Abstract
Although mature enamel is predominantly composed of mineral, a previously uncharacterized organic matrix layer remains in the post-eruptive tissue that begins at the dentin enamel junction and extends 200–300 µm towards the outer tooth surface. Identification of the composition of this layer has been hampered by its insolubility; however, we have developed a single step method to isolate the organic enamel matrix relatively intact. After dissociative dissolution of the matrix with SDS and urea, initial characterization by Western blotting and gel zymography indicates the presence of type IV and type VII basement membrane collagens and active matrix metalloproteinase-20. When combined with data from transgenic knockout mice and from human mutations, these data suggest that the enamel organic matrix (EOM) and dentin enamel junction may have a structural and functional relationship with basement membranes, e.g. skin. To clarify this relationship, we hypothesize a “foundation” model which proposes that components of the EOM form a support structure that stabilizes the crystalline enamel layer, and bonds it to the underlying dentin along the dentin enamel junction. Since we have also co-localized an active matrix metalloproteinase to this layer, our hypothesis suggests that, under pathologic conditions, MMP-mediated degradation of the EOM could destabilize the enamel–dentin interface.
Keywords: Basement membrane, dentin enamel junction, mature human enamel, MMP-20, type IV collagen, type VII collagen
Introduction
The crown of a mature tooth is composed of two unique layers. Enamel, which is highly mineralized and acellular, forms the outer crystalline surface of teeth. Underlying the enamel is a tougher mineralized protein-rich tissue known as dentin. Conjoined dissimilar materials such as rigid enamel and flexible dentin might be expected to concentrate stresses leading to delamination of the surface enamel layer. However, the junction between the two disparate tissues, the dentin enamel junction (DEJ), is known to inhibit crack propagation and rarely undergoes catastrophic mechanical failure, despite a lifetime of masticatory and parafunctional loading (1).
Tooth development, like that for similar embryologically-derived tissues such as skin, is the result of epithelial-mesenchymal inductive signaling that is essential for development of the hard tissue layers. Yet unlike mesenchymal tissues that contain a relatively stable type I collagenous matrix, the initial extracellular matrix which contains highly-ordered crystalline rod-like enamel exists only transiently, largely disappearing as the tissue forms.
Enamel forms through a process of biomineralization where ameloblasts secrete proteins such as enamelin, amelogenin, and ameloblastin that self-assemble to form an extracellular organic matrix that governs the formation of the inorganic phase. Prior to maturation, the majority of the extracellular protein matrix is proteolytically removed (2). The enamel organic matrix (EOM) in the post-eruptive tissue is small (~1% wt), containing proteolyzed fragments and an insoluble protein matrix distributed along the dentinal surface (1). These remaining proteins are believed to toughen the inner enamel region (3), yet they are not regarded as a structural component that stabilizes and bonds the enamel–dentin interface (4). The molecular composition of this EOM layer has remained a mystery for over 50 years (5), hampered by its insolubility and resistance to dissolution (6). The goal of this study was to develop a single step method to isolate this layer and to begin its biochemical characterization.
Materials and methods
Scanning electron microscopy
Healthy human third molars with closed apices and no restorations or caries obtained via an IRB-approved protocol were processed for scanning electron microscopy (SEM) and were observed at low voltage (1 kV) on non-coated specimens as described in detail previously (4).
Preparation of the enamel organic matrix
Individual whole third molar crowns, from different patients, were suspended in 0.5 M EDTA, pH 7.4. After 7 d, the residual EOM layer was physically removed with a brush. Subsequent to dialysis and lyophilization, the precipitate was then dissociated in SDS/8M urea sample buffer, heated at 95 °C, and subjected to gel electrophoresis (7) and Western blotting.
SDS PAGE, Western blotting, and gel zymography
Isolated EOM was solubilized with SDS PAGE sample buffer and subjected to Western blotting on 7.5% or 4–20% gradient gels (8). After transfer to PVDF membranes, the blots were developed with rabbit polyspecific antibodies against the α2 chain of type IV collagen (T-15, 1:500, Santa Cruz Biotechnology, Santa Cruz, CA) or the helical domain of α1(IV) and α2(IV) chains (M3F7, 1:500, Developmental Studies Hybridoma Bank, University of Iowa, IA). Type VII collagen antibodies used were from Millipore (Billerica, MA) (1:500, #234192) and from Sigma-Aldrich (St. Louis, MO) (1:500, clone LH7.2). For comparison, whole crowns (minus roots) were pulverized and extracted with 4 M guanidine HCl and 0.5 M EDTA containing protease inhibitors (9); the lyophilized extract was solubilized with SDS PAGE sample buffer and subjected to Western blotting with rabbit anti-MMP-20 antibodies specific to the N-terminal domain (1:2000, Sigma-Aldrich, #M-5934) and C-terminal domain (1:200, Origene, Rockville, MD, clone EP1275Y), and to casein gel zymography (10). Casein gels were visualized after staining with Coomassie brilliant blue dye.
Results
Enamel organic matrix in mature teeth
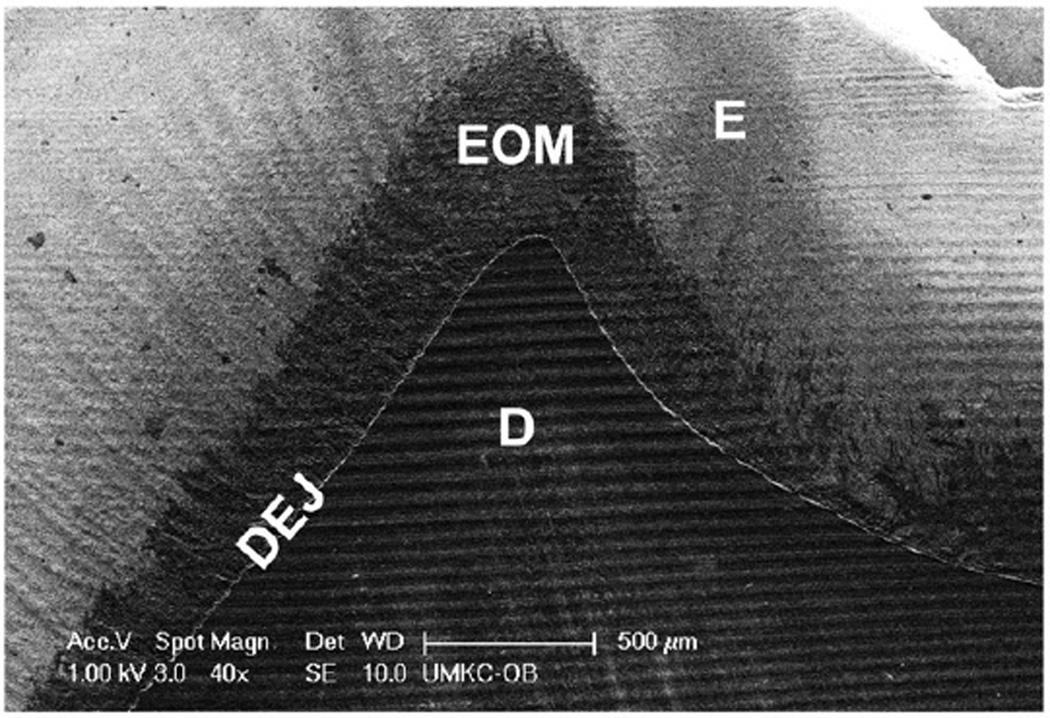
As shown in the scanning electron microscopic image in Figure 1, mature third molar teeth contain an organic matrix layer within the enamel layer. This layer begins at the DEJ and extends 200–300 µm towards the outer tooth surface (dark area, Figure 1). As illustrated with this tooth, we routinely observe a thicker matrix layer under the cuspal regions. We have previously shown that this layer also demonstrates a Raman spectral signature consistent with its protein content (4). Based on its location adjacent to the dentin enamel junction within the mineralized phase of mature teeth, we devised a single-step procedure to physically isolate the EOM layer as a particulate residue after demineralization. The dentin layer was visually unaffected by this treatment (Figure 1), however, minor contamination with dentin-derived proteins in the EOM fraction cannot be excluded at this time.
Figure 1.
The enamel organic matrix within the inner enamel layer of mature teeth. An SEM image of the cuspal region of a maxillary third molar demonstrates that the enamel organic matrix is congruent with the dentin at the dentin enamel junction, and extends 200–300 µm towards the outer tooth surface. Notably, the organic matrix is thicker in the cuspal/occlusal regions. Scale bar: 500 µm. Key: E, enamel; EOM, enamel organic matrix; D, dentin.
Initial biochemical characterization of the enamel organic matrix layer
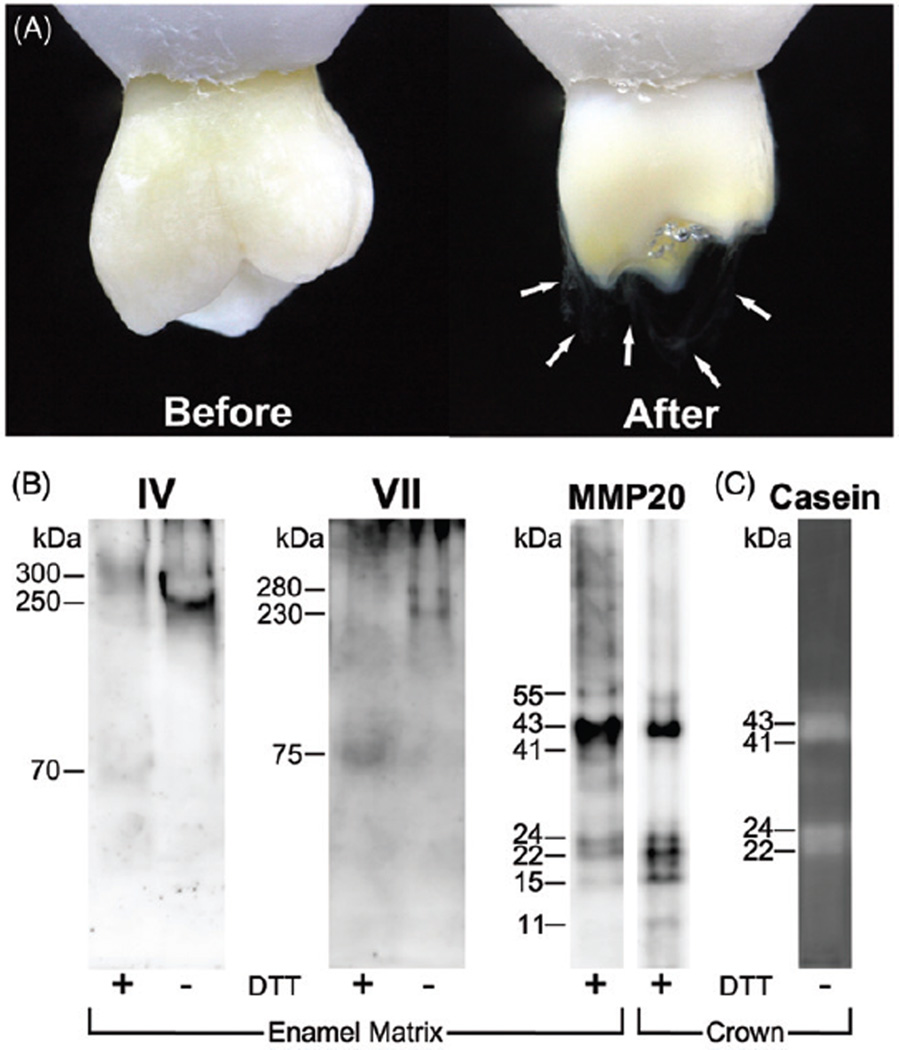
The EOM layer was isolated from whole tooth crowns (Figure 2A). The particulate nature of the enamel matrix is evident as wispy white protein strands (arrows, Figure 2A). After solubilization, the enamel matrix fraction was processed for Western blotting using a series of antibodies against extracellular matrix proteins. Candidate targets were provided by separate mass spectral analyses on gel slices (not shown). As shown in Figure 2(B), the EOM layer contained positive immunoreactivity for type IV collagen, type VII collagen, and MMP-20 which was confirmed in each case with at least two separate antibodies (not shown). Specifically, type IV collagen was present as a prominent single 250 kDa band under non-reducing conditions which shifted to an apparent 300 and 70 kDa bands when reduced. Also, type VII immunoblots revealed doublet bands of 230 and 280 kDa which resolved into a 75 kDa band upon reduction. Finally, immunostaining for MMP-20 identified characteristic bands of 43, 24, 22, and 15 kDa under reducing conditions (Figure 2B). As demonstrated by casein gel zymography in Figure 2(C) under non-reducing conditions, broad bands at 43–41 kDa and at 24–22 kDa represent catalytically active MMP-20. While the zymographic results depicted were from a total crown extract (Figure 2C), similar results are expected for the EOM fraction given their identical blotting patterns (Figure 2B). For reference, inactive proMMP-20 (Mr = 55 kDa) is activated upon cleavage to a 43–41 kDa form, while the 24–22 kDa forms are well-known active fragments. As expected, these MMP-20 bands were dependent upon the presence of exogenous calcium ion, yet did not cleave gelatin in parallel studies (not shown). Taken together, our results show that the EOM contains at least two different macromolecular basement membrane collagen types and a catalytically active metalloproteinase.
Figure 2.
(A) Enamel organic matrix resides in the inner region of enamel following complete demineralization. Before and after images of a whole maxillary third molar crown demineralized for 1 week as described in METHODS section. Following complete demineralization of enamel, the residual particulate organic matrix is seen along the dentin, predominantly in the cuspal regions (white arrowheads). The amount of residual organic matrix can be appreciated as it suspends from the dentinal surface. (B) Immunoblotting of enamel matrix fraction and an extract of whole tooth crown demonstrate the presence of type IV and VII collagen and MMP-20. Protein extracts exclusively from enamel and from a whole tooth crown were electrophoresed as described in METHODS section using 7.5% gels (type IV and type VII collagen) and a 4–20% linear gradient gel (MMP-20), respectively. For type IV collagen, the non-reduced sample displayed higher molecular weights with mobilities of 300 and 250 kDa, which shifted to a 300 kDa monomer and a 70 kDa fragment after reduction with DTT. Similarly, for type VII collagen, the non-reduced sample presented as a 280 and 250 kDa dimer, which shifted to a 75 kDa fragment after reduction. For MMP-20, 5–6 bands were detected at 55, 43–41, 24, 22 and 15–11 kDa. These bands correspond in size to the pro-form (55 kDa), activated forms (43 and 41 kDa), and fragments (24, 22, and 15–11 kDa) of MMP-20. Molecular weight estimates are based on standards co-electrophoresed on the same gel. Twenty and thirty micrograms of enamel matrix and crown extract protein were applied to these lanes, respectively. (C) Casein gel zymography demonstrates catalytically active MMP-20 bands are present in a human tooth crown extract. Thirty micrograms of protein were applied.
Discussion
Basement membrane degradation and removal is unique to teeth
Basement membranes are regarded as thin, sheet-like layers of specialized extracellular matrix that form scaffolds and flexible boundaries between differing tissues. The major shared components of all basement membranes are type IV collagen, laminin, nidogen, heparin sulfate proteoglycans, and type VII collagen (11). Although basement membranes are ubiquitous throughout many tissue compartments, their macromolecular structure, composition, and functions differ and are tissue specific, e.g. kidney versus skin. Their complexity has become more evident within the past several years as more components have been characterized (12). However, a common feature of basement membranes is their functional role in linking or bonding different tissue layers. This stabilizing action is evident in the skin blistering which develops when inactivating mutations in type IV or type VII collagen permit epithelial layer separation and movement when stress is applied. In developing tooth germs, the dental basement membrane mediates interactions between the opposing epithelium and ectomesenchyme (13).
As the tissue forming cells of enamel (ameloblasts) and dentin (odontoblasts) differentiate along the epithelial-mesenchymal junction, they secrete their respective matrices. However, as this secretory activity initiates, the dental basement membrane is degraded and removed, allowing direct contact between the underlying odontoblasts and ameloblasts. By the time mineralization of enamel and dentin begins, the dental basement membrane is believed to be removed (14), replaced with an interdigitated calcified interface.
Removal of the basement membrane in teeth is unique among other tissues and appears to coincide with matrix and/or mineral deposition along the developing DEJ. Brought to its logical conclusion, we speculate that mineralization of the developing DEJ could bury residual macromolecular basement membrane proteins, e.g. type IV and type VII collagen, resulting in their reported disappearance during odontogenesis.
Enamel organic matrix at the DEJ contains basement membrane components
Prior evidence supports functional roles for type IV collagen in DEJ development (14), and for type VII collagen in amelogenesis (15) during tooth development in mice. Specifically, murine ameloblasts express type VII collagen mRNA and type VII collagen null mice display an abnormal enamel rod orientation with an abnormal network arrangement. These abnormal rods were caused by type VII collagen deficiency because these changes were completely rescued by restoration of expression (15). Type VII collagen deficiency also leads to a general reduction in enamel protein expression by ameloblasts (15). In contrast, no genetic defects of α1(IV) or α2(IV) genes have yet been linked to tooth malformation because these mutations are embryonically lethal (16). However, degradation by matrix metalloproteinases-2, -9 (Type IV collagenases) and -20 (MMP-20) and kallikrein-related peptidase-4 (KLK-4) proteases prior to and during the maturation stage has been shown to degrade the basement membrane and enamel matrix proteins (17). Yet, a question remains. If the dental basement membrane is degraded and removed during development, how could macromolecular constituents of this membrane remain in mature enamel matrix at the DEJ? We speculate that inter- and intra-molecular chemical cross-links within type IV and type VII collagen could protect them during matrix degradation and facilitate their selective retention.
Though previous investigations have demonstrated that the dental basement membrane during development is composed in part of type IV and type VII collagen, it should be noted that these studies have been limited to developing tooth germs (14,15). To our knowledge, our study is the first to investigate if these constituents are present in mature teeth. Since the DEJ forms at the site of the dental basement membrane, we believe that components of this membrane are selectively retained and comprise a portion of the protein composition of the DEJ and EOM observed with Raman spectroscopy and SEM (4).
Developmental, compositional, and functional parallels between teeth and skin
Teeth are rarely, if ever, compared to skin. Despite the obvious differences, several developmental, functional, and compositional parallels exist between the two. First, the outer protective layers of these organs, enamel and epidermis, are ectodermally derived, whereas their inner supportive layers, dentin and dermis, are of mesodermal origin (3,12). Second, development of both teeth and skin requires epithelial–mesenchymal cross-talk signaling (3,12). Third, the integrity of both organs is maintained by attachment to an intervening interfacial layer known as the dentin–enamel and dermal–epidermal junction in teeth and skin, respectively. Fourth, both teeth and skin are mechanically stable and uniquely adapted to function in their environments (3,11), rarely separating into their respective layers under normal applied and functional stresses, e.g. occlusal loading of teeth during mastication and plantar loads generated on skin during running.
Compositional similarities also exist between teeth and skin. For example, type I collagen is a major fibrillar constituent of the dermis and dentin, connecting them to their overlying layers (1,11). In addition, type IV and type VII collagen, which are critical for dermal-epidermal integrity via their association with type I collagen (11), have been transiently localized to the dental basement membrane (14,15).
Based on these parallels, we envision that the dermal–epidermal junction in skin and the DEJ in mature teeth exhibit additional previously unappreciated compositional similarities, e.g. enriched content of type IV and type VII collagen. Furthermore, we hypothesize that type IV and type VII collagen found in this study within the EOM play a previously unappreciated role in the damage tolerance and fracture resistance of the DEJ.
A model of the structural role of the enamel organic matrix at the DEJ
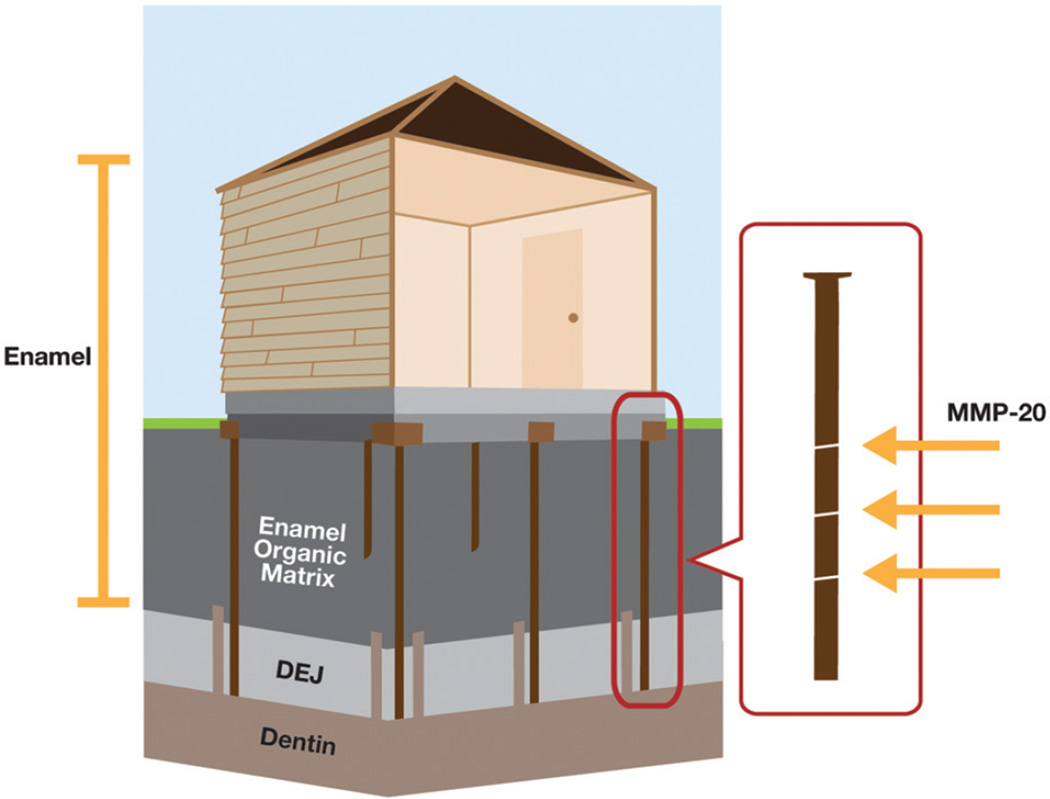
Based on prior biomaterial studies, we propose that inner enamel’s inorganic–organic hybrid structure close to the DEJ is a determinant of its material properties (Figure 3). Specifically, when fracture toughness and crack growth were measured, the inner enamel closer to the DEJ was found to be tougher and to resist crack propagation more than outer enamel (18,19). A positive contribution by the EOM was shown by a reduction in fracture toughness after its removal or alteration (20,21). Finally, enamel exhibits about a three times greater fracture toughness than geologic hydroxyapatite (without an organic matrix), however, White et al. (2) ascribe this finding to the inclusion of biological contaminants in the former. Consistent with a stabilizing role, the EOM is more prevalent in cuspal enamel which is subjected to more compressive and shearing stresses, as compared to the cervical region which is primarily exposed to flexural stresses. We envision enamel as a compositional composite in which the outer highly mineralized layer is designed to withstand occlusal stress and wear, and an inner layer, which is toughened by the EOM. The ~5 µm wide optical DEJ links the enamel and dentin layers.
Figure 3.
Hypothetical DEJ interface “foundation” model. This simplistic model includes the enamel and dentin matrix components that may contribute to the structural integrity of the dentin enamel interface. We hypothesize that degradation of the collagenous complex of the enamel organic matrix due to the proteolytic activity of MMP-20 and/or other proteases under pathologic conditions could be linked to DEJ instability and lead to enamel separation from the dentin.
In summary, our “DEJ-enamel matrix model” (Figure 3) proposes that, in addition to inorganic–inorganic interactions between enamel and dentin across the DEJ and previously reported type I collagen fibers crossing from dentin into enamel (1), there are also interactions between protein components of the EOM and the dentin matrix across the DEJ. Our model proposes that both organic and inorganic interaction(s) between components contributes to the stability of the dentin enamel interface. Additionally, we hypothesize that the EOM functions to reduce occlusal stress concentrations from enamel to dentin. As such, this model contradicts the current view that enamel protein retained in the post-eruptive tissue represents proteolyzed fragments of the original matrix with little or no functional importance.
Pathologic delamination of enamel from dentin is a rare occurrence under normal conditions. However, oral cancer patients treated with high dose radiation develop a distinct pattern of dentition breakdown, which initiates with shear fracturing of enamel that can result in partial to total enamel delamination (22). When viewed in terms of the “DEJ-enamel matrix model”, we hypothesize that the delamination process may be due to destabilization of the DEJ-enamel matrix interface arising from direct or indirect radiation damage. In this regard, co-localization of active MMP-20 in the EOM causes us to speculate that proteolytic degradation of this type IV and type VII collagen containing matrix may be part of the underlying causative mechanism (Figure 3). In support of this hypothesis, radiotherapy has been shown to cause up-regulation and activation of specific MMPs in the lung, brain, and colon (22).
Acknowledgments
The authors wish to thank Ms. Rachel Reed for her excellent technical assistance and Carla Preuss for artwork.
Declaration of interest
This project was supported by NIH/NIDCR grants R01-DE021462 and F32-DE022984.
References
- 1.Paine M, White S, Luo W, Fong H, Sarikaya M, Snead M. Regulated gene expression dictates enamel structure and tooth function. Matrix Biol. 2001;20:273–292. doi: 10.1016/s0945-053x(01)00153-6. [DOI] [PubMed] [Google Scholar]
- 2.White SN, Luo W, Paine MP, Sarikaya M, Snead ML. Biological organization of hydroxyapatite crystallites into a fibrous continuum toughens and controls anisotropy in human enamel. J Dent Res. 2001;80:321–326. doi: 10.1177/00220345010800010501. [DOI] [PubMed] [Google Scholar]
- 3.White SN, Paine MP, Luo W, Sarikaya M, Fong H, Yu Z, Li ZC, Snead ML. The dentino-enamel junction is a broad transitional zone uniting dissimilar bioceramic composites. J Am Ceram Soc. 2000;83:238–240. [Google Scholar]
- 4.Dusevich V, Xu C, Wang Y, Walker M, Gorski J. Identification of a protein-containing enamel matrix layer which bridges with the dentine-enamel junction of adult human teeth. Arch Oral Biol. 2012;57:1585–1594. doi: 10.1016/j.archoralbio.2012.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eastoe J. Organic matrix of tooth enamel. Nature. 1960;197:411–412. doi: 10.1038/187411b0. [DOI] [PubMed] [Google Scholar]
- 6.Robinson C, Hudson J. Tuft protein: protein cross-linking in enamel development. Eur J Oral Sci. 2011;119:50–54. doi: 10.1111/j.1600-0722.2011.00906.x. [DOI] [PubMed] [Google Scholar]
- 7.Laemmli UK. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nat Biotechnol. 1970;15:680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- 8.Gorski JP, Huffman NT, Chittur S, Midura RJ, Black C, Oxford J, Seidah NG. Inhibition of proprotein convertase SKI-1 blocks transcription of key extracellular matrix genes regulating osteoblastic mineralization. J Biol Chem. 2011;286:1836–1849. doi: 10.1074/jbc.M110.151647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gorski JP, Krember EA, Chen Y, Ryan S, Fullenkamp C, Delviscio J, Jensen K, McKee MD. Bone acidic glycoprotein-75 self-associates to form macromolecular complexes in vitro and in vivo with the potential to sequester phosphate ions. J Cell Biochem. 1997;64:547–564. [PubMed] [Google Scholar]
- 10.Kremer EA, Chen Y, Suzuki K, Nagase H, Gorski JP. Hydroxyapatite induces autolytic degradation and inactivation of matrix metalloproteinase-1 and -3. J Bone Miner Res. 1998;13:1890–1902. doi: 10.1359/jbmr.1998.13.12.1890. [DOI] [PubMed] [Google Scholar]
- 11.Timpl R. Structure and biological activity of basement membrane proteins. Eur J Biochem. 1989;180:487–502. doi: 10.1111/j.1432-1033.1989.tb14673.x. [DOI] [PubMed] [Google Scholar]
- 12.Erickson AC, Couchman JR. Still more complexity in mammalian basement membranes. J Histochem Cytochem. 2000;48:1291–1306. doi: 10.1177/002215540004801001. [DOI] [PubMed] [Google Scholar]
- 13.Kollar EJ. Epithelial-mesenchymal interactions in the mammalian integument: tooth development as a model for instructive induction. In: Fallon JF, Sawyer RH, editors. Epithelial-mesenchymal interactions in development. New York (NY): Praeger Press; 1983. pp. 27–49. [Google Scholar]
- 14.Nagai N, Nakano K, Sado Y, Naito I, Gunduz M, Tsujigiwa H, Nagatsuka H, Ninomiya Y, Siar CH. Localization of type IV collagen alpha 1 to alpha 6 chains in basement membrane during mouse molar germ development. Int J Dev Biol. 2001;45:827–831. [PubMed] [Google Scholar]
- 15.Umemoto H, Akiyama M, Domon T, Nomura T, Shinkuma S, Ito K, Asaka T, Sawamura D, Uitto J, Uo M, Kitagawa Y, Shimizu H. Type VII collagen deficiency causes defective tooth enamel formation due to poor differentiation of ameloblasts. Am J Pathol. 2012;181:1659–1671. doi: 10.1016/j.ajpath.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 16.Poschl E, Sclotzer-Schrehart U, Brachvogel B, Saito K, Ninomiya Y, Mayer U. Collagen IV is essential for basement membrane stability but dispensable for initiation of its assembly during early development. Development. 2004;131:1619–1628. doi: 10.1242/dev.01037. [DOI] [PubMed] [Google Scholar]
- 17.Simmer J, Hu J-C. Dental enamel formation and its impact on clinical dentistry. J Dent Educ. 2001;65:896–905. [PubMed] [Google Scholar]
- 18.Bajaj D, Arola DD. On the R-curve behavior of human tooth enamel. Biomaterials. 2009;30:4037–4046. doi: 10.1016/j.biomaterials.2009.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zheng Q, Xu H, Song F, Zhang L, Zhou X, Shao Y, Huang D. Spatial distribution of the human enamel fracture toughness with aging. J Mech Behav Biomed Mater. 2013;26:148–154. doi: 10.1016/j.jmbbm.2013.04.025. [DOI] [PubMed] [Google Scholar]
- 20.Baldassarri M, Margolis HC, Beniash E. Compositional determinants of mechanical properties of enamel. J Dent Res. 2008;87:645–649. doi: 10.1177/154405910808700711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seghi RR, Denry J. Effects of external bleaching on indentation and abrasion characteristics of human enamel in vitro. J Dent Res. 1992;71:1340–1344. doi: 10.1177/00220345920710061201. [DOI] [PubMed] [Google Scholar]
- 22.Walker MP, Wichman B, Cheng A-L, Coster J, Williams KB. Impact of radiotherapy dose on dentition breakdown in head and neck cancer patients. Pract Radiat Oncol. 2011;1:142–148. doi: 10.1016/j.prro.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]