epidermal growth factor (EGF)-induced generation of hydrogen peroxide. Role in EGF receptor-mediated tyrosine phosphorylation. J. Biol. Chem. 1997;272:217–221. [PubMed] [Google Scholar]
- 128.Goldman R, Moshonov S, Zor U. Generation of reactive oxygen species in a human keratinocyte cell line: role of calcium. Arch. Biochem. Biophys. 1998;350:10–18. doi: 10.1006/abbi.1997.0478. [DOI] [PubMed] [Google Scholar]
- 129.Sundaresan M, Yu ZX, Ferrans VJ, Sulciner DJ, Gutkind JS, Irani K, Goldschmidt-Clermont PJ, Finkel T. Regulation of reactive-oxygen-species generation in fibroblasts by Rac1. Biochem. J. 1996;318(Pt 2):379–382. doi: 10.1042/bj3180379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Patterson C, Ruef J, Madamanchi NR, Barry-Lane P, Hu Z, Horaist C, Ballinger CA, Brasier AR, Bode C, Runge MS. Stimulation of a vascular smooth muscle cell NAD(P)H oxidase by thrombin. Evidence that p47(phox) may participate in forming this oxidase in vitro and in vivo. J. Biol. Chem. 1999;274:19814–19822. doi: 10.1074/jbc.274.28.19814. [DOI] [PubMed] [Google Scholar]
- 131.Sundaresan M, Yu ZX, Ferrans VJ, Irani K, Finkel T. Requirement for generation of H2O2 for platelet-derived growth factor signal transduction. Science. 1995;270:296–299. doi: 10.1126/science.270.5234.296. [DOI] [PubMed] [Google Scholar]
- 132.Wang Y, Lou MF. The regulation of NADPH oxidase and its association with cell proliferation in human lens epithelial cells. Invest. Ophthalmol. Vis. Sci. 2009;50:2291–2300. doi: 10.1167/iovs.08-2568. [DOI] [PubMed] [Google Scholar]
- 133.Lo YY, Cruz TF. Involvement of reactive oxygen species in cytokine and growth factor induction of c-fos expression in chondrocytes. J. Biol. Chem. 1995;270:11727–11730. doi: 10.1074/jbc.270.20.11727. [DOI] [PubMed] [Google Scholar]
- 134.Colavitti R, Pani G, Bedogni B, Anzevino R, Borrello S, Waltenberger J, Galeotti T. Reactive oxygen species as downstream mediators of angiogenic signaling by vascular endothelial growth factor receptor-2/KDR. J. Biol. Chem. 2002;277:3101–3108. doi: 10.1074/jbc.M107711200. [DOI] [PubMed] [Google Scholar]
- 135.Sattler M, Winkler T, Verma S, Byrne CH, Shrikhande G, Salgia R, Griffin JD. Hematopoietic growth factors signal through the formation of reactive oxygen species. Blood. 1999;93:2928–2935. [PubMed] [Google Scholar]
- 136.Mahadev K, Wu X, Zilbering A, Zhu L, Lawrence JT, Goldstein BJ. Hydrogen peroxide generated during cellular insulin stimulation is integral to activation of the distal insulin signaling cascade in 3T3-L1 adipocytes. J. Biol. Chem. 2001;276:48662–48669. doi: 10.1074/jbc.M105061200. [DOI] [PubMed] [Google Scholar]
- 137.May JM, de Haen C. Insulin-stimulated intracellular hydrogen peroxide production in rat epididymal fat cells. J. Biol. Chem. 1979;254:2214–2220. [PubMed] [Google Scholar]
- 138.Matsuzawa A, Saegusa K, Noguchi T, Sadamitsu C, Nishitoh H, Nagai S, Koyasu S, Matsumoto K, Takeda K, Ichijo H. ROS-dependent activation of the TRAF6-ASK1-p38 pathway is selectively required for TLR4-mediated innate immunity. Nat. Immunol. 2005;6:587–592. doi: 10.1038/ni1200. [DOI] [PubMed] [Google Scholar]
- 139.Bonizzi G, Piette J, Schoonbroodt S, Greimers R, Havard L, Merville MP, Bours V. Reactive oxygen intermediate-dependent NF-kappaB activation by interleukin-1beta requires 5-lipoxygenase or NADPH oxidase activity. Mol. Cell. Biol. 1999;19:1950–1960. doi: 10.1128/mcb.19.3.1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Los M, Schenk H, Hexel K, Baeuerle PA, Droge W, Schulze-Osthoff K. IL-2 gene expression and NF-kappa B activation through CD28 requires reactive oxygen production by 5-lipoxygenase. EMBO J. 1995;14:3731–3740. doi: 10.1002/j.1460-2075.1995.tb00043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ohba M, Shibanuma M, Kuroki T, Nose K. Production of hydrogen peroxide by transforming growth factor-beta 1 and its involvement in induction of egr-1 in mouse osteoblastic cells. J. Cell Biol. 1994;126:1079–1088. doi: 10.1083/jcb.126.4.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lassegue B, Sorescu D, Szocs K, Yin Q, Akers M, Zhang Y, Grant SL, Lambeth JD, Griendling KK. Novel gp91(phox) homologues in vascular smooth muscle cells: nox1 mediates angiotensin II-induced superoxide formation and redox-sensitive signaling pathways. Circ. Res. 2001;88:888–894. doi: 10.1161/hh0901.090299. [DOI] [PubMed] [Google Scholar]
- 143.Ushio-Fukai M, Alexander RW, Akers M, Yin Q, Fujio Y, Walsh K, Griendling KK. Reactive oxygen species mediate the activation of Akt/protein kinase B by angiotensin II in vascular smooth muscle cells. J. Biol. Chem. 1999;274:22699–22704. doi: 10.1074/jbc.274.32.22699. [DOI] [PubMed] [Google Scholar]
- 144.Zafari AM, Ushio-Fukai M, Akers M, Yin Q, Shah A, Harrison DG, Taylor WR, Griendling KK. Role of NADH/NADPH oxidase-derived H2O2 in angiotensin II-induced vascular hypertrophy. Hypertension. 1998;32:488–495. doi: 10.1161/01.hyp.32.3.488. [DOI] [PubMed] [Google Scholar]
- 145.Chen Q, Olashaw N, Wu J. Participation of reactive oxygen species in the lysophosphatidic acid-stimulated mitogen-activated protein kinase kinase activation pathway. J. Biol. Chem. 1995;270:28499–28502. doi: 10.1074/jbc.270.48.28499. [DOI] [PubMed] [Google Scholar]
- 146.Sekharam M, Cunnick JM, Wu J. Involvement of lipoxygenase in lysophosphatidic acid-stimulated hydrogen peroxide release in human HaCaT keratinocytes. Biochem. J. 2000;346(Pt. 3):751–758. [PMC free article] [PubMed] [Google Scholar]
- 147.Mukhin YV, Garnovskaya MN, Collinsworth G, Grewal JS, Pendergrass D, Nagai T, Pinckney S, Greene EL, Raymond JR. 5-Hydroxytryptamine1A receptor/Gibetagamma stimulates mitogen-activated protein kinase via NAD(P)H oxidase and reactive oxygen species upstream of src in chinese hamster ovary fibroblasts. Biochem. J. 2000;347(Pt. 1):61–67. [PMC free article] [PubMed] [Google Scholar]
- 148.Veal EA, Findlay VJ, Day AM, Bozonet SM, Evans JM, Quinn J, Morgan BA. A 2-Cys peroxiredoxin regulates peroxide-induced oxidation and activation of a stress-activated MAP kinase. Mol. Cell. 2004;15:129–139. doi: 10.1016/j.molcel.2004.06.021. [DOI] [PubMed] [Google Scholar]
- 149.Brennan JP, Bardswell SC, Burgoyne JR, Fuller W, Schroder E, Wait R, Begum S, Kentish JC, Eaton P. Oxidant-induced activation of type I protein kinase A is mediated by RI subunit interprotein disulfide bond formation. J. Biol. Chem. 2006;281:21827–21836. doi: 10.1074/jbc.M603952200. [DOI] [PubMed] [Google Scholar]
- 150.Giannoni E, Buricchi F, Raugei G, Ramponi G, Chiarugi P. Intracellular reactive oxygen species activate Src tyrosine kinase during cell adhesion and anchorage-dependent cell growth. Mol. Cell. Biol. 2005;25:6391–6403. doi: 10.1128/MCB.25.15.6391-6403.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kemble DJ, Sun G. Direct and specific inactivation of protein tyrosine kinases in the Src and FGFR families by reversible cysteine oxidation. Proc. Natl. Acad. Sci. U.S.A. 2009;106:5070–5075. doi: 10.1073/pnas.0806117106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ahn SG, Thiele DJ. Redox regulation of mammalian heat shock factor 1 is essential for Hsp gene activation and protection from stress. Genes Dev. 2003;17:516–528. doi: 10.1101/gad.1044503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Manalo DJ, Lin Z, Liu AY. Redox-dependent regulation of the conformation and function of human heat shock factor 1. Biochemistry. 2002;41:2580–2588. doi: 10.1021/bi0159682. [DOI] [PubMed] [Google Scholar]
- 154.Delaunay A, Pflieger D, Barrault MB, Vinh J, Toledano MB. A thiol peroxidase is an H2O2 receptor and redox-transducer in gene activation. Cell. 2002;111:471–481. doi: 10.1016/s0092-8674(02)01048-6. [DOI] [PubMed] [Google Scholar]
- 155.Fuangthong M, Helmann JD. The OhrR repressor senses organic hydroperoxides by reversible formation of a cysteine-sulfenic acid derivative. Proc. Natl. Acad. Sci. U.S.A. 2002;99:6690–6695. doi: 10.1073/pnas.102483199. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.