Abstract
Background:
More than 80 percent of the China’s population is located in the rural areas, 95 percent of which use coal, wood etc for cooking and heating. Limited by data availability, the association between household solid fuels and cardiovascular diseases (CVDs) in China’s rural areas is ignored in prior studies.
Methods:
This cross sectional study was conducted from 2010–2012 and carried out on rural population aging 20–80 yr, comprised of 13877 participants from eighteen villages. Self-report questionnaire data were collected. Each outcome represents whether the participant has a kind of CVDs or not and it is reported in participants’ questionnaire. Then the collected data is analyzed by logistic regression models with odds ratios (OR) and 95 percent confidence interval.
Results:
After adjusting for potential confounders, the use of household solid fuels was significantly associated with an increased risk for hypertension (OR 1.751), CHD (OR 2.251), stroke (OR 1.642), diabetes (OR 1.975) and dyslipidemia (OR 1.185). Residents with the highest tertile of the duration of household solid fuel exposure had an increased odd of hypertension (OR 1.651), stroke (OR 1.812), diabetes (OR 2.891) and dyslipidemia (OR 1.756) compared with those in the lowest tertile of the duration of solid fuel exposure.
Conclusion:
Indoor pollution exposure from household solid fuels combustion may be a positive risk factor for CVDs in the perspectives of China’s rural population. Our findings should be corroborated in longitudinal studies.
Keywords: Household solid fuels, Rural areas, Cardiovascular diseases, China
Introduction
Half of the world still uses solid biomass or coal fuels for the basic cooking and heating (1, 2). These fuels are often burned inside poorly ventilated spaced with simple stoves that release substantial pollutants such as respirable particulate matter (PM). Indoor air pollution (IAP) from solid fuel use in developing countries is estimated by the WHO to be the eighth leading health risk worldwide, leading to such serious illnesses as acute lower respiratory infections (ALRI) (3). IAP from solid fuel use is estimated to be responsible for more than 1.6 million annual deaths and nearly 3% of the global burden of disease (4–6).
More than 70% of China’s population lives in rural areas, where most of the people still use solid fuels for cooking and heating. Especially, biomass (wood, crop residues) and coal are the primary fuels for almost 98% of the rural population in Jingle County, Shanxi Province, China. Most of the county is low-income remote region. These fuels are often burned inside the poorly ventilated spaces with thermally inefficient stoves usually emitting a complex pollutant mixture of particulate matter (PM), polycyclic aromatic hydrocarbons (PAHs), heavy metals and many other organic pollutants which have been linked to (CVDs) (7–9). Recently, the scientific statement from the American Heart Association (AHA) shows PM exposure can trigger acute cardiovascular events and accelerate chronic CVDs. In China, CVDs is considered to increase considerably, and in the future, blood pressure, diabetes, total cholesterol, and body mass index may drive the CVDs epidemic during the next 20 years (1, 4, 10–16).
The effects of indoor air pollution using coal on chronic obstructive pulmonary disease and lung cancer in adults and pneumonia in children are well documented (17, 18). Human experiments and observational studies suggest that indoor air pollution exposure could raise systolic blood pressure and diastolic blood pressure (13, 19, 20), however some studies did not attribute these diseases outcomes to household use of solid fuels (21, 22).
Although previous studies have conducted research on the relationship between indoor air pollution generated by solid fuels use and body health, there are still some issues that need to be discussed. First, CVDs have always been the leading cause of death worldwide (23–26), especially in rural areas, but the impact of solid fuels use on CVDs is neglected. Second, most prior studies are confined to urban areas; systematic studies on association between household fuels use and CVDs in rural areas are rarely seen. However, China is a large agricultural country, and rural areas account for a large proportion in the population and energy consumption. Third, most prior studies analyzed the impact of the fuels use on health based limited data and the sample size normally less than 5000. Such sample data does not have a good representativeness.
This paper attempts to contribute to the research on the CVDs and its factors. On the one hand, our work is helpful for understanding the influence of household fuel use on human health, which is really an important issue for people. On the other hand, our work can provide decision support for energy transformation and health policy in the current background of China energy consumption structure.
The cardiovascular diseases mainly are defined as atherosclerotic heart disease, cerebrovascular disease, hypertension, peripheral arterial disease, rheumatic heart disease, diabetes and dyslipidemia, etc. (27). In this study, we examined whether household solid fuel exposure in rural areas from cooking and heating is in relationship with adverse CVDs, focusing on particularly hypertension, coronary heart disease (CHD), stroke, diabetes and dyslipidemia in the rural areas.
Materials and Methods
Study location and population
The study took place in loess plateau, Jingle County in the northwestern of Shanxi province, China (N 38°3′, E 110°14′). Most of the participants were peasants in rural villages and have similar socioeconomic background and dietary habits. All households used coal and biomass for cooking and heating. Ninety-six percent of the residents used biomass and coal as their primary cooking fuels. Ninety-eight percent of residents commonly use coal block, wood and biomass for heating during winter. They scarcely did use biogas, electricity and liquefied petroleum gas.
Study design and sampling procedure
The research project is a regional survey conducted by the Jingle County People’s Hospital (JCPH) to collect cardiovascular disease and household solid fuel usage situation of the population in remote rural areas. This regionally representative, cross-sectional survey recruited the subjects using a multistage, systematic sampling design.
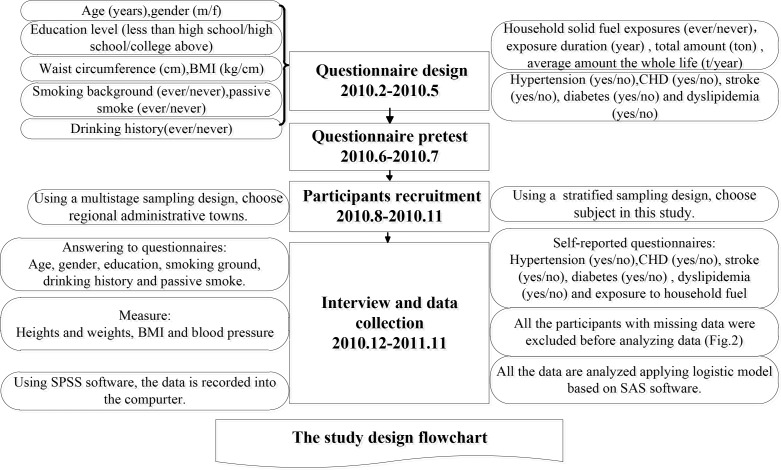
JCPH and we designed questionnaires in February 2010 to May 2010, and test the draft questionnaire in June 2010 to July 2010 (Fig. 1). There are 145320 rural inhabitants in Jingle county of China. We consider five percent of this population for our sample in our study, which was calculated as 7266 individuals. To enhance the power of study, we increased sample size up to 14100 individuals. Using a multistage sampling method, a random sample of 14100 individuals was selected randomly. At the first stage, six regional administrative towns were chosen as primary sampling units from all the fourteen administrative towns. Secondly, 3 villages were sampled from each town based on gender and age using a stratified multistage probability sampling method. Thirdly, 700∼800 individuals were selected based on simple random sampling.
Fig. 1:
The study design flowchart
JCPH recruited 6,600 men and 7,500 women from August 2010 to November 2010 from 18 rural villages based on sampling procedure following eligible criteria: above age 20 years with no restrictions with respect to prior health history. The number of residents in the area during the study period determined the sample size. Briefly, in this study, to investigate the household solid fuel in rural village, Jingle County at a confidence level of 95%, a sampling error of plus or minus three percent and design effect of 2, 14100 individuals were enough to study association between household solid fuel and CVDs. Of the 14,100 accounting for about 10% of the total rural population, 13,877 (98.4%) subjects with age >=20 years were provided with written informed consent to participate in this study and accepted the baseline clinical examination and questionnaire. The participants recruited did not know exposure status or knowledge of their disease. The subjects participated in this study were not informed of the study aim or hypothesis of the research reported in here. Participants were interviewed face-to-face, using structured questionnaires. Before beginning to survey, all personnel relevant to it were performed at least one day of strict special training. The questionnaires contains the information about socio-demographic factors, health, drinking history, age, gender, education, marital status, household income, smoking history (smoking status, pack-years of smoking, and passive smoke), working experience, former disease history, and household fuel exposure. For each participant, their household exposure to solid fuel (coal, wood fuel and straw) during cooking and heating was assessed as: ever used, duration (the number of years for cooking or heating using solid fuels), total number (multiplying the number of fuel used by the annual amount of fuel used), and lifetime average amount (multiplying duration by annual amount by dividing age). The outcome of interest in current study, participants’ stroke, CHD, diabetes and dyslipidemia was assessed by self-reported questionnaire ascertained with a subject answered “Yes” to the question, during their lifetime, if these diseases were diagnosed by a doctor.
For the subject, the doctor with professional medical direction measured their height, weight, and waist circumference, from which the body mass index value (BMI) was calculated by dividing weight by height. After resting for >10 minutes in a sitting position, systolic blood pressure (SBP) and diastolic blood pressure (DBP) at the right brachial artery were measured by a nurse practitioner using a mercury manometer. Blood pressure was measured 3 times at 2-minute intervals. The nurse specialist recorded the date and time. The average of three measures was used as the subject’s final SBP and DBP estimate.
In order to reduce the sampling error associated with multistage sampling, we increased sampling fraction during the first stage of sampling, and make an appropriate sampling fraction reduction in the second stage. The validity and reliability of SBP and DBP measurement were improved through 3 times. We tried to minimize potential sources of measurement bias by doing this.
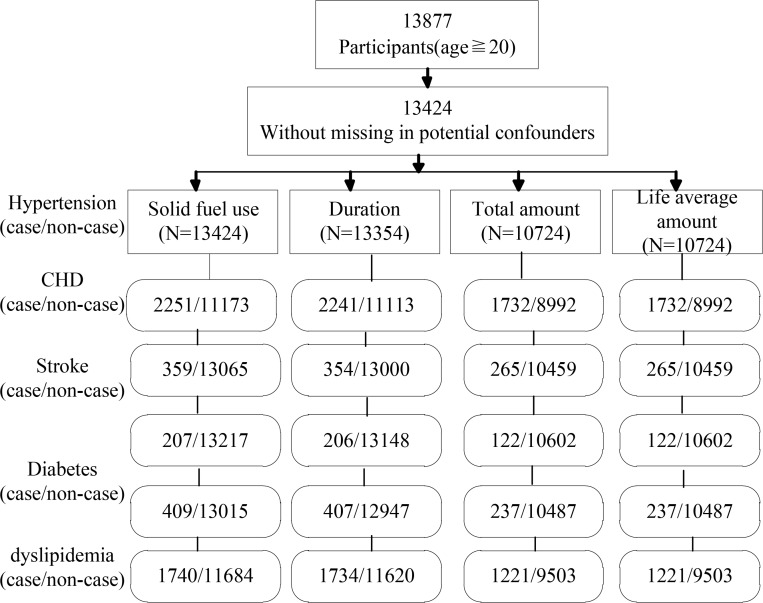
The data reported in this study were collected from December 2010 to November 2011. The data is recorded into the computer using SPSS software. All study data were reviewed carefully for missing data, and all the participants with missing data were excluded before data analysis (Fig. 2).
Fig. 2:
Flow diagram showing inclusion and exclusion of study participants
Statistical analysis
In this study, household exposure to solid fuel for heating and cooking was described as use of solid fuels (ever users versus nonusers), duration using solid fuels use in years, and total number of solid fuel use in kilograms, and average amount of it in kilograms per year. These test terms were assessed on a continuous scale and categorized into each tertile based on exposure distribution. To evaluate the association of independent variable i.e. age, gender, education level, smoking, passive smoking, BMI, and waist circumference) with the risk of CVDs, we first applied Logistic regression to test the association between household solid fuel exposure and each CVDs outcome after adjusting for independents. In the model, the main key independent variables considered were age, gender, education level, smoking conditions, passive smoking (ever and never), waist circumference above 80 (female) or 90 (male), below 80 (female) or 90 (male), and BMI below 18.5, 18.5–24.9, and above 25. We estimated the following regression equation:
Where y denotes each CVDs outcome and xm represents the values of the independent variables. Trend test was conducted by considering the exposure variables grouped into tertile and then putting into the model as a continuous variable. By observing the result of model, we analyze whether the risk of CVDs is associated with in different duration and amount of solid fuel exposure. In addition, a modeling strategy with interaction terms was adopted to see the results in Table 5. Further analysis for the association of solid fuel with each CVDs were tested for sub-population stratified by age (<50 and >=50), for CVDs is main disease prevalence in Chinese above 50 years (28), gender (male and female) and smoking status (ever and never). Partial regression coefficient (β), odds ratios (OR) and 95% confidence intervals (C.I.) were calculated based on logistic regression model. The statistically significant criterion was set at (P<0.05). All statistical analysis was performed using SAS Version 9.2 (SAS Institute Inc. Cary, NC, USA)
Table 5:
Result of Logistic regression about association between household solid fuel use and CVDs grouped by age, gender, smoking status and drinking history
| Hypertension β/OR/95%C.I. | CHD β/OR/95%C.I. | Stroke β/OR/95%C.I. | Diabetes β/OR/95%C.I. | Dyslipidemia β/OR/95%C.I. | |
|---|---|---|---|---|---|
| Agea | |||||
| ≤50 | 0.141/1.151/0.561–2.023 | NCe | NCe | −0.576/0.562/0.163–2.682 | 0.078/1.081/0.542–1.982 |
| >50 | 0.323/1.382/1.023–1.574 | 0.503/1.653/1.182–3.021 | 0.248/1.282/1.023–2.014 | 0.638/1.893/1.223–2.432 | 0.226/1.253/1.034–1.493 |
| p for interaction | 0.29 | 0.98 | 0.99 | 0.46 | 0.27 |
| Genderb | |||||
| Male | 0.372/1.451/1.153–1.892 | 0.578/1.783/0.894–3.952 | 0.484/1.622/0.753–3.873 | 0.684/1.981/0.892–2.993 | 0.365/1.441/1.023–2.561 |
| Female | 0.638/1.892/1.49–2.62 | 0.976/2.653/1.972–3.891 | 0.115/1.122/0.341–3.103 | 0.419/1.521/0.562–4.232 | 0.465/1.592/1.102–2.353 |
| p for interaction | 0.05 | 0.45 | 0.82 | 0.64 | 0.06 |
| Smoking statusc | |||||
| Ever | 0.352/1.422/1.213–2.754 | 0.096/1.101/0.812–1.593 | 0.577/1.781/0.972–3.123 | 1.027/2.792/1.282–3.123 | 0.419/1.521/1.122–1.873 |
| Never | 0.495/1.64/1.35–2.89 | 1.012/2.752/1.782–3.563 | 0.554/1.74/0.842–2.561 | 0.648/1.912/1.023–2.541 | 0.359/1.432/1.353–1.765 |
| p for interaction | 0.02 | 0.25 | 0.18 | 0.59 | 0.08 |
| Drinking historyd | |||||
| Ever | 0.851/2.342/1.234–2.982 | 0.445/1.561/1.022–2.103 | 0.351/1.421/1.023–1.553 | 0.446/1.562/0.823–1.991 | 0.794/2.212/1.783–3.123 |
| Never | 0.209/1.232/1.124–1.993 | 0.114/1.121/1.013–1.553 | 0.193/1.213/1.023–1.343 | 0.515/1.673/0.991–2.123 | 0.177/1.193/1.022–2.783 |
| p for interaction | 0.05 | 0.02 | 0.23 | 0.25 | 0.05 |
Adjusted for gender, education level, smoking, passive smoking, drink history, BMI, and waist circumference.
Adjusted for age, education level, smoking, passive smoking, drink history, BMI, and waist circumference.
Adjusted for age, gender, education level, drinking history, BMI, and waist circumference.
Adjusted for age, gender, education level, smoking, passive smoking, BMI, and waist circumference.
ORs and 95% CIs are not estimated due to small number of cases [number of cases for CHD (n=12) and for stroke (n=1), respectively.
Results
Descriptive Statistics
From the 13,877 subjects, 453 participants were not included, because of their missing potential confounder’s data including BMI, education, waist circumference, smoking, pack-years of smoking and passive smoking. This study include 13424 (96.7% of 13877) subjects, the subjects with missing information about the duration of solid fuel use (n=70), lifetime average amount and total number (n=2700) were also excluded. There were included 13354 subjects in the final analysis for the duration of solid fuel use and 10724 subjects for the analysis of total number and lifetime average amount using solid fuel use respectively (Fig. 2).
There were 6,477 men (46.7 percent) and 7400 women (53.3 percent) included in this study. Their mean (±SD) age is 48.5±15.1. 2775 (20%), 402 (2.9%), 235 (1.7%), 534 (3.8%) and 1838 (13.2%) has hypertension, CHD, stroke, diabetes and dyslipidemia, respectively (Table 1).
Table 1:
General characteristics of the study population, n (%) or Mean ± SD. Data are expressed as mean ± standard deviation or n (%)
| Variables | Overall (n=13877) |
|---|---|
| Age, yr | 48.5±15.1 |
| 20–29 | 2110 (15.2) |
| 30–39 | 2053 (14.8) |
| 40–49 | 2238 (16.1) |
| 50–59 | 3976 (28.7) |
| 60–79 | 3500 (25.2) |
| Gender | |
| Male | 6477 (46.7) |
| Female | 7400 (53.3) |
| Education level | |
| Less than high school | 7610 (54.8) |
| High school | 5827 (42.1) |
| College or above | 439 (3.1) |
| Waist circumference, cm | |
| ≥80 (female) or 90 (male) | 9782 (0.70) |
| <80 (female or 90 (male) | 4163 (0.30) |
| BMI, kg/cm | |
| ≥25 | 3094 (22.3) |
| 18.5–24.9 | 9588 (69.1) |
| <18.5 | 984 (7.1) |
| Smoking background | |
| Currently a smoker | 6244 (0.45) |
| Never smoked | 6938 (0.50) |
| Smoking index, pack-years | 8.2±23.5 |
| Passive smoke | |
| Never | 2456 (0.18) |
| Ever | 11420 (0.82) |
| Drinking history | |
| Never | 5210 (37.5) |
| Ever | 8667 (62.4) |
| Household solid fuel exposures, cooking or heating | |
| Exposure duration, year | 22±1.62 |
| Total amount, ton | 16.2±10.6 |
| Average amount the whole life, ton/year | 256.7±211.4 |
| Hypertension | |
| Yes | 2775 (20) |
| No | 11102 (80) |
| Coronary heart disease | |
| Yes | 402 (2.9) |
| No | 13475 (97.1) |
| Stroke | |
| Yes | 235 (1.7) |
| No | 13642 (98.3) |
| Diabetes | |
| Yes | 534 (3.8) |
| No | 13343 (96.2) |
| Dyslipidemia | |
| Yes | 1838 (13.2) |
| No | 12039 (86.8) |
Relationship between household solid fuel use and its potential factors
We found that there are the biological and potential cardiovascular risk factors by stratifying household solid fuel. There exists a significance difference between ever users and non-users, which are found in age, gender, education, smoking, passive smoke and drinking history after adjusting for the other potential confounders (Table 2).
Table 2:
General characteristics of the study population, stratified by household solid fuel use, n (%) or mean±SD
| Variables | Ever user (n=11390) | Nonuser (n=2487) | P-value |
|---|---|---|---|
| Age, yrs | 46.5 | <0.001 | |
| 20–29 | 1129 (53.5) | 981 (46.5) | |
| 30–39 | 1365 (66.5) | 688 (33.5) | |
| 40–49 | 1850 (82.7) | 388 (17.3) | |
| 50–59 | 3609 (90.8) | 367 (9.2) | |
| 60–79 | 3437 (98.2) | 63 (1.8) | |
| Gender | |||
| Male | 5615 (86.7) | 826 (13.3) | 0.05 |
| Female | 5775 (78) | 1625 (22) | Reference |
| Education level | |||
| Less than high school | 7305 (95.2) | 266 (3.8) | 0.001 |
| High school | 5287 (78) | 784 (22) | 0.701 |
| College or above | 254 (58) | 184 (42) | Reference |
| Waist circumference, cm | |||
| ≥80 (female) or 90 (male) | 8314 (84.8) | 1486 (15.2) | 0.07 |
| <80 (female or 90 (male) | 2905 (68.2) | 1382 (33.2) | Reference |
| BMI, kg/cm | |||
| ≥25 | 2561 (82.8) | 532 (17.2) | 0.1 |
| 18.5–24.9 | 7497 (78.1) | 2090 (21.8) | 0.72 |
| <18.5 | 608 (61.8) | 375 (38.2) | Reference |
| Smoking | |||
| Current smoker | 5120 (88) | 749 (12) | 0.01 |
| Never smoker | 5204 (75) | 1735 (25) | Reference |
| Passive smoke | |||
| Never | 1743 (71) | 712 (29) | <0.001 |
| Ever | 9592 (0.82) | 1773 (16) | Reference |
| Drinking history | |||
| Ever | 6947 (80.1) | 1720 (19.8) | <0.001 |
| Never | 4248 (81.6) | 962 (18.2) | Reference |
P-value for comparing the difference between ever users versus nonusers, given by logistic regression analysis after adjusting for all potential confounding variables
Relationship between CVDs and household fuel use
Table 3 and Table 4 list the relationship of household solid fuel use for cooking and heating, assessed by ever use, duration, total amount, and life-time amount during the lifetime, with hypertension, CHD, stroke, diabetes and dyslipidemia.
Table 3:
Result of Logistic regression about association between household solid fuel use and CVDs after adjusted for age and gender in model1
| Variable | Hypertension Model 1 β/OR/95%C.I. | CHD Model 1 β/OR/95%C.I. | Stroke Model 1 β/OR/95%C.I. | Diabetes Model 1 β/OR/95%C.I. | Dyslipidemia Model 1 β/OR/95%C.I. |
|---|---|---|---|---|---|
| Household fuel use (case/noncase) | 2251/11173 | 359/13065 | 207/13217 | 409/13015 | 1740/11684 |
| Ever | 0.636/1.888/1.396–2.384 | 0.777/2.175/1.545–3.061 | 0.501/1.650/1.175–2.341 | 0.754/2.126/1.336–3.383 | 0.219/1.245/0.892–2.564 |
| Never | Reference | ||||
| Duration (year) (case/noncase) | 2241/11113 | 354/13000 | 206/13148 | 407/12947 | 1734/11620 |
| >20 | 0.626/1.870/1.530–2.020 | 0.542/1.720/1.020–1.990 | 0.683/1.980/0.970–2.230 | 1.102/3.010/1.990–4.250 | 0.655/1.925/1.101–2.700 |
| 8–20.1 | 0.458/1.581/1.340–1.971 | 0.600/1.750/0.790–2.011 | 0.482/1.620/1.201–2.309 | 1.055/2.873/2.121–3.120 | 0.432/1.541/1.001–2.103 |
| <8 | Reference | ||||
| P | 0.001 | 0.546 | 0.005 | 0.001 | 0.001 |
| Total amount (Ton) (case/noncase) | 1732/8992 | 265/10459 | 122/10602 | 237/10487 | 1221/9503 |
| >18.5 | 0.599/1.821/1.252–1.973 | 0.549/1.732/0.872–2.011 | 0.419/1.521/0.921–1.852 | 1.012/2.752/1.823–4.221 | 0.566/1.762/1.223–2.105 |
| 5–18.5 | 0.432/1.541/1.111–1.872 | 0.330/1.391/0.742–1.853 | 0.271/1.311/0.782–1.367 | 1.072/2.921/1.753–4.123 | 0.611/1.843/1.024–2.542 |
| <5 | Reference | ||||
| P | 0.001 | 0.175 | 0.021 | 0.001 | 0.001 |
| Lifetime average Amount (ton/year) (case/noncase) | 1732/8992 | 265/10459 | 122/10602 | 237/10487 | 1221/9503 |
| >0.55 | 0.351/1.421/1.101–1.752 | −0.161/0.851/0.622–1.182 | 0.279/1.322/0.751–1.522 | 0.393/1.481/0.992–1.851 | 0.373/1.452/1.214–1.982 |
| 0.09–0.55 | 0.316/1.372/1.154–1.623 | −0.028/0.972/0.521–1.232 | 0.098/1.103/0.543–1.322 | −0.137/0.872/0.39–1.123 | 0.202/1.224/1.023–1.982 |
| <0.09 | Reference | ||||
| P | 0.001 | 0.005 | 0.030 | 0.005 | 0.005 |
Table 4:
Result of Logistic regression about association between household solid fuel use and CVDs after adjusted for age, gender, education level, smoking background, alcoholic history, BMI and waist circumference in model 2
| Variable | Hypertension Model 2 β/OR/95%C.I. | CHD Model 2 β/OR/95%C.I. | Stroke Model 2 β/OR/95%C.I. | Diabetes Model 2 β/OR/95%C.I. | Dyslipidemia Model 2 β/OR/95%C.I. |
|---|---|---|---|---|---|
| Household fuel use (case/noncase) | 2251/11173 | 359/13065 | 207/13217 | 409/13015 | 1740/11684 |
| Ever | 0.560/1.751/1.273–2.106 | 0.811/2.251/1.232–3.101 | 0.450/1.642/1.182–2.245 | 0.681/1.975/1.201–2.634 | 0.170/1.185/1.101–2.311 |
| Never | Reference | ||||
| Duration (year) (case/noncase) | 2241/11113 | 354/13000 | 206/13148 | 407/12947 | 1734/11620 |
| >20 | 0.501/1.651/1.233–1.972 | 0.143/1.554/0.782–1.982 | 0.167/1.812/1.213–2.213 | 1.061/2.891/1.972–4.021 | 0.563/1.756/1.123–2.233 |
| 8–20.1 | 0.302/1.352/1.023–1.802 | 0.521/1.682/1.023–2.003 | 0.302/1.353/0.874–2.023 | /0.975/2.652/1.823–3.642 | 0.353/1.423/1.134–2.342 |
| <8 | Reference | ||||
| P | 0.001 | 0.878 | 0.012 | 0.001 | 0.001 |
| Total amount (Ton) (case/noncase) | 1732/8992 | 265/10459 | 122/10602 | 237/10487 | 1221/9503 |
| >18.5 | 0.452/1.572/1.223–1.873 | 0.316/1.372/ 0.753–2.232 | 0.538/1.713/0.921–2.232 | 0.897/2.452/1.823–4.351 | 0.421/1.524/1.031–1.993 |
| 5–18.5 | 0.192/1.212/1.023–1.672 | 0.807/2.242/1.651–3.452 | 0.293/1.341/0.841–2.103 | 0.851/2.342/1.712–3.973 | 0.483/1.621/1.023–2.012 |
| <5 | Reference | ||||
| P | 0.001 | 0.198 | 0.035 | 0.001 | 0.001 |
| Lifetime average Amount (ton/year) (case/noncase) | 1732/8992 | 265/10459 | 122/10602 | 237/10487 | 1221/9503 |
| >0.55 | 0.264/1.302/1.103–1.532 | −0.135/0.874/0.513–1.122 | 0.302/1.352/0.622–1.852 | 0.303/1.354/1.128–1.981 | 0.332/1.393/1.124–1.563 |
| 0.09–0.55 | 0.226/1.253/1.024–1.523 | −0.018/0.982/0.623–1.754 | 0.089/1.093/0.584–1.363 | −0.158/0.854/0.692–1.232 | 0.116/1.123/1.013–1.991 |
| <0.09 | Reference | ||||
| P | 0.001 | 0.006 | 0.051 | 0.007 | 0.001 |
In model 1, we initially controlled age and gender, two covariates as potential confounders. In general, CVDs are influenced by such factors as smoking, education, drinking history, BMI, second-hand smoke, and waist circumference, thus these potential confounders were further adjusted in model 2 (13). Household solid fuel use is associated with hypertension (OR 1.751), CHD (OR 2.251), stroke (OR 1.642), diabetes (OR 1.975) and dyslipidemia (OR 1.185,), adjusting for potential cardiovascular risk and confounding factors in model 2. Longer duration of solid fuel use is associated with an increased odds of hypertension (OR 1.651), stroke (OR 1.812), diabetes (OR 2.891) and dyslipidemia (OR 1.756) in the highest compared with lowest tertile. Total amount of solid fuel during the lifetime are associated with an increased odds of hypertension (OR 1.572), diabetes (OR 2.452) and dyslipidemia (OR 1.524), in the highest compared with lowest tertile. The results of these effects in model 2 were not changeable much compared to in model 1, adjusted for age and gender.
By age group, similar associations were known between household solid fuel use and the risk of hypertension (OR 1.382), CHD (OR 1.653), and stroke (OR 1.282), and diabetes (OR 1.893), and dyslipidemia (OR 1.253) among the group of age ≥ 50 (Table 5), which is the same as the result of Lee’s study except the stroke disease, for the rural villages in Jingle county is much poorer (13).
In contrast, even none association was seen among subjects with age < 50 and the number of case with CHD and stroke in this age group was few to none. The interaction term has not statistically significant in the model. By gender, the relationships between household solid fuel use with CVDs end points were similar for men and women, but the odds of household fuel use with hypertension was greater among woman (OR 1.892) than men (OR 1.451) and there is the statistically significant difference (P for interaction = 0.05). In dyslipidemia, female (OR 1.592) is also different from man (OR 1.441). No statistically significant difference was found by gender in the association of household solid fuel use with other CVDs and points. By smoking status, slightly higher ORs for hypertension and dyslipidemia were observed among never smokers compared to those among ever smokers and interaction term (hypertension 0.02, dyslipidemia 0.08) in the logistic model was significant, respectively. By drinking history, the odds of household solid fuel use with hypertension (OR 2.342), CHD (OR 1.561) and dyslipidemia (OR 2.212) was a bit higher than those without drinking history.
Discussion
Major findings
In this rural household solid fuel and CVDs based cross-sectional study, the result shows that members particularly using the house hold solid fuels during cooking and heating, can have an easily higher risk of hypertension, CHD, stroke, diabetes and dyslipidemia than those of non-solid fuel users, especially among population over 50 years in rural areas of China, which is partly not the same as the previous studies (13). As the sample included ten percent of adult population living in Jingle County based on a multistage sampling method, so it could be almost generalized to the whole people living there. We can also conclude people over 50 years get the higher risk for CVDs. Therefore these findings might be of interest to clinicians, scientists, policy makers and health planners to consider aging process and transformation of household fuel for cooking and heating, as an important risk factor for reducing CVDs and they should have effective interventions to prevent the effects of household fuel on CVDs. Little epidemiologic data on the effect using household solid fuel on the cardiovascular diseases are studied. Lack of epidemiologic data makes direct comparison with our findings difficult, but there are numerous cardiovascular epidemiological studies, which showed they are associated with indoor air pollutants such as PM10, PM2.5, SO2 and heavy metals, contributing to indoor high particulate level during combustion of solid fuel (13, 29–34). Personal PM2.5 exposure was positively associated with post-exposure measurement of systolic blood pressure (SBP) and diastolic blood pressure (DBP).
A 1-log-ug/m3 increase in PM2.5 exposure was associated with 2.2 mm Hg higher SBP and 0.5 mm Hg higher DBP in China (19). In Australia, exposure to particles with PM10 due to ambient bio-mass smoke was associated with an increased risk of cardiovascular and respiratory mortality during winter months (35). Woman in India who cooked with fossil and biomass fuel had higher incidence of hypertension than women using cleaner fuel for cooking (36). Two recent epidemiological studies implied that the longer exposure to PM2.5 from incomplete combustion was positively associated with systolic and diastolic blood pressure (BP) in woman of rural China (37, 38).
Several studies on cardiovascular effects due to using solid fuel for cooking and heating have also shown positive associations with hypertension and blood pressure (8, 9, 19, 31, 36, 38, 39). Our results are consistent with previous epidemiological studies on exposure to household solid fuel and blood pressure. As for hypertension, there exists stronger association in this study among women, with an OR of 1.892 for women and 1.451 for men, whereas the associations of household solid fuel with other results are not consistent by gender, as previous studies related to air pollution and cardiovascular effects are inconsistent. It is generally believed that women usually spend more time in their home and do a few more cooking (40), so they are more at risk for household solid fuel exposure, but due to the lack of data on amount of time spent of staying home and cooking, we did not resolve it. In our study, however, we observe the association with an increased risk of hypertension in men and women, implying home solid fuel use may also be an important risk for men. Our studied outcomes classified by smoking indicated that there was a stronger association between home solid fuel and hypertension, CHD among never smokers and small or null among ever smokers. Some epidemiologic studies show that there is a stronger environmental pollutants-CVDs association among never smokers than ever smokers, which implied that this might indicate the influence of pressures (41). Our results classified by cigarette smoking suggests that residual confounding by smoking impacts couldn’t interpret our results, however, we cannot exclude partly hidden facts.
Inefficient and incomplete burning of home solid fuels, including fossil fuels and biomass for cooking and heating emit particles, gases, and semi volatile compounds, which in total we refer them as household air pollution (HAP) (42). HAP contains a multitude of compounds which have toxic effects on public health, though potential toxic effects about household solid fuel emission associated with cardiovascular system are unclear, the main mechanisms are likely related to inflammation by the generation of reactive oxygen species (ROS) and oxidative stress (43, 44). A study indicated that the Oxidative stress, defined as an excess production of reactive oxygen species (ROS) relative to antioxidant defense, has been shown to play an important role in the pathophysiology of cardiac remodeling and heart failure (HF) (45). The evidences of the recent study showed using fossil fuels or biomass for cooking and heating greatly contribute to PM exposure, especially for women performing the cooking. Suspended fine particulate matter (PM2.5, aerodynamic diameter less than 2.5μm) from household fuels burning is a major constituent of HAP, and PM2.5 is recognized as a risk factor for cardiovascular diseases (8, 13, 40, 42, 46). These particles are predominantly in the size range, capable of depositing deeply in the lungs, particularly in particle stage, which may contribute to oxidative DNA damage and secretion of pro-inflammatory cytokines and chemokines that cause cardiovascular diseases (13, 47). There are strong associations between longer HAP exposure and oxidative DNA damage evaluated by 8-hydroxy-2-deoxyguanosine in Chinese restaurant workers (13, 48).
Practical implications
According the results of this study, probably the simplest way to reduce the occurrence of CVDs is to use clean fuel for cooking and heating. Therefore, first, it is necessary to develop biogas energy for cooking and heating in rural areas, for producing biogas by using anerobic fermentation technology can not only develop energy but also reduce environmental pollution. Second, local governments increase the subsidies to biogas development in rural areas and devote to expanding the availability of cleaner energy technologies to reduce poverty and improve health. Third, the Chinese government should help peasants develop the large-scale dissemination of clean cook stoves and fuels.
Limitations and future research
Our study has several limitations as well. First, we assessed the association of household fuels and hypertension, CHD, stroke, diabetes and dyslipidemia based on cross-sectional study, from which we get the results by chance because of cross-sectional with inherent temporal problems. These findings need warrant in the prospective studies. Second, all participants in this study are from regional rural areas, not urban areas, and therefore might not represent the exposure of the whole town of China. Third, there are associations between exposure to household solid fuels and CVDs from our study, but these diseases may be linked to the other factors, such as the income levels of China’s ordinary residents, nutritional status and person’s immunity, and so we should explain this association with cautions. Fourth, of concern is the potential bias caused lack of data on lifetime average amount of solid fuel use (23% of 13877). To check this, the association between each CVDs outcome and missing in lifetime average amount of household fuel use among ever users were analyzed. No association was found with CHD and diabetes among the subjects with missing data in lifetime average amount of household solid fuel use compared with the participants without missing, whereas an increased risk of dyslipidemia was found. The results of our study are consistent when we considered many household solid fuel exposure indexes such as total amount, duration and lifetime average amount. Therefore, it is unlikely that our observed results are due to possible selection bias by lack of data in lifetime average amount of solid fuel use. Although in our study there was the source of exposure in this large population, we did not assure which constituents of household fuel exposure were strong relation to cardiovascular effects, and had bad effects on CVDs. We should use biomarkers of exposure in the future longitudinal research to identify the special chemicals of household solid fuels associated with cardiovascular, in order to better understand impacts of household fuels emission on people cardiovascular system.
In fact, when we were talking about the association between household fuel and CVDs, essentially, what we were talking about were the health risks of indoor air pollution resulting from household solid fuel for cooking and heating. It is also known that other factors such as family income level and social supports affected the citizen’s health. These factors were not measured in this research. Therefore, in spite of large sample size of this study, it seems that the results of this study could not be generalized to complete rural people of China. For these reasons, further studies on household fuel and CVDs in rural areas of China which focus on the integration of new energy policy for cooking and heating, economic level and living conditions, and consider the rural village of different town while adjusting for all other probably variables are strongly recommended.
Conclusion
Household solid fuel in China’s rural area maybe associated with an increased risk of hypertension, CHD, diabetes and dyslipidemia in the general rural adult population. The longer the exposures to household solid fuel are, the greater their risk for CVDs are, which showed evidence of toxicity of household solid fuel emission. The studied outcome in this paper, however, need be explained cautiously due to the cross-sectional attribute of the design. Our findings should be confirmed in prospective cohort studies.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, and/or falsification, double publication) have been considered carefully.
Acknowledgements
This paper was funded by Program for New Century Excellent Talents in University (NCET-11-0792), National Natural Science Foundation of China (71272057, 70972006). We would like to express our gratitude to the nursing and administration staff of Jingle County People’s hospital. The authors declare that there is no conflict of interests.
References
- 1. Jeuland MA, Pattanayak SK. (2012). Benefits and costs of improved cookstoves: assessing the implications of variability in health, forest and climate impacts. PLoS One, 7( 2): 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rehfuess E, Mehta S, Pruss-Ustun A. (2006). Assessing household solid fuel use: multiple implications for the Millennium Development Goals. Environ Health Persp, 114( 3): 373–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hu G, Ran P. (2009). Indoor air pollution as a lung health hazard: focus on populous countries. Curr Opin Pulm Med, 15( 2): 158–164. [DOI] [PubMed] [Google Scholar]
- 4. Diaz-Guzman E, Mannino DM. (2014). Epidemiology and Prevalence of Chronic Obstructive Pulmonary Disease. Clin Chest Med, 35( 1): 7–16. [DOI] [PubMed] [Google Scholar]
- 5. Fatmi Z, Coggon D, Kazi A, Naeem I, Kadir M, Sathiakumar N. (2014). Solid fuel use is a major risk factor for acute coronary syndromes among rural women: a matched case control study. Public Health, 128( 1): 77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Urmee T, Gyamfi S. (2014). A review of improved Cookstove technologies and programs. Renew Sust Energ Rev, 33( 2): 625–635. [Google Scholar]
- 7. Su J, Mu L-n, Yu S-z, Niu R-g, Han X-y, Liu L, Shi J-p, Zhang Z-f. (2013). The case-control study of lung cancer in Taiyuan, China. Tumor, 33( 10): 884–890. [Google Scholar]
- 8. McCracken JP, Wellenius GA, Bloomfield GS, Brook RD, Tolunay HE, Dockery DW, Rabadan-Diehl C, Checkley W, Rajagopalan S. (2012). Household air pollution from solid fuel use: evidence for links to CVD. Global Heart, 7( 3): 223–234. [DOI] [PubMed] [Google Scholar]
- 9. Baumgartner J, Smith KR, Chockalingam A. (2012). Reducing CVD through improvements in household energy: implications for policy-relevant research. Global Heart, 7( 3): 243–247. [DOI] [PubMed] [Google Scholar]
- 10. Fan JS, Shao LY, Wang J, Wang JY, Li ZX. (2012). Variations in mass concentrations of indoor inhalable particulates in the coal-burning indoor air in Xuanwei County, Yunnan province. Chin Environ Sci, 32( 8): 1379–1383. [Google Scholar]
- 11. Moran A, Gu D, Zhao D, Coxson P, Wang YC, Chen CS, Liu J, Cheng J, Bibbins-Domingo K, Shen YM, He J, Goldman L. (2010). Future cardiovascular disease in china: markov model and risk factor scenario projections from the coronary heart disease policy model-china. Circ Cardiovasc Qual Outcomes, 3( 3): 243–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhang Y, Mo J J., Weschler C. (2013). Reducing health risks from indoor exposures in rapidly developing urban China. Environ Health Persp, 121( 7): 751–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lee M-S, Hang J, Zhang F, Dai H, Su L, Christiani DC. (2012). In-home solid fuel use and cardiovascular disease: a cross-sectional analysis of the Shanghai Putuo study. Environ Health, 11( 1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jin-Ho Y, Wi-Young S. (2013). Associations of Hypertension Status with Physical Fitness Variables in Korean Women. Iran J Public Health, 42( 7): 673–680. [PMC free article] [PubMed] [Google Scholar]
- 15. Namayandeh S, Sadr S, Rafiei M, Modares-Mosadegh M, Rajaefard M. (2011). Hypertension in Iranian urban population, epidemiology, awareness, treatment and control. Iran J Public Health, 40( 3): 63–70. [PMC free article] [PubMed] [Google Scholar]
- 16. Aunan K, Wang S. (2014). Internal migration and urbanization in China: Impacts on population exposure to household air pollution (2000–2010). Sci Total Environ, 481( 2): 186–195. [DOI] [PubMed] [Google Scholar]
- 17. Bautista LE, Correa A, Baumgartner J, Breysse P, Matanoski GM. (2009). Indoor charcoal smoke and acute respiratory infections in young children in the Dominican Republic. Am J Epidemiol, 169( 5): 572–580. [DOI] [PubMed] [Google Scholar]
- 18. Kurmi OP, Semple S, Simkhada P, Smith WC, Ayres JG. (2010). COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax, 65( 3): 221–228. [DOI] [PubMed] [Google Scholar]
- 19. Baumgartner J, Schauer JJ, Ezzati M, Lu L, Cheng C, Patz JA, Bautista LE. (2011). Indoor air pollution and blood pressure in adult women living in rural China. Environ Health Persp, 119( 10): 1390–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Brook RD, Bard RL, Burnett RT, Shin HH, Vette A, Croghan C, Phillips M, Rodes C, Thornburg J, Williams R. (2011). Differences in blood pressure and vascular responses associated with ambient fine particulate matter exposures measured at the personal versus community level. Occup Environ Med, 68( 3): 224–230. [DOI] [PubMed] [Google Scholar]
- 21. Harrabi I, Rondeau V, Dartigues JF, Tessier JF, Filleul L. (2006). Effects of particulate air pollution on systolic blood pressure: A population-based approach. Environ Res, 101( 1): 89–93. [DOI] [PubMed] [Google Scholar]
- 22. Madsen C, Nafstad P. (2006). Associations between environmental exposure and blood pressure among participants in the Oslo Health Study (HUBRO). Eur J Epidemiol, 21( 7): 485–491. [DOI] [PubMed] [Google Scholar]
- 23. Sussan TE, Ingole V, Kim J-H, McCormick S, Negherbon J, Fallica J, Akulian J, Yarmus L, Feller-Kopman D, Wills-Karp M. (2013). Source of biomass cooking fuel determines pulmonary response to household air pollution. Am J Resp Cell Mol, 50( 3): 538–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fernandes L, Mesquita AM. (2014). Household Air pollution due to Biomass smoke exposure and Chronic Obstructive Pulmonary Disease. Int J Biomed Adv Res, 5( 2): 65–67. [Google Scholar]
- 25. Hosgood HD, III, Chapman RS, He X, Hu W, Tian L, Liu LZ, Lai H, Chen W, Rothman N, Lan Q. (2013). History of lung disease and risk of lung cancer in a population with high household fuel combustion exposures in rural China. Lung Cancer, 81( 3): 343–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sapkota A, Zaridze D, Szeszenia-Dabrowska N, Mates D, Fabiánová E, Rudnai P, Janout V, Holcatova I, Brennan P, Boffetta P. (2013). Indoor air pollution from solid fuels and risk of upper aerodigestive tract cancers in Central and Eastern Europe. Environ Res, 120( 1): 90–95. [DOI] [PubMed] [Google Scholar]
- 27. Chen L, Zhou X. (2010). Progress in global research and development of cardiovascular medicines. Chin J New Drugs, 19( 1): 8–16. [Google Scholar]
- 28. Li SL, Zhou Dh, Wan L, Fu Y, Zhang JH, Li N, Yao FC. (2010). Status quo analysis for treatment of myocardial infarction in rural Liaoning. Chin J Pract Intern Med, 30( 12): 1129–1130. [Google Scholar]
- 29. Liu Y, Lu X, Huang ZJ, Yuan H. (2010). Air pollution and its health impact. Chin J Mod Med, 21( 1): 87–91. [Google Scholar]
- 30. Mei XM, Pan XC, Ping JY, Xing LG. (2011). Evaluation of Personal Integrated Exposure to Fine Particle in a Community in Beijing. J Environ Health, 28( 11): 941–944. [Google Scholar]
- 31. Wold LE, Ying Z, Hutchinson KR, Velten M, Gorr MW, Velten C, Youtz DJ, Wang A, Lucchesi PA, Sun Q. (2012). Cardiovascular remodeling in response to long-term exposure to fine particulate matter air pollution. Circulation: Heart Fail, 5( 4): 452–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lin L-Y, Chuang H-C, Liu I, Chen H-W, Chuang K-J. (2013). Reducing indoor air pollution by air conditioning is associated with improvements in cardiovascular health among the general population. Sci Total Environ, 463( 5): 176–181. [DOI] [PubMed] [Google Scholar]
- 33. Yamamoto S, Phalkey R, Malik A. (2014). A systematic review of air pollution as a risk factor for cardiovascular disease in South Asia: Limited evidence from India and Pakistan. In J of Hyg Envir Heal, 217( 2): 133–144. [DOI] [PubMed] [Google Scholar]
- 34. Kan H, Chen R, Tong S. (2012). Ambient air pollution, climate change, and population health in China. Environ Int, 42( 1): 10–19. [DOI] [PubMed] [Google Scholar]
- 35. Johnston FH, Hanigan IC, Henderson SB, Morgan GG. (2013). Evaluation of interventions to reduce air pollution from biomass smoke on mortality in Launceston, Australia: retrospective analysis of daily mortality, 1994–2007. BMJ, 346: e8446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dutta A, Ray MR. (2013). Hypertension and respiratory health in biomass smoke-exposed premenopausal Indian women. Air Qual Atmos Health, 7( 2): 229–238. [Google Scholar]
- 37. Dong FM, Mo YZ, Li GX, Xu MM, Pan XC. (2013). Association between ambient PM10/PM2.5 levels and population mortality of circulatory diseases: a case-crossover study in Beijing. J Peking Univ (Health Sci), 45( 3): 398–404. [PubMed] [Google Scholar]
- 38. Mestl HE, Edwards R. (2011). Global burden of disease as a result of indoor air pollution in Shaanxi, Hubei and Zhejiang, China. Sci Total Environ, 409( 8): 1391–1398. [DOI] [PubMed] [Google Scholar]
- 39. Brook RD, Rajagopalan S, Pope CA, 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC, Jr., Whitsel L, Kaufman JD. (2010). Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation, 121( 21): 2331–2378. [DOI] [PubMed] [Google Scholar]
- 40. Baumgartner J, Schauer J, Ezzati M, Lu L, Cheng C, Patz J, Bautista L. (2011). Patterns and predictors of personal exposure to indoor air pollution from biomass combustion among women and children in rural China. Indoor Air, 21( 9282): 479–488. [DOI] [PubMed] [Google Scholar]
- 41. Satarug S, Garrett SH, Sens MA, Sens DA. (2010). Cadmium, environmental exposure, and health outcomes. Environ Health Persp, 118( 5): 182–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Khalequzzaman M, Kamijima M, Sakai K, Ebara T, Hoque BA, Nakajima T. (2011). Indoor air pollution and health of children in biomass fuel-using households of Bangladesh: comparison between urban and rural areas. Environ Health and Prev Med, 16( 6): 375–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Araujo JA. (2011). Particulate air pollution, systemic oxidative stress, inflammation, and atherosclerosis. Air Qual Atmos Health, 4( 1): 79–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Shiraiwa M, Selzle K, Pöschl U. (2012). Hazardous components and health effects of atmospheric aerosol particles: reactive oxygen species, soot, polycyclic aromatic compounds and allergenic proteins. Free Radical Res, 46( 8): 927–939. [DOI] [PubMed] [Google Scholar]
- 45. Tsutsui H, Kinugawa S, Matsushima S. (2011). Oxidative stress and heart failure. Am J Physiol-Heart C, 301(6): H2181–H2190. [DOI] [PubMed] [Google Scholar]
- 46. Li W, Wang C, Wang H, Chen J, Yuan C, Li T, Wang W, Shen H, Huang Y, Wang R. (2014). Distribution of atmospheric particulate matter (PM) in rural field, rural village and urban areas of northern China. Environ Pollut, 185( 4): 134–140. [DOI] [PubMed] [Google Scholar]
- 47. Danielsen PH, Møller P, Jensen KA, Sharma AK, Wallin Hk, Bossi R, Autrup H, Mølhave L, Ravanat J-L, Briedé JJ. (2011). Oxidative stress, DNA damage, and inflammation induced by ambient air and wood smoke particulate matter in human A549 and THP-1 cell lines. Chem Res Toxicol, 24( 2): 168–184. [DOI] [PubMed] [Google Scholar]
- 48. Sun Z, Shao L, Mu Y, Hu Y. (2014). Oxidative capacities of size-segregated haze particles in a residential area of Beijing. J Environ Sci, 26( 1): 167–174. [DOI] [PubMed] [Google Scholar]