Abstract
Objective
Recent evidence suggests that the efficacy of smoking cessation pharmacotherapy can vary across patients based on their genotypes. This study tests whether the coding variant rs16969968 in the CHRNA5 nicotinic receptor gene predicts the effects of combination nicotine replacement therapy (cNRT) and varenicline on treatment outcomes.
Method
In two randomized smoking cessation trials comparing cNRT vs. placebo, and varenicline vs. placebo, we used logistic regression to model associations between CHRNA5 rs16969968 and abstinence at end of treatment.
Results
For abstinence at end of treatment, there was an interaction between cNRT and rs16969968 (X2=8.15, df=2, omnibus-p=0.017 for the interaction); individuals with the high-risk AA genotype were more likely to benefit from cNRT. In contrast, varenicline increased abstinence, but its effect did not vary with CHRNA5. However, the genetic effects differed between the placebo control groups across two trials (wald=3.94, df=1, p=0.047), this non-replication can alter the interpretation of pharmacogenetic findings.
Conclusions
Results from two complementary smoking cessation trials demonstrate inconsistent genetic results in the placebo arms. This evidence highlights the need to compare the most effective pharmacotherapies with the same placebo control to establish pharmacogenetic evidence to aid decisions on medication choice for patients trying to quit smoking.
Keywords: smoking cessation, nicotine replacement therapy, varenicline, CHRNA5, pharmacogenetic
1. INTRODUCTION
Smoking is a leading cause of preventable death and disability worldwide (Knopik et al., 2012; Schroeder, 2013; Thun et al., 2013; Whiteford and Baxter, 2013), and smoking cessation greatly diminishes the increased risk of mortality (Jha et al., 2013). Two pharmacotherapies have been shown to be more effective than others for smoking cessation: combination Nicotine Replacement Therapy (cNRT) and varenicline (Fiore and Baker, 2011; Fiore et al., 2008; Piper et al., 2009).
Cessation treatment may be improved via personalized medicine: i.e., using individual genetic markers to maximize efficacy and minimize side effects (McMahon and Insel, 2012; Vaidyanathan, 2012). Smokers vary greatly in the benefit they derive from particular pharmacotherapies, and genotypes may predict their response to a specific pharmacotherapy (Chen et al., 2014; David et al., 2013; Gold and Lerman, 2012; McGeary et al., 2012; Ray et al., 2009; Rose et al., 2010; Uhl et al., 2010). Large scale genome-wide association (GWA) meta-analyses (Liu et al., 2010; TAG, 2010; Thorgeirsson et al., 2010) have confirmed an association between nicotine dependence and the genetic variant rs16969968, which results in an amino acid change (D398N) in the nicotinic receptor gene CHRNA5 (Saccone et al., 2007). CHRNA5 encodes the α5 nicotinic receptor subunit and plays a role in the pharmacodynamic pathway of nicotine dependence (Fowler et al., 2011). Further studies have demonstrated change in the receptor function in response to nicotine agonists given this amino acid change in the a5 nicotinic receptor subunit (Bierut et al., 2008a; Brown et al., 2007). Growing evidence indicates that rs16969968 in CHRNA5 is a predictor for smoking cessation in some circumstances and predicts a delay in successful smoking cessation (Baker et al., 2009; Bergen et al., 2013; Chen et al., 2012, 2015; Freathy et al., 2009; Munafo et al., 2011; Sarginson et al., 2011; Zhu et al., 2014).
Using data from the University of Wisconsin Transdisciplinary Tobacco Use Research Center (UW-TTURC), we have previously shown that CHRNA5 gene modulates clinical response to NRT. Specifically, smokers with the high risk genotypes were less likely to quit while receiving placebo medication (Chen et al., 2012). Whether the effects of these two effective pharmacotherapies (cNRT and varenicline) vary with CHRNA5 is of clinical interest because these results may potentially inform medication choice.
Using data from both the UW-TTURC trial and the varenicline smoking cessation trial by Pfizer (Gonzales et al., 2006; Jorenby et al., 2006), we can examine the effects of CHRNA5 and the two most effective cessation pharmacotherapies (varenicline and cNRT) on smoking abstinence. These two studies differ in type of participants, medication comparator, study duration, and design. However, complementary analyses can be developed for these two research designs. Our primary aim was to obtain and compare evidence on how the genetic effect of CHRNA5 predicts smoking abstinence when subjects receive different treatments.
2. METHODS
2.1 University Of Wisconsin Transdisciplinary Tobacco Use Research Center (Uw-Tturc) Trial
Participants were eligible if they were 18 years of age or older, and smoked 10 or more cigarettes per day (Piper et al., 2009). The University of Wisconsin-Madison IRB approved this trial, and all subjects provided written informed consent. Participants (N = 328) were randomly assigned to either placebo (n = 135) or cNRT (nicotine patch and nicotine lozenge, n =193) for 8 weeks. Additional arms in this trial, not analyzed in this analysis, included nicotine patch, nicotine lozenge, bupropion SR, and bupropion/nicotine lozenge (n = 747). All participants received individual counseling.
The primary outcome was the biochemically confirmed 7-day abstinence at end of treatment (EOT, 8 weeks post-quit). All self-reports of abstinence were confirmed by an expired carbon monoxide (CO) level of less than 10 parts per million (ppm). Individuals with missing data were considered to be smoking. This sample was previously examined by Chen et al. (2012) who reported the interaction of CHRNA5 and medication on smoking abstinence (Chen et al., 2012). This paper presents new analyses targeting the effect of CHRNA5 rs16969968 in the cNRT and placebo arms.
Genotyping was performed by the Center for Inherited Disease Research at Johns Hopkins University using the Illumina Omni2.5 microarray (www.illumina.com). Data cleaning was led by the GENEVA Coordinating Center at the University of Washington.
2.2 Varenicline Randomized Controlled Trial
Participants were eligible if they were 18–75 years of age, smoked 10 or more cigarettes per day, and had < 3 months of abstinence in the past year (Gonzales et al., 2006; Jorenby et al., 2006). This trial was conducted at 19 centers in the US and the IRB at each site approved this trial. All subjects provided written informed consent including genetic analyses. Participants (N=790) were randomly assigned to either placebo (n = 376) or varenicline (n = 414) for 12 weeks. An additional study arm not included in this analysis was bupropion (n = 345). All participants received individual counseling.
The primary endpoint was 4-week continuous abstinence for the last 4 weeks of treatment (weeks 9–12). Abstinence at each visit was defined as a self-report of no smoking since the previous visit, confirmed by an expired CO level of 10 ppm or less. In the case of missed visits, if at the next visit there was a self-report of no smoking and no use of other tobacco products, a status of not smoking was imputed. This sample was previously examined by King et al who reported association of multiple nicotinic receptor genes including CHRNA5 (reported variant rs518425 has low correlation with rs16969968) and abstinence in the varenicline arm (King et al., 2012). This paper presents new analyses targeting the comparison of cNRT vs. placebo arms focusing on the CHRNA5 rs16969968 genotype.
Genotyping was performed on the Illumina Golden Gate platform, ABI Taqman and SNPlex methods. Genotyping call rates and Hardy-Weinberg equilibrium were previously published (King et al., 2012).
2.3 Analysis
The primary phenotype was smoking abstinence at EOT, and the primary predictor was the rs16969968 genotype. We used logistic regression models. Subjects of European ancestry were examined. The following covariates were tested: gender, age, cigarettes per day (in 4 levels: < 10, 11–20, 21–30, ≥31), and treatment (placebo vs. cNRT in the UW-TTURC trial; placebo vs. varenicline in the varenicline trial). Age did not differ across treatment arms and was not significantly associated with cessation outcomes, so it was not included in the final models.
3. RESULTS
3.1 CHRNA5 and pharmacotherapy are associated with abstinence
3.1.1 UW-TTURC Trial (N=328)
Table S11 shows demographics and genotype frequencies. 48.5% of participants were abstinent at EOT (8 weeks post-quit). Receiving cNRT, compared to placebo, increased abstinence (60.1% in cNRT n =193; 31.9% in placebo n =135; OR=3.17, 95% CI=1.99–5.05, df=1, p= 8.1×10−6).
Consistent with our previous findings, the association of rs16969968 genotypes with abstinence depended upon treatment condition. Rs16969968 genotypes were associated with abstinence in the placebo group (X2=6.54, df=2, p=0.038), but not in the cNRT group (X2=2.55, df=2, p=0.28). The effect of cNRT differed across genotype groups (GG: OR=1.57, 95% CI=0.79–3.16, df=1, p= 0.20; GA: OR=4.45, 95% CI=2.21–8.98, df=1, p= 3.1×10−5; AA: OR=14.7, 95% CI=2.57–84.3, df=1, p= 0.0025). These results reflect a significant interaction between treatment (placebo versus cNRT) and rs16969968 genotypes (Table 1; Figure 1).
Table 1.
CHRNA5 rs16969968 and the Medication Effect on Abstinence at End-of-Treatment
| UW-TTURC Trial (N=328) | Abstinence at End of Treatment | ||
|---|---|---|---|
|
| |||
| Odds Ratio | 95% C.I. | P-value | |
|
|
|||
| Genotypes (rs16969968) | |||
| GG | reference | ||
| GA | 0.42 | (0.19, 0.90) | 0.025 |
| AA | 0.23 | (0.05, 1.15) | 0.073 |
| Treatment Status | |||
| Placebo | reference | ||
| Combination NRT (cNRT) | 1.57 | (0.78, 3.13) | 0.21 |
| Interaction of Genotypes and Intervention | (a) | ||
| GG*cNRT | reference | ||
| GA*cNRT | 2.92 | (1.09, 7.82) | 0.033 |
| AA*cNRT | 9.79 | (1.51, 63.6) | 0.017 |
|
| |||
| Varenicline Trial (N=790) | |||
|
| |||
| Genotypes (rs16969968) | |||
| GG | reference | ||
| GA | 0.82 | (0.59, 1.13) | 0.23 |
| AA | 0.75 | (0.45, 1.24) | 0.26 |
| Treatment Status(b) | |||
| Placebo | reference | ||
| Varenicline | 4.18 | (3.05, 5.72) | 5.5*10−19 |
All models were adjusted for gender. C.I.=Confidence Interval
chi squared=8.15, df=2, omnibus p=0.017 for the overall interaction effect.
test of gene-treatment interaction is not significant with chi square=0.32, df=2, omnibus p=0.85.
Figure 1.
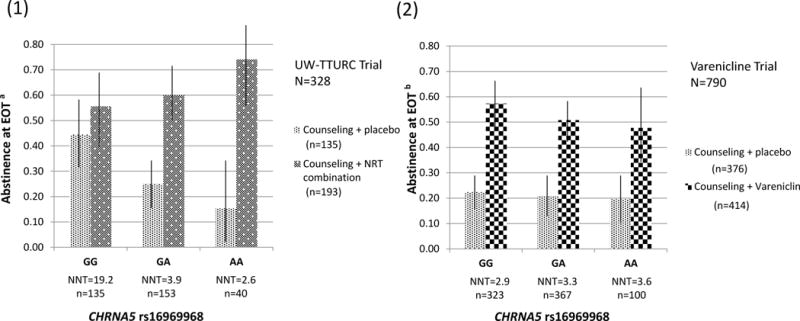
- UW-TTURC trial shows that combination NRT increases abstinence EOT in genotypes GA and AA, but not GG. Varenicline trial shows that varenicline increases abstinence across genotypes.
- Genotypic effects in the placebo groups differ between these two trials.
aUW-TTURC trial: Combination NRT increases abstinence(OR=3.17, 95% CI=1.99–5.05, df=1, p= 8.1×10−6). A significant interaction between treatment (placebo versus combination NRT) and rs16969968 genotypes (X2=8.15, df=2, omnibus-p=0.017 for the interaction).
bVarenicline trial: Varenicline increases abstinence (OR=4.18, 95% CI=3.05–5.72, df=1, p=5.5×10−19).
The CHRNA5 rs16969968 genotypic effects on abstinence in the placebo groups differ significantly between the two studies (rs16969968*Study Interaction Wald=3.94, df=1, p=0.047). There is a genotypic effect in the UW-TTURC trial placebo arm, but not in the varenicline trial placebo arm.
NNT: number needed to treat
We found a similar pharmacogenetic interaction result after adjusting for cigarettes per day (CPD; Table S32). We identified the utility of CHRNA5 genotypes in predicting response to cNRT (Fig 1A): the clinical impact of this interaction was exemplified by the number needed to treat (NNT), which varied with genotypes. Smokers with AA and GA genotypes were more likely to respond to cNRT (NNT=2.6 and 3.9, respectively). Conversely, smokers with the GG genotype received less benefit from cNRT (NNT=19.2).
3.1.2 Varenicline Trial (N=790)
In the trial, 38.0% of participants had 4-week continuous abstinence at EOT (weeks 9–12 post-quit). Receiving varenicline, compared to placebo, increased abstinence (53.1% in varenicline arm n=414; 21.3% in placebo arm n=376; OR=4.18, 95% CI=3.05–5.72, df=1, p= 5.5×10−19). Varenicline was associated with abstinence across all three genotype groups (GG: OR=4.65, CI=2.85–7.57, p= 7.0×10−10; GA: OR=3.89, 95% CI=2.44–6.20, df=1, p= 1.0×10−8; AA: OR=3.80, 95% CI=1.56–9.27, df=1, p= 0.0033).
Unlike the UW-TTURC trial results, rs16969968 genotype was not associated with abstinence in the placebo group or the varenicline group (Table 1; Figure 1), and there is no pharmacogenetic interaction. Given the sample size (n=403 in placebo; n=428 in varenicline), 2-sided α of 0.05, and baseline abstinence rate of 0.21, we had power to detect a genotypic association with an OR of 0.66 or lower. In the varenicline trial, NNT for varenicline did not vary much by genotype (NNT=3.6, 3.3, 2.9 for smokers with AA, GA GG genotypes, respectively).
3.2. Placebo arms differ between trials
Both trials include a placebo arm and the genotypic associations in the placebo arms significantly differed between these two trials (interaction wald=3.94, df=1, p=0.047). In the UW-TTURC trial, CHRNA5 rs16969968 genotypes were associated with abstinence at EOT in the placebo group (X2=6.54, df=2, p=0.038). Unlike the UW-TTURC trial results, rs16969968 genotype was not associated with abstinence at EOT in the placebo group (X2=0.21, df=2, p=0.90) in the varenicline trial.
4. DISCUSSION
Our findings demonstrate the significant difference in the CHRNA5 genetic effect on abstinence at end of treatment in the placebo groups in two cessation trials. This difference across the two trials is likely due to heterogeneity in study design such as ascertainment, placebo conditions, and counseling effects. This difference in placebo groups substantially alters the interpretation and comparison of pharmacogenetic effects of two highly effective smoking cessation pharmacotherapies (cNRT and varenicline). Comparison of results from these two important trials highlights the need for a head-to-head comparison trial with a uniform placebo control to compare the pharmacogenetic effects related to both pharmacotherapies. No randomized trial has yet compared the efficacy of varenicline and cNRT with the same placebo control (Rigotti, 2013). Thus, the current results are intriguing and suggest caution in extrapolating research findings into clinical practice.
Combination NRT (cNRT) and varenicline have been identified as the two most effective smoking cessation medications (Cahill et al., 2013; Fiore et al., 2008). In the UW-TTURC trial, the efficacy of cNRT varied with rs16969968 genotypes, representing a pharmacogenetic interaction. In contrast, in the varenicline trial, we found that the efficacy of varenicline did not vary with CHRNA5 genotypes, which then leads to the conclusion that all subjects respond to varenicline regardless of CHRNA5 rs16969968 genotype. These results are based on retrospective analyses of existing trials testing different medications, using dissimilar designs, and showing markedly different clinical success in the placebo arms (e.g., 44% vs. 22% abstinence for GG genotypes in the UW-TTURC and varenicline trials), all of which suggest caution in the interpretation of these pharmacogenetic effects as well as raise the question about why the placebo responses are differing significantly between the two studies.
The results of this study should be interpreted in the context of several limitations. First, the power was limited in specific treatment or placebo arms due to sample sizes. Thus, the observed association or lack of association between CHRNA5 and smoking cessation should be considered preliminary. Second, the genetic risk for cessation cannot be directly compared across the different pharmacotherapy conditions (cNRT vs. varenicline) due to dissimilar study designs. Third, this work studies only one gene and it is clear that multiple genes contribute to smoking cessation success. Finally, this study only included subjects of European descent.
In summary, this work highlights the challenges and needed evidence to translate genetic research findings in the area of precision medicine. Using two complementary trials, the genetic effect on placebo response differs significantly between the two trials and this difference then influences the interpretation of pharmacogenetic response of smoking cessation. If the results in the placebo groups were reversed in the two trials, a completely different interpretation of the pharmacogenetic results would follow. This finding highlights the importance of having a head-to-head comparison with the same placebo control in pharmacogenetic research in order to achieve the goal of precise smoking cessation treatments (Rutter, 2006).
Supplementary Material
Highlights.
Comparisons of smoking cessation trials demonstrate inconsistent genetic results.
A placebo control arm is important to determine the pharmacogenetic effect.
Individuals with risk genotypes have difficulty quitting smoking without treatment.
This increased risk may be ameliorated by effective pharmacological treatment.
Acknowledgments
The Wisconsin State Laboratory of Hygiene provided considerable technical assistance in this research effort. Glaxo Wellcome provided bupropion at no cost in the UW-TTURC clinical trial. The authors thank John Budde and Nick McKenna for their technical assistance with Open Array platform genotyping, Joseph Mullaney for his assistance in preparing the data, Sherri Fisher and Nina Smock for their assistance in project coordination and editing/preparing the manuscript.
ROLE OF FUNDING SOURCE
This research was supported by NIH grants P01 CA089392 (LJB), P30 CA036583 (LJB), P50 CA84724 (TBB), and K05 CA139871 (TBB) from the National Cancer Institute, P50 DA19706 (TBB), K02 DA021237 (LJB), R01 DA036583 (LJB), R01 DA025888 (LJB), K08 DA030398 (LSC), and R01 DA038076 (LSC) from the National Institute on Drug Abuse, U01 HG004422 (LJB) from the National Human Genome Research Institute, sub-award KL2 RR024994 (LSC) from the National Center for Research Resources, and from The Alvin J. Siteman Cancer Center (SCC) at Washington University School of Medicine (WUSM) and Barnes-Jewish Hospital (BJH) cancer center support grant P30 CA091842 (LJB). The content is solely the responsibility of the authors and does not necessarily represent the views of the National Institutes of Health. Genotyping services for the UW-TTURC sample were provided by the Center for Inherited Disease Research (CIDR). Funding support for CIDR was provided by NIH grant U01 HG004438 and NIH contract HHSN268200782096C to The Johns Hopkins University. Assistance with genotype cleaning was provided by the Gene Environment Association Studies (GENEVA) Coordinating Center (U01 HG004446). Pfizer conducted the varenicline Trial and supported an Investigator-initiated data use agreement for this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
CONFLICT OF INTEREST
Laura J. Bierut is listed as an inventor on issued U.S. Patent 8,080,371, “Markers for Addiction” covering the use of certain SNPs in determining the diagnosis, prognosis, and treatment of addiction. Nancy Saccone’s spouse is also listed as an inventor on the above issued U.S. Patent 8,080,371. Robert M. Carney or a member of his family owns stock in Pfizer, Inc. Douglas Jorenby has received research support from Pfizer. All other authors declare no potential conflict of interest.
CONTRIBUTORS
Authors Li-Shiun Chen, Timothy Baker, Douglas Jorenby, Megan Piper, and Laura Bierut designed the study. Authors Li-Shiun Chen, Timothy Baker, and Laura Bierut wrote summaries of previous related work. Authors Douglas Jorenby, Megan Piper, Nancy Saccone, Eric Johnson, Naomi Breslau, Dorothy Hatsukami, and Robert Carney advised on the analysis designs and plans. Author Li-Shiun Chen undertook the statistical analysis, and authors Li-Shiun Chen, Timothy Baker, and Laura Bierut wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
References
- Baker TB, Weiss RB, Bolt D, von Niederhausern A, Fiore MC, Dunn DM, Piper ME, Matsunami N, Smith SS, Coon H, McMahon WM, Scholand MB, Singh N, Hoidal JR, Kim SY, Leppert MF, Cannon DS. Human neuronal acetylcholine receptor A5-A3-B4 haplotypes are associated with multiple nicotine dependence phenotypes. Nicotine Tob Res. 2009;11:785–796. doi: 10.1093/ntr/ntp064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergen AW, Javitz HS, Krasnow R, Nishita D, Michel M, Conti DV, Liu J, Lee W, Edlund CK, Hall S, Kwok PY, Benowitz NL, Baker TB, Tyndale RF, Lerman C, Swan GE. Nicotinic acetylcholine receptor variation and response to smoking cessation therapies. Pharmacogenet Genomics. 2013;23:94–103. doi: 10.1097/FPC.0b013e32835cdabd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierut LJ, Stitzel JA, Wang JC, Hinrichs AL, Grucza RA, Xuei X, Saccone NL, Saccone SF, Bertelsen S, Fox L, Horton WJ, Breslau N, Budde J, Cloninger CR, Dick DM, Foroud T, Hatsukami D, Hesselbrock V, Johnson EO, Kramer J, Kuperman S, Madden PA, Mayo K, Nurnberger J, Jr, Pomerleau O, Porjesz B, Reyes O, Schuckit M, Swan G, Tischfield JA, Edenberg HJ, Rice JP, Goate AM. Variants in nicotinic receptors and risk for nicotine dependence. Am J Psychiatry. 2008a;165:1163–1171. doi: 10.1176/appi.ajp.2008.07111711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RW, Collins AC, Lindstrom JM, Whiteaker P. Nicotinic alpha5 subunit deletion locally reduces high-affinity agonist activation without altering nicotinic receptor numbers. J Neurochem. 2007;103:204–215. doi: 10.1111/j.1471-4159.2007.04700.x. [DOI] [PubMed] [Google Scholar]
- Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database Syst Rev. 2013;5:CD009329. doi: 10.1002/14651858.CD009329.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LS, Baker TB, Piper ME, Breslau N, Cannon DS, Doheny KF, Gogarten SM, Johnson EO, Saccone NL, Wang JC, Weiss RB, Goate AM, Bierut LJ. Interplay of genetic risk factors (CHRNA5-CHRNA3-CHRNB4) and cessation treatments in smoking cessation success. Am J Psychiatry. 2012;169:735–742. doi: 10.1176/appi.ajp.2012.11101545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LS, Bloom JA, Baker TB, Smith SS, Piper ME, Martinez M, Saccone NL, Hatsukami D, Goate AM, Bierut LJ. Pharmacotherapy effects on smoking cessation vary with nicotine metabolism gene (CYP2A6) Addiction. 2014;109:128–137. doi: 10.1111/add.12353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LS, Hung RJ, Baker T, Horton A, Culverhouse R, Saccone N, Cheng I, Deng B, Han Y, Hansen HM, Horsman J, Kim C, Lutz S, Rosenberger A, Aben KK, Andrew AS, Breslau N, Chang SC, Dieffenbach AK, Dienemann H, Frederiksen B, Han J, Hatsukami DK, Johnson EO, Pande M, Wrensch MR, McLaughlin J, Skaug V, van der Heijden HF, Wampfler J, Wenzlaff A, Woll P, Zienolddiny S, Bickeboller H, Brenner H, Duell EJ, Haugen A, Heinrich J, Hokanson JE, Hunter DJ, Kiemeney LA, Lazarus P, Le Marchand L, Liu G, Mayordomo J, Risch A, Schwartz AG, Teare D, Wu X, Wiencke JK, Yang P, Zhang ZF, Spitz MR, Kraft P, Amos CI, Bierut LJ. chrna5 risk variant predicts delayed smoking cessation and earlier lung cancer diagnosis-a meta-analysis. J Natl Cancer Inst. 2015 doi: 10.1093/jnci/djv100. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David SP, Strong DR, Leventhal AM, Lancaster MA, McGeary JE, Munafo MR, Bergen AW, Swan GE, Benowitz NL, Tyndale RF, Conti DV, Brown RA, Lerman C, Niaura R. Influence of a dopamine pathway additive genetic efficacy score on smoking cessation: results from two randomized clinical trials of bupropion. Addiction. 2013;108:2202–2211. doi: 10.1111/add.12325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Baker TB. Clinical practice. Treating smokers in the health care setting. N Engl J Med. 2011;365:1222–1231. doi: 10.1056/NEJMcp1101512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, TB B . Treating Tobacco Use And Dependence: 2008 Update. U.S. Department Of Health And Human Services, U.S. Public Health Service; Rockville, MD: 2008. [Google Scholar]
- Fowler CD, Lu Q, Johnson PM, Marks MJ, Kenny PJ. Habenular alpha5 nicotinic receptor subunit signalling controls nicotine intake. Nature. 2011;471:597–601. doi: 10.1038/nature09797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freathy RM, Ring SM, Shields B, Galobardes B, Knight B, Weedon MN, Smith GD, Frayling TM, Hattersley AT. A common genetic variant in the 15q24 nicotinic acetylcholine receptor gene cluster (CHRNA5-CHRNA3-CHRNB4) is associated with a reduced ability of women to quit smoking in pregnancy. Hum Mol Genet. 2009;18:2922–2927. doi: 10.1093/hmg/ddp216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold AB, Lerman C. Pharmacogenetics of smoking cessation: role of nicotine target and metabolism genes. Hum Genet. 2012 doi: 10.1007/s00439-012-1143-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales D, Rennard SI, Nides M, Oncken C, Azoulay S, Billing CB, Watsky EJ, Gong J, Williams KE, Reeves KR. Varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs sustained-release bupropion and placebo for smoking cessation: a randomized controlled trial. JAMA. 2006;296:47–55. doi: 10.1001/jama.296.1.47. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, McAfee T, Peto R. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368:341–350. doi: 10.1056/NEJMsa1211128. [DOI] [PubMed] [Google Scholar]
- Jorenby DE, Hays JT, Rigotti NA, Azoulay S, Watsky EJ, Williams KE, Billing CB, Gong J, Reeves KR. Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA. 2006;296:56–63. doi: 10.1001/jama.296.1.56. [DOI] [PubMed] [Google Scholar]
- King DP, Paciga S, Pickering E, Benowitz NL, Bierut LJ, Conti DV, Kaprio J, Lerman C, Park PW. Smoking cessation pharmacogenetics: analysis of varenicline and bupropion in placebo-controlled clinical trials. Neuropsychopharmacology. 2012;37:641–650. doi: 10.1038/npp.2011.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knopik VS, Maccani MA, Francazio S, McGeary JE. The epigenetics of maternal cigarette smoking during pregnancy and effects on child development. Dev Psychopathol. 2012;24:1377–1390. doi: 10.1017/S0954579412000776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JZ, Tozzi F, Waterworth DM, Pillai SG, Muglia P, Middleton L, Berrettini W, Knouff CW, Yuan X, Waeber G, Vollenweider P, Preisig M, Wareham NJ, Zhao JH, Loos RJ, Barroso I, Khaw KT, Grundy S, Barter P, Mahley R, Kesaniemi A, McPherson R, Vincent JB, Strauss J, Kennedy JL, Farmer A, McGuffin P, Day R, Matthews K, Bakke P, Gulsvik A, Lucae S, Ising M, Brueckl T, Horstmann S, Wichmann HE, Rawal R, Dahmen N, Lamina C, Polasek O, Zgaga L, Huffman J, Campbell S, Kooner J, Chambers JC, Burnett MS, Devaney JM, Pichard AD, Kent KM, Satler L, Lindsay JM, Waksman R, Epstein S, Wilson JF, Wild SH, Campbell H, Vitart V, Reilly MP, Li M, Qu L, Wilensky R, Matthai W, Hakonarson HH, Rader DJ, Franke A, Wittig M, Schafer A, Uda M, Terracciano A, Xiao X, Busonero F, Scheet P, Schlessinger D, St Clair D, Rujescu D, Abecasis GR, Grabe HJ, Teumer A, Volzke H, Petersmann A, John U, Rudan I, Hayward C, Wright AF, Kolcic I, Wright BJ, Thompson JR, Balmforth AJ, Hall AS, Samani NJ, Anderson CA, Ahmad T, Mathew CG, Parkes M, Satsangi J, Caulfield M, Munroe PB, Farrall M, Dominiczak A, Worthington J, Thomson W, Eyre S, Barton A, Mooser V, Francks C, Marchini J. Meta-analysis and imputation refines the association of 15q25 with smoking quantity. Nat Genet. 2010;42:436–440. doi: 10.1038/ng.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGeary JE, Knopik VS, Hayes JE, Palmer RH, Monti PM, Kalman D. Predictors of relapse in a bupropion trial for smoking cessation in recently-abstinent alcoholics: preliminary results using an aggregate genetic risk score. Subst Abuse. 2012;6:107–114. doi: 10.4137/SART.S8866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon FJ, Insel TR. Pharmacogenomics and personalized medicine in neuropsychiatry. Neuron. 2012;74:773–776. doi: 10.1016/j.neuron.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munafo MR, Johnstone EC, Walther D, Uhl GR, Murphy MF, Aveyard P. CHRNA3 rs1051730 genotype and short-term smoking cessation. Nicotine Tob Res. 2011;13:982–988. doi: 10.1093/ntr/ntr106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, Smith SS, Schlam TR, Fiore MC, Jorenby DE, Fraser D, Baker TB. A randomized placebo-controlled clinical trial of 5 smoking cessation pharmacotherapies. Arch Gen Psychiatry. 2009;66:1253–1262. doi: 10.1001/archgenpsychiatry.2009.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray R, Tyndale RF, Lerman C. Nicotine dependence pharmacogenetics: role of genetic variation in nicotine-metabolizing enzymes. J Neurogenet. 2009;23:252–261. doi: 10.1080/01677060802572887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigotti NA. Smoking cessation in patients with respiratory disease: existing treatments and future directions. Lancet Respir Med. 2013;1:241–250. doi: 10.1016/S2213-2600(13)70063-8. [DOI] [PubMed] [Google Scholar]
- Rose JE, Behm FM, Drgon T, Johnson C, Uhl GR. Personalized smoking cessation: interactions between nicotine dose, dependence and quit-success genotype score. Mol Med. 2010;16:247–253. doi: 10.2119/molmed.2009.00159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter JL. Symbiotic relationship of pharmacogenetics and drugs of abuse. AAPS J. 2006;8:E174–184. doi: 10.1208/aapsj080121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saccone SF, Hinrichs AL, Saccone NL, Chase GA, Konvicka K, Madden PA, Breslau N, Johnson EO, Hatsukami D, Pomerleau O, Swan GE, Goate AM, Rutter J, Bertelsen S, Fox L, Fugman D, Martin NG, Montgomery GW, Wang JC, Ballinger DG, Rice JP, Bierut LJ. Cholinergic nicotinic receptor genes implicated in a nicotine dependence association study targeting 348 candidate genes with 3713 SNPs. Hum Mol Genet. 2007;16:36–49. doi: 10.1093/hmg/ddl438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarginson JE, Killen JD, Lazzeroni LC, Fortmann SP, Ryan HS, Schatzberg AF, Murphy GM., Jr Markers in the 15q24 nicotinic receptor subunit gene cluster (CHRNA5-A3-B4) predict severity of nicotine addiction and response to smoking cessation therapy. Am J Med Genet B Neuropsychiatr Genet. 2011;156B:275–284. doi: 10.1002/ajmg.b.31155. [DOI] [PubMed] [Google Scholar]
- Schroeder SA. New evidence that cigarette smoking remains the most important health hazard. N Engl J Med. 2013;368:389–390. doi: 10.1056/NEJMe1213751. [DOI] [PubMed] [Google Scholar]
- TAG. Genome-wide meta-analyses identify multiple loci associated with smoking behavior. Nat Genet. 2010;42:441–447. doi: 10.1038/ng.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas KH, Martin RM, Knipe DW, Higgins JP, Gunnell D. Risk of neuropsychiatric adverse events associated with varenicline: systematic review and meta-analysis. BMJ. 2015;350:h1109. doi: 10.1136/bmj.h1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorgeirsson TE, Gudbjartsson DF, Surakka I, Vink JM, Amin N, Geller F, Sulem P, Rafnar T, Esko T, Walter S, Gieger C, Rawal R, Mangino M, Prokopenko I, Magi R, Keskitalo K, Gudjonsdottir IH, Gretarsdottir S, Stefansson H, Thompson JR, Aulchenko YS, Nelis M, Aben KK, den Heijer M, Dirksen A, Ashraf H, Soranzo N, Valdes AM, Steves C, Uitterlinden AG, Hofman A, Tonjes A, Kovacs P, Hottenga JJ, Willemsen G, Vogelzangs N, Doring A, Dahmen N, Nitz B, Pergadia ML, Saez B, De Diego V, Lezcano V, Garcia-Prats MD, Ripatti S, Perola M, Kettunen J, Hartikainen AL, Pouta A, Laitinen J, Isohanni M, Huei-Yi S, Allen M, Krestyaninova M, Hall AS, Jones GT, van Rij AM, Mueller T, Dieplinger B, Haltmayer M, Jonsson S, Matthiasson SE, Oskarsson H, Tyrfingsson T, Kiemeney LA, Mayordomo JI, Lindholt JS, Pedersen JH, Franklin WA, Wolf H, Montgomery GW, Heath AC, Martin NG, Madden PA, Giegling I, Rujescu D, Jarvelin MR, Salomaa V, Stumvoll M, Spector TD, Wichmann HE, Metspalu A, Samani NJ, Penninx BW, Oostra BA, Boomsma DI, Tiemeier H, van Duijn CM, Kaprio J, Gulcher JR, McCarthy MI, Peltonen L, Thorsteinsdottir U, Stefansson K. Sequence variants at CHRNB3-CHRNA6 and CYP2A6 affect smoking behavior. Nat Genet. 2010;42:448–453. doi: 10.1038/ng.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thun MJ, Carter BD, Feskanich D, Freedman ND, Prentice R, Lopez AD, Hartge P, Gapstur SM. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368:351–364. doi: 10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhl GR, Drgon T, Johnson C, Ramoni MF, Behm FM, Rose JE. Genome-wide association for smoking cessation success in a trial of precessation nicotine replacement. Mol Med. 2010a;16:513–526. doi: 10.2119/molmed.2010.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaidyanathan G. Redefining clinical trials: the age of personalized medicine. Cell. 2012;148:1079–1080. doi: 10.1016/j.cell.2012.02.041. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Baxter AJ. The Global Burden of Disease 2010 Study: what does it tell us about mental disorders in Latin America? Rev Bras Psiquiatr. 2013;35:111–112. doi: 10.1590/1516-4446-2012-3502. [DOI] [PubMed] [Google Scholar]
- Zhu AZ, Zhou Q, Cox LS, David SP, Ahluwalia JS, Benowitz NL, Tyndale RF. Association of CHRNA5-A3-B4 SNP rs2036527 with smoking cessation therapy response in african-american smokers. Clin Pharmacol Ther. 2014;96:256–265. doi: 10.1038/clpt.2014.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


