Abstract
Purpose
Bruton’s tyrosine kinase (BTK) is a critical enzyme in the B-cell receptor pathway and is inhibited by ibrutinib due to covalent binding to the kinase domain. Though ibrutinib results in impressive clinical activity in chronic lymphocytic leukemia (CLL), most patients achieve only partial remission due to residual disease. We performed a pharmacologic profiling of residual circulating CLL cells from patients receiving ibrutinib to identify optimal agents that could induce cell death of these lymphocytes.
Experimental design
Ex vivo serial samples of CLL cells from patients on ibrutinib were obtained prior and after (weeks 2, 4, and 12) the start of treatment. These cells were incubated with PI3K inhibitors (idelalisib or IPI-145), bendamustine, additional ibrutinib, or BCL-2 antagonists (ABT-737 or ABT-199) and cell death was measured. In vitro investigations complemented ex vivo studies. Immunoblots for BTK signaling pathway and antiapoptotic proteins were performed.
Results
The BCL-2 antagonists, especially ABT-199, induced high cell death during ex vivo incubations. In concert with the ex vivo data, in vitro combinations also resulted highly cytotoxicity. Serial samples of CLL cells obtained before and 2, 4, 12, or 36 weeks after the start of ibrutinib showed inhibition of BTK activity and sensitivity to ABTs. Among the three BCL-2 family anti-apoptotic proteins that are overexpressed in CLL, levels of MCL-1 and BCL-XL were decreased after ibrutinib while ABT-199 selectively antagonizes BCL-2.
Conclusions
Our biological and molecular results suggest that ibrutinib and ABT-199 combination should be tested clinically against CLL.
Keywords: Bcl-2 antagonist, ibrutinib, ABT-199, ABT-737, CLL
Introduction
Chronic lymphocytic leukemia (CLL) is a neoplastic disorder characterized by mature B-lymphocytes that accumulate due to impaired program cell death (1). These cells reside in microenvironmental niches such as peripheral blood, bone marrow, and lymph nodes (2). The gene expression profile differs between compartments, however current treatments do not target the unique biology of this disease (3, 4). In fact, the standard of care for CLL is a cytotoxic therapy that includes fludarabine plus cyclophosphamide with the monoclonal antibody rituximab (FCR) (5–7). In newly diagnosed patients, FCR results in a 95% overall response rate, with a 70% rate of complete remissions, and about 1/3 of patients have event-free survival for ~10 years (i.e. cure). Yet, the FCR regimen has many limitations. For example, fludarabine-based regimens were not associated with improved outcomes in older (age ≥ 65 yrs) patients, who make up the majority of the CLL population (8). Additionally, patients with markers of poor prognosis, such as 11q del, 17p del, or IgVH unmutated gene or mutated TP53, remain high-risk with shorter progression-free survival even with FCR combination therapy (9). Moreover, recent long-term results in first salvage FCR-treated 300 CLL patients emphasize alternative therapeutic strategies. In these individuals, only one-third maintained remission after 12 years, while about 50% developed relapsed/refractory disease, 8% died in remission, and 7% developed second and aggressive malignancies such as acute leukemias or Richter’s transformation (10). These statistics underscore the need for a regimen that targets the biology of CLL disease.
Studies of the B-cell receptor (BCR) axis and its downstream kinases have provided a targeted non-chemotherapy alternative, as this pathway is a primary requisite for development and maintenance of both normal and malignant B-cells(11, 12). This network is important for B-cell proliferation, differentiation, and survival as well as cell migration and tissue homing (13). Bruton’s tyrosine kinase (BTK) is a pivotal enzyme in the BCR pathway (14). Ibrutinib (PCI-32765) is a relatively selective and irreversible inhibitor of BTK (14); this oral agent binds covalently to cysteine-481, which is located in the active site of this enzyme, thus inhibiting its activity (with an IC50 = 0.5 nM, and t1/2 > 24 hours)(15, 16). Lymph nodes and bone morrow provide tumorigenic protective microenvironments for CLL cells via the BCR network, and consequently, BCR kinase inhibitors disrupt this pathway (11, 17). In in vitro, ex vivo, and in vivo settings, ibrutinib inhibited the cytoprotective signals from the microenvironment, down-regulated survival and proliferative pathways, and lacked cytotoxicity toward T-cells (12, 18–21). Importantly, a Phase I trial(14), Phase Ib/II trial (22), and subsequent trial of ibrutinib in elderly patients with CLL (23) demonstrated high tolerability and an overall response rate of >70%, with a 26 month progression-free and overall survival rate of >75% (22).
Although ibrutinib results in impressive clinical outcomes, it has limitations. First, most responses have been partial remissions, and continuous use of the drug is required. For patients with 17p abnormalities, even ibrutinib as a front-line therapy did not produce any complete remissions (24). Second, recent genomic profiling studies of CLL patients who acquired resistance to ibrutinib identified resistance mutations in BTK and phospholipase Cγ2 kinase, as well as genetic alterations unrelated to the BCR pathway (25–28). Third, while lymph nodes shrink after ibrutinib therapy, the disease is not cleared efficiently from the bone marrow (22).
To overcome these limitations, we performed a pharmacologic profiling in residual circulating CLL cells after ibrutinib therapy to identify agents that could induce cell death of these lymphocytes. These post-ibrutinib CLL cells were incubated with phosphatidylinositol-3 kinase (PI3K) inhibitors (idelalisib or IPI-145), a chemotherapeutic agent (bendamustine), additional ibrutinib, BCL-2 antagonist (venetoclax, ABT-199), or BCL-2 and BCL-XL antagonist (ABT-737). The BCL-2 antagonists (especially ABT-199) most effectively induced cell death during ex vivo incubations. In accordance with these results, the in vitro combination of ibrutinib and a BCL-2 antagonist showed additive or more than additive cytotoxicity. Serial samples of CLL cells obtained from patients on clinical trial, before (base line) and after (at 2, 4, 12 and 36 weeks) ibrutinib therapy initiation, showed inhibition of BTK activity, decreased MCL-1 protein, and increased sensitivity to the BCL-2 antagonists. Collectively, among the agents tested, our results identified ABT-199 as an ideal partner to be combined with ibrutinib.
Materials and Methods
Drugs and Reagents
Ibrutinib and ABT-199 were respectively purchased from Selleckchem (Houston, TX) and Xcessbio (San Diego, CA), while ABT-737 was provided by Abbott (Park, IL). Goat F(ab′)2 fragments to human IgM was purchased from MP Biomedicals (Santa Ana, CA).
Isolation of Lymphocytes
All experiments were carried out using freshly isolated cells from peripheral blood of patients with CLL. After isolation, cells were immediately suspended in warm medium; there was no interval freezing. Patients gave written informed consent to participate in this laboratory protocol, which was approved by the institutional review board of MD Anderson Cancer Center. Cells were isolated using Ficoll-Hypaque (Life Technologies, Grand Island, NY) as described (18). The isolated lymphocytes were resuspended (1 x 107 cells/mL) in RPMI-1640 medium supplemented with 10% human AB serum (Cambrex Biosciences, East Rutherford, NJ). The cell number and mean cell volume were determined using a Coulter Channelyzer (Coulter Electronics, Hialeah, FL).
Sample Collection during Clinical Trial
For ex vivo incubations and for serial sampling, blood samples were obtained from patients enrolled in ibrutinib trials. All patients received 420 mg of ibrutinib per day, and samples were collected before and/or at 2, 4, and 12 weeks after start of ibrutinib treatment. Collection of blood sample at baseline and at 36 weeks post ibrutinib therapy (used for Supplementary Figure 3) was also done at Ohio State University using an IRB approved clinical protocol.
Cell Death Assessment
After in vitro or ex vivo treatments, CLL cells were resuspended in binding buffer (Roche, Indianapolis, IN) and stained with Annexin V (BD Pharmingen, San Diego, CA) plus propidium iodide (PI; Sigma-Aldrich, St. Louis, MO). Cells were measured using a Becton Dickinson FACSCalibur flow cytometer (San Jose, CA). A time-matched control was treated with DMSO alone and % cell death obtained in this control was subtracted from drug-treated value.
Immunoblot Assays
Treated or untreated cells were lysed using Complete Mini Protease Inhibitor Cocktail (Roche) in RIPA buffer (Bio-Rad, Hercules, CA). Protein content was measured using a DC protein assay kit (Bio-Rad). Protein samples were electrophoresed on Criterion bis-Tris gels using XT MOPS buffer (Bio-Rad) and transferred to nitrocellulose membranes. Multiple proteins of similar size were analyzed using stripping and re-probing of the membrane. Primary antibodies to detect total and phosphorylated proteins and their sources are listed (Supplementary Table S1).
Gene Expression Assay
RNA was isolated using the RNAeasy kit (Qiagen, Valencia, CA), and relative transcript levels of gene expression were assessed using TaqMan One Step RT-PCR (Applied Biosystems, Foster City, CA). Predesigned primers and probes are listed (Supplementary Table S1). Experiments were done in triplicate, and the results were plotted as fold change compared to control.
Reverse-Phase Protein Array (RPPA)
Protein lysates from CLL cells from patients on clinical trials were arrayed on nitrocellulose coated slides and were probed with antibodies. The signal obtained was amplified using a Dako Cytomation–catalyzed system (Dako, Carpinteria, CA). Relative protein levels were determined by interpolation of each dilution curve, and all data were normalized for protein loading. Linear mixed-effect modeling was used to assess the differences in protein expression. This model includes the fixed effect of time point (2 levels: pre- vs. post-treatment) and the random effect of patient. To account for multiple testing, we estimated the false discovery rates of the F-tests of the time point effect using the Benjamini-Hochberg method (29).
TCL1 CLL Adoptive Transfer Mouse Model
We used a TCL1 adoptive transfer CLL mouse model with a TCL1 leukemic clone (TCL1-192) that expresses BCR-reactive malignant cells (30). Spleen cells were provided by Dr. Chiorazzi (Feinstein Institute for Medical Research, Manhasset, NY). Once mice developed the disease, CLL cells were obtained from mouse blood and incubated with no drug, ibrutinib, ABT-199, and ibrutinib plus ABT-199. Flow cytometry analyses were done for Annexin V/PI staining to quantitate percent apoptosis and for the CLL B-cell markers CD5 and B220.
Statistical Analysis and Determination of Drug Interactions
Statistical tests were done using GraphPad Prism (GraphPad Software, San Diego, CA). For calculation of ibrutinib and second drug interaction, we used the fractional product method described by JL Webb. The fractional product was used to determine whether the effect on cell viability and apoptosis induced by the combinations was additive/synergistic/antagonistic. This method is appropriate when nonexclusive drugs (agents with independent mechanisms of action) are combined.
Results
Ex vivo studies of post-ibrutinib residual circulating CLL cells
Blood from patient #595, who had been treated with ibrutinib for 4 weeks, was obtained and lymphocytes were isolated and incubated ex vivo for 24 hours with 6 drugs at the indicated concentrations and cell death was measured. The level of endogenous cell death was subtracted from each sample. ABT-737 and ABT-199 (5 and 10 nM) resulted in >60% apoptosis, while a low cytotoxic effect was observed for the other agents (Fig. 1A). In order to confirm this pattern of cytotoxicity, we obtained blood samples from 10 additional patients who had received ibrutinib for 4 weeks and incubated their lymphocytes in the same manner (Fig. 1B). Overall, ABT-199 was the most potent cytotoxic agent (median cell death: 61%), followed by ABT-737 (median cell death: 33%) (Fig. 1B and Supplementary Table S2), regardless of the patients’ cytogenetics, disease stage, and previous treatment (Supplementary Table S3). Significant cytotoxicity was determined for ABT-199 when it was compared to the rest of agents including ABT-737 (Fig. 1B, p value < 0.004). Still, excluding ABT-199, when compared to the other agents, ABT-737 also induced significant cell death. Altogether, these data suggest that BCL-2 inhibition is effective in ibrutinib-treated lymphocytes.
Figure 1. Ex vivo studies in circulating residual CLL cells from patients enrolled in an ibrutinib clinical trial.
A, Lymphocytes isolated from 1 ibrutinib-treated CLL patient (#595) were incubated ex vivo for 24 hours with therapeutic agents currently in clinical trials or approved for CLL: inhibitors of PI3K (idelalisib [GS1101; GS] and IPI-145), BTK inhibitor (ibrutinib [IB]), BCL-2 antagonists (ABT-737 and ABT-199), and an alkylating agent (bendamustine [Benda]). The concentrations of the drugs are shown on the abscissa. After the incubation period, cell death was determined by Annexin V / PI staining using flow cytometry. Untreated (U) and vehicle-treated (V) cells were also included for each experiment. The level of endogenous cell death, determined in vehicle control (DMSO)-treated cultures, was subtracted from all treatments in each sample to determine the cytotoxicity exerted only by the agents. B, Additional CLL cells were isolated from peripheral blood obtained from patients (n=10) who had received ibrutinib for 4 weeks and were treated ex vivo under the same conditions as in Figure 1A. C and D, Lymphocytes were isolated from the blood of patients who had received ibrutinib for 2, 4, and 12 weeks and were treated with ABT-737 (C) and ABT-199 (D) ex vivo for 24 hours. Cell death was measured and plotted as described for Fig. 1A.
To determine if the ABTs’ cytotoxicity could be replicated at earlier and later time points, we isolated lymphocytes from peripheral blood collected at shorter and longer times after patients began ibrutinib treatment. The rates of ABT-737-mediated cell death were a median 47%, 33%, and 38% in samples collected at 2 (n=2), 4 (n= 9), and 12 weeks (n=7) post-ibrutinib, respectively (Fig. 1C, Supplementary Table S4). Comparison of week 4 data with week 12 data suggested similar extent of cell death (p = 0.98). Similar to ABT-737, ex vivo treatment with ABT-199 resulted in median 49%, 62%, and 58% cell death in week 2 (n=2), week 4 (n= 9), and week 12 samples (n=8) (Fig. 1D, Supplementary Table S4), and was similar at week 4 and 12 (p = 0.84). Comparison of data with ABT-737 and ABT-199 demonstrated that ABT-199 is more potent. Collectively, these data suggest that CLL lymphocytes are sensitive to BCL-2 inhibition regardless of ibrutinib treatment duration or patient characteristics (Supplementary Table S3) and that ABT-199 is the more potent agent under these conditions.
In vitro studies in lymphocytes from ibrutinib-naïve CLL patients
To determine if the ex vivo results could be recapitulated in vitro, we studied lymphocytes from ibrutinib-naïve CLL patients. To determine optimal concentrations to use, we calculated the IC50 values of ibrutinib and the BCL-2 antagonists alone and in combination; the IC50 value for ibrutinib was ~10 μM (Fig. 2A), while those for ABT-737 (Fig. 2B) and ABT-199 (Fig. 2C) were 6 and 2 nM, respectively. It should be noted that of this 10 μM ibrutinib, >97% is protein bound. Hence the free concentration of the drug is below 0.3 μM, which is clinically achievable (22). Ibrutinib at 5 μM induced 8, 3, 11, and 12% cell death in patient samples, 146J, 403, 087, and 592, respectively. At 10 μM this resulted in undetectable, 15, 30 and 24% apoptosis, respectively. When combined with 5 μM ibrutinib, the IC50 values of ABT-737 and ABT-199 dropped to 2 and 1 nM (Fig. 2D–F). In addition, when combined with 10 μM ibrutinib, the IC50 values of ABT-737 and ABT-199 dropped to 1 and 0.5 nM, respectively (Fig. 2E–G). These data suggest that ibrutinib enhances ABT-199 and ABT-737-induced cytotoxicity. To maintain equimolar doses and physiologically achievable values, we selected 1 nM for both ABTs in all combination experiments and 10 μM for ibrutinib.
Figure 2. In vitro studies in CLL lymphocytes obtained from blood of ibrutinib-naïve CLL patients.
A–C, IC50 values were calculated for ibrutinib (A), ABT-737 (B), and ABT-199 (C). For this, CLL cells were incubated with the individual drugs at various concentrations, and cell viability was then tested using Annexin V/PI staining. D–G, A second IC50 assessment was performed for the combinations using 2 ibrutinib concentrations, 5 and 10 μM, with ABT-737 (D, E) and ABT-199 (F, G). Cells were incubated with escalating concentrations of ABT-737 and a fixed concentration of ibrutinib, 5 μM (D) or 10 μM (E), or with escalating doses of ABT-199 and a fixed concentration of ibrutinib, 5 μM (F) and 10 μM (G). Cell death was measured as described before. H and I, Assessment of combination. (H) Lymphocytes were left untreated (Unt) or incubated with the vehicle DMSO (0), ABT-737, ibrutinib, or the combination of ABT-737 plus ibrutinib for 24 hours. A parallel experiment of the same 4 treatments was done in cells stimulated with 10 μg/mL anti-IgM 30 min after vehicle, ibrutinib, or ABT-737 was added to the culture. (I) Conditions similar to those described in Fig. 2H were followed, except ABT-737 was replaced with ABT-199. Cell death was measured as described before. J, Changes in levels of phosphorylated and total protein after in vitro incubations. Immunoblots were obtained after 24 hours of incubation of CLL cells from patient #424 with single-agent ibrutinib in the absence (left panel) or presence (right panel) of anti-IgM (added 30 minutes after ibrutinib); analyzing for targets in the BTK signaling pathway and BCL-2 family proteins. Only one GAPDH was needed because all proteins were done from same gel and membrane by cutting in several sections and using antibodies from different species. We use a fluorescence based imaging system, LiCor Odyssey system to analyze our immunoblots. With this system, our secondary antibodies against primary antibodies derived from different species are tagged with different fluorescence colors.
To define the in vitro cytotoxic impact of the combination strategy, we incubated CLL cells with vehicle (DMSO), ibrutinib, an ABT, and their combination for 24 hours (Fig. 2H–I). To investigate the role of ibrutinib when the BCR pathway is active, we conducted a parallel experiment of the same 4 treatments in cells stimulated with 10 μg/mL anti-IgM. This stimulation always resulted in less cell death. Still, both combination treatments (ibrutinib plus ABT-737 or ABT-199) were more cytotoxic than the single agents (Fig. 2H–I). Similar studies were performed in additional primary CLL samples (Table 1). The combination of ABT-737 and ibrutinib in the absence of anti-IgM stimulation resulted in a cytotoxic range of 15–45% similar to the expected cell death range (13–44%). While in the presence of IgM, the observed range of cell death was 4–47%, which was higher than the expected value (2–38%). The combination of ABT-199 and ibrutinib in the absence of anti-IgM stimulation resulted in 36–63% cell death, which was higher than expected (23–53%). Similar results were observed in the stimulation treatments (8–60%), with rates of cell death higher than expected (3–50%). These data suggest that the combination of ibrutinib and an ABT is more cytotoxic against CLL cells than any of the agents alone, regardless of whether BCR is active and independent of the patients’ cytogenetics (Supplementary Table S3); the combined level of cytotoxicity was either additive or synergistic.
Table 1. In vitro evaluation of ABT-199 and ABT-737 in combination with ibrutinib using previously untreated lymphocyte samples.
CLL cells were obtained from several patients and were treated with DMSO (vehicle), 1 nM ABT-737 or ABT-199, 10 μM ibrutinib, or a combination of ibrutinib and an ABT for 24 hours in the absence or presence of IgM. Total cell death was determined by flow cytometry, and endogenous cell death observed in DMSO control was subtracted from the drug-treated conditions. The expected percentage of cells surviving after treatment with the combination was calculated using fractional two-drug combinational analysis. P values compare expected versus observed cell death for each of the combinations with or without IgM stimulation.
To compare the expected and observed (Annexin V/PI staining) levels of cell death for the combination treatments, we first calculated the expected level of cell survival for each combination. This was done by multiplying the percentage of cells surviving ibrutinib treatment (100% - X% Annexin V/PI staining) by the percentage of cells surviving ABT-199 or ABT-737 treatment (100% - X% Annexin V/PI staining) and then dividing the result by 100.
| Non stimulated | IgM stimulated | Non stimulated | IgM stimulated | |||||
|---|---|---|---|---|---|---|---|---|
| CLL patient | ABT-737 1nM + Ibrutinib 10μM % Cell Death |
ABT-737 1nM + Ibrutinib 10μM % Cell Death |
ABT-199 1nM + Ibrutinib 10μM % Cell Death |
ABT-199 1nM + Ibrutinib 10μM % Cell Death |
||||
| # 403 | Expected | Observed | Expected Observed | Expected | Observed | Expected | Observed | |
| 19 | 25 | 25 | 40 | |||||
| 87 | 44 | 43 | 53 | 52 | ||||
| 592 | 39 | 42 | 49 | 54 | ||||
| 270 | 2 | 4 | 3 | 8 | ||||
| 288 | 38 | 47 | 49 | 54 | ||||
| 868 | 50 | 50 | 32 | 46 | ||||
| 103 | 13 | 20 | 31 | 32 | ||||
| 279 | 37 | 40 | 28 | 38 | 51 | 50 | 50 | 60 |
| 833 | 21 | 25 | 37 | 45 | ||||
| 189 | 48 | 63 | 44 | 53 | ||||
| 424 | 25 | 33 | 25 | 32 | 44 | 47 | 38 | 50 |
| 256 | 24 | 26 | 23 | 27 | 34 | 41 | 31 | 35 |
| 202 | 37 | 45 | 30 | 43 | 51 | 50 | 48 | 52 |
| 75 | 23 | 21 | 16 | 23 | 45 | 41 | 38 | 39 |
| 625 | 13 | 15 | 12 | 13 | 23 | 36 | 14 | 26 |
| p = 0.04; n = 9 | p = 0.0004; n = 10 | p = 0.05; n = 11 | p = 0.0002; n = 12 | |||||
The molecular impact of ibrutinib on CLL cells in the absence or presence of anti-IgM was analyzed by immunoblots evaluating for targets in the BTK signaling pathway and BCL-2 family proteins prevalent in CLL cells. IgM stimulation resulted in phosphorylation (activation) of p-BTK-Y223, p-AKT-S473, and pERK-T202/Y204 (Fig. 2J). Activation of these kinases was abrogated in ibrutinib-incubated CLL cells. Interestingly, our results showed heterogeneity in MCL-1 and BCL-XL protein levels at 24 hour of ibrutinib treatment in 5 non-stimulated CLL samples (Supplementary Fig. S1). As expected, BCL-2 protein levels did not change in any sample (Supplementary Fig. S1). Similarly, mRNA levels were determined for MCL-1, BCL-XL, and BCL-2 (Supplementary Fig. S2A–C). Real-time reverse transcriptase polymerase chain reaction (RT-PCR) data showed no consistent change in MCL-1 and BCL-XL and BCL-2 mRNA levels in the same samples. Collectively, these data suggest that ibrutinib can abrogate BTK activation when stimulatory antigens are present; however, in the absence of IgM, ibrutinib has a heterogeneous effect on the antiapoptotic proteins that drive CLL pathogenesis.
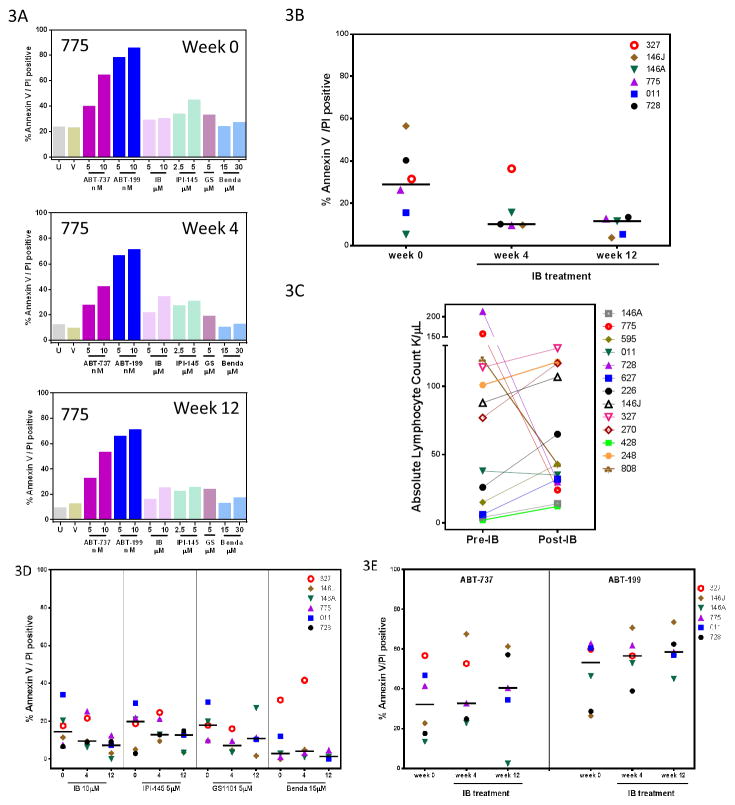
Ex vivo studies of pre- and post-ibrutinib residual circulating CLL cells
To establish if lymphocytes differed in drug sensitivity before and after ibrutinib therapy, we collected a sample (from patient #775) at weeks 0 (pre-ibrutinib), 4, and 12 (post-ibrutinib) (Fig. 3A). ABT-737 and especially ABT-199 resulted in increased cell death compared to the other agents regardless of ibrutinib treatment time. To confirm these results, we collected 5 additional patient samples for the same weeks and tested them under similar conditions with all 6 drugs as well as with vehicle (DMSO) control. Endogenous cell death (in vehicle control sample) was higher in pre-ibrutinib lymphocyte sample (median endogenous cell death, 29%, range 5–57%) than in sample 4-weeks post-ibrutinib (median 10%, range 10–36%) and sample 12-week post-ibrutinib(median 12%, range: 4–13%) (Fig. 3B). The level of endogenous cell death was not associated with the increase or decrease in lymphocyte count after ibrutinib therapy (Fig. 3C). Except in 1 patient (#327) treated with bendamustine, all drugs elicited <40% cytotoxicity (Fig. 3D). ABT-737- and ABT-199-induced cytotoxicity was plotted for the same 6 CLL samples at weeks 0, 4, and 12 (Fig. 3E). ABT-737-mediated median cell death was similar in pre-ibrutinib and post-ibrutinib CLL samples (Supplementary Table S5). ABT-199 treatment yielded higher levels of cell death overall, but the values were similar in pre-ibrutinib samples (median, 53%) and samples obtained at 4 weeks (57%) and 12 weeks (59%) after the start of ibrutinib therapy (Supplementary Table S5). Samples obtained at 36 weeks and treated at a separate site (Ohio State University) also showed similar extent of sensitivity to ABT-199 (median 58% apoptosis; Supplementary Fig. S3). These data suggest that lymphocytes prior to ibrutinib or residual CLL cells post-ibrutinib are similarly sensitive to ABT-induced cytotoxicity. Furthermore, both the in vitro and ex vivo studies demonstrated that ABT-199 is more potent than ABT-737.
Figure 3. Ex vivo studies in cells obtained from the blood of CLL patients before and after ibrutinib therapy.
A, Lymphocytes were isolated from the blood of a CLL patient (#775) collected at weeks 0 (pre-ibrutinib; top panel), 4 (post-ibrutinib; middle panel), and 12 (post-ibrutinib; bottom panel). Cells were left untreated (U) or treated with vehicle (V), ABT-199, ABT-737, ibrutinib (IB), IPI-145, GS1101 (GS), and bendamustine (Benda) at the indicated concentrations for 24 hours. Annexin V /PI staining was performed by flow cytometry to determine cell death level. B, Endogenous cell death in CLL cells before and after ibrutinib therapy was assessed after 24 hour in vitro incubations in lymphocytes isolated from 6 patient samples on pre- (week 0) and post- (weeks 4 and 12) ibrutinib therapy. C, Peripheral blood was obtained from CLL patients (n= 13) before ibrutinib treatment (Pre-IB) and 4 weeks after ibrutinib administration was initiated (Post-IB). The absolute lymphocyte count for each sample was determined from clinical blood count was determined and is plotted as 1000 lymphocytes per microliter (μL) of blood. D, Six CLL patient samples were collected at weeks 0, 4, and 12 of ibrutinib treatment, and lymphocytes isolated and treated under the same conditions described for Fig. 3A. E, Cytotoxicity exerted by ex vivo treatment with ABT-737 and ABT-199 on lymphocytes isolated at weeks 0, 4, and 12 of ibrutinib treatment.
Immunoblots were performed in lymphocytes obtained from patients on ibrutinib treatment. Ibrutinib administration resulted in inhibition of BTK activity in primary CLL cells, as shown by the decrease in autophosphorylation at p-BTK-Y223 (Fig. 4A–B). To evaluate the impact of this inhibition on changes in the levels of BCL-2 family proteins, we performed reverse phase protein array (RPPA) in the same freshly obtained CLL cells isolated from peripheral blood of patients receiving ibrutinib. There was a consistent and significant decline in MCL-1 protein levels (Fig. 5A, p=0.0042), with some changes in BCL-XL and BCL-2 (Fig. 5B–C, respectively). Immunoblot assays followed by quantitation validated the RPPA results. For example, levels of antiapoptotic proteins MCL-1 and BCL-XL (Fig. 5D) declined significantly after 4 and 12 weeks of ibrutinib therapy (Fig. 5E–F, respectively). In contrast, BCL-2 (Fig. 5D and 5G) levels showed no consistent decrease or increase after ibrutinib therapy on the 6 analyzed CLL samples. This was not related to cytogenetics, prognostic factor, or disease state. Levels of Bim, total and p-ERK1/2-T202/Y204, and total and p-AKT-S473 (Supplementary Fig. S4) remained unchanged or showed heterogeneity in response to ibrutinib therapy (quantitation of phosphorylated versus total AKT and ERK proteins are provided below the immunoblot).
Figure 4. Total and phospho BTK protein levels in cells obtained from the blood of CLL patients before and after ibrutinib therapy.
A, Immunoblots analyzing for p-BTK-Y223 and total BTK protein levels in untreated lymphocytes isolated from patients before (week 0) and after ibrutinib (weeks 2, 4, and 12) initiation. Both total and phospho-BTK were from the same gel. Since the antibodies were from the same species, the membrane was stripped and re-probed. We use a fluorescence based imaging system, LiCor Odyssey system to analyze our immunoblots. B, Quantitation was performed for each band, and results plotted as change compared to control (week 0) for each post-ibrutinib sample (weeks 2, 4, or 12) and plotted for p-BTK.
Figure 5. Antiapoptotic protein and transcript levels in cells obtained from the blood of CLL patients before and after ibrutinib therapy.
A–C, Lymphocytes were isolated from the peripheral blood of 6 CLL patients prior to and after therapy with ibrutinib for up to 12 weeks. Cell pellets for RPPA analysis were collected right after lymphocyte isolation (no in vitro drug treatment was performed on these cells). The plots show normalized linear data for the 3 proteins of interest, MCL-1 (A), BCL-XL (B), and BCL-2 (C). D–G, Immunoblots analyzing for MCL-1, BCL-XL, and BCL-2 (D) protein levels in untreated lymphocytes isolated from patients before (week 0) and after ibrutinib (weeks 2, 4, and 12) initiation. All three BCL-2 antiapoptotic proteins were from the same gel and were visualized using antibodies from different species. We use a fluorescence based imaging system, LiCor Odyssey system to analyze our immunoblots. With this system, our secondary antibodies against primary antibodies derived from different species are tagged with different fluorescence colors. Quantitation was performed for each band, and results plotted as change compared to control (week 0) for each post-ibrutinib sample (weeks 2, 4, or 12) and plotted for MCL-1 (E), BCL-XL (F), and BCL-2 (G). P values are from paired t-tests comparing pre- and post-ibrutinib levels of the proteins in samples from all patients. H–J, Real time RT-PCR analysis of MCL-1 (H), BCL-XL(I), and BCL-2 (J) mRNA levels in untreated lymphocytes isolated from patients before (week 0) and after ibrutinib (weeks 2, 4, and 12) initiation. mRNA levels are expressed as fold change over week 0 (pretreatment) for each sample. Eukaryotic 18S ribosomal RNA was used as an internal control.
RT-PCR analyses for the antiapoptotic proteins MCL-1, BCL-XL, and BCL-2 were performed to determine if the decrease observed at the protein level was due to diminished mRNA levels. Only 4 of 6 samples showed a decline in MCL-1 and BCL-XL transcript levels; BCL-2 results were heterogeneous (Fig. 5H–J, respectively).
In vitro studies in lymphocytes from TCL1 mouse model
To determine if the human CLL cell studies could be recapitulated in lymphocytes derived from a CLL mouse model, cells from the TCL1 mouse were isolated and incubated with ABT-199 (0.5 and 1nM) and ibrutinib (10 μM) for 24 hours. These data resulted in an additive or more than additive cell death as assessed by Annexin V/PI staining (Supplementary Fig. S5), which is consistent with human CLL cell studies (Table 1).
Discussion
Ibrutinib has revolutionized how we treat CLL; it targets the very pathway that is involved in production and maintenance of B-lymphocytes. Ibrutinib covalently binds and inhibits BTK, which is critical in the BCR pathway. Recent investigations have identified that signaling proteins in the BCR axis not only play a pivotal role in the development of normal and malignant B-cells but also become mutated or modified in CLL cells from patients whose disease is becoming resistant to ibrutinib (25–28). Hence, targeting additional elements in the BCR pathway could result in increased cytotoxicity. Idelalisib (GS1101) targets the p110 delta isoform of PI3K, while IPI-145 targets both delta and gamma isoforms (31, 32). These PI3K subunits are expressed at high levels primarily in lymphocytes, providing selectivity with these inhibitors. Because these kinases dominate the BCR pathway, they were primary molecules for our testing. Consistent with the data with idelalisib and IPI-145, additional ibrutinib also did not provide increased cytotoxic benefit (Fig. 1B and 3D). While these inhibitors may provide an advantage in the clinic by mobilizing CLL cells from the lymph nodes, our primary goal was to induce cell death in cells that are either mobilized or residual after ibrutinib. Furthermore, the kinase inhibitors may be effective for ibrutinib-resistant CLL clone (33). Bendamustine, an approved and well-tolerated alkylating agent for CLL, also was not a stimulator for cell death (34). In contrast to these above tested agents, inhibition of BCL-2 consistently resulted in induction of cell death. Furthermore, between the two BH3-mimetics, ABT-199 unfailingly produced the higher percentage of cell death.
For the current investigation, we selected 6 drugs based on their current use for treatment of CLL and mechanistic rationale to combine with ibrutinib. Earlier preliminary investigations in ibrutinib-treated CLL patient samples identified transcription inhibitor, dinaciclib, that targets cyclin-dependent kinase (CDK) inhibitor as a potent cell death inducer in these lymphocytes (35). In contrast, similar to present investigation, kinase inhibitors that impact components of BCR pathway did not induce apoptosis. Recent investigations using similar model system suggested carfilzomib, an endoplasmic reticulum (ER) stress agent, as a potential partner with ibrutinib (36). The positive interaction between these drugs was prevalent at different times after start of ibrutinib. For example in our studies, cells obtained after week 2, 4, 12 (Fig. 1C and 1D), and 36 (Supplementary Fig. S3) showed similar cell death with ABT-199. Because, ABT-199-mediated cytotoxicity was similar in pre- and post-ibrutinib samples, these data suggest that most of the cell death response is generated by ABT-199. Similar to CLL model system, major efforts have been utilized in other B-cell malignancies where ibrutinib and BCL-2 antagonists have shown promising activity in B-cell diseases such as mantle cell lymphoma (37), Waldenstrom’s macroglobulinaemia (38), and diffuse-large B-cell lymphoma (39). Ibrutinib’s primary action on cell proliferation is in concert with co-operation with transcription inhibitor dinaciclib, ER stressor carfilzomib, and BCL-2 antagonist, ABT-199. These reports direct us to recognizing best small molecule combination drug partner with ibrutinib. However, combination strategies that pair ibrutinib with rituximab, GA101, or ofatumumab warrant preclinical testing especially because efficacy with antibodies to treat CLL has been shown in the clinic and these agents are FDA approved (40).
While detailed mechanistic studies were not performed, CLL biology, characteristics of these agents, and the results obtained with these combinations provide clues to explain these cell death differences. Among the 6 BCL-2 family survival proteins, BCL-2, BCL-XL, and MCL-1 are the most abundant in CLL cells (41). In addition, among these 3 proteins, BCL-2 and BCL-XL are present at levels 4–12 times higher than MCL-1(42). While ABT-737 targets and binds with high affinity (Ki ≤ 1 nM) to the hydrophobic BH3-binding groove of BCL-XL, BCL-2, and BCL-w (43); ABT-199 targets only BCL-2 with much higher potency (Ki ≤ 0.01 nM) (44). Prolonged and potent perturbation of either BCL-2 or BCL-XL should result in apoptosis, as the overall stoichiometry of these molecules is a determinant of CLL cell survival or death (37). Ibrutinib and ABT-737 cooperated well in DLBCL (39). Finally, our data suggest that ibrutinib therapy constantly causes an intracellular MCL-1 decrease (Fig. 5A, 5D, and 5E), which may further augment ABT-199-induced apoptosis. While detailed time kinetics were not captured in our investigations, at 4 and 12 weeks after ibrutinib initiation, CLL cells consistently showed a decline in MCL-1 protein levels in RPPA and immunoblot assays (Fig. 5A, 5D, 5E). This result however was not observed during in vitro incubations, which can be attributed to limited incubation time (24 hour for in vitro assays versus minimum 2 weeks for in vivo studies) with ibrutinib (Supplementary Fig. S1). MCL-1 protein decrease or induction of pro-apoptotic protein Noxa by dinaciclib and carfilzomib, respectively may be the primary mechanisms for increased cell death.
The decline in MCL-1 protein level was partly (4 of 6 samples) associated with a decrease in MCL-1 transcript level in post-ibrutinib samples (Fig. 5H). The BCR pathway, including the PI3K/AKT axis, has been shown to impact transcriptional, translational, and post-translational modifications of MCL-1, resulting in increased transcription, over-expression of protein and longer maintenance of protein (45–47). Both during in vitro incubations (Fig. 2J) and especially during clinical trials (Fig. 4A–B), ibrutinib reliably inhibited BTK activity (measured as p-BTK). Our results are in accordance with a previous study showing a decrease in BTK phosphorylation in circulating CLL cells during therapy and consistent with the observation that at a dose of 420 mg/day, ibrutinib completely occupied the BTK binding pocket (14, 35). Hence, it can be presumed that the BTK pathway would be abrogated in the leukemia cells of these CLL patients, impacting transcriptional and translational modifications of MCL-1 and other proteins.
Inhibition of BTK pathway resulted in unexpected increase in circulating leukemia cells that were due to mobilization of lymphocytes from lymph nodes (22). It has been established that at the molecular level, there are differences in malignant CLL lymphocytes from peripheral blood, bone marrow, and lymph nodes. An increased BCR signature, proliferation markers, and NF-kB activity was identified in gene expression array analyses in cells from lymph node compared to those from marrow or blood (4). Furthermore, transcripts such as STAT-1, MYC, FOS, AKT and BCL-2 were also several fold higher in lymph node CLL cells compared to those from other compartments (48). Increased expression of BCL-2 transcript is of specific interest because this protein assists CLL cells to survive longer. Compared to the baseline samples, in the ibrutinib-therapy-mediated lymphocytosed cells, we observed either similar or an increased expression of BCL-2 protein measured by RPPA assay (Fig. 5C) and validated by immunoblot assay (Fig. 5G).
To mimic these ex vivo studies, we performed in vitro combination cytotoxicity assays by combining BH3 mimetics with ibrutinib. To model BCR stimulation, parallel cultures were anti-IgM stimulated. Compared to expected cytotoxicity, calculated based on single agent response in each sample, the observed cytotoxicity was significantly higher. The extent of this difference was strongest when cells were stimulated for the BCR pathway (p values = 0.0004 and 0.0002 with ABT-737 and ABT-199, respectively, Table 1). Collectively these in vitro and ex vivo results demonstrate the utility and benefit of combining ABT-199 with ibrutinib in the clinic. Translation of these preclinical results to clinic should be feasible. The clinically-decided dose of ibrutinib for CLL (420 mg) is well-tolerated and is actually below the maximum tolerated dose. At this dose, the peak plasma concentration of free drug is around 80 ng/ml; equivalent to 0.2 μM. While in the present work, ibrutinib is used at 10 μM, due to serum/plasma protein binding, the free drug is less than 3% (i.e. 0.3 μM) which is similar to what is acquired during therapy (22). Similarly, the concentration of ABT-199 in our experiments was 1–10 nM, which is easily achievable in the clinic (44, 49).
While these ex vivo investigations of CLL cells during ibrutinib therapy provide a novel and unique cell population to identify small molecule drugs that collaborate well with ibrutinib, there are limitations of this system. First, we only used annexin/PI positivity to identify partner agent for ibrutinib. It is highly likely that agents which may not induce profound CLL lymphocyte death will be missed during such interrogations. Second, CLL cells pre and post ibrutinib are non-proliferative during ex vivo or in vitro culturing. Needless to say that in such a model system, agents that are tackling cell proliferation would not be identified. Third, pathways such as PI3K, AKT, mTOR, and NF-kB that may be critical in CLL biology were not tested during these incubations. Investigations on impact of these networks may provide other molecules to be added to ibrutinib. Finally, animal model system that can recapitulate CLL cells in different niches and microenvironment (blood, bone-marrow, and lymph node) may provide selective targeted agents to be coupled with ibrutinib.
Even with these shortcomings, our data and prior investigations provide clear rationale that ABT-199 (and ABT-737) is beneficial to ibrutinib therapy. First, among the tested agents, addition of ABT-199 was most conducive in inducing apoptosis. Second, residual or lymphocytosed cells were sensitive to ABT-199-mediated cytotoxicity. Third, compared to base-line (prior to ibrutinib) CLL cells, post-ibrutinib mobilized CLL cells were relatively resistant to cell death (data not shown). However, they were equally sensitive to ABT-199 (Supplementary Table S5). Fourth, at the systemic level, CLL cells reside in 3 different niches in the human body: lymph nodes, bone marrow, and peripheral blood. Ibrutinib preferentially targets the lymph node reservoir, while ABT-199 addresses CLL cells residing in blood and marrow. Early preliminary data (44) and data from a subsequent Phase I study of ABT-199 in patients with high-risk relapsed or refractory CLL (49) reported an overall response rate of 84%, with a complete remission rate of 23%. Notably, ABT-199 resulted in the clearance of leukemia cells from the blood and marrow. In fact, no or low minimum residual disease was observed in 8 patients treated (49). Consequently, these 2 drugs would be beneficial in removing malignant cells from all three compartments.
Our data also suggest that ibrutinib may add benefit to ABT-737 or ABT-199. First, when 2 different doses of ibrutinib were added to ABT-737, the IC50 of ABT-737 changed from 6 nM to 2 nM to 1 nM (Fig. 2B, 2D and 2F). Such reduction in IC50 demonstrates the advantage of adding ibrutinib and it also indicates that in the clinic we can do a dose reduction for ABT-263 which will alleviate drug-induced thromobocytopenia which was problematic for its use. Second, when two different doses of ibrutinib were combined with ABT-199, the IC50 of ABT-199 was reduced from 2 nM to 1 nM to 0.5 nM (Fig. 2C, 2F and 2G). Hence, in clinic, ibrutinib may be combined with lowest dose of ABT-199 as suggested in the current clinical trial in high-risk patients with relapsed/refractory CLL (49). Third, data presented in Table 1, provide cytotoxic basis of synergy when ibrutinib is added to ABT-199 or ABT-737 in IgM stimulated cells (p values = 0.0002 and 0.0004). Fourth, decrease in MCL-1 protein level by ibrutinib (Fig. 5A, 5D, 5E) provides another advantage to ABT-737 and ABT-199 as these BCL-2 antagonists do not target MCL-1 and this has been shown to be one of the mechanisms for resistance to ABT-263 (50). At the cellular and molecular level, our data suggest that by combining these two agents (ibrutinib and ABT-199 or ABT-737) we will target all 3 BCL-2 survival proteins, MCL-1, BCL-XL, and BCL-2. CLL malignant cells have been shown to be addicted to these proteins for their maintenance and survival; for example, an ABT-199 resistant cell line was sensitized to ABT-199 by BCR nexus (such as PI3K, AKT, and mTOR) inhibitors (51). Hence, we postulate that the combination approach described in this study has the potential to eradicate CLL cells and a clinical trial combining these 2 agents is needed to validate this combination.
Supplementary Material
Translational Relevance.
Ibrutinib has revolutionized the way CLL is treated due to its impressive clinical activity in this disease. Despite its clinical effectiveness, the drug does not result in deep remission and has not been able to cure this malignancy. Recent studies have also suggested an emerging mechanism of resistance found in some patients on ibrutinib treatment hence prompting the development of combination strategies. Using residual CLL cells after ibrutinib therapy in our pharmacological profile, we identified that the BCL-2 antagonist ABT-199 was able to augment ibrutinib’s effects making these two drugs a potential combination to use in the clinic. In vitro combination studies further confirmed the synergy.
At the molecular level, our results show ibrutinib therapy reduced MCL-1 and BCL-XL protein levels while ABT-199 targeted BCL-2; hence, this combination targets the three antiapoptotic Bcl-2 family proteins that drive the survival and proliferation of CLL cells.
Acknowledgments
Grant support: VG, KB, and WGW are members of the CLL Research Consortium. This work was supported in part by grant PO1CA81534 and K23CA178183-01 from the NCI, DHHS, a CLL Global Research Foundation award, sponsored research agreement from Pharmacyclics, and generous philanthropic contributions to The University of Texas MD Anderson MoonShot Program.
We thank Kathryn B. Carnes for critically reviewing this manuscript and Miss Chen, Fu, and Datar for transportation of patient samples.
Footnotes
Conflict-of-interest: VG received sponsored research agreement from Pharmacyclics; other authors declare no competing financial interests.
Authorship contributions
FCG performed experiments, analyzed data, and wrote the manuscript. BL and JAW were involved in supporting experiments. MJK and WGW identified and directed obtainment of blood samples from ibrutinib-naïve or during ibrutinib therapy patients with CLL. KB designed research. VG analyzed data, wrote the manuscript, and obtained financial support. All authors reviewed and approved the final version of the manuscript.
References
- 1.Zenz T, Mertens D, Kuppers R, Dohner H, Stilgenbauer S. From pathogenesis to treatment of chronic lymphocytic leukaemia. Nature reviews Cancer. 2010;10:37–50. doi: 10.1038/nrc2764. [DOI] [PubMed] [Google Scholar]
- 2.Chiorazzi N, Rai KR, Ferrarini M. Chronic lymphocytic leukemia. The New England journal of medicine. 2005;352:804–15. doi: 10.1056/NEJMra041720. [DOI] [PubMed] [Google Scholar]
- 3.Burger JA, Quiroga MP, Hartmann E, Burkle A, Wierda WG, Keating MJ, et al. High-level expression of the T-cell chemokines CCL3 and CCL4 by chronic lymphocytic leukemia B cells in nurselike cell cocultures and after BCR stimulation. Blood. 2009;113:3050–8. doi: 10.1182/blood-2008-07-170415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herishanu Y, Perez-Galan P, Liu D, Biancotto A, Pittaluga S, Vire B, et al. The lymph node microenvironment promotes B-cell receptor signaling, NF-kappaB activation, and tumor proliferation in chronic lymphocytic leukemia. Blood. 2011;117:563–74. doi: 10.1182/blood-2010-05-284984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tam CS, O’Brien S, Wierda W, Kantarjian H, Wen S, Do KA, et al. Long-term results of the fludarabine, cyclophosphamide, and rituximab regimen as initial therapy of chronic lymphocytic leukemia. Blood. 2008;112:975–80. doi: 10.1182/blood-2008-02-140582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Montserrat E, Moreno C, Esteve J, Urbano-Ispizua A, Gine E, Bosch F. How I treat refractory CLL. Blood. 2006;107:1276–83. doi: 10.1182/blood-2005-02-0819. [DOI] [PubMed] [Google Scholar]
- 7.Wierda W, O’Brien S, Wen S, Faderl S, Garcia-Manero G, Thomas D, et al. Chemoimmunotherapy with fludarabine, cyclophosphamide, and rituximab for relapsed and refractory chronic lymphocytic leukemia. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2005;23:4070–8. doi: 10.1200/JCO.2005.12.516. [DOI] [PubMed] [Google Scholar]
- 8.Eichhorst BF, Busch R, Stilgenbauer S, Stauch M, Bergmann MA, Ritgen M, et al. First-line therapy with fludarabine compared with chlorambucil does not result in a major benefit for elderly patients with advanced chronic lymphocytic leukemia. Blood. 2009;114:3382–91. doi: 10.1182/blood-2009-02-206185. [DOI] [PubMed] [Google Scholar]
- 9.Stilgenbauer S, Schnaiter A, Paschka P, Zenz T, Rossi M, Dohner K, et al. Gene mutations and treatment outcome in chronic lymphocytic leukemia: results from the CLL8 trial. Blood. 2014;123:3247–54. doi: 10.1182/blood-2014-01-546150. [DOI] [PubMed] [Google Scholar]
- 10.Tam CS, O’Brien S, Plunkett W, Wierda W, Ferrajoli A, Wang X, et al. Long-term results of first salvage treatment in CLL patients treated initially with FCR (fludarabine, cyclophosphamide, rituximab) Blood. 2014;124:3059–64. doi: 10.1182/blood-2014-06-583765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oppezzo P, Dighiero G. Role of the B-cell receptor and the microenvironment in chronic lymphocytic leukemia. Blood cancer journal. 2013;3:e149. doi: 10.1038/bcj.2013.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herman SE, Gordon AL, Hertlein E, Ramanunni A, Zhang X, Jaglowski S, et al. Bruton tyrosine kinase represents a promising therapeutic target for treatment of chronic lymphocytic leukemia and is effectively targeted by PCI-32765. Blood. 2011;117:6287–96. doi: 10.1182/blood-2011-01-328484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burger JA. Inhibiting B-cell receptor signaling pathways in chronic lymphocytic leukemia. Current hematologic malignancy reports. 2012;7:26–33. doi: 10.1007/s11899-011-0104-z. [DOI] [PubMed] [Google Scholar]
- 14.Advani RH, Buggy JJ, Sharman JP, Smith SM, Boyd TE, Grant B, et al. Bruton tyrosine kinase inhibitor ibrutinib (PCI-32765) has significant activity in patients with relapsed/refractory B-cell malignancies. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2013;31:88–94. doi: 10.1200/JCO.2012.42.7906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan Z, Scheerens H, Li SJ, Schultz BE, Sprengeler PA, Burrill LC, et al. Discovery of selective irreversible inhibitors for Bruton’s tyrosine kinase. ChemMedChem. 2007;2:58–61. doi: 10.1002/cmdc.200600221. [DOI] [PubMed] [Google Scholar]
- 16.Honigberg LA, Smith AM, Sirisawad M, Verner E, Loury D, Chang B, et al. The Bruton tyrosine kinase inhibitor PCI-32765 blocks B-cell activation and is efficacious in models of autoimmune disease and B-cell malignancy. Proceedings of the National Academy of Sciences of the United States of America. 2010;107:13075–80. doi: 10.1073/pnas.1004594107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burger JA. Targeting the microenvironment in chronic lymphocytic leukemia is changing the therapeutic landscape. Current opinion in oncology. 2012;24:643–9. doi: 10.1097/CCO.0b013e3283589950. [DOI] [PubMed] [Google Scholar]
- 18.Ponader S, Chen SS, Buggy JJ, Balakrishnan K, Gandhi V, Wierda WG, et al. The Bruton tyrosine kinase inhibitor PCI-32765 thwarts chronic lymphocytic leukemia cell survival and tissue homing in vitro and in vivo. Blood. 2012;119:1182–9. doi: 10.1182/blood-2011-10-386417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Rooij MF, Kuil A, Geest CR, Eldering E, Chang BY, Buggy JJ, et al. The clinically active BTK inhibitor PCI-32765 targets B-cell receptor- and chemokine-controlled adhesion and migration in chronic lymphocytic leukemia. Blood. 2012;119:2590–4. doi: 10.1182/blood-2011-11-390989. [DOI] [PubMed] [Google Scholar]
- 20.Cheng S, Ma J, Guo A, Lu P, Leonard JP, Coleman M, et al. BTK inhibition targets in vivo CLL proliferation through its effects on B-cell receptor signaling activity. Leukemia. 2014;28:649–57. doi: 10.1038/leu.2013.358. [DOI] [PubMed] [Google Scholar]
- 21.Herman SE, Mustafa RZ, Gyamfi JA, Pittaluga S, Chang S, Chang B, et al. Ibrutinib inhibits BCR and NF-kappaB signaling and reduces tumor proliferation in tissue-resident cells of patients with CLL. Blood. 2014;123:3286–95. doi: 10.1182/blood-2014-02-548610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Byrd JC, Furman RR, Coutre SE, Flinn IW, Burger JA, Blum KA, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. The New England journal of medicine. 2013;369:32–42. doi: 10.1056/NEJMoa1215637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Brien S, Furman RR, Coutre SE, Sharman JP, Burger JA, Blum KA, et al. Ibrutinib as initial therapy for elderly patients with chronic lymphocytic leukaemia or small lymphocytic lymphoma: an open-label, multicentre, phase 1b/2 trial. The lancet oncology. 2014;15:48–58. doi: 10.1016/S1470-2045(13)70513-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farooqui MZ, Valdez J, Martyr S, Aue G, Saba N, Niemann CU, et al. Ibrutinib for previously untreated and relapsed or refractory chronic lymphocytic leukaemia with TP53 aberrations: a phase 2, single-arm trial. The lancet oncology. 2015;16:169–76. doi: 10.1016/S1470-2045(14)71182-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chang BY, Furman RR, Zapatka M, Barrientos JC, Li D, Steggerda S, et al. Use of tumor genomic profiling to reveal mechanisms of resistance to the BTK inhibitor ibrutinib in chronic lymphocytic leukemia (CLL) Journal of Clinical Oncology. 2013;(suppl):abstr 7014. [Google Scholar]
- 26.Burger JA, Landau D, Hoellenriegel J, Sougnez C, Schlesner M, Ishaque N, et al. Clonal evolution in patients with chronic lymphocytic leukemia (CLL) developing resistance to BTK inhibition. Blood. 2013;(suppl):abstr 866. [Google Scholar]
- 27.Furman RR, Cheng S, Lu PL, Setty M, Perez A, Guo A, et al. A novel mutation in Bruton tyrosine kinase confers acquired resistance to Ibrutinib (PCI-32765) in CLL. Blood. 2013;(suppl):abstr 4914. [Google Scholar]
- 28.Woyach JA, Furman RR, Liu TM, Ozer HG, Zapatka M, Ruppert AS, et al. Resistance mechanisms for the Bruton’s tyrosine kinase inhibitor ibrutinib. The New England journal of medicine. 2014;370:2286–94. doi: 10.1056/NEJMoa1400029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Edwards LK, editor. Applied Analysis of Variance in the Behavioral Sciences. New York, New York: Marcel Dekker Inc; 1993. [Google Scholar]
- 30.Chen SS, Batliwalla F, Holodick NE, Yan XJ, Yancopoulos S, Croce CM, et al. Autoantigen can promote progression to a more aggressive TCL1 leukemia by selecting variants with enhanced B-cell receptor signaling. Proceedings of the National Academy of Sciences of the United States of America. 2013;110:E1500–7. doi: 10.1073/pnas.1300616110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herman SE, Gordon AL, Wagner AJ, Heerema NA, Zhao W, Flynn JM, et al. Phosphatidylinositol 3-kinase-delta inhibitor CAL-101 shows promising preclinical activity in chronic lymphocytic leukemia by antagonizing intrinsic and extrinsic cellular survival signals. Blood. 2010;116:2078–88. doi: 10.1182/blood-2010-02-271171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Winkler DG, Faia KL, DiNitto JP, Ali JA, White KF, Brophy EE, et al. PI3K-delta and PI3K-gamma inhibition by IPI-145 abrogates immune responses and suppresses activity in autoimmune and inflammatory disease models. Chemistry & biology. 2013;20:1364–74. doi: 10.1016/j.chembiol.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 33.Cheng S, Guo A, Lu P, Ma J, Coleman M, Wang YL. Functional characterization of BTK mutation that confers ibrutinib resistance: exploration of alternative kinase inhibitors. Leukemia. 2014 doi: 10.1038/leu.2014.263. [DOI] [PubMed] [Google Scholar]
- 34.Gandhi V, Burger JA. Bendamustine in B-Cell Malignancies: The New 46-Year-Old Kid on the Block. Clinical cancer research : an official journal of the American Association for Cancer Research. 2009;15:7456–61. doi: 10.1158/1078-0432.CCR-08-3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Woyach JA, Smucker K, Smith LL, Lozanski A, Zhong Y, Ruppert AS, et al. Prolonged lymphocytosis during ibrutinib therapy is associated with distinct molecular characteristics and does not indicate a suboptimal response to therapy. Blood. 2014;123:1810–7. doi: 10.1182/blood-2013-09-527853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lamothe B, Cervantes-Gomez F, Sivina M, Wierda WG, Keating MJ, Gandhi V. Proteasome inhibitor carfilzomib complements ibrutinib’s action in chronic lymphocytic leukemia. Blood. 2015;125:407–10. doi: 10.1182/blood-2014-07-585364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhao X, Bodo J, Sun D, Durkin L, Lin J, Smith MR, et al. Combination of ibrutinib with ABT-199: synergistic effects on proliferation inhibition and apoptosis in mantle cell lymphoma cells through perturbation of BTK, AKT and BCL2 pathways. British journal of haematology. 2015;168:765–8. doi: 10.1111/bjh.13149. [DOI] [PubMed] [Google Scholar]
- 38.Cao Y, Yang G, Hunter ZR, Liu X, Xu L, Chen J, et al. The BCL2 antagonist ABT-199 triggers apoptosis, and augments ibrutinib and idelalisib mediated cytotoxicity in CXCR4 and CXCR4 mutated Waldenstrom macroglobulinaemia cells. British journal of haematology. 2015 doi: 10.1111/bjh.13278. [DOI] [PubMed] [Google Scholar]
- 39.Mathews Griner LA, Guha R, Shinn P, Young RM, Keller JM, Liu D, et al. High-throughput combinatorial screening identifies drugs that cooperate with ibrutinib to kill activated B-cell-like diffuse large B-cell lymphoma cells. Proceedings of the National Academy of Sciences of the United States of America. 2014;111:2349–54. doi: 10.1073/pnas.1311846111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burger JA, Keating MJ, Wierda WG, Hartmann E, Hoellenriegel J, Rosin NY, et al. Safety and activity of ibrutinib plus rituximab for patients with high-risk chronic lymphocytic leukaemia: a single-arm, phase 2 study. The Lancet Oncology. 2014;15:1090–9. doi: 10.1016/S1470-2045(14)70335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Balakrishnan K, Gandhi V. Bcl-2 antagonists: a proof of concept for CLL therapy. Investigational new drugs. 2013;31:1384–94. doi: 10.1007/s10637-013-0002-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Del Gaizo Moore V, Brown JR, Certo M, Love TM, Novina CD, Letai A. Chronic lymphocytic leukemia requires BCL2 to sequester prodeath BIM, explaining sensitivity to BCL2 antagonist ABT-737. The Journal of clinical investigation. 2007;117:112–21. doi: 10.1172/JCI28281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oltersdorf T, Elmore SW, Shoemaker AR, Armstrong RC, Augeri DJ, Belli BA, et al. An inhibitor of Bcl-2 family proteins induces regression of solid tumours. Nature. 2005;435:677–81. doi: 10.1038/nature03579. [DOI] [PubMed] [Google Scholar]
- 44.Souers AJ, Leverson JD, Boghaert ER, Ackler SL, Catron ND, Chen J, et al. ABT-199, a potent and selective BCL-2 inhibitor, achieves antitumor activity while sparing platelets. Nature medicine. 2013;19:202–8. doi: 10.1038/nm.3048. [DOI] [PubMed] [Google Scholar]
- 45.Longo PG, Laurenti L, Gobessi S, Sica S, Leone G, Efremov DG. The Akt/Mcl-1 pathway plays a prominent role in mediating antiapoptotic signals downstream of the B-cell receptor in chronic lymphocytic leukemia B cells. Blood. 2008;111:846–55. doi: 10.1182/blood-2007-05-089037. [DOI] [PubMed] [Google Scholar]
- 46.Petlickovski A, Laurenti L, Li X, Marietti S, Chiusolo P, Sica S, et al. Sustained signaling through the B-cell receptor induces Mcl-1 and promotes survival of chronic lymphocytic leukemia B cells. Blood. 2005;105:4820–7. doi: 10.1182/blood-2004-07-2669. [DOI] [PubMed] [Google Scholar]
- 47.Balakrishnan K, Burger JA, Fu M, Doifode T, Wierda WG, Gandhi V. Regulation of Mcl-1 expression in context to bone marrow stromal microenvironment in chronic lymphocytic leukemia. Neoplasia. 2014;16:1036–46. doi: 10.1016/j.neo.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gilling CE, Mittal AK, Chaturvedi NK, Iqbal J, Aoun P, Bierman PJ, et al. Lymph node-induced immune tolerance in chronic lymphocytic leukaemia: a role for caveolin-1. British journal of haematology. 2012;158:216–31. doi: 10.1111/j.1365-2141.2012.09148.x. [DOI] [PubMed] [Google Scholar]
- 49.Seymour JF, Davids MS, Pagel JM, Pagel JM, Kahl BS, Wierda WG, et al. Bcl-2 inhibitor ABT-199 (GDC-0199) monotherapy shows anti-tumor activity including complete remissions in high-risk relapsed/refractory (R/R) chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL) Blood. 2013;(suppl):abstr 872. [Google Scholar]
- 50.Roberts AW, Seymour JF, Brown JR, Wierda WG, Kipps TJ, Khaw SL, et al. Substantial susceptibility of chronic lymphocytic leukemia to BCL2 inhibition: results of a phase I study of navitoclax in patients with relapsed or refractory disease. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2012;30:488–96. doi: 10.1200/JCO.2011.34.7898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Choudhary GS, Al-Harbi S, Mazumder S, Hill BT, Smith MR, Bodo J, et al. MCL-1 and BCL-xL-dependent resistance to the BCL-2 inhibitor ABT-199 can be overcome by preventing PI3K/AKT/mTOR activation in lymphoid malignancies. Cell death & disease. 2015;6:e1593. doi: 10.1038/cddis.2014.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.