Abstract
Context:
Blood pressure (BP) is routinely measured in children and adolescents during primary care visits. However, elevated BP or hypertension is frequently not diagnosed or evaluated further by primary care providers. Barriers to recognition include lack of clinician buy-in, competing priorities, and complexity of the standard BP tables.
Case Description:
We have developed and piloted TeenBP— a web-based, electronic health record (EHR) linked system designed to improve recognition of prehypertension and hypertension in adolescents during primary care visits.
Major Themes:
Important steps in developing TeenBP included the following: review of national BP guidelines, consideration of clinic workflow, engagement of clinical leaders, and evaluation of the impact on clinical sites. Use of a web-based platform has facilitated updates to the TeenBP algorithm and to the message content. In addition, the web-based platform has allowed for development of a sophisticated display of patient-specific information at the point of care. In the TeenBP pilot, conducted at a single pediatric and family practice site with six clinicians, over a five-month period, more than half of BPs in the hypertensive range were clinically recognized. Furthermore, in this small pilot the TeenBP clinical decision support (CDS) was accepted by providers and clinical staff. Effectiveness of the TeenBP CDS will be determined in a two-year cluster-randomized clinical trial, currently underway at 20 primary care sites.
Conclusion:
Use of technology to extract and display clinically relevant data stored within the EHR may be a useful tool for improving recognition of adolescent hypertension during busy primary care visits. In the future, the methods developed specifically for TeenBP are likely to be translatable to a wide range of acute and chronic issues affecting children and adolescents.
Keywords: Health Information Technology, Research Translation, Evidence Based Medicine
Introduction
Hypertension (HTN) during adolescence, although generally asymptomatic, is associated with both short- and long-term adverse health effects. Adolescent HTN increases risk for adult HTN and for long-term cardiovascular morbidity and mortality.1–3 Definitions for HTN in children and adolescents were developed by the National High Blood Pressure Education Program (NHBPEP), and were then reiterated in the 2011 Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents (Integrated Guidelines).4,5 In both consensus guidelines, HTN is defined on the basis of blood pressure (BP) percentile. Both guidelines recommend that a single BP ≥95th percentile is repeated, and then the BP percentile for the average of two or more measurements at one visit is determined with the use of standardized tables—based on sex, age, and height percentile. HTN is defined as having systolic and/or diastolic BPs on at least three different visits that are ≥ 95th percentile. It has been estimated that between 1–5 percent of children and adolescents meet this clinical definition for HTN.6,7 The NHBPEP and Integrated Guidelines provide additional recommendations regarding the management of prehypertension (BP between the 90th and 95th percentile) and HTN.
Unfortunately, among otherwise healthy children and adolescents, prehypertension and HTN are usually not recognized.6,8 In an electronic database review of more than 500 children and adolescents who met clinical criteria for HTN, only 26 percent were diagnosed.6 Similarly, in a manual chart review of more than 700 pediatric, primary care visits in which an elevated BP was recorded, only 13 percent were clinically recognized, either diagnosed or acknowledged through additional clinical actions related to the elevated BP.8 In a Dutch study of pediatricians, nearly half of providers surveyed did not recognize one or more prehypertensive or hypertensive BPs.9 Although both the NHBPEP and Integrated Guidelines recommend that a BP in the stage 1 hypertensive range be repeated within 1–2 weeks, in a multisite observational study of pediatric HTN, only 21 percent of hypertensive BPs were repeated within a month, and the median time for a repeat BP was nearly five months.10
Low rates of recognition and failure to follow up on prehypertension or HTN are likely due to multiple factors. First, many clinicians may not be familiar with the criteria needed to diagnose HTN or they may be unaware of recommended intervals for follow-up visits to remeasure an initial hypertensive BP. Second, because the need for routine BP screening during adolescence has not been uniformly endorsed,11,12 clinician buy-in of the consensus guidelines may be low. Third—and probably most critical—as described above, the classification of HTN is too complex to be easily and accurately implemented in routine clinical practice.8 Briefly, in order to determine if a systolic or diastolic BP is elevated, a measurement (e.g., 127/75 mmHG) must be converted to systolic and diastolic BP percentiles. BP percentiles and thresholds for defining elevated BP are not intuitive; they vary based on a patient’s sex, age, and height percentile. Stage 1 HTN is defined as having three or more BPs at or above the 95th percentile but <99th percentile +5 mmHG. Stage 2 HTN is defined as having three or more BPs at or above the 99th percentile + 5 mmHG.
Time pressures reported by clinicians in providing comprehensive care for adolescents,13,14 complexities of classifying BP percentiles, and the need to review several previous BP measurements to diagnose HTN all clearly contribute to underrecognition. In their 2010 article on predictors of unrecognized elevated BP in children, Brady et al. concluded, “To improve recognition and, ultimately, to increase early diagnosis and treatment of children with HTN, it is imperative that systems such as computerized alerts be put into place.”8 To date, many available electronic health records (EHRs) have the ability to calculate BP percentiles and to alert providers based on a cutoff for a single BP measurement. However, we are not aware of tools within existing EHRs that provide the more complex clinical decision support (CDS) needed to diagnose and treat pediatric and adolescent HTN including the following:
Calculating BP percentiles for an average of two or more BPs;
Reviewing prior BPs in order to identify cases meeting clinical criteria for HTN;
Reviewing prior diagnoses to distinguish prevalent from incident HTN; and
Reviewing each patient’s medications, body mass index (BMI), and comorbidities to understand factors that may be contributing to an observed BP elevation.
In this case study, we describe the development and piloting of an EHR-linked, web-based CDS system, “TeenBP,” designed to improve the quality of care delivered to children and adolescents within a large health system.
Methods
Overview
The work presented represents the developmental and pilot phase of a larger-cluster, randomized controlled trial (ClinicalTrials.gov registry number identifier: NCT01760239). This project has been approved by the HealthPartners Institutional Review Board. All providers and staff surveyed provided written informed consent.
Setting
HealthPartners (HP) is a consumer-governed, nonprofit health care organization in Minnesota. HealthPartners Medical Group (HPMG) includes 21 primary care clinics, 15 urgent care clinics, and more than 30 specialty clinics, with 780 physicians. The TeenBP CDS was piloted in a single HealthPartners community-based, primary care clinic located in the southern metropolitan region of Minneapolis–Saint Paul, with approximately 1,400 visits annually among 10–17 year olds. Pediatric patients at the pilot clinic are cared for by three family physicians, one family nurse practitioner, one physician assistant, and one pediatrician.
Obtaining Buy-In from Clinical and Operational Leaders
Input and support from HPMG clinical and operational leaders was critical in the development and implementation of TeenBP. At the start of the project we convened a clinical advisory board that included the Associate Medical Director of Primary Care; department heads in Pediatrics and Family Medicine; and leaders in Nursing, Nutrition, and Information Systems and Technology. We also consulted with several authors of the NHBPEP guidelines. Our advisory board, including experts in pediatric hypertension, reviewed our full algorithm and provided input regarding the clinical recommendations, with an eye to maintaining clinic workflow, minimizing the burden on clinic staff, patients, and patient families, and ensuring patient safety.
Design of Decision Support Tool
The goals of the TeenBP CDS were to improve clinician recognition of elevated BPs and incident HTN—integrating all relevant clinical data within the EHR to provide tailored, patient-specific recommendations—while adhering to national guidelines. Key elements of TeenBP development were the following:
Incorporating CDS based on the NHBPEP and Integrated Guidelines within the existing clinic workflow;
Assessing technologic feasibility of a practical CDS system;
Obtaining buy-in from HPMG clinical and operational leaders;
Translating guidelines into feasible, actionable steps;
Piloting and refining the timing of alerts and nurse- and provider messaging within the TeenBP system; and
Obtaining feedback from staff at the pilot site.
Further description of each of these steps follows.
Providing CDS Based on Consensus Guidelines Within Existing Clinic Workflows
Our first task in the development of TeenBP was to assess how best to incorporate the NHBPEP and Integrated Guidelines within the existing clinic workflow. In the HPMG medical group, vital signs, height, and weight are measured by rooming staff (licensed practical nurses and certified medical assistants) as part of standard rooming procedures, before providers begin their evaluation. BP is measured at all preventive visits and at the discretion of the rooming staff at other types of visits. The NHBPEP guidelines recommend that children three years old and older have their BP measured at least once during every clinical encounter, while the Integrated Guidelines recommend that children and adolescents have their BP measured at least once each year. In a recent survey of pediatric- and family-medicine rooming staff across the HealthPartners health system, nearly all reported checking BP at well-child visits, 75 percent stated they measure BP routinely at sick or acute care visits, and half reported routinely measuring BP at follow-up visits. With this data in mind and in order to not increase demands on rooming staff, our first decision was to initiate the TeenBP CDS only after a BP is entered into the EHR (Figure 1). TeenBP is not activated during visits where the BP is not recorded.
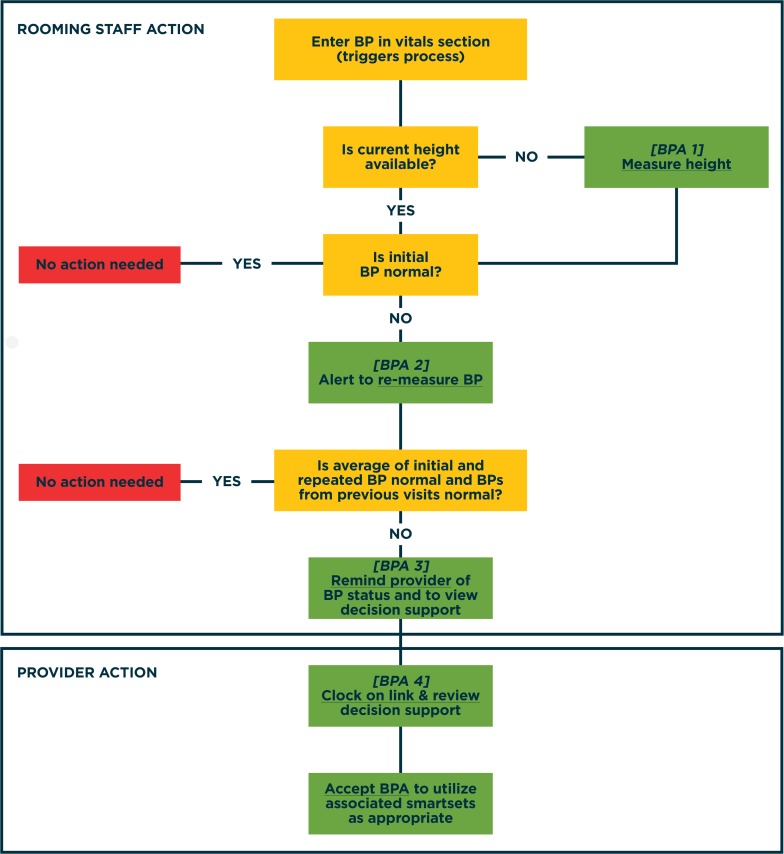
Figure 1.
Overview of TeenBP CDS, Best Practice Advisories (BPAs), Rooming Staff and Provider actions
In order to calculate a BP percentile in a child or adolescent, a height percentile is needed. The current clinic process is for height to be recorded at least once per year. Even during growth spurts, children and adolescents tend to maintain their height percentile. Therefore, consistent with the workflow of the medical group, we allow TeenBP to utilize a height percentile recorded up to 12 months earlier to classify the BP percentile. If there is no height recorded within 12 months, the first alert from TeenBP following entry of a BP in the EHR requests that rooming staff measure a height (Figure 1, BPA 1).
The NHBPEP and Integrated Guidelines recommend that any elevated BP be repeated twice and that final classification is based on the average of three BP measurements. The standard across our health system is for rooming staff to repeat an elevated BP after five minutes. In a recent survey of pediatric and family medicine rooming staff across the health system, a majority reported relying on “clinical judgment” and an EHR-based alert to determine whether a BP is elevated and should be repeated. It is clear that many BPs ≥95th percentile on initial measurement will not be elevated when repeated. In order to reduce the impact of the TeenBP CDS on clinic workflow and minimize alert fatigue, we recommend that an elevated BP be repeated once and that BP percentile then be assigned based on the average of the initial and repeat measurement. We do not provide additional decision support at a visit where an elevated BP is not remeasured.
Both the NHBPEP and Integrated Guidelines recommend that in an otherwise healthy child or adolescent, if the average BP from a single clinical encounter is in the Stage 1 hypertension range or ≥95th percentile but <99th percentile + 5mmHG, the BP should be remeasured in 1–2 weeks. Given busy family and provider schedules, in TeenBP we advise that an elevated BP be remeasured in 1–3 weeks. We recommend that BPs in the Stage 2 hypertension range, 99th percentile + 5mmHG, be repeated in 5–7 days.
Assessing Technologic Feasibility of an Ideal CDS
The TeenBP CDS system needed to be able to do the following:
Deliver advice at specific points of EHR activity during the patient encounter;
Tailor the CDS information to a particular clinical scenario;
Limit the number of calls from the EHR to the Web service for extracting and processing data;
Provide many patient-specific order sets; and
Allow the provider an opportunity to view the full web-based CDS display with patient-specific content.
As the CDS algorithms are external to the EHR, in a web-based system, updates are simplified. Furthermore, in the future, this web-based CDS could be integrated with EHRs in other health care systems.
Four Best Practice Advisories (BPAs) are used to trigger the CDS process and to deliver guidance. The first two of these BPAs are described above: requesting that a height be measured (if needed), and requesting that an elevated BP be remeasured. When an elevated BP is repeated by the rooming staff, the third BPA notifies the rooming staff either that the average of the initial and repeat is normal and no further action is needed or that the BP remains elevated and requests that the provider is notified. The fourth and final BPA occurs when the average of the initial and repeat BP is elevated. This BPA is triggered when the provider opens the patient’s record in the EHR and alerts the provider that the BP is elevated. This fourth BPA provides links to the full CDS and tailored SmartSets or patient specific sets of orders. (Figures 2 and 3).
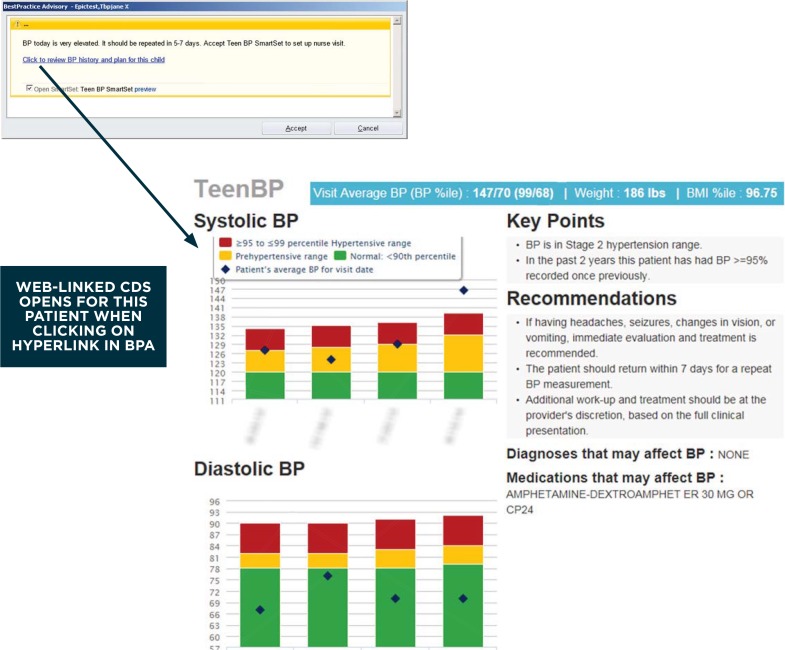
Figure 2.
Example of Provider Alert and Link to Full TeenBP CDS
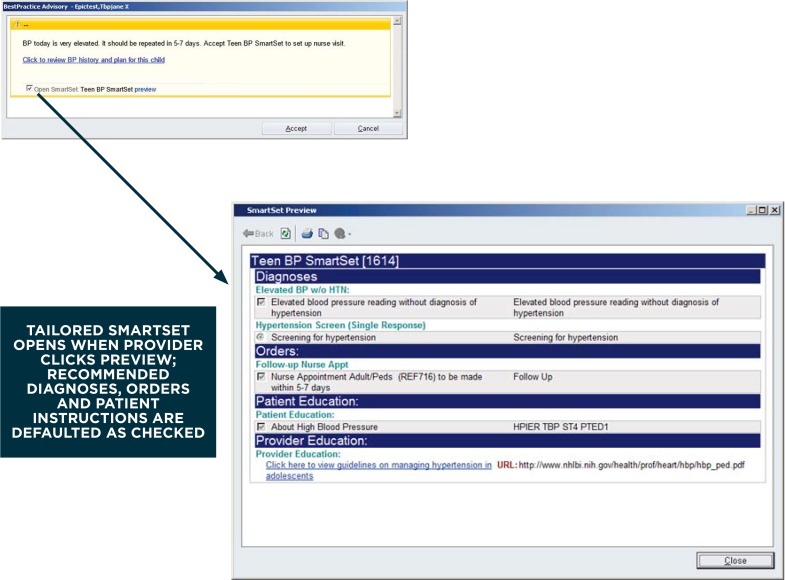
Figure 3.
Example of Provider Alert and Link to SmartSet
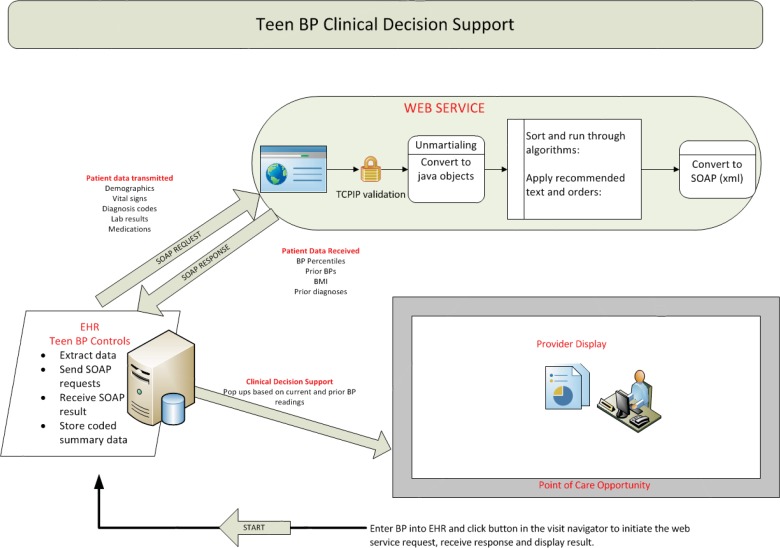
The determination of “elevated BP” is made outside of the EHR in the Web service. When the first BP is measured, the patient’s current BP, age, height, and sex are extracted by EHR routines and sent to the Web service using the Simple Object Access Protocol (SOAP). The Web service calculates systolic and diastolic BP percentiles using the algorithm from the Fourth Report.4 If either systolic or diastolic BP is ≥95th percentile, the Web service guides the display of the BPA to remeasure BP. If the nurse does remeasure the BP, a second call is made, and the Web service determines if the CDS is required and triggers the display of the fourth BPA and any required SmartSets. Additional data elements exchanged between the EHR and Web service include weight, prior heights, prior BPs, current medications, diagnosis codes, and lab values.
A provider flowsheet-data structure is used to store response data from the Web service, and this data can then be integrated into the patient record. This flowsheet data is then used to populate text within each BPA: as triggering criteria, to dynamically define SmartSet content (more than 250 possible order combinations), and to present the physician with a website link to the full CDS display. Examples of these SmartSet combinations are provided below and in Figure 3. A diagram displaying the flow of data and communication between the EHR and Web service is shown in Figure 4.
Figure 4.
Flow of Data between Electronic Health Record (EHR) and Web Service
Translating Guidelines into Feasible, Actionable Steps
After adapting the TeenBP decision support to be consistent with clinic workflow, reviewing technical issues, and obtaining support from institutional leaders, the next step was to translate recommendations into actionable steps. Figure 1 provides an overview of these steps, highlighting actions for rooming staff and those for the provider.
In patients for whom the average of at least two BP measurements is elevated, the provider CDS includes two key features. First, we integrate all relevant clinical information in a web-based display (Figure 2). This Web display graphs the systolic and diastolic BP for that day’s visit, along with all BPs recorded at primary care visits in the past two years. The graph is color coded such that BPs in the green zone are not elevated, those in yellow are in the prehypertensive range, and those in red or above are in the hypertensive range. When viewed as a Web link, scrolling over each bar in the graph displays the exact BP cutoffs for each BP category. The provider web-based CDS also provides a summary of the patient’s BP status at the current visit and any medications (e.g., stimulants, steroids, or antihypertensives) or comorbidities (e.g., cardiac, renal, or endocrine disorders) that may affect BP, and then offers tailored clinical recommendations. The patient’s weight and BMI percentile at the current visit are also displayed in the blue bar. Additional CDS is targeted to patients with prior hypertension diagnoses. Although the CDS is designed for use by providers, to be viewed during a clinical encounter, it can be printed and used as part of a patient handout.
The second key part of the TeenBP provider CDS is a set of patient-specific orders or a SmartSet based on available data within the EHR (Table 1). SmartSets were created with tailored diagnoses and recommendations. The SmartSets include diagnoses (HTN or elevated BP without hypertension), recommendations for the timing of follow-up visits and referrals, or laboratory testing (cholesterol screening). For example, for patients with BP in the Stage 2 HTN range and fewer than two prior elevated BPs, the tailored SmartSet will recommend a diagnosis of “elevated blood pressure” and a recheck appointment with a nurse in 5–7 days (Figure 3). As a second example, for a patient who meets criteria for HTN and has not been previously diagnosed, a tailored SmartSet recommending a diagnosis of “hypertension,” referral to the dietician, and cholesterol screening would appear. The SmartSets also provide Web links to the NHBPEP guidelines and patient educational material that can be inserted into the patient’s “after visit summary” (AVS).
Table 1.
Clinical Variables Pulled from EHR to Create Tailored SmartSets
| PRIOR HYPERTENSION DIAGNOSIS | CURRENT BP | PRIOR BP | BMI PERCENTILE | LIPID SCREEN |
|---|---|---|---|---|
|
|
|
|
|
Piloting and Refining the TeenBP CDS
Our pilot began at the end of November 2013. After conducting two in-person trainings where we introduced the CDS to rooming staff and providers, we turned on TeenBP v1. In TeenBP v1, if the average BP was elevated after remeasuring, rooming staff received the generic message, “Thanks for re-measuring BP. Specific recommendations for this patient will display when the provider opens the chart.” Also in TeenBP v1, the text of provider alerts was generic: “Click to view PERSONALIZED Decision Support for this patient.” Detailed clinical information was limited to the CDS and SmartSets, and was visible only when the provider opened the embedded link.
After an initial two-week period we began monitoring TeenBP. Between December 12, 2013 and March 4, 2014 there were 375 visits from 10–17 year olds at the pilot clinical site. Of these visits, 18 (4.8 percent) had an average systolic or diastolic BP that was ≥ 95th percentile. This included 13 patients (3.4 percent) with a first or second elevated BP who did not meet criteria for hypertension. Half of elevated BPs and 25 percent of patients meeting criteria for hypertension were clinically recognized by the provider. Clinical recognition included one or more of the following: diagnosing hypertension, diagnosing elevated BP, initiating additional work-up related to prehypertension or HTN, or initiating treatment for prehypertension or HTN. Informal feedback from providers and rooming staff at the pilot site was positive.
Based on this initial pilot data and provider feedback, we refined our messaging with the aim of further increasing clinical recognition of elevated BP and HTN. We changed our messaging to rooming staff to be consistent with how other abnormal vital signs would be communicated to providers. In TeenBP v2, when an elevated BP is repeated and the average BP is ≥95th percentile, the message to rooming staff is: “Please let the provider know that the BP is high and further action is needed.” In addition, the provider alert was modified so that key clinical recommendations did not require an additional link to be opened. For example, for a patient with a first or second BP ≥ 95th percentile who does not meet criteria for HTN, the message to providers is the following: “The BP is elevated today. It should be repeated in 1–3 weeks. Accept TeenBP SmartSet to set up nurse visit.” These changes were implemented in early April 2014. A second round of monitoring followed, and brief surveys of rooming staff and providers were conducted.
Between April 4, 2014 and July 8, 2014 the pilot site had 360 visits from adolescents 10–17 years of age. During this period there were 31 initial BPs ≥95th percentile, of which 23 (74 percent) were repeated. In 8 patients (2.2 percent), the average of the initial and repeat BP was ≥95th percentile; 2 patients newly met criteria for hypertension. Using definitions described above, 63 percent of those with elevated BP were clinically recognized, including 1 patient with incident HTN.
Feedback from Staff at the Pilot Clinic
Brief paper surveys were given to providers and staff at the pilot clinic. Surveys included both fixed-response and open-ended questions. The wordings of surveys varied for rooming staff and providers, but both included questions regarding training and work experience (three items), adolescent patient volume (one item), experience with TeenBP alerts (two items), and response to alerts (eight items). Surveys were hand delivered to providers, along with a $50 gift card. Completion of the surveys implied consent from the providers. The clinic supervisor distributed staff surveys, and $200 was provided to a clinic pool. All eight rooming staff from the pilot clinic completed the written survey. Six out of eight (75 percent) reported that alerts to measure the height were “always” or “sometimes” helpful. All eight reported that the alerts to repeat BP were always or sometimes helpful. Four of eight (50 percent) rooming staff respondents reported that alerts to remeasure a BP “sometimes” interfered with their workflow, and the remaining responded that the alerts “rarely” interfered.
Surveys were completed by two of six providers from the pilot clinic. One pilot clinic provider reported that they received few alerts, and because they were infrequent, they were not well integrated into the provider’s workflow. The other pilot clinic provider responded, “I think this is a great program and it is nice to have the alerts.”
Discussion
In the current report, we describe our strategy for developing and piloting a web-based EHR-linked CDS to improve the recognition of prehypertension and HTN in children and adolescents. The potential for EHR technology to improve the quality of care has been widely recognized, but few EHR-based CDS systems have shown positive results with respect to chronic disease care, especially in pediatric or adolescent populations.15,16 To date, our CDS has been accepted among providers and clinical staff, with concerns raised by some regarding how the CDS is incorporated into their workflow. In our single-site pilot, more than half of elevated BPs were clinically recognized.
The TeenBP CDS system incorporates the following innovative features.
The CDS goes beyond simple computer prompts and reminders to provide more sophisticated, tailored CDS, taking into account multiple factors to provide guideline-standardized and locally feasible HTN identification support and recommendations for a range of clinical actions during clinical encounters.
The CDS is provided to both the rooming nurse and provider early in the encounter. This takes advantage of the standardized clinic workflow and increases the likelihood that providers will see the CDS in a timely fashion.
The CDS is implemented in a Web application linked to the EHR, simplifying clinical updates over time—for example, changing the text of the alerts in TeenBP v2—and enhancing the translatability of the CDS to other EHR systems.
The CDS introduces a provider interface that graphically represents BP percentile range and variation over time.
Lessons learned from the development and piloting of TeenBP included the importance of accounting for workflow when providing CDS at the point of care. Our goals for the CDS were to provide the “right information to the right person at the right time in the workflow” while minimizing the burden on clinic staff, patients, and patients’ families. Engagement of key stakeholders and awareness of any potential impact of the CDS on clinical care were also important to CDS implementation. For example, raising the threshold for requesting that a BP be repeated, from the 90th to the 95th percentile, reduced the burden of the CDS on clinical staff while increasing adherence to recommendations.
Despite these strengths, persistent challenges with CDS adoption remain. First, the TeenBP CDS was designed to provide recommendations based on the average of the initial and repeat BP. Therefore, a key step is for the rooming nurse to repeat the BP measurement when prompted. When the BP measurement is not repeated, the CDS does not provide any additional decision support. Similarly, if the BP is remeasured at the end of the visit or if nurse documentation occurs after the provider logs into the EHR, the provider will not receive the full CDS. Thus, continued training and reinforcement of when to enter BP and height measures into the EHR has been important. Furthermore, the CDS will treat all BPs as valid; it cannot identify BPs that are falsely elevated due to measurement error (e.g., patient movement, or inappropriate cuff size.)
An additional challenge has been provider buy-in. During the course of clinic training some providers expressed concerns that the TeenBP clinical recommendations focused too narrowly on the diagnosis and management of essential hypertension. Although most hypertension diagnosed in adolescence is essential hypertension,17 pediatric providers must also consider secondary causes for hypertension. Thus, continued provider education regarding the scope and usefulness of the tool is needed. Similarly, although the NHBPEP and Integrated Guidelines recommend that a BP percentile should be based on the average of several BP measurements at a single visit, we have observed a preference among clinicians to base their assessment and recommendations on the final (and often lowest) BP recorded in the EHR. Therefore, provider awareness and agreement with existing guidelines is needed for TeenBP and other similar EHR-linked CDS tools to have a positive impact on care.
Conclusion
In summary, this report describes the development and piloting of a web-based, EHR-linked CDS system to improve recognition and early management of HTN in children and adolescents. Our pilot of TeenBP demonstrated that the CDS was generally accepted by providers and rooming staff, although integration with clinical workflow remains a challenge. Preliminary findings from TeenBP are promising. During the pilot more than half of BPs in the hypertensive range were clinically recognized. In order to fully evaluate the clinical effectiveness and economic impact of this CDS tool, we are currently conducting a two-year cluster randomized clinical trial across 20 primary care sites within our health system. The full CDS intervention went “live” at the 10 intervention clinics on April 15, 2014. The trial has proceeded thus far without complications. Monitoring of the trial is ongoing; end-of-study data will be available for analyses in fall of 2016. Further details regarding this trial can be found at: https://clinicaltrials.gov/ct2/show/NCT01760239. The results of the full study will help guide further development and dissemination of the TeenBP CDS system.
Acknowledgments
We would like to thank Olga Godlevsky, Vijay Thirumalai and Nicole Trower for their help with programming for this project. We would also like to thank Julie Anderson for work related to this project. Finally, we would like to thank the HealthPartners Medical Group for their support of this effort. This work was supported by the National Heart, Lung and Blood Institute (R01 HL115082-01, PI: Kharbanda).
Footnotes
Disciplines
Health Information Technology | Pediatrics
References
- 1.Tirosh A, Afek A, Rudich A, et al. Progression of normotensive adolescents to hypertensive adults: a study of 26,980 teenagers. Hypertension. 2010 Aug;56(2):203–209. doi: 10.1161/HYPERTENSIONAHA.109.146415. [DOI] [PubMed] [Google Scholar]
- 2.Israeli E, Korzets Z, Tekes-Manova D, et al. Blood-pressure categories in adolescence predict development of hypertension in accordance with the European guidelines. Am J Hypertens. 2007 Jun;20(6):705–709. doi: 10.1016/j.amjhyper.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 3.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008 Jun 24;117(25):3171–3180. doi: 10.1161/CIRCULATIONAHA.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004 Aug;114(2 Suppl 4th Report):555–576. [PubMed] [Google Scholar]
- 5.Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011 Dec;128(Suppl 5):S213–256. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007 Aug 22;298(8):874–879. doi: 10.1001/jama.298.8.874. [DOI] [PubMed] [Google Scholar]
- 7.Lo JC, Sinaiko A, Chandra M, et al. Prehypertension and hypertension in community-based pediatric practice. Pediatrics. 2013 Feb;131(2):e415–424. doi: 10.1542/peds.2012-1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brady TM, Solomon BS, Neu AM, Siberry GK, Parekh RS. Patient-, provider-, and clinic-level predictors of unrecognized elevated blood pressure in children. Pediatrics. 2010 Jun;125(6):e1286–1293. doi: 10.1542/peds.2009-0555. [DOI] [PubMed] [Google Scholar]
- 9.Bijlsma MW, Blufpand HN, Kaspers GJ, Bokenkamp A. Why pediatricians fail to diagnose hypertension: a multicenter survey. The Journal of pediatrics. 2014 Jan;164(1):173–177. e177. doi: 10.1016/j.jpeds.2013.08.066. [DOI] [PubMed] [Google Scholar]
- 10.Daley MF, Sinaiko AR, Reifler LM, et al. Patterns of care and persistence after incident elevated blood pressure. Pediatrics. 2013 Aug;132(2):e349–355. doi: 10.1542/peds.2012-2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moyer VA. Screening for primary hypertension in children and adolescents: U.S. Preventive Services Task Force recommendation statement. Pediatrics. 2013 Nov;132(5):907–914. doi: 10.1542/peds.2013-2864. [DOI] [PubMed] [Google Scholar]
- 12.Thompson M, Dana T, Bougatsos C, Blazina I, Norris SL. Screening for hypertension in children and adolescents to prevent cardiovascular disease. Pediatrics. 2013 Mar;131(3):490–525. doi: 10.1542/peds.2012-3523. [DOI] [PubMed] [Google Scholar]
- 13.McKee MD, Rubin SE, Campos G, O’Sullivan LF. Challenges of providing confidential care to adolescents in urban primary care: clinician perspectives. Ann Fam Med. 2011 Jan-Feb;9(1):37–43. doi: 10.1370/afm.1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henry-Reid LM, O’Connor KG, Klein JD, Cooper E, Flynn P, Futterman DC. Current pediatrician practices in identifying high-risk behaviors of adolescents. Pediatrics. 2010 Apr;125(4):e741–747. doi: 10.1542/peds.2009-0271. [DOI] [PubMed] [Google Scholar]
- 15.Institute of Medicine (US) Committee on Improving the Patient Record. Dick RS, Steen EB. The computer-based patient record : an essential technology for health care. Washington, D.C: National Academy Press; 1991. [PubMed] [Google Scholar]
- 16.Fiks AG. Designing computerized decision support that works for clinicians and families. Curr Probl Pediatr Adolesc Health Care. 2011 Mar;41(3):60–88. doi: 10.1016/j.cppeds.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoon EY, Cohn L, Freed G, et al. Use of antihypertensive medications and diagnostic tests among privately insured adolescents and young adults with primary versus secondary hypertension. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2014 Jul;55(1):73–78. doi: 10.1016/j.jadohealth.2013.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]