Abstract
The number of studies on psychological treatments of depression in older adults has increased considerably in the past years. Therefore, we conducted an updated meta-analysis of these studies. A total of 44 studies comparing psychotherapies to control groups, other therapies or pharmacotherapy could be included. The overall effect size indicating the difference between psychotherapy and control groups was g=0.64 (95% CI: 0.47∼0.80), which corresponds with a NNT of 3. These effects were maintained at 6 months or longer post randomization (g=0.27; 95%CI 0.16∼0.37). Specific types of psychotherapies that were found to be effective included cognitive behavior therapy (g=0.45; 95% CI: 0.29∼0.60), life review therapy (g=0.59; 95% CI: 0.36∼0.82) and problem-solving therapy (g=0.46; 95% CI: 0.18∼0.74). Treatment compared to waiting list control groups resulted in larger effect sizes than treatments compared to care-as-usual and other control groups (p<0.05). Studies with lower quality resulted in higher effect sizes than high-quality studies (p<0.05). Direct comparisons between different types of psychotherapy suggested that cognitive behavior therapy and problem-solving therapy may be more effective than non-directive counseling and other psychotherapies may be less effective than other therapies. This should be considered with caution, however, because of the small number of studies. There were not enough studies to examine the long-term effects of psychotherapies and to compare psychotherapy with pharmacotherapy or combined treatments. We conclude that it is safe to assume that psychological therapies in general are effective in late-life depression, and this is especially well-established for cognitive behavior therapy and problem-solving therapy.
Keywords: depression, older adults, psychotherapy, cognitive behavior therapy, life review, problem-solving therapy, meta-analysis
Introduction
It is well-established that psychological interventions are effective in the treatment of depression in adults, and that includes cognitive behavior therapy (CBT) [1], interpersonal psychotherapy (IPT) [2], behavioral activation therapy [3], problem-solving therapy (PST) [4], and possibly psychodynamic therapy [5] and non-directive counseling [6]. Whether psychological therapies are also effective in older adults has been less well-established. Depression in older adults tends to be more chronic than in their younger counterparts. And due to such a chronic nature and developmental stage that increase individual's exposure risk factors (e.g., medical condition, loss and grief, decreasing social support), psychotherapies may be less effective in older adults than in their younger counterparts.
Although several trials with different kinds of psychological treatment have focused specifically on older adults, the field is changing rapidly. In an earlier meta-analysis of these studies, we included 25 randomized trials [7], and other meta-analyses from this period included comparable numbers of studies [8-10]. Since 2010, however, 15 more randomized trials have been conducted, indicating that the field is expanding rapidly. It may be possible to examine research questions that were not answered sufficiently with meta-analyses of earlier trials. For example, several new trials have focused on life review treatments of depression, and earlier meta-analyses had to be careful in drawing definite conclusions on this type of therapy.
Since the overall meta-analyses focusing on psychological treatments in older adults from 2006 to 2008, no general meta-analyses have been conducted. Meta-analyses that were conducted since focused on specific types of therapies [11-14]. We decided therefore, to conduct a new meta-analysis of trials on psychological treatments of depression in older adults. Because the number of trials has increased since the previous comprehensive meta-analysis, we focus specifically on subgroup analyses. In these subgroup analyses we can examine whether specific characteristics of the studies are associated with higher or lower effect sizes, for example different types of psychotherapy, types of control groups, recruitment methods, diagnosis, or treatment format.
Methods
Identification and selection of studies
We constructed a database of papers on the psychological treatment of depression that has been described in detail elsewhere [15] and that has been used in a series of earlier published meta-analyses (www.evidencebasedpsychotherapies.org). This database has been continuously updated through comprehensive literature searches (from 1966 to January 2014). In these searches, we examined 14,902 abstracts from Pubmed, PsycInfo, Embase and the Cochrane Register of Trials. These abstracts were identified by combining terms indicative of psychological treatment and depression (both MeSH terms and text words). For this database, we also checked the primary studies from earlier meta-analyses of psychological treatment for depression to ensure that no published studies were missed. From the 14,902 abstracts, we retrieved 1,613 full-text papers for possible inclusion in the database.
We included (a) randomized controlled trials in which (b) a psychological intervention (c) was compared to a control condition (d) in older adults (> 50 years of age) (e) with depression (established through a diagnostic interview or through a cut-off on a self-report scale). We included randomized trials in which psychological treatments were compared with a control group, with another psychological treatment, and with pharmacotherapy. We also included studies in which the combination of psychotherapy and pharmacotherapy was compared with psychotherapy alone or pharmacotherapy alone.
We excluded studies in younger adults, adolescents or children (≥ 18 years). Comorbid general medical or psychiatric disorders were not used as an exclusion criterion. No language restrictions were applied.
Quality assessment and data extraction
We assessed the validity of included studies using four criteria of the ‘Risk of bias’ assessment tool, developed by the Cochrane Collaboration [16]. This tool assesses possible sources of bias in randomized trials, including the adequate generation of allocation sequence; the concealment of allocation to conditions; the prevention of knowledge of the allocated intervention (masking of assessors); and dealing with incomplete outcome data (this was assessed as positive when intention-to-treat analyses were conducted, meaning that all randomized patients were included in the analyses).
We also coded additional aspects of the included studies, including characteristics of the participants, the interventions and the study. Quality assessment and data extraction was done by two independent researchers.
Meta-analyses
For each comparison between a psychotherapy condition and a control or comparison group, the effect size indicating the difference between the two groups at post-test was calculated (Hedges's g). Because several studies had relatively small sample sizes, we corrected the effect size for small sample bias [18].
In the calculations of effect sizes, we used only those instruments that explicitly measured symptoms of depression. If more than one depression measure was used, the mean of the effect sizes was calculated, so that each comparison yielded only one effect (using the methods described in Borenstein et al.) [19]. If dichotomous outcomes were reported without means and standard deviations, we used the procedures described by Borenstein et al. [19] to calculate the standardized mean difference.
To calculate pooled mean effect sizes, we used the computer program Comprehensive Meta-Analysis (version 2.2.021). Because we expected considerable heterogeneity among the studies, we used a random effects pooling model in all analyses. Numbers-needed-to-treated (NNT) were calculated using the formulae provided by Kraemer and Kupfer [20]. The NNT indicates the number of patients that have to be treated in order to generate one additional positive outcome [21]. As a test of homogeneity of effect sizes, we calculated the I2-statistic as an indicator of heterogeneity in percentages. A value of 0% indicates no observed heterogeneity, and larger values indicate increasing heterogeneity, with 25% as low, 50% as moderate, and 75% as high heterogeneity. We calculated 95% confidence intervals around I2 [22], using the non-central chi-squared-based approach within the heterogi module for Stata [23].
Subgroup analyses were conducted according to the mixed effects model [19], in which studies within subgroups are pooled with the random effects model, while tests for significant differences between subgroups are conducted with the fixed effects model. For continuous variables, we used meta-regression analyses to test whether there was a significant relationship between the continuous variable and effect size, as indicated by a Z-value and an associated p-value.
Publication bias was tested by inspecting the funnel plot on primary outcome measures and by Duval and Tweedie's trim and fill procedure [24], which yields an estimate of the effect size after the publication bias has been taken into account. We also conducted Egger's test for the asymmetry of the funnel plot.
Results
Selection of studies and characteristics of included studies
Figure 1 presents a flowchart describing the inclusion process. Of the 1,613 retrieved full-text papers, 1,569 were excluded (Figure 1), while 44 studies met inclusion criteria [25-68]. In the included studies, 4,409 patients participated (2,512 in psychotherapy, 1,595 in control conditions, 194 in psychotherapy plus pharmacotherapy conditions, and 108 in the pharmacotherapy-only conditions). Selected characteristics of the 44 studies are presented in Table 1.
Figure 1. Flowchart of inclusion of studies.
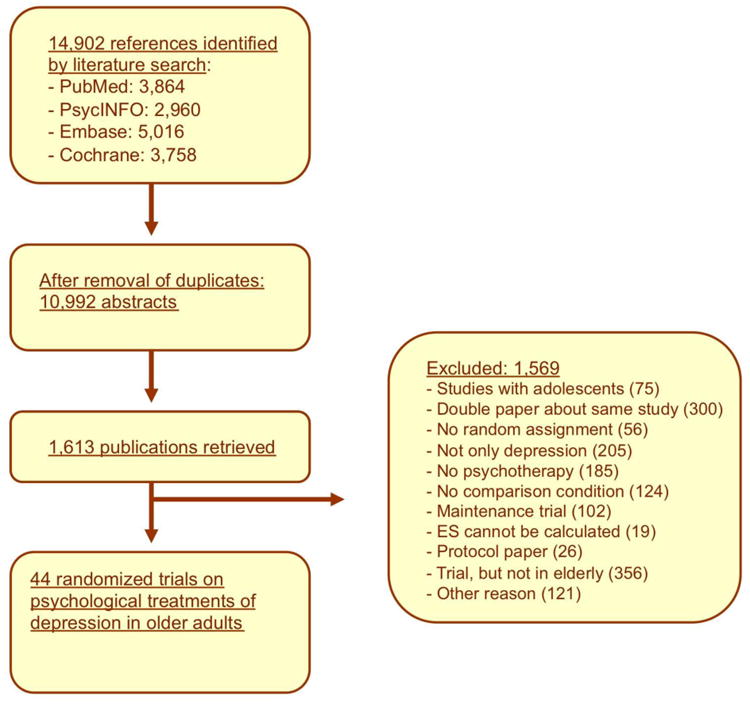
Table 1. Selected characteristics of studies examining psychological treatments of depression in older adults.
| Age | Recr | Diagn | Conditions | N | For-mat | Nsess | Quality a) | Country | |
|---|---|---|---|---|---|---|---|---|---|
| Alexopoulos, 2011 | ≥ 59 | Comm | MDD | 1. PST 2. Supportive |
110 111 |
Ind | 12 | − + + + | US |
| Alexopoulos, 2003 | ≥ 65 | Clin | MDD | 1. PST 2. Supportive |
12 13 |
Ind | 12 | − − + + | US |
| Arean, 2010 | ≥ 65 | Comm | MDD | 1. PST 2. Supportive |
90 97 |
Ind | 12 | + + + + | US |
| Arean, 1993 | ≥ 55 | Comm | MDD | 1. PST 2. Life review 3. WL |
19 28 20 |
Grp | 12 | − − + − | US |
| Burns, 2007 | ≥ 65 | Other | Cut-off | 1. OthTher 2. CAU |
50 54 |
Ind | 6 | + + + + | UK |
| Chan, 2013 | ≥ 60 | Comm | Cut-off | 1. Life review 2. CAU |
14 12 |
Ind | 5 | + − + + | Singap |
| Choi, 2013 | ≥ 50 | Other | Cut-off | 1. Tele- PST 2. PST 3. Telecare |
42 43 36 |
Ind | 6 | − − − + | US |
| Ekkers, 2011 | ≥ 65 | Clin | MDD | 1. CBT 2. CAU |
53 34 |
Grp | 7 | + + + + | NL |
| Floyd, 2004 | ≥ 60 | Comm | Mood | 1. CBT - gsh 2. CBT - ind 3. WL |
13 8 14 |
GshInd | 416 | − − − − | US |
| Fry, 1983 | 65-82 | Other | Cut-off | 1. Life rev - struct 2. Life rev - unstruct 3. Other control |
54 54 54 |
Ind | 5 | − − + − | US |
| Gallagher, 1982 | ≥ 55 | Comm | MDD | 1. CBT 2. BAT 3. DYN |
10 10 10 |
Ind | 16 | − − + − | US |
| Gitlin, 2013 | ≥ 55 | Comm | Cut-off | 1. Multicomponent 2. Waiting list |
106 102 |
Ind | 10 | + + + + | US |
| Haringsma, 2005 | 55-85 | Comm | Subclin | 1. CBT 2. WL |
52 58 |
Grp | 10 | − − + + | NL |
| Hautzinger, 2008 | ≥ 65 | Comm | Cut-off | 1. CBT - ind 2. Supportive - ind 3. CBT - grp 4. Supportive – grp |
24 25 34 26 |
Ind Ind Grp Grp |
15 | − − + + | GER |
| Hautzinger, 2004 | ≥ 60 | Comm | Mood | 1. CBT 2. WL |
55 30 |
Grp | 12 | + + + + | GER |
| Heckman, 2011 | ≥ 50 | Comm | Cut-off | 1. Coping ther 2. Supportive 3. OthCtr |
104 105 86 |
Grp | 12 | + + + + | US |
| Joling, 2011 | ≥ 75 | Other | Cut-off | 1. CBT 2. CAU |
86 84 |
Gsh | 3 | + + + + | NL |
| Kiosses, 2010 | ≥ 65 | Comm | MDD | 1. PST 2. Supportive |
13 12 |
Ind | 12 | − − − + | US |
| Korte, 2012 | ≥ 55 | Comm | Cut-off | 1. Life review 2. CAU |
100 102 |
Grp | 8 | + + + + | NL |
| Laidlaw, 2008 | ≥ 60 | Clin | MDD | 1. CBT 2. CAU |
20 20 |
Ind | 8 | + + + − | UK |
| Lamers, 2010 | ≥ 60 | Other | Mood | 1. CBT 2. CAU |
111 125 |
Ind | 6 | + + + + | NL |
| Landreville, 1997 | ≥ 55 | Comm | Cut-off | 1. CBT 2. WL |
10 13 |
Gsh | 4 | − − + − | Canada |
| Lynch, 2003 | ≥ 60 | Clin | MDD | 1. Dialect beh + PHA 2. PHA (protocol) |
15 16 |
Grp | 56 | − − − − | US |
| Mossey, 1996 | ≥ 60 | Other | Subclin | 1. IPT 2. CAU |
31 38 |
Ind | 10 | − − + − | US |
| Pot, 2010 | ≥ 50 | Comm | Subclin | 1. Life review 2. OthCtr |
83 88 |
Grp | 12 | − + + + | NL |
| Preschl, 2012 | ≥ 65 | Comm | Cut-off | 1. Life review 2. WL |
20 16 |
Ind | 8 | + − + + | Switz |
| Reynolds, 1999 | ≥ 50 | Comm | MDD | 1. IPT + PHA (TCA) 2. PHA 3. IPT + Placebo 4. Placebo |
16 25 17 22 |
Ind | 16 | − − + + | US |
| Scogin, 1987 | ≥ 60 | Comm | Cut-off | 1. CBT 2. WL 3. Attention-control |
9 8 8 |
Gsh | 4 | − − − − | US |
| Scogin, 1989 | ≥ 60 | Comm | Cut-off | 1. CBT – cwd 2. CBT – ct 3. WL |
19 21 21 |
Gsh | 4 | − − − − | US |
| Serfaty, 2009 | ≥ 65 | Comm | Mood | 1. CBT 2. Talking control 3. CAU |
64 58 55 |
Ind | 12 | + + + + | UK |
| Serrano, 2004 | 65-93 | Other | Cut-off | 1. Life review 2. CAU |
20 23 |
Ind | 4 | − − + − | Spain |
| Serrano, 2012 | 64-83 | Clin | MDD | 1. Life review 2. Other control |
9 8 |
Ind | 6 | − − + + | Spain |
| Sirey, 2005 | 65-85 | Clin | MDD | 1. OthTher + PHA 2. PHA |
21 24 |
Ind | 5 | − − + + | US |
| Sloane, 1985 | M = 64.4 | Other | MDD | 1. IPT 2. PHA 3. Placebo |
19 10 14 |
Ind | 6 | − − + − | US |
| Snarksi, 2011 | ≥ 65 | Clin | Cut-off | 1. BAT 2. CAU |
16 13 |
Ind | 8 | − − + + | US |
| Spek, 2007 | 50-75 | Comm | Subclin | 1. CBT 2. iCBT (unguided) 3. WL |
102 99 100 |
Grp | 10 | + + + + | NL |
| Teri, 1997 | M = 76.4 | Other | Cut-off | 1. PST 2. BAT 3. CAU 4. WL |
23 19 10 20 |
Ind | 9 | − − + − | US |
| Thompson, 1987 | ≥ 60 | Comm | MDD | 1. CBT 2. BAT 3. DYN |
14 6 9 |
Ind | 18 | − − − − | US |
| hompson, 1984 | ≥ 60 | Other | MDD | 1. CBT 2. BAT 3. DYN |
21 17 20 |
Ind | 18 | − − − − | US |
| Thompson, 2001 | ≥ 60 | Comm | MDD | 1. PHA (TCA) 2. CBT 3. CBT + PHA |
33 31 36 |
Ind | 18 | − − − + | US |
| Van Schaik, 2006 | ≥ 55 | Clin | MDD | 1. IPT 2. CAU |
69 74 |
Ind | 10 | + + + + | NL |
| Watt, 2000 | ≥ 60 | Comm | Cut-off | 1. Life rev – integr 2. Life rev – instr 3. Other control |
9 9 9 |
Grp | 6 | − − + − | Canada |
| Williams, 2000 | ≥ 60 | Comm | Mood | 1. PHA (SSRI) 2. PST 3. Placebo |
106 113 119 |
Ind | 6 | + + + + | US |
| Wuthrich, 2013 | ≥ 60 | Comm | Cut-off | 1. CBT 2. Waiting list |
27 35 |
Grp | 12 | + − + + | Austra-lia |
In this column a positive (+), or negative (-)sign is given for four quality criteria, respectively: allocation sequence; concealment of allocation to conditions; blinding of assessors; and intention-to-treat analyses
Abbreviations: BAT: behavioral activation therapy; CAU: care-as-usual; CBT: cognitive behavior therapy; Clin: clinical; Comm: community; Cwd: Coping with Depression course; Diagn: diagnosis; Dialect beh: dialectic behavior therapy; DYN: psychodynamic therapy; GER: Germany; Grp: group; Gsh: guided self-help; iCBT: Internet-based CBT; Ind: individual; Instr: instrumental; Integr: integrated; IPT: interpersonal psychotherapy; Life rev: life review; MDD: major depressive disorder; Mood: mood disorder; NL: Netherlands; Nsess: number of sessions; OthCtr: Other control group; OthTher: other type of therapy; PHA: pharmacotherapy; PST: problem-solving therapy; Recr: recruitment; Singap: Singapore; Struct: structured; Switz: Switzerland; Ther: therapy; UK: United Kingdom; Unstruct: unstructured; US: United States; WL: waiting list.
The quality of the included studies varied (Table 1). Seventeen of the 44 studies reported an adequate sequence generation. Sixteen studies reported allocation to conditions by an independent (third) party. A total of 35 studies reported blinding of outcome assessors or used only self-report outcome measures, and in 28 studies intention-to-treat analyses were conducted. Thirteen studies met all four quality criteria, 13 met 2 or 3 criteria; and the remaining 18 studies had a lower quality (0 or 1 of the four criteria).
Effects of psychotherapy versus control groups at post-test
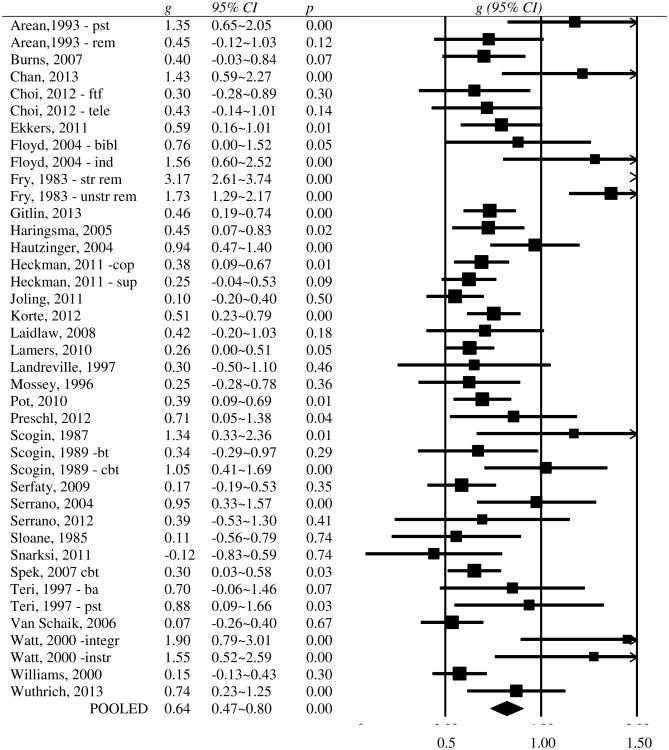
We compared the effects of psychotherapy with a control group in 40 comparisons from 32 studies (in 8 studies two types of psychotherapy were compared with a control group). The overall effect size was g=0.64 (95% CI: 0.47∼0.80), which corresponds with a NNT of 2.86. Heterogeneity was high (I2=80; 95% CI: 73∼85). A forest plot of the effect sizes and 95% CIs are presented in Figure 2.
Figure 2. Forest plot of effect sizes of randomized trials on psychotherapy for depression in older adults.
Inspection of this forest plot indicated that there were potential outliers. We excluded five studies with an effect size of g=1.5 or higher, and ran the analyses again. This resulted in a lower effect size (g=0.43; 95% CI: 0.33∼0.52; NNT=4.20), but also in a reduction of heterogeneity (I2=36; 95% CI: 4∼58).
In this meta-analysis we included eight studies in which two psychological treatments were compared with the same control group. This means that multiple comparisons from these studies were included in the same analysis, that are not independent of each other, which may have resulted in an artificial reduction of heterogeneity and may have affected the pooled effect size. We examined the possible effects of this by conducting an analysis in which we included only one effect size per study. First, we included only the comparison with the largest effect size from these studies and then we conducted another analysis in which we included only the smallest effect size. As can be seen from Table 2, the resulting effect sizes did not affect the overall mean effect size very much, nor did it affect heterogeneity considerably.
Table 2. Effects of psychological treatments of depression in older adults compared with control groups: Hedges' ga).
| Ncomp | g | 95% CI | I2 | 95% CI | NNT | 95% CI | p b) | ||
|---|---|---|---|---|---|---|---|---|---|
| All studies | 40 | 0.64 | 0.47∼0.80 | 80 | 73∼85 | 2.86 | 2.34∼3.85 | ||
| 5 possible outliers excluded c) | 35 | 0.43 | 0.33∼0.52 | 36 | 4∼58 | 4.20 | 3.50∼5.43 | 4.20 | |
| One effect size per study (only highest) | 32 | 0.62 | 0.43∼0.80 | 80 | 72∼85 | 2.96 | 2.34∼4.20 | 2.96 | |
| One effect size per study (only lowest) | 32 | 0.50 | 0.33∼0.67 | 62 | 44∼74 | 3.62 | 2.75∼4.10 | 3.62 | |
| GDS only | 19 | 0.50 | 0.33∼0.67 | 42 | 0∼66 | 3.62 | 2.75∼4.10 | ||
| HAMD only | 13 | 1.26 | 0.86∼1.65 | 70 | 47∼83 | 1.59 | 1.32∼2.19 | ||
| BDI only | 12 | 0.76 | 0.26∼1.26 | 91 | 87∼94 | 2.44 | 1.59∼6.85 | ||
| CES-D only | 7 | 0.46 | 0.29∼0.62 | 34 | 0∼72 | 3.91 | 2.96∼6.17 | ||
| Subgroup analysesd) | |||||||||
| Recruitment | Community | 20 | 0.49 | 0.36∼0.61 | 46 | 8∼68 | 3.68 | 2.99∼5.00 | 0.26 |
| Clinical samples only | 5 | 0.27 | -0.01∼0.54 | 19 | 0∼83 | 6.58 | e) | ||
| Other | 10 | 0.36 | 0.17∼0.55 | 9 | 0∼66 | 5.00 | 3.31∼10.42 | ||
| Diagnosis | Diagnosed mood dis. | 14 | 0.42 | 0.25∼0.58 | 49 | 6∼73 | 4.27 | 3.14∼7.14 | 0.73 |
| Cut-off selfreport | 17 | 0.47 | 0.32∼0.61 | 39 | 0∼66 | 3.85 | 2.99∼5.56 | ||
| Subclinical depression | 4 | 0.36 | 0.11∼0.60 | 0 | 0∼85 | 5.00 | 3.05∼16.13 | ||
| Psychotherapy | CBT | 14 | 0.45 | 0.29∼0.60 | 43 | 0∼70 | 4.00 | 3.05∼6.17 | 0.24 |
| Life review | 7 | 0.59 | 0.36∼0.82 | 20 | 0∼64 | 3.09 | 2.28∼5.00 | ||
| PST | 5 | 0.46 | 0.18∼0.74 | 65 | 9∼87 | 3.91 | 2.50∼9.80 | ||
| Other | 9 | 0.29 | 0.11∼0.47 | 0 | 0∼65 | 6.17 | 3.85∼16.13 | ||
| Format f) | Individual | 18 | 0.36 | 0.22∼0.50 | 25 | 0∼58 | 5.00 | 3.62∼8.06 | 0.41 |
| Group | 11 | 0.50 | 0.35∼0.65 | 36 | 0∼69 | 3.62 | 2.82∼5.10 | ||
| Guided self-help | 6 | 0.47 | 0.19∼0.75 | 58 | 0∼83 | 3.85 | 2.48∼9.43 | ||
| Number of sessions | 12-16 | 8 | 0.48 | 0.29∼0.66 | 57 | 6∼80 | 3.76 | 2.78∼6.17 | 0.19 |
| 6-10 | 19 | 0.36 | 0.23∼0.49 | 0 | 0∼49 | 5.00 | 3.68∼7.69 | ||
| 3-5 | 8 | 0.61 | 0.35∼0.86 | 65 | 25∼83 | 2.99 | 2.19∼5.10 | ||
| Control group | Waiting list | 13 | 0.60 | 0.44∼0.76 | 33 | 0∼65 | 3.05 | 2.44∼4.10 | 0.02 |
| Care as usual | 13 | 0.38 | 0.24∼0.52 | 47 | 0∼72 | 4.72 | 3.50∼7.46 | ||
| Other | 9 | 0.28 | 0.12∼0.44 | 0 | 0∼65 | 6.41 | 4.10∼14.71 | ||
| Quality score | 4 | 12 | 0.34 | 0.21∼0.46 | 38 | 0∼69 | 5.26 | 3.91∼8.47 | 0.05 |
| Lower than 4 | 23 | 0.52 | 0.39∼0.66 | 29 | 0∼57 | 3.50 | 2.78∼4.59 | ||
| Direct comparisonsg) | |||||||||
| - CBT vs other therapies | 8 | 0.31 | 0.05∼0.57 | 0 | 0∼68 | 5.75 | 3.18∼35.71 | ||
| - Behavioral activation vs other therapies | 6 | 0.06 | -0.26∼0.39 | 0 | 0∼75 | 29.41 | e) | ||
| - Psychodynamic vs other therapies | 6 | -0.30 | -0.63∼0.03 | 0 | 0∼75 | 5.95 | e) | ||
| - Problem solving ther. vs other therapies | 6 | 0.30 | 0.08∼0.52 | 55 | 0∼82 | 5.95 | 3.50∼21.74 | ||
| - Supportive counseling vs other therapies | 6 | -0.34 | -0.55∼ -0.12 | 61 | 6∼84 | 5.26 | e) | ||
| Comparisons with pharmacotherapyf) | |||||||||
| Combined versus pharmacotherapy | 4 | 0.41 | -0.05∼0.88 | 0 | 0∼85 | 4.39 | e) | ||
| Psychotherapy versus pharmacotherapy | 3 | -0.11 | -0.54∼0.33 | 0 | 0∼90 | 16.13 | e) | ||
: p<0.05 **: p<0.01 ***: p<0.001
Abbreviations: CI: Confidence interval; Ncomp: number of comparisons; NNT: Numbers-needed-to-treat.
according to the random effects model.
the p-values in this column indicate whether the difference between the effect sizes in the subgroups is significant.
2 effect sizes from Fry, 1983; 2 effect sizes from Watt et al., 2000, and one effect size from Floyd et al., 2004.
In the subgroup analyses the 5 possible outliers were not included
95% confidence intervals of NNTs in which one of the limits is negative and the other positive, cannot be calculated;
In one study (Choi et al., 2012) tele-psychotherapy was used; this was coded as individual format.
A positive effect size indicates that the first intervention was superior to the second
We also calculated the effect sizes based on the most used depression measures, the GDS, the HRSD, the BDI, and the CES-D. As can be seen in Table 2, these effect sizes did not differ considerably from the overall pooled effect size, except for the effect size based on the HRSD (g=1.26; 95% CI: 0.86∼1.65; I2=70; 95% CI: 47∼83; NNT=1.59). This effect size was much larger than the overall effect size and the 95% confidence intervals of HRSD effect size did not overlap with the overall effect size.
Inspection of the funnel plot suggested considerable publication bias. Egger's test of the intercept was highly significant (intercept: 2.58; 95% CI: 0.99∼4.16; p=0.001). Duvall and Tweedie's trim and fill procedure indicated that 12 studies were missing and that after adjustment for these missing studies the effect size would drop to g=0.35 (95% CI: 0.16∼0.54). When the 5 possible outliers were removed, there was still significant publication bias according to Egger's test (p<0.001), and to Duvall and Tweedie's trim and fill procedure (n missing studies= 9; adjusted effect size g=0.32; 95% CI: 0.21∼0.44).
Effects of psychotherapy versus control groups at 6 months or longer post-randomization
We examined the long-term effects of psychotherapy compared to control groups across 12 comparisons from 11 studies (in one study two types of psychotherapy were compared to control group). The results indicated that psychotherapy outperformed control groups at 6 months or longer after the beginning of the treatment of older adults with depressive symptoms (g=0.27; 95%CI: 0.16∼0.37). Heterogeneity was zero (95%CI: 0∼58) while there was no indication for publication bias.
Subgroup and metaregression analyses
In order to examine possible sources of heterogeneity we conducted a series of subgroup analyses. Because the effect sizes of the five possible outliers were so large, we knew in advance that these would have a large impact on the effect sizes and heterogeneity levels of the subgroups. Therefore, we ran the subgroup analyses twice, one time with the outliers and one time without.
The analyses in which the outliers were excluded are reported in Table 2. We did not find significant differences between subgroups of studies using different recruitment methods, definitions of depression, types of psychotherapy, treatment format and number of treatment sessions. We did find a significant difference between studies according to the type of control group that was used. Studies in which a waiting list control group was used resulted in a higher effect size than studies in which a care-as-usual or another type of control group was used (p<0.05). We also found that studies with a higher quality score resulted in a lower effect size than studies with a lower quality score (p<0.05).
The subgroup analyses in which we did not remove the outliers resulted in comparable outcomes than the analyses in which the outliers were not removed (results are not reported in Table 2). The only major difference was that in these analyses we did find a significant difference between types of psychotherapy, with life review resulting in a much higher effect size (g=1.14; 95% CI: 0.83∼1.45) than each of the other categories of psychotherapy. The reason for this was that four of the five outliers examined a life review intervention. We also found that studies with interventions of three to five sessions (g=1.11; 95% CI: 0.78∼1.44) had significant higher effects than other studies (p<0.01) in these analyses.
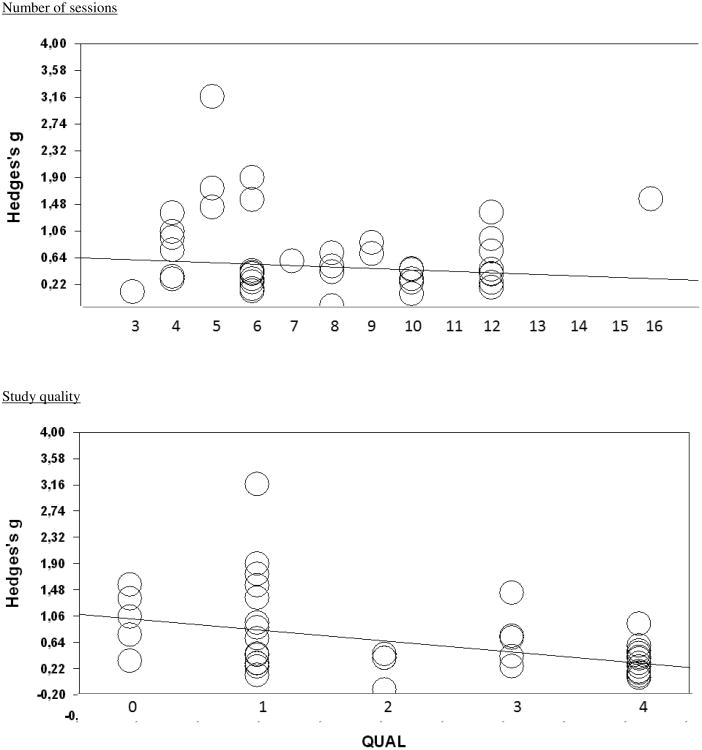
We further examined the association between two continuous variables (number of treatment sessions and quality of the studies) in metaregression analyses (Figure 3). We did not find a significant association between the effect size and the number of sessions (although there was a trend suggesting that the effect size was smaller with a higher number of sessions; slope: -0.02; 95% CI: -0.05∼0.00; p=0.06). We did find that the effect size was significantly associated with the quality of the study, with higher effect sizes in lower-quality studies (slope: -0.018; 95% CI: -0.23∼-0.12; p<0.001).
Figure 3. Relation of effect size to number of treatment sessions and study quality in psychological treatments of depression in older adults.
Other comparisons
There were 8 comparisons in which CBT was directly compared with another psychotherapy (Table 2). It was found that CBT was somewhat more effective than the other therapies (g=0.31; 95% CI: 0.05∼0.57; I2=0; 95% CI: 0∼68; NNT=5.75). We also found that problem-solving therapy was more effective than other psychotherapies (g=0.30; 95% CI: 0.08∼0.52; I2=55; 95% CI: 0∼82; NNT=5.95). Furthermore, we found that non-directive supportive counseling was significantly less effective than other therapies (g=-0.34; 95% CI: -0.55∼ -0.12; I2=61; 95% CI: 6∼84; NNT=5.26). We did not find significant differences between behavioral activation therapy and other therapies, and between psychodynamic therapy and other psychotherapies. Because of the small number of studies in each of these categories, we did not conduct further analyses.
There were four studies in which the combination of psychotherapy and pharmacotherapy was compared with pharmacotherapy alone. The difference was not significant (g=0.41; 95% CI: -0.05∼0.88; I2=0; 95% CI: 0∼85; NNT=4.39), but this be caused by the small number of studies. The 3 studies in which psychotherapy was directly compared with pharmacotherapy did not result in a significant difference either (g=-0.11; 95% CI: -0.54∼0.33; I2=0; 95% CI: 0∼90; NNT=16.13). Because we only found one study in which combined treatment was compared with psychotherapy only (Thompson et al., 2001),[62] we did not conduct any analysis with this outcome.
Discussion
In this updated meta-analysis of psychological treatments of depression in older adults, we could confirm that these treatments have moderate to high effect on depression, which were maintained at 6 months or longer post-randomization. The effects are probably overestimated because of publication bias and because of the low quality of several of the included studies. In the subgroup analyses, we could confirm that CBT is an effective treatment for older adults, as confirmed in earlier meta-analyses [8-14]. However, we also found evidence that life-review therapy and problem-solving therapy are also effective treatments. We did not find evidence that the effect size was related to the way in which patients were recruited, to how depression was defined, to the type of treatment or to the length of treatment. Effect sizes were, however, significantly lower in high-quality studies, which is in line with previous research in younger adults [69].
We also found that waiting list control groups resulted in larger effect sizes then care-as-usual and other control groups, which is also in line with earlier research [70,71]. A problem with “care-as-usual” is that it could range from doing nothing to alerting the patient's depression status to the primary care provider or to prescribing antidepressant and psychotherapy. This is confirmed by the relatively high levels of heterogeneity found in our subgroup analyses for care-as-usual.
We found different effects of different types of psychological interventions: CBT and PST were found to be more effective than other therapies investigated, whereas non-directive counseling was found to be less effective. This is not in line with meta-analytic research in younger age groups, in which no or only small differences between psychotherapies for depression has been found [17,72] It is possible that CBT and problem-solving therapy are indeed more effective in older adults. It is also possible, however, that this is a chance finding caused by low-quality studies or a low number of studies, which makes further interpretation of the findings premature. For non-directive counseling we did find in a previous meta-analysis that this type of treatment is less effective than other therapies [6]. However, researcher allegiance in favor of other therapies than counseling is a common phenomenon in this research area, and after adjustment for researcher allegiance the difference between counseling and other therapies was found to be no longer significant. Whether this is also the case in research on counseling in older adults cannot be established at this moment, because the number of studies is too small.
We found that the outcomes when measured with the HAM-D were considerably larger than when these measured with self-report instruments, such as the GDS or BDI. This is in line with earlier meta-analytic research in which self-report instruments were found to be more conservative when used as outcome instrument in depression outcome research [73] This could indicate that self-report measures are more conservative, that clinician-rated instruments are more sensitive to change, or that both are true.
Unfortunately, we still did not have sufficient studies to compare psychotherapy with pharmacotherapy, or to compare the combination of psychotherapy and pharmacotherapy to either of them alone. These are important goals for future studies in this area.
The results of this meta-analysis should be considered with caution for the following reasons. First, we found that the quality of many included studies was not optimal. Secondly, the number of effect sizes for different types of interventions we could include was still relatively small, although the number of effect sizes has increased steadily over the past years. Thirdly, most studies used a waiting list or a care-as-usual comparison group, and very few studies used placebo control groups.
It is also not clear whether the studies are representative of depressed older adults in general. Most studies include older adults from 60 or 65, but it is not clear whether “older” elderly, over 75 or 80 are included in these studies. The majority of studies was also aimed at older adults who scored above a cut-off on a self-report measure or who had subthreshold depression, and the number of studies aimed at older adults with a diagnosed major depressive disorder was relatively small. The results of this meta-analysis can not therefore be automatically generalized to older adults with a severe depressive disorder. Furthermore, in many older adults depression coexists with cognitive impairment, comorbid medical illness, and disabilities born of these illnesses, and it is not clear whether these older adults have participated in these studies. From a clinical perspective one could also wonder whether it would be useful to include caregivers of depressed older adults in the treatments, as these caregivers have a major role in the care for older adults. It is remarkable that only a few of the included studies did include these caregivers.
Despite these limitations it is safe to assume that psychological therapies in general are effective in old age depression, and this is especially well-established for cognitive behavior therapy and problem-solving therapy. Further dissemination of these treatments seems to be justified.
References
- 1.Cuijpers P, Berking M, Andersson G, Quigley L, Kleiboer A, Dobson KS. A meta-analysis of cognitive behavior therapy for adult depression, alone and in comparison to other treatments. Canadian Journal of Psychiatry. 2013;58:376–385. doi: 10.1177/070674371305800702. [DOI] [PubMed] [Google Scholar]
- 2.Cuijpers P, Geraedts AS, van Oppen P, Andersson G, Markowitz JC, van Straten A. Interpersonal psychotherapy of depression: A meta-analysis. American Journal of Psychiatry. 2011;168:581–592. doi: 10.1176/appi.ajp.2010.10101411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ekers D, Richards D, Gilbody S. A meta-analysis of randomized trials of behavioral treatment of depression. Psychological Medicine. 2008;8:611–623. doi: 10.1017/S0033291707001614. [DOI] [PubMed] [Google Scholar]
- 4.Malouff JM, Thorsteinsson EB, Schutte NS. The efficacy of problem solving therapy in reducing mental and physical health problems: a meta-analysis. Clinical Psychology Review. 2007;7:46–57. doi: 10.1016/j.cpr.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 5.Driessen E, Cuijpers P, de Maat SCM, Abbass AA, de Jonghe F, Dekker JJM. The efficacy of short-term psychodynamic psychotherapy for depression: A meta-analysis. Clinical Psychology Review. 2010;30:25–36. doi: 10.1016/j.cpr.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 6.Cuijpers P, Driessen E, Hollon SD, van Oppen P, Barth J, Andersson G. The efficacy of non-directive supportive therapy for adult depression: A meta-analysis. Clinical Psychology Review. 2012;32:280–291. doi: 10.1016/j.cpr.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Cuijpers P, van Straten A, Smit F. Psychological treatment of late-life depression: A meta-analysis of randomized controlled trials. International Journal of Geriatric Psychiatry. 2006;21:1139–1149. doi: 10.1002/gps.1620. [DOI] [PubMed] [Google Scholar]
- 8.Pinquart M, Duberstein PR, Lyness JM. Effects of psychotherapy and other behavioral interventions on clinically depressed older adults: a meta-analysis. Aging Ment Health. 2007;11:645–657. doi: 10.1080/13607860701529635. [DOI] [PubMed] [Google Scholar]
- 9.Pinquart M, Duberstein PR, Lyness JM. Treatments for later-life depressive conditions: a meta-analytic comparison of pharmacotherapy and psychotherapy. American Journal of Psychiatry. 2006;163:1493–1501. doi: 10.1176/ajp.2006.163.9.1493. [DOI] [PubMed] [Google Scholar]
- 10.Wilson KC, Mottram PG, Vassilas CA. Psychotherapeutic treatments for older depressed people. Cochrane Database of Systematic Reviews. 2008;23(1):CD004853. doi: 10.1002/14651858.CD004853.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Samad Z1, Brealey S, Gilbody S. The effectiveness of behavioural therapy for the treatment of depression in older adults: a meta-analysis. International Journal of Geriatric Psychiatry. 2011;26:1211–1220. doi: 10.1002/gps.2680. [DOI] [PubMed] [Google Scholar]
- 12.Pinquart M, Forstmeier S. Effects of reminiscence interventions on psychosocial outcomes: a meta-analysis. Aging and Mental Health. 2012;16:541–558. doi: 10.1080/13607863.2011.651434. [DOI] [PubMed] [Google Scholar]
- 13.Gould RL, Coulson MC, Howard RJ. Cognitive behavioral therapy for depression in older people: a meta-analysis and meta-regression of randomized controlled trials. Journal of the American Geriatric Society. 2012;60:1817–1830. doi: 10.1111/j.1532-5415.2012.04166.x. [DOI] [PubMed] [Google Scholar]
- 14.Krishna M, Jauhari A, Lepping P, Turner J, Crossley D, Krishnamoorthy A. Is group psychotherapy effective in older adults with depression? A systematic review. International Journal of Geriatric Psychiatry. 2011;26:331–340. doi: 10.1002/gps.2546. [DOI] [PubMed] [Google Scholar]
- 15.Cuijpers P, van Straten A, Warmerdam L, Andersson G. Psychological treatment of depression: A meta-analytic database of randomized studies. BMC Psychiatry. 2008;8:36. doi: 10.1186/1471-244X-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] The Cochrane Collaboration. 2011 Available from www.cochrane-handbook.org.
- 17.Cuijpers P, van Straten A, Andersson G, van Oppen P. Psychotherapy for depression in adults: A meta-analysis of comparative outcome studies. Journal of Consulting and Clinical Psychology. 2008;76:909–922. doi: 10.1037/a0013075. [DOI] [PubMed] [Google Scholar]
- 18.Hedges LV, Olkin I. Statistical methods for meta-analysis. San Diego, CA: Academic Press; 1985. [Google Scholar]
- 19.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Chichester, UK: Wiley; 2009. [Google Scholar]
- 20.Kraemer HC, Kupfer DJ. Size of treatment effects and their importance to clinical research and practice. Biological Psychiatry. 2006;59:990–996. doi: 10.1016/j.biopsych.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 21.Laupacis A, Sackett DL, Roberts RS. An assessment of clinically useful measures of the consequences of treatment. New England Journal of Medicine. 1988;318:1728–1733. doi: 10.1056/NEJM198806303182605. [DOI] [PubMed] [Google Scholar]
- 22.Ioannidis JPA, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. British Medical Journal. 2007;335:914–916. doi: 10.1136/bmj.39343.408449.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Orsini N, Higgins J, Bottai M, Buchan I. Heterogi: Stata module to quantify heterogeneity in a meta-analysis. [Accessed 27 February 2013];2005 http://EconPapers.repec.org/RePEc:boc:bocode:s449201)
- 24.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 25.Alexopoulos GS, Raue P, Arean P. Problem-solving therapy versus supportive therapy in geriatric major depression with executive dysfunction. American Journal of Geriatric Psychiatry. 2003;11:46–52. [PubMed] [Google Scholar]
- 26.Alexopoulos GS, Raue PJ, Kiosses DN, MacKin RS, Kanellopoulos D, McCulloch C, et al. Problem-solving therapy and supportive therapy in older adults with major depression and executive dysfunction: Effect on disability. Archives of General Psychiatry. 2011;68:33–41. doi: 10.1001/archgenpsychiatry.2010.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arean PA, Raue P, Mackin RS, Kanellopoulos D, McCulloch C, Alexopoulos GS. Problem-solving therapy and supportive therapy in older adults with major depression and executive dysfunction. American Journal of Psychiatry. 2010;167:1391–1398. doi: 10.1176/appi.ajp.2010.09091327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arean PA, Perri MG, Nezu AM, Schein RL, Christopher F, Joseph TX. Comparative effectiveness of social problem-solving therapy and reminiscence therapy as treatments for depression in older adults. Journal of Consulting and Clinical Psychology. 1993;61:1003–1010. doi: 10.1037//0022-006x.61.6.1003. [DOI] [PubMed] [Google Scholar]
- 29.Burns A, Banerjee S, Morris J, Woodward Y, Baldwin R, Proctor R, Tarrier N, Pendleton N, Sutherland D, Andrew G, Horan M. Treatment and prevention of depression after surgery for hip fracture in older people: Randomized, controlled trials. Journal of the American Geriatrics Society. 2007;55:75–80. doi: 10.1111/j.1532-5415.2007.01016.x. [DOI] [PubMed] [Google Scholar]
- 30.Chan MF, Ng SE, Tien A, Ho RCM, Thayala J. A randomised controlled study to explore the effect of life story review on depression in older Chinese in Singapore. Health & Social Care in the Community. 2013;21:545–553. doi: 10.1111/hsc.12043. [DOI] [PubMed] [Google Scholar]
- 31.Choi NG, Marti CN, Bruce ML, Hegel MT. Depression in homebound older adults: problem-solving therapy and personal and social resourcefulness. Behavior Therapy. 2013;44:489–500. doi: 10.1016/j.beth.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ekkers W, Korrelboom K, Huijbrechts I, Smits N, Cuijpers P, van der Gaag M. Competitive Memory Training for treating depression and rumination in depressed older adults: A randomized controlled trial. Behaviour Research and Therapy. 2011;49:588–596. doi: 10.1016/j.brat.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 33.Floyd M, Scogin F, McKendree-Smith NL, Floyd DL, Rokke PD. Cognitive Therapy for Depression: A Comparison of Individual Psychotherapy and Bibliotherapy for Depressed Older Adults. Behaviour Modification. 2004;28:297–318. doi: 10.1177/0145445503259284. [DOI] [PubMed] [Google Scholar]
- 34.Fry PS. Structured and unstructured reminiscence training and depression among the elderly. Clinincal Gerontologist. 1983;1:15–37. [Google Scholar]
- 35.Gallagher DE, Thompson LW. Treatment of major depressive disorder in older adult outpatients with brief psychotherapies. Psychotherapy. 1982;19:482–490. [Google Scholar]
- 36.Gitlin LN, Harris LF, McCoy MC, Chernett NL, Pizzi LT, Jutkowitz E, Hess E, Hauck WW. A home-based intervention to reduce depressive symptoms and improve quality of life in older African Americans: a randomized trial. Annals of Internal Medicine. 2013;159:243–252. doi: 10.7326/0003-4819-159-4-201308200-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Haringsma R, Engels GI, Cuijpers P, Spinhoven P. Effectiveness of the Coping With Depression (CWD) course for older adults provided by the community-based mental health care system in the Netherlands: A randomized controlled field trial. International Psychogeriatrics. 2006;18:307–325. doi: 10.1017/S104161020500253X. [DOI] [PubMed] [Google Scholar]
- 38.Hautzinger M, Welz S. Kurz- und lngerfristige wirksamkeit psychologischer interventionen bei depressionen im alter./Short- and long-term efficacy of psychological intervention for depression in older adults. Zeitschrift für Klinische Psychologie und Psychotherapie: Forschung und Praxis. 2007;37:52–60. [Google Scholar]
- 39.Hautzinger M, Welz S. Kognitive Verhaltenstherapie bei Depressionen im Alter: Ergebnisse einer Kontrollierten Vergleichsstudie unter Ambulanten Bedingungen an Depressionen Mittleren Schweregrads. Zeitschrift fur Gerontologie und Geriatrie. 2004;37:427–435. doi: 10.1007/s00391-004-0262-x. [DOI] [PubMed] [Google Scholar]
- 40.Heckman TG, Sikkema KJ, Hansen N, Kochman A, Heh V, Neufeld S. A randomized clinical trial of a coping improvement group intervention for HIV-infected older adults. Journal of Behavioral Medicine. 2011;34:102–111. doi: 10.1007/s10865-010-9292-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Joling KJ, van Hout HP, van't Veer-Tazelaar PJ, van der Horst HE, Cuijpers P, van de Ven PM, et al. How effective is bibliotherapy for very old adults with subthreshold depression? A randomized controlled trial. American Journal of Geriatric Psychiatry. 2011;19:256–265. doi: 10.1097/JGP.0b013e3181ec8859. [DOI] [PubMed] [Google Scholar]
- 42.Kiosses DN, Arean PA, Teri L, Alexopoulos GS. Home-delivered problem adaptation therapy (PATH) for depressed, cognitively impaired, disabled elders: A preliminary study. American Journal of Geriatric Psychiatry. 2010;18:988–998. doi: 10.1097/JGP.0b013e3181d6947d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Korte J, Bohlmeijer ET, Cappeliez P, Smit F, Westerhof GJ. Life review therapy for older adults with moderate depressive symptomatology: a pragmatic randomized controlled trial. Psychological Medicine. 2012;42:1163–1173. doi: 10.1017/S0033291711002042. [DOI] [PubMed] [Google Scholar]
- 44.Laidlaw K, Davidson K, Toner H, Jackson G, Clark S, Law J, Howley M, Bowie G, Connery H, Cross S. A randomised controlled trial of cognitive behaviour therapy vs treatment as usual in the treatment of mild to moderate late life depression. International Journalof Geriatric Psychiatry. 2008;23:843–850. doi: 10.1002/gps.1993. [DOI] [PubMed] [Google Scholar]
- 45.Lamers F, Jonkers CCM, Bosma H, Chavannes NH, Knottnerus JA, van Eijk JT. A minimal psychological intervention in chronically ill elderly patients with depression: a randomized trial. Psychotherapy and Psychosomatics. 2010;79:217–226. doi: 10.1159/000313690. [DOI] [PubMed] [Google Scholar]
- 46.Landreville P, Bissonnette L. Effects of cognitive bibliotherapy for depressed older adults with a disability Clinical Gerontologist. 1997;17:35–55. [Google Scholar]
- 47.Lynch TR, Morse JQ, Mendelson T, Robins CJ. Dialectical behavior therapy for depressed older adults: a randomized pilot study. American Journal of Geriatric Psychiatry. 2003;11:33–45. [PubMed] [Google Scholar]
- 48.Mossey JM, Knott KA, Higgins M, Talerico K. Effectiveness of a psychosocial intervention, interpersonal counseling, for subdysthymic depression in medically ill elderly. Journals of Gerontology Series A, Biological sciences and Medical sciences. 1996;51:M172–178. doi: 10.1093/gerona/51a.4.m172. [DOI] [PubMed] [Google Scholar]
- 49.Pot AM, Bohlmeijer ET, Onrust S, Melenhorst AS, Veerbeek M, De Vries W. The impact of life review on depression in older adults: A randomized controlled trial. International Psychogeriatrics. 2010;22:572–581. doi: 10.1017/S104161020999175X. [DOI] [PubMed] [Google Scholar]
- 50.Preschl B, Maercker A, Wagner B, Forstmeier S, Baños RM, Alcañiz M, Castilla D, Botella C. Life-review therapy with computer supplements for depression in the elderly: A randomized controlled trial. Aging & Mental Health. 2012;16:964–974. doi: 10.1080/13607863.2012.702726. [DOI] [PubMed] [Google Scholar]
- 51.Reynolds CF, Miller MD, Pasternak RE, Frank E, Perel JM, Cornes C, Houck PR, Mazumdar S, Dew MA, Kupfer DJ. Treatment of bereavement-related major depressive episodes in later life: a controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy. American Journal of Psychiatry. 1999;156:202–208. doi: 10.1176/ajp.156.2.202. [DOI] [PubMed] [Google Scholar]
- 52.Scogin F, Hamblin D, Beutler L. Bibliotherapy for depressed older adults: a self-help alternative. Gerontologist. 1987;27:383–387. doi: 10.1093/geront/27.3.383. [DOI] [PubMed] [Google Scholar]
- 53.Scogin F, Jamison C, Gochneaur K. Comparative efficacy of cognitive and behavioral bibliotherapy for mildly and moderately depressed older adults. Journal of Consulting and Clinical Psychology. 1989;57:403–407. doi: 10.1037//0022-006x.57.3.403. [DOI] [PubMed] [Google Scholar]
- 54.Serfaty MA, Haworth D, Blanchard M, Buszewicz M, Murad S, King M. Clinical effectiveness of individual cognitive behavioral therapy for depressed older people in primary care: A randomized controlled trial. Archives of General Psychiatry. 2009;66:1332–1340. doi: 10.1001/archgenpsychiatry.2009.165. [DOI] [PubMed] [Google Scholar]
- 55.Serrano JP, Latorre JM, Gatz M, Montanes J. Life review therapy using autobiographical retrieval practice for older adults with depressive symptomatology. Psychology and aging. 2004;19:270–277. doi: 10.1037/0882-7974.19.2.270. [DOI] [PubMed] [Google Scholar]
- 56.Serrano Selva JP, Postigo JML, Segura LR, Bravo BN, Córcoles MJA, López MN, Trives JJR, Gatz M. Life review therapy using autobiographical retrieval practice for older adults with clinical depression. Psicothema. 2012;24:224–229. [PubMed] [Google Scholar]
- 57.Sirey JA, Bruce ML, Alexopoulos GS. The Treatment Initiation Program: an intervention to improve depression outcomes in older adults. American Journal of Psychiatry. 2005;162:184–186. doi: 10.1176/appi.ajp.162.1.184. [DOI] [PubMed] [Google Scholar]
- 58.Sloane RB, Staples FR, Schneider LS. Interpersonal therapy vs. nortriptyline for depression in the elderly. Clinical and pharmacological studies in psychiatric disorders. Biological psychiatry - new prospects. 1985:344–6. [Google Scholar]
- 59.Snarski M, Scogin F, DiNapoli E, Presnell A, McAlpine J, Marcinak J. The Effects of Behavioral Activation Therapy With Inpatient Geriatric Psychiatry Patients. Behavior Therapy. 2011;42:100–108. doi: 10.1016/j.beth.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 60.Spek V, Nyklicek I, Smits N, Cuijpers P, Riper H, Keyzer J, Pop V. Internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years old: A randomized controlled clinical trial. Psychological Medicine. 2007;37:1797–1806. doi: 10.1017/S0033291707000542. [DOI] [PubMed] [Google Scholar]
- 61.Teri L, Logsdon RG, Uomoto J, McCurry SM. Behavioral treatment of depression in dementia patients: a controlled clinical trial. Journals of Gerontology B Psychological Sciences and Social Sciences. 1997;52:159–166. doi: 10.1093/geronb/52b.4.p159. [DOI] [PubMed] [Google Scholar]
- 62.Thompson LW, Coon DW, Gallagher-Thompson D, Sommer BR, Koin D. Comparison of desipramine and cognitive/behavioral therapy in the treatment of elderly outpatients with mild-to-moderate depression. American Journal of Geriatric Psychiatry. 2001;9:225–240. [PubMed] [Google Scholar]
- 63.Thompson LW, Gallagher D. Efficacy of psychotherapy in the treatment of late-life depression. Advances in Behavior Research and Therapy. 1984;6:127–139. [Google Scholar]
- 64.Thompson LW, Gallagher D, Breckenridge JS. Comparative effectiveness of psychotherapies for depressed elders. Journal of Consulting and Clinical Psychology. 1987;55:385–90. doi: 10.1037//0022-006x.55.3.385. [DOI] [PubMed] [Google Scholar]
- 65.van Schaik A, van Marwijk H, Ader H, van Dyck R, de Haan M, Penninx B, van der Kooij K, van Hout H, Beekman A. Interpersonal psychotherapy for elderly patients in primary care. American Journal of Geriatr Psychiatry. 2006;14:777–786. doi: 10.1097/01.JGP.0000199341.25431.4b. [DOI] [PubMed] [Google Scholar]
- 66.Watt LM, Cappeliez P. Integrative and instrumental reminiscence therapies for depression in older adults: intervention strategies and treatment effectiveness. Aging & Mental Health. 2000;4:166–177. [Google Scholar]
- 67.Williams JW, Barrett J, Oxman T, Frank E, Katon W, Sullivan M, Cornell J, Sengupta A. Treatment of dysthymia and minor depression in primary care: A randomized controlled trial in older adults. Journal of the American Medical Association. 2000;284:1519–1526. doi: 10.1001/jama.284.12.1519. [DOI] [PubMed] [Google Scholar]
- 68.Wuthrich VM, Rapee RM. Randomised controlled trial of group cognitive behavioural therapy for comorbid anxiety and depression in older adults. Behaviour Research and Therapy. 2013;51:779–786. doi: 10.1016/j.brat.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 69.Cuijpers P, van Straten A, Bohlmeijer E, Hollon SD, Andersson G. The effects of psychotherapy for adult depression are overestimated: A meta-analysis of study quality and effect size. Psychological Medicine. 2010;40:211–223. doi: 10.1017/S0033291709006114. [DOI] [PubMed] [Google Scholar]
- 70.Mohr DC, Spring B, Freedland KE, Beckner V, Arean P, Hollon SD, Ockene J, Kaplan R. The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychotherapy and Psychosomatics. 2009;78:275–284. doi: 10.1159/000228248. [DOI] [PubMed] [Google Scholar]
- 71.Mohr DC, Ho J, Hart SL, Baron KG, Berendsen M, Beckner V, Cai X, Cuijpers P, Spring B, Kinsinger SW, Schroder KE, Duffecy J. Control condition design and implementation features in controlled trials: A meta-analysis of trials evaluating psychotherapy for depression. Translational Behavioral Medicine: Practice, Policy and Research. 2014 doi: 10.1007/s13142-014-0262-3. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Barth J, Munder T, Gerger H, Nuesch E, Trelle S, Znoj H, Juni P, Cuijpers P. Comparative efficacy of seven psychotherapeutic interventions for depressed patients: A network meta-analysis. Plos Medicine. 2013;10(5):e1001454. doi: 10.1371/journal.pmed.1001454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cuijpers P, Li J, Hofmann SG, Andersson G. Self-reported versus clinician-rated symptoms of depression as outcome measures in psychotherapy research on depression: A meta-analysis. Clinical Psychology Review. 2010;30:768–778. doi: 10.1016/j.cpr.2010.06.001. [DOI] [PubMed] [Google Scholar]