Abstract
Acute Respiratory Distress Syndrome (ARDS) and Acute Lung Injury (ALI) result in high permeability pulmonary edema causing hypoxic respiratory failure with high morbidity and mortality. As the population ages, the incidence of ALI is expected to rise. Over the last decade, several studies have identified biomarkers in plasma and bronchoalveolar lavage fluid providing important insights into the mechanisms involved in the pathophysiology of ALI. Several biomarkers have been validated in subjects from the large, multicenter ARDS clinical trials network. Despite these studies, no single or group of biomarkers has made it into routine clinical practice. New high throughput ‘omics’ techniques promise improved understanding of the biologic processes in the pathogenesis in ALI and possibly new biomarkers that predict disease and outcomes. In this article we review the current knowledge on biomarkers in ALI.
Acute Respiratory Distress in adults was first described by Ashbaugh and Petty in 1967 (1) in a case series of twelve subjects with acute onset of tachypnea, hypoxia and loss of compliance after a variety of stimuli. Subsequent research has increased our understanding of this disease’s pathophysiology (2), epidemiology (3), treatment options (4–11), and outcomes (3, 12), A uniform definition of this syndrome has been adopted for research, epidemiology and clinical care based on a report of the American-European consensus conference on Acute Respiratory Distress Syndrome (ARDS)(13). The incidence of ARDS – and its less severe form, Acute Lung Injury (ALI) – is believed to be 58.7 and 78.9 cases per 100,000 person-years respectively (3) with an estimated 74,500 deaths and 2.2 million ICU days annually. As the U.S. population ages, it is expected that ALI will become an even greater health problem (14).
Over the last two decades biologic markers have revealed novel information about the pathophysiology of lung injury and repair and identified cells and putative mediators involved in ALI. However, despite this new knowledge biomarkers in ALI remain primarily a research tool. The focus of this review is to outline the current state of biomarkers in ALI and ARDS.
Biomarkers
Biomarkers are broadly defined as markers of a biological process or state. A commonly used definition of a biomarker is ‘a characteristic that is objectively measured and evaluated as an indicator of normal biological process, pathogenic processes, or pharmacologic responses to a therapeutic intervention’ (15). Thus clinical parameters such as vital signs, physiological measurements, biochemical or molecular markers could be used as biomarkers to determine its relationship with an endpoint.
Endpoints in Biomarker Research in Acute Lung Injury
Several clinical endpoints for biomarker research have been investigated in critically ill patients with hypoxic respiratory failure from ALI. These end points have focused on the ability to diagnose ALI in high-risk patients or discriminate patients with hydrostatic from high permeability pulmonary edema. Also of interest are identifying subgroups of patients with different outcomes or response to treatment in patients at risk of or with established ALI. As these are surrogate endpoints, the most clinically relevant outcome is mortality and therefore biomarker research has concentrated on prediction of short and long-term mortality in ALI. Besides a potential utility in the clinical arena for diagnosis, stratification and prediction of mortality, biomarkers in ALI could also be used in clinical trials for selection of homogenous patients and as end points.
Statistical basis for use of Biomarkers
The rationale of when to measure laboratory parameters, which marker may be useful, and how to interpret the results are not well defined. It is vital that validation and confirmation of candidate biomarkers by robust statistical methods are performed during biomarker discovery. Sensitivity and specificity are common quality parameters for biomarkers. Sensitivity describes the probability of a positive test in cases and specificity describes probability of negative test in controls. An association between sensitivity and specificity is represented in the receiver-operating characteristic (ROC) by graphing sensitivity versus 100-specificity. Area under the ROC curve (AUROCC) is a measure of performance of a marker. There is no absolute cutoff value of AUROCC for robustness of a marker though a minimum of 0.7 is required and values greater than 0.8 are good particularly in a heterogeneous patient population seen with critical illnesses (16).
An ideal biomarker in ALI should have a clear relationship between the biomarker and the pathophysiological events. The markers would need to be reliable and reproducible, relatively inexpensive, measure changes in response to interventions, have little or no diurnal variation, be sensitive, disease specific with high positive and negative predictive values and be sampled by simple methods. Exhaled breath condensate (17, 18), urine (19, 20), undiluted pulmonary edema fluid (21–23), bronchoalveolar lavage fluid (BALF) and plasma/serum have been studied for biomarker discovery in ALI.
Biomarkers of ARDS/ALI Stages
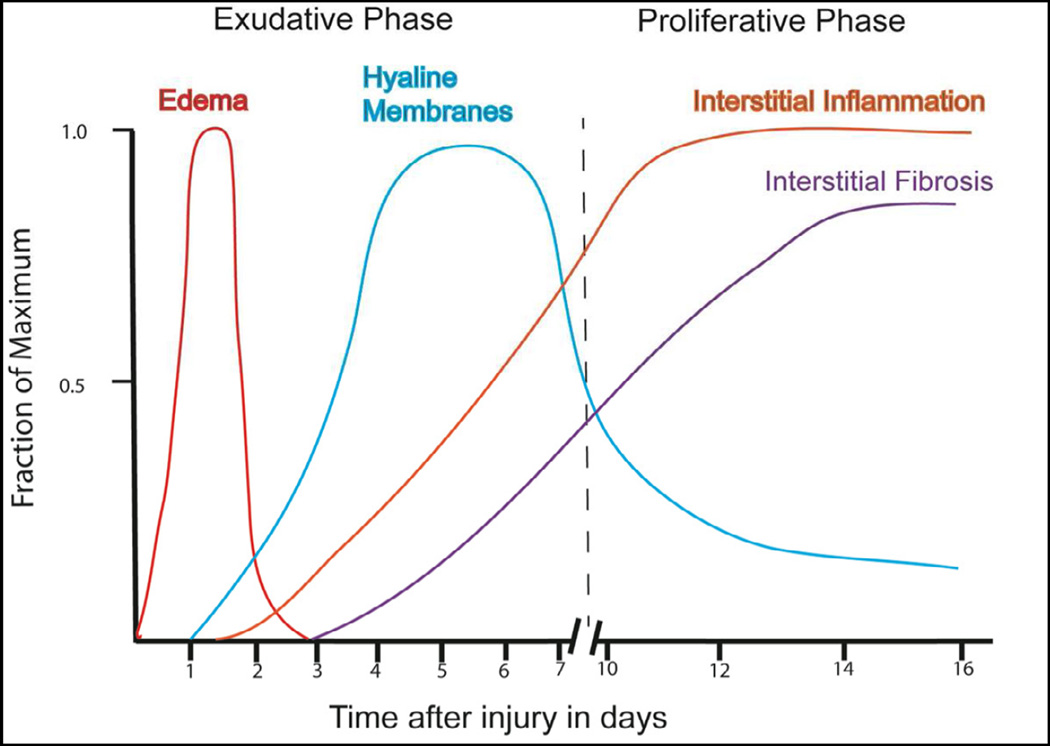
The pathological states of ARDS consist of three discrete stages that overlap both temporally and spatially (figure 1(24)). Histologically, the initial exudative phase is characterized by diffuse alveolar damage. In this early phase the epithelial and endothelial cells release factors reacting to injury and death. The loss of cellular integrity results in flooding of the alveolus with a proteinaceous exudate that results in the impairment of gas exchange. The subsequent dilution of surfactant proteins leads to alveolar collapse and decreased lung compliance. Over the ensuing days the pulmonary edema fluid is cleared and a proliferative stage develops. Histologically this is marked by proliferation and phenotypic changes in type II alveolar cells and fibroblasts. In the absence of recovery some patients progress to a fibrotic stage that is characterized by diffuse fibrosis and the obliteration of normal lung architecture. Various observational and clinical studies identify biomarkers that correlate with these stages, some of which have been associated with clinical outcomes. To put the biomarkers in the context of the physiological stages of ALI we have segregated them to correspond to the exudative (Table 1) and proliferative phase (Table 2) of ALI.
Figure 1.
Time course in Acute Lung Injury. Early in the course the alveoli are filled with protein rich permeability pulmonary edema. By day five to seven, there is proliferation of type II alveolar epithelial cells, leading to repithelialization and restoration of the alveolar structure or progressive fibrosis and irreversible hypoxic respiratory failure. (Redrawn from Katzenstein AA, Askin FB. Surgical Pathology of Non-neoplastic Lung)
Table 1.
Summary of biomarkers reflective of the Exudative Phase of ALI/ARDS.
| System | Subtype | Molecule |
Biologic Source |
Altered in ALI/ARDS |
Predicts Outcome |
Validated | References |
| Lung Injury | |||||||
| Alveolar Type II | Surfactant A, B | BALF | Decreased | YES | NO | Greene (50), | |
| Surfactant A | Plasma | Increased | NO | YES | Eisner (52) | ||
| Surfactant D | Plasma | Increased | YES | YES | Eisner (31) | ||
| KL-6 | ELF, plasma | Increased | YES | NO | Ishizaka (55) | ||
| Alveolar Type I | RAGE | Plasma | Increased | YES | YES | Uchida (57), Calfee (58), Fremont (59) | |
| Lung Matrix | Laminin | Plasma, ELF | Increased | YES | NO | Katayama (63) | |
| Desmosine | Urine | Increased | NO | YES | McClintock (19) | ||
| Endothelial Cell | vWF | Plasma | Increased | YES | YES | Ware (68) | |
| sICAM | Plasma, ELF | Increased | YES | YES | Agouridakis (70), Conner (21), Calfee (69) | ||
| Coagulation | PAI-1 | Plasma, ELF | Increased | YES | Prabhakaran (23) | ||
| Protein C | Plasma, ELF | Decreased | YES | NO | Ware (87), McClintock (88) | ||
| Inflammation | Proinflammatory | IL-1â | Plasma, BALF | Increased | YES | NO | Pugin (43), Suter (44), Park (45) |
| IL6 | Plasma, BALF | Increased | YES | YES | Bouros (35), Meduri (37), Parsons (28) | ||
| IL-8 | Plasma, BALF | Increased | YES | YES | Donnely (38), Takala (36), Parsons (28) | ||
| CRP | Serum | Increased | YES | NO | Bajwa (48) | ||
| Antinfllammatory | sTNFR-I and II | Plasma | Increased | YES | YES | Parsons (29), Calfee (27) | |
| IL-10 | Plasma | Increased | YES | YES | Parsons (28) | ||
| System | Subtype | Molecule |
Biologic Source |
Altered in ALI/ARDS |
Predicts Outcome |
Validated | References |
| Lung Injury | |||||||
| Alveolar Type II | Surfactant A, B | BALF | Decreased | YES | NO | Greene (50), | |
| Surfactant A | Plasma | Increased | NO | YES | Eisner (52) | ||
| Surfactant D | Plasma | Increased | YES | YES | Eisner (31) | ||
| KL-6 | ELF, plasma | Increased | YES | NO | Ishizaka (55) | ||
| Alveolar Type I | RAGE | Plasma | Increased | YES | YES | Uchida (57), Calfee (58), Fremont (59) | |
| Lung Matrix | Laminin | Plasma, ELF | Increased | YES | NO | Katayama (63) | |
| Desmosine | Urine | Increased | NO | YES | McClintock (19) | ||
| Endothelial Cell | vWF | Plasma | Increased | YES | YES | Ware (68) | |
| sICAM | Plasma, ELF | Increased | YES | YES | Agouridakis (70), Conner (21), Calfee (69) | ||
| Coagulation | PAI-1 | Plasma, ELF | Increased | YES | Prabhakaran (23) | ||
| Protein C | Plasma, ELF | Decreased | YES | NO | Ware (87), McClintock (88) | ||
| Inflammation | Proinflammatory | IL-1â | Plasma, BALF | Increased | YES | NO | Pugin (43), Suter (44), Park (45) |
| IL6 | Plasma, BALF | Increased | YES | YES | Bouros (35), Meduri (37), Parsons (28) | ||
| IL-8 | Plasma, BALF | Increased | YES | YES | Donnely (38), Takala (36), Parsons (28) | ||
| CRP | Serum | Increased | YES | NO | Bajwa (48) | ||
| Antinfllammatory | sTNFR-I and II | Plasma | Increased | YES | YES | Parsons (29), Calfee (27) | |
| IL-10 | Plasma | Increased | YES | YES | Parsons (28) |
BALF = bronchoalveolar lavage fluid, ELF= epithelial lining fluid, CCSP = clara cell secretory protein, vWF = von Willebrand Factor, sICAM = soluble intercellular adhesion molecule-1, PAI-1 = plasminogen activator inhibitor-1, sTNFR 1 and II= soluble TNF receptor 1 and II.
Table 2.
Summary of biomarkers reflective of the Proliferative Phase of ALI/ARDS.
| Type of Proliferation |
Growth Factor | Biologic Source |
Altered in ALI/ARDS |
Predicts Outcome |
Validated | References |
|---|---|---|---|---|---|---|
| Epithelial | KGF | BALF | Increased | YES | NO | Stern (94) |
| HGF | BALF | Increased | NO | NO | Stern (94) | |
| Endothelial | VEGF | Plasma | Increased | NO | NO | Thickett (96, 97) |
| Ang-2 | Plasma | Increased | YES | YES | Gallagher (72), Ong (74) |
EXUDATIVE PHASE
A hallmark of ARDS is diffuse alveolar damage consisting of widespread epithelial and endothelial injury and death accompanied by a proteinaceous exudate. With this histological finding in mind many investigators have sought to determine if specific cellular proteins released during injury could represent biomarkers for the diagnosis or prognosis of ARDS.
Inflammation
In ALI, a complex network of cytokines mediates the inflammatory response to a primary infection in the lungs or systemic inflammation such as seen in sepsis or pancreatitis (25). Greater prominence in bronchoalveolar lavage fluid (BALF) of certain cytokines suggests that inflammatory mediators have a pulmonary origin. Levels of both pro-inflammatory (interleukin (IL) 1β, tumor necrosis factor (TNF)- α, IL-6 and IL-8) and anti-inflammatory cytokines (IL- 1ra, IL-10, IL-13) are elevated in plasma or BALF in ALI indicating a balance of these mediators governs the development of ALI (26). Both pro- and anti-inflammatory biomarkers have been studied to establish their role in predicting the development, diagnosis and in prognosticating ALI but only a few have been validated in multicenter studies (20, 27–29).
TNF is an important mediator in ALI (30). Higher plasma levels of TNF- α have been reported in at-risk patients with sepsis (31). Though elevated plasma TNF-α levels were seen in patients with ARDS, they were not different from patients at-risk of developing ARDS (32). Similarly, other studies have demonstrated no significant difference in serum TNF-α levels in patients at-risk of ARDS compared to patients with ARDS (33), though in this study mean BAL levels of TNF- α were significantly higher in patients with ARDS in comparison to normal subjects. Parsons et al (29) measured plasma levels of TNF- α and soluble TNF receptors I and II (sTNFR-I and II) from patients enrolled in the ARDS Network low tidal volume study. Plasma TNF- α levels at the time of enrollment were detectable only in 9% of the subjects and were not different at baseline or in 3 days in those who did or did not survive. In contrast, sTNFR-I and sTNFR-II were detectable and were strongly related to an increased risk of death, fewer non-pulmonary organ failure free days and fewer ventilator free days. Calfee, et al, (27) have reported lower levels of sTNFR- I in trauma related ALI patients in the ARDS Network low tidal volume study and the ALVEOLI study (4).
IL-6 is one of the most important mediators of fever and in ARDS high plasma and BALF levels are predictive of poor outcomes. Though IL-6 activates both pro- and anti-inflammatory pathways, early in ARDS it correlates with a pro-inflammatory profile with increased levels seen in response to LPS in experimental models (34). Elevated plasma IL-6 were seen patients at risk for developing ARDS who met criteria within 48 hours (35). In that study, the higher BALF IL-6 levels seen in at-risk patients who developed ARDS were similar to patients with ARDS and there was a strong negative predictive value of serum and BALF IL-6 levels for the development of ARDS. Other investigators have also reported high plasma IL-6 levels in patients with risk factors who developed ALI in comparison to those who did not develop ALI (36). High baseline (day 1) levels were seen in patients with ALI who died and a persistent elevation predicted mortality (37). In 593 patients from the ARDS network study (5), baseline levels of IL-6 were higher in non-survivors (28) even after controlling for ventilation strategy, severity of illness, vasopressor use, platelet count and severity of impairment in gas exchange in a multivariate analysis. In addition, higher IL-6 levels were independently associated with fewer ventilator free days and organ failure free days.
IL-8 is a pro-inflammatory cytokine with high plasma and BALF levels found early in ALI (35–38) that predicts outcomes. In early studies the predictive power of IL-8 in identifying cases of ALI varied (35, 39, 40) (36) (38). However, in the larger ARDS network low tidal volume study (5), higher baseline levels of plasma IL-8 were associated with increased risk of death and in a multivariate analysis controlling for ventilation strategy, severity of illness, vasopressor use, platelet count and severity of impairment in gas exchange, were associated with fewer ventilator free and organ failure free days. Similar to IL-6, ventilation using low tidal volume was associated with a faster decline in IL-8 levels.
IL-1β is a potent cytokine secreted by activated macrophages (41) resulting in elevated levels in plasma, BALF and edema fluid (42) early in ARDS (43, 44) and is an important bioactive cytokine in the BALF in the early phase of ALI. Large multicenter studies looking into the role of IL-1β are lacking, but small studies show persistent elevation of plasma IL-1β (37) and elevated BALF IL-1β (43) are associated with worse outcomes. IL-1Ra levels peak between day 1 and 3 (45), suggesting a balance between these molecules contributing to the overall pro-inflammatory state in the lung.
In addition to IL-1Ra, a number of other anti-inflammatory mediators contribute to the overall inflammatory balance in the lung. Park et al identified anti-inflammatory responses that peaked after the onset of ARDS and these mediators included IL-1Ra, IL-1RII, sTNF-I, siL-6R and IL-10.(45) Only IL-10 (28) and sTNFR-I and II (29) have been studied in multicenter trials. In the ARDS Network low tidal volume study, high baseline IL-10 levels were associated with higher mortality but were less strongly associated with morbidity as measured by organ failure and ventilator free days. Similarly, higher baseline sTNFR-I and II levels have been associated with higher mortality in patients from the ARDS Network low tidal volume ventilation study (29).
Overall, the current evidence indicates that cytokine levels are characteristic and may have utility in prognostication but are only weakly predictive for the development of ALI. Other mediators of inflammation have been studied to identify biomarkers to predict the development of ARDS in at-risk patients. High mobility group box nuclear protein 1 (HMGB1), which is a DNA nuclear binding protein, was increased within 30 minutes after severe trauma and correlated with severity of injury, tissue hypoperfusion, early posttraumatic coagulopathy, systemic inflammatory response, acute kidney injury and subsequent development of respiratory failure. In addition, higher levels are correlated with higher mortality (46). Villar et al (47) investigated the role of Lipopolysaccharide Binding Protein (LBP), an acute phase protein that mediates inflammation, in 180 patients with sepsis. Though the baseline LBP serum levels were similar in survivors and non-survivors at study entry, at 48 hours and seven days the levels were higher in ARDS patients than ALI patients. An increase in serum LBP at 48 hours was also associated with high mortality. Nitric oxide (NO), a marker of oxidative stress, was investigated in patients from ARDS Network low tidal volume ventilation study (20) with a working hypothesis that peroxinitrites would oxidize proteins such as α1- antitrypsin and surfactant protein A and promote an inflammatory state. It was thus hypothesized that the lower tidal volume ventilation group would have lower urine NO levels. Surprisingly, higher urine NO levels were strongly associated with better clinical outcomes including mortality, organ failure free days and ventilator free days. Mechanism that could be responsible for these findings will need further evaluation. Similarly, higher levels of CRP (48) within 48 hours of onset of ARDS was found to be associated with better survival, lower number of organ failure free day and days on mechanical ventilation, a finding that contradicts long held views.
Injury
Alveolar type II cell injury
In the acute phase of ARDS the alveolar epithelial cell is injured, a key component to the clinical presentation. An important function of the type II cell is the production of surfactant. These surface-active lipoprotein complexes decrease surface tension keeping the alveolus open and increasing compliance. Surfactant proteins are important in normal lung physiology and host defenses. Surfactant proteins (SP) A and D are also involved in innate immunity. Early observations in ARDS revealed a loss in surface tension suggesting a functional loss of the surfactant proteins (1). In 1999 Greene and colleagues described complex changes in various surfactant proteins in ARDS both prior to its onset and throughout the exudative period (49). They observed that early in the exudative phase SP-A and SP-B decreased in BALF. They felt it was not due to dilution since SP-D concentration remained stable. This implies that surfactant proteins are either consumed and/or there is a concomitant decrease in production due to cellular injury. Interestingly, serum levels did not correlate with BALF levels for either SP-A or SP-D, with both increasing during the first seven days after diagnosis. This report suggested that surfactant proteins in the BALF are markers for survival. A subsequent study by the same group found serum SP-A to be a predictor of developing ARDS in 51 individuals at risk (50). Subgroup analysis revealed this to be a good predictor for ARDS associated with sepsis or aspiration, but not trauma. In addition to SP-A, a single center study of 54 patients found plasma levels of SP-B to be predictive of those that develop ARDS (51). A subsequent larger and longitudinal study of 565 clinical trial participants used a multivariate analysis to determine clinical outcomes based on the plasma levels of SP-A and SP-D (52). Baseline plasma SP-A levels did not correlate to any clinical outcome in this large, multicenter study. However, higher baseline SP-D plasma levels were associated with a higher mortality and co-morbidities such as the number of ventilator and organ-failure days. A finding that a polymorphism in SP-B is associated with an increase risk of developing ARDS in women further suggests the importance of surfactant proteins in lung homeostasis and its role in ARDS (53).
Another marker for alveolar epithelial type II cells is the membrane glycoprotein KL-6 that belongs to the mucin family of proteins. Type II cells that are injured or proliferating have increased expression and measurable levels of KL-6 are present in both the BALF and plasma. This marker of cellular injury appears non-specific since elevated levels of KL-6 have been found in patients with interstitial lung disease (54). In ALI/ARDS Ishizaka and colleagues found higher concentrations in epithelial lining fluid and plasma correlated with higher mortality (55) suggesting these higher levels represent a higher degree of epithelial cell injury.
Alveolar type I cell injury
Highly susceptible to injury, the thin and fragile type I cell covers the majority of the alveolus. Present predominantly on the basal surface of type I cells is the receptor for advanced glycation end products (RAGE). RAGE belongs to the immunoglobulin superfamily and functions as a multi-ligand receptor that propagates the inflammatory response via NFKB (56, 57). Elevated levels of RAGE have been reported in ALI (57) and in the ARDS Network low tidal volume trial (5) higher baseline plasma levels of RAGE were associated with increased mortality (58). These findings persisted when adjusted for multiple confounders such as age, gender, severity of illness and sepsis. However, this finding was limited to the high tidal volume group that had a higher mortality and presumably higher injury. In a separate retrospective nested case control study of 192 patients, RAGE was one of seven biomarkers out of 21 measured that had a high diagnostic accuracy in distinguishing ALI from non-ALI in trauma patients (59).
Bronchiolar cell injury
Although the alveolar epithelium plays a central role in the pathophysiology of ARDS, the injury extends beyond the alveolus to the distal airways. Present in the small airways are bronchial epithelial cells that produce Clara cell secretory protein (CCSP). Its role is unclear, but CCSP has been implicated in regulating the inflammatory response (60). In a single center study, elevated serum levels of CCSP were associated with an increased risk of mortality (61), however this association with mortality was not found in a similar small study (22). In yet another small, single center study, elevated plasma levels of CCSP in patients with ventilator-associated pneumonia identified those with ALI/ARDS (62). Although one could postulate that CCSP production would increase in the presence of injury, its association with higher mortality suggests the elevated levels actually reflect clara cell injury. Until larger studies are performed, the role of CCSP as a biomarker for ALI/ARDS remains unclear.
Lung Matrix injury
The extracellular matrix of the lung functions as the scaffold that supports the epithelium and vascular structures. It consists of collagens, glycoproteins and proteoglycans. Laminin is an extracellular protein deposited in the basement membrane that is important for cellular adhesion, growth and differentiation; therefore, important for re-populating and repairing the epithelium. In a small, single center study plasma and lung edema fluid levels of laminin Υ2 fragments, an amino terminal fragment of the gamma 2 chain of Laminin-5, were elevated in those with ALI/ARDS compared to controls (63). Interestingly, elevated levels at day 5 of lung injury correlated with an increase in mortality, presumably reflecting ongoing injury. Elastin is another critical protein in the extracellular matrix that gives the lung its elastic recoil ability. When damaged it releases small fragments containing desmosine and iso-desmosine that can be measured in extracellular fluids, including serum, BALF and urine. In the same ARDS network trial of low tidal volume, the investigators measured urinary desmosine levels by radioimmunoassay. Individuals ventilated with high tidal volumes had higher urinary desmosine levels, presumably a reflection of structural lung damage. However, there were no correlations to clinical outcomes, such as mortality (19).
Endothelial cell injury
In addition to the epithelium, the endothelium is also a site of injury in ALI/ARDS. The endothelial cell produces a number of compounds important in vasoregulation and hemostasis. Although responsive vasoconstriction in ALI/ARDS has been recognized, it has not been a target to define biomarkers. Several endothelial derived hemostasis factors are elevated in ARDS presumably as a response to cellular injury, although it is not clear what stimulus accounts for the elevated levels. The endothelial cell product von Willebrand factor (vWF) forms a complex with Factor VIII that is essential for platelet adhesion to damaged endothelium and platelet aggregation. These factors help maintain vascular integrity, however in excess the balance could shift toward in situ thrombosis and extension of vascular injury. In a sentinel paper in 1982 Carvalho, et al, reported 100 patients with ALI/ARDS that demonstrated a five-fold increase in vWF levels in ARDS (64). In a prospective study of 45 patients with non-pulmonary sepsis Rubins and colleagues found elevations in vWF to be predictive of developing ALI with a sensitivity of 87% and specificity of 77% (65). However, these findings were not confirmed in subsequent trials, including one by Bajaj and coworkers where vWF along with other endothelial markers, tissue factor pathway inhibitor and thrombomodulin, were not found to be predictive of developing ARDS (66). This study was limited due to its small size; where only eight of the 15 patients at risk actually developed ARDS. In a larger study of 96 patients with sepsis and non-sepsis risk factors for developing ARDS, Moss and colleagues did not find vWF levels helpful in predicting the progression to ARDS in either group (67). Although levels were elevated in ARDS the sensitivity in detecting ARDS was 70% or less. In a definitive study of 559 subjects of the ARDS network trial for low tidal volume, Ware and coworkers measured vWF plasma levels and reported similar baseline levels comparing sepsis to non-sepsis patients, however, significantly higher levels were found in non-survivors. Higher levels were also significantly associated with fewer organ failure free days suggesting the degree of endothelial activation and injury is strongly associated with outcomes in ALI/ARDS (68).
The soluble intercellular adhesion molecule-1 (sICAM-1) is a low-molecular weight adhesion molecule. It is present in both epithelial and endothelial cells and is released in the setting of injury where elevated levels have been found in both lung edema fluid and plasma (21, 69, 70). In a prospective cohort study of pediatric patients with ALI, elevated plasma levels of sICAM-1 had increased risk of death or prolonged mechanical ventilation (71). In an observational study by Calfee and colleagues they found edema fluid levels of sICAM-1 to be elevated in ALI in 67 patients from their center. In a large study of patients (778 individuals) from the ARDS network low tidal volume trial they confirmed elevated levels of sICAM-1 were associated with ALI and found that elevated levels over the first three days portended a higher risk of death (69).
Angiopoietin-1 and -2 (Ang-1 and -2) are vascular growth factors that have been proposed as biomarkers for ALI/ARDS. Both function through the endothelial tyrosine kinase receptor; however, they have opposite effects. Ang-1 stabilizes the endothelium by decreasing apoptosis and inflammation. Whereas, Ang-2 is pro-inflammatory, promotes both endothelial and epithelial apoptosis, increases neutrophil adhesion and induces permeability by altering the cellular cytoskeleton. Hypothesizing that Ang-2 may be associated with a poor outcome, Gallagher and colleagues measured Ang-2 levels in critically ill patients. They found elevated plasma levels in those with ALI and in non-survivors (72). This finding is supported by two single nucleotide polymorphisms in Ang-2 associating with a risk in developing ALI (73). Ong and colleagues found the concentration of angiopoietin-2 relative to angiopoietin-1 was an independent predictor of death in an observational cohort study of ALI/ARDS patients (74). These findings not only identify a potential biomarker for ALI/ARDS and survival, but also suggest a possible therapeutic target to prevent vascular leak.
E-selectin belongs to a family of adhesion molecules only expressed on endothelial cells that is involved in leukocyte-endothelial adhesion. It has been shown to be released in the presence of TNF and elevated levels of this molecule have been associated with sepsis and signal a higher mortality(75). Since sepsis and ALI can co-exist and have similar vascular injuries, Okajima, et al, measured E-selectin plasma levels in 55 individuals at risk for developing ALI/ARDS and found that higher E-selectin levels were associated both with ALI and a higher mortality (76).
These studies highlight that endothelial cell activation and/or injury is present in ALI/ARDS and release of endothelial specific proteins strongly associate with outcomes, such as survival. This suggests that the endothelial cell and its components are potential targets for therapeutic intervention.
Coagulation
A hallmark of ARDS is the formation of hyaline membranes from intra-alveolar fibrin deposition due to an imbalance in coagulation and fibrinolysis during the exudative phase (77, 78). This fibrin can serve as a provisional matrix for epithelial cells to repopulate the damaged alveolus (79, 80). However, fibrin deposition can also be detrimental if excessive and occurs in the absence of re-epithelialization. In addition, fibrin can act as a sump for certain anti-inflammatory proteins such as surfactant and thereby activate the inflammatory process (81–85). Therefore, a balance between procoagulant and fibrinolytic processes is necessary to effectively close the damaged alveolus and allow effective epithelial repopulation without excessive inflammation or persistent obstruction of the alveolar space.
Given the presence of fibrin and fibronectin deposits in the exudative phase of ARDS, several observational studies were performed to determine if pro-coagulant and anti-fibrinolytic molecules are biomarkers for ARDS. Bertozzi and colleagues reported a decrease in urokinase activity in BALF in a small observational study of ARDS patients (82). This decrease in activity occurred despite normal levels of urokinase suggesting urokinase inactivation and possible urokinase inhibitor presence. This was supported by the presence of increased levels of the urokinase inhibitor plasminogen activator inhibitor-1 (PAI-1) in the BALF. In a larger, more complex population of patients, it was observed that ARDS was associated with both increased pro-coagulant and decreased fibrinolytic activities (86). This alteration in coagulation state was in part due to decreased levels of urokinase-type plasminogen activator and increased PAI-1 and a2-antiplasmin levels, which favored a pro-coagulant environment. These observational studies were followed by studies to determine if alterations in the procoagulant/fibrinolytic pathways determined outcomes. In 2003 Prabhakaran and colleagues found that elevated levels of PAI-1 in plasma and edema fluid were associated with a higher mortality (23). That same year a study by Ware identified lower levels of the anti-coagulant protein C were associated with a higher mortality in ARDS/ALI patients (87). Interestingly, thrombomodulin levels were ten-fold higher in edema fluid compared to healthy controls and two-fold higher compared to ARDS plasma. This implied thrombomodulin is produced locally in the lung. Thrombomodulin is an activator of the anti-coagulant protein C. Protein C activity was not measured so the significance of these levels is not known. In a separate study multivariate analysis that included protein C and thrombomodulin, decreased levels of protein C along with elevated levels of IL-8 and intercellular adhesion molecule were predictors of survival (88).
PROLIFERATIVE PHASE
Recovery from ALI/ARDS requires a well-orchestrated repair of the damaged alveolus and vascular structures. The exudative phase of lung injury results in a rich, proteinaceous environment that can function as a provisional matrix for subsequent cellular repopulation. As early as a few days into acute lung injury, type II cells begin to regenerate along the alveolar septa and signal the onset of the proliferative phase (89). Presumably, the exudative phase subsides due to improved vascular integrity and subsequently by seven to tenth day a fibroproliferative process is underway (Figure 1). Various stages of proliferation can occur throughout the lung simultaneously. With increasing duration of ALI/ARDS the fibroproliferative phase can predominate and recovery occurs in those able to remodel the lung. If well orchestrated, this process results in repair of the alveolus and vascular structures. If the process is incomplete or the fibroproliferative phase is over-exuberant in the absence of remodeling, then too often death ensues.
Epithelial Proliferation
Certain growth factors, such as keratinocyte growth factor (KGF) and hepatocyte growth factor (HGF) are known to be potent mitogens for type II alveolar epithelial cells. Important in the development of the fetal lung, KGF is a member of the fibroblast growth factor (FGF) family and is expressed by mesenchymal cells. However, KGF’s receptors only occur on epithelial cells thereby conferring its epithelial cell specificity (90–92). Numerous in vitro and in vivo studies have demonstrated beneficial effects on the proliferating epithelium including enhancing motility, resistance to injury, surfactant production, decreased apoptosis and release of autocrine factors (93). However, few human studies have been done to identify KGF’s role in ALI/ARDS. In a small study, Stern and colleagues measured KGF in BALF from 32 patients (17 ARDS, 8 hydrostatic edema, 7 non-ARDS) compared to 10 non-ventilated controls. KGF was detected in 13 of the 17 ARDS patients and was associated with detectable type III procollagen, a biomarker of fibroproliferation (94). Only one of the hydrostatic edema patients and none of the non-ARDS patients or controls had detectable KGF levels. Although this was a small study, measurable KGF was associated with death (p=0.02). In one other study by Verghese, KGF was detected in low levels in the edema fluid in patients with ALI and hydrostatic pulmonary edema but no statistical difference in the KGF concentration was observed (95).
HGF is a non-specific mitogen that is produced by a variety of cells including neutrophils, macrophages, endothelial cells and fibroblasts. HGF has several effects including protecting cells from DNA damage and inducing motility. Unlike KGF, there is a paucity of animal lung injury studies for HGF. In addition to measuring KGF, Stern and coworkers also measured HGF in the same cohort described above. They found HGF levels to be less specific for ARDS. HGF was not detected in any controls; however, it was measureable in 15 of the 17 ARDS patients, 7 of the 8 patients with hydrostatic edema and 6 of the 10 non-ARDS patients (94). When all groups were pooled, HGF concentrations were higher in non-survivors compared to survivors. Although KGF and HGF have favorable effects on epithelial cell protection and proliferation, elevated levels portend a poor outcome in this small study. This finding may reflect an exaggerated response to severe, ongoing injury. Verghese et al. also observed high HGF levels in edema fluid in patients with ALI in comparison to hydrostatic edema and higher levels were associated with worse outcomes (95). As these studies have small number of subjects, these findings need to be validated in a larger, multi-center study.
Endothelial Proliferation
Vascular endothelial growth factor (VEGF) has a complex role in the lung that not only includes mitogen activity but it is also a key player in inducing vascular permeability. Many cells in the lung including alveolar type II cells, alveolar macrophages and neutrophils release VEGF. Acute over-expression of VEGF leads to pulmonary edema in animal models. Therefore, its role in the pathophysiology and as a biomarker of ALI/ARDS has been sought. The first report of VEGF in ALI/ARDS was by Thickett and colleagues in 2001, where they observed elevated plasma VEGF in ARDS patients compared to those at risk for ARDS in both ventilated and non-ventilated controls (96). Subsequently, they and others found decreased levels of VEGF in both BALF and epithelial lining fluid in ARDS patients compared to controls or those at risk for ARDS (97, 98). It was not clear why there was a difference in plasma levels versus BALF. In 2005, Ware and coworkers measured VEGF in plasma and undiluted pulmonary edema fluid comparing ARDS/ALI to severe hydrostatic pulmonary edema and epithelial lining fluid in normal lungs. They found that pulmonary edema fluid VEGF levels were lower in both ARDS/ALI and hydrostatic edema compared to normal lungs (99). They concluded that dilution might be a factor in decreased pulmonary levels. Therefore, the physiological role and biomarker utility VEGF plays in ARDS/ALI remains unclear.
Fibroblast Proliferation
The fibroproliferative phase of ALI is felt to occur late, however the underpinnings for fibroproliferation may start as early as 24 hours of the diagnosis of ALI. A number of observational studies have demonstrated a marker of collagen turnover, N-terminal procollagen peptide-III (N-PCP-III), is elevated within 24 hours of the diagnosis of ARDS (100–102) suggesting an early up-regulation of the fibroproliferative process. Marshall and colleagues measured N-PCP-III levels in BALF and serum along with BALF activity, i.e. ability of BALF to stimulate human lung fibroblasts in vitro. They found at 24 hours serum N-PCP-III levels were elevated in ARDS compared to controls and were significantly elevated in non-survivors of ARDS compared to survivors. This corresponded to an elevated mitogen activity of the BALF. This mitogenic activity remained elevated in ARDS at 7 days and was also significantly higher in non-survivors. This indicates that fibroproliferation can occur early in ARDS and may signal a poor outcome (103).
Combining Biomarkers in ALI
Despite evidence that individual biomarkers might identify patients with ALI and also assist in classifying patients with worse outcomes, no single biomarker diagnoses or prognosticates ALI with high accuracy. To identify if a panel of markers will perform better than any individual biomarker, Freemont and colleagues (59) conducted a retrospective nested study in a trauma intensive care unit. From the twenty-one biomarkers studied, a panel of seven biomarkers that included RAGE, Angiopoietin-2, PCP III, BNP, IL-10, TNF-α and IL-8, discriminated ALI/ARDS cases from critically ill trauma control patients with clear chest radiographs or hydrostatic pulmonary edema. AUCROCC analysis showed an AUC of 0.86 (95% CI 0.82–0.92). McClintock et al (88) studied plasma biomarkers of inflammation (IL-6, IL-8, ICAM-1), coagulation (Thrombomodulin, protein C) and fibrinolysis (PAI-1) in 50 patients with early ALI ventilated by low tidal volume to determine if these markers remained predictive of outcomes with lung protective ventilation. All markers except IL-6 were significantly different between survivors and non-survivors. After multivariate analysis that included clinical and demographic variables, three markers, IL-8, ICAM-1 and protein C were independently associated with a higher risk of death. In another study, Gajic (104) investigated clinical and demographic parameters for the prediction of death and prolonged mechanical ventilation in ALI. A model based on age, oxygen index and cardiovascular failure at day 3 was identified in a derivation cohort and it performed better in the clinical trial validation cohort with a AUCROCC of 0.81 (95% CI 0.77–0.84) than population-based validation cohort (0.71, 95% CI 0.65–0.76). A lung injury prediction score (LIPS) has recently been described and validated for prediction of development of ALI in a multicenter observational cohort study (105, 106). LIPS discriminated patients who developed ALI from those who did not with an AUC of 0.80 (95% CI, 0.78–0.82). Combining clinical risk factors with biologic markers in plasma were also investigated in subjects enrolled in the ARDS Network higher versus lower positive end expiratory pressure trial (4). Six clinical parameters and eight biological markers were studied to predict mortality at sixty days (107). Clinical predictors that included APACHE III, organ failure, age, underlying cause, alveolar-arterial oxygen gradient and plateau pressure, and predicted mortality with AUCROCC of 0.82. When the clinical parameters were used with the eight biological markers that included vFW, SP-D, TNFR I, IL-6, IL-8, ICAM-1, Protein-C and PAI-1 the discrimination improved to AUCROCC of 0.85. The best performing biomarkers were IL-8 and SP-D suggesting the key role of inflammation and alveolar epithelial injury in ALI/ARDS.
New Approaches for Biomarker Discovery in ALI/ARDS
Biological systems are complex with a large number of functionally diverse and frequently multifunctional sets of elements interacting selectively and non-linearly. Because of the intrinsic complexity of these biological systems, a combination of experimental and systems level approaches are expected to improve our understanding of heterogeneous conditions like ARDS/ALI. Genomics tools have been used both with candidate gene approach (53, 108–111) and genome wide analysis (108). Gene expression profiling at the level of the proteome have also been utilized in ARDS/ALI using DIGE and mass spectrometric studies. Chang et al. have found complex protein interactions in the BALF protein expression in patients with ARDS. These changes were dynamic over the course of injury and network analysis demonstrated unexpected ‘central components’ in the protein interaction networks (112). Proteomic studies in the BALF from three patients using liquid chromatography combined with tandem MS (LC-MS/MS) demonstrated higher levels of insulin like growth factor binding protein-3 (IGFBP-3) in ARDS patients in comparison to controls (113) and that IGFBP-3/IGF pathway was involved in pathogenesis of ALI by repressing apoptosis in fibroblasts but not epithelial cells. In a pilot study of nuclear magnetic resonance (NMR) based plasma metabolomics, Stringer et al. have observed distinct metabolic pathways that distinguished sepsis induced ALI from healthy controls (114).
Conclusion
Biomarkers in Acute Lung Injury have provided valuable knowledge into the pathogenesis. In the last ten years a number of biomarkers have been tested in large studies. A single biomarker or panels of markers that are easily available and predict either the development of ALI or diagnose ALI for routine clinical use remain elusive. With improvement in high through put ‘omics’ platforms and availability of increasingly sophisticated bioinformatics tools, there is great hope of identifying new gene signatures and protein or small molecules that would serve as biomarkers for prediction, prognostication and diagnosis of ALI. These findings will hopefully provide insight into the biology of the disease and identify novel targets for therapeutic interventions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet. 1967 Aug 12;2(7511):319–323. doi: 10.1016/s0140-6736(67)90168-7. [DOI] [PubMed] [Google Scholar]
- 2.Suratt BT, Parsons PE. Mechanisms of acute lung injury/acute respiratory distress syndrome. Clin Chest Med. 2006 Dec;27(4):579–589. doi: 10.1016/j.ccm.2006.06.005. [Research Support, N.I.H., Extramural Review]. abstract viii. [DOI] [PubMed] [Google Scholar]
- 3.Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, et al. Incidence and outcomes of acute lung injury. N Engl J Med. 2005 Oct 20;353(16):1685–1693. doi: 10.1056/NEJMoa050333. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 4.Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004 Jul 22;351(4):327–336. doi: 10.1056/NEJMoa032193. [Clinical Trial Comparative Study Multicenter Study Randomized Controlled Trial Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 5.Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000 May 4;342(18):1301–1308. doi: 10.1056/NEJM200005043421801. [Clinical Trial Comparative Study Multicenter Study Randomized Controlled Trial Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 6.Steinberg KP, Hudson LD, Goodman RB, Hough CL, Lanken PN, Hyzy R, et al. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N Engl J Med. 2006 Apr 20;354(16):1671–1684. doi: 10.1056/NEJMoa051693. [Multicenter Study Randomized Controlled Trial]. [DOI] [PubMed] [Google Scholar]
- 7.Wheeler AP, Bernard GR, Thompson BT, Schoenfeld D, Wiedemann HP, deBoisblanc B, et al. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med. 2006 May 25;354(21):2213–2224. doi: 10.1056/NEJMoa061895. [Comparative Study Multicenter Study Randomized Controlled Trial Research Support, N.I.H., Extramural]. [DOI] [PubMed] [Google Scholar]
- 8.Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006 Jun 15;354(24):2564–2575. doi: 10.1056/NEJMoa062200. [Comparative Study Multicenter Study Randomized Controlled Trial Research Support, N.I.H., Extramural]. [DOI] [PubMed] [Google Scholar]
- 9.Ketoconazole for early treatment of acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. The ARDS Network. Jama. 2000 Apr 19;283(15):1995–2002. doi: 10.1001/jama.283.15.1995. [Clinical Trial Multicenter Study Randomized Controlled Trial Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 10.Randomized, placebo-controlled trial of lisofylline for early treatment of acute lung injury and acute respiratory distress syndrome. Crit Care Med. 2002 Jan;30(1):1–6. doi: 10.1097/00003246-200201000-00001. [Clinical Trial Multicenter Study Randomized Controlled Trial Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 11.Jain R, DalNogare A. Pharmacological therapy for acute respiratory distress syndrome. Mayo Clin Proc. 2006 Feb;81(2):205–212. doi: 10.4065/81.2.205. [Review]. [DOI] [PubMed] [Google Scholar]
- 12.Stapleton RD, Wang BM, Hudson LD, Rubenfeld GD, Caldwell ES, Steinberg KP. Causes and timing of death in patients with ARDS. Chest. 2005 Aug;128(2):525–532. doi: 10.1378/chest.128.2.525. [Research Support, N.I.H., Extramural Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 13.Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. Report of the American-European Consensus conference on acute respiratory distress syndrome: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Consensus Committee. J Crit Care. 1994 Mar;9(1):72–81. doi: 10.1016/0883-9441(94)90033-7. [Consensus Development Conference Review]. [DOI] [PubMed] [Google Scholar]
- 14.Herridge MS, Angus DC. Acute lung injury--affecting many lives. N Engl J Med. 2005 Oct 20;353(16):1736–1738. doi: 10.1056/NEJMe058205. [Comment Editorial]. [DOI] [PubMed] [Google Scholar]
- 15.De Gruttola VG, Clax P, DeMets DL, Downing GJ, Ellenberg SS, Friedman L, et al. Considerations in the evaluation of surrogate endpoints in clinical trials. summary of a National Institutes of Health workshop. Control Clin Trials. 2001 Oct;22(5):485–502. doi: 10.1016/s0197-2456(01)00153-2. [DOI] [PubMed] [Google Scholar]
- 16.Gerlach H, Toussaint S. Sensitive, specific, predictive… statistical basics: how to use biomarkers. Crit Care Clin. 2011 Apr;27(2):215–227. doi: 10.1016/j.ccc.2010.12.007. [Review]. [DOI] [PubMed] [Google Scholar]
- 17.Roca O, Gomez-Olles S, Cruz MJ, Munoz X, Griffiths MJ, Masclans JR. Effects of salbutamol on exhaled breath condensate biomarkers in acute lung injury: prospective analysis. Crit Care. 2008;12(3):R72. doi: 10.1186/cc6911. [Research Support, Non-U.S. Gov't]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sack U, Scheibe R, Wotzel M, Hammerschmidt S, Kuhn H, Emmrich F, et al. Multiplex analysis of cytokines in exhaled breath condensate. Cytometry A. 2006 Mar;69(3):169–172. doi: 10.1002/cyto.a.20231. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 19.McClintock DE, Starcher B, Eisner MD, Thompson BT, Hayden DL, Church GD, et al. Higher urine desmosine levels are associated with mortality in patients with acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2006 Oct;291(4):L566–L571. doi: 10.1152/ajplung.00457.2005. [Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McClintock DE, Ware LB, Eisner MD, Wickersham N, Thompson BT, Matthay MA. Higher urine nitric oxide is associated with improved outcomes in patients with acute lung injury. Am J Respir Crit Care Med. 2007 Feb 1;175(3):256–262. doi: 10.1164/rccm.200607-947OC. [Multicenter Study Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conner ER, Ware LB, Modin G, Matthay MA. Elevated pulmonary edema fluid concentrations of soluble intercellular adhesion molecule-1 in patients with acute lung injury: biological and clinical significance. Chest. 1999 Jul;116(1 Suppl):83S–84S. doi: 10.1378/chest.116.suppl_1.83s. [Comparative Study Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 22.Kropski JA, Fremont RD, Calfee CS, Ware LB. Clara cell protein (CC16), a marker of lung epithelial injury, is decreased in plasma and pulmonary edema fluid from patients with acute lung injury. Chest. 2009 Jun;135(6):1440–1447. doi: 10.1378/chest.08-2465. [Comparative Study Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prabhakaran P, Ware LB, White KE, Cross MT, Matthay MA, Olman MA. Elevated levels of plasminogen activator inhibitor-1 in pulmonary edema fluid are associated with mortality in acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2003 Jul;285(1):L20–L28. doi: 10.1152/ajplung.00312.2002. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S. Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 24.Katzenstein A-LA. Katzenstein and Askin's Surgical Pathology of Non-Neoplastic Lung Disease. Fourth Edition ed. Chapter 2. Philadelphia: Saunders; 2006. p. 18. Figure 2.1. [Google Scholar]
- 25.Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000 May 4;342(18):1334–1349. doi: 10.1056/NEJM200005043421806. [Historical Article Review]. [DOI] [PubMed] [Google Scholar]
- 26.Cross LJ, Matthay MA. Biomarkers in acute lung injury: insights into the pathogenesis of acute lung injury. Crit Care Clin. 2011 Apr;27(2):355–377. doi: 10.1016/j.ccc.2010.12.005. [Review]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Calfee CS, Eisner MD, Ware LB, Thompson BT, Parsons PE, Wheeler AP, et al. Trauma-associated lung injury differs clinically and biologically from acute lung injury due to other clinical disorders. Crit Care Med. 2007 Oct;35(10):2243–2250. doi: 10.1097/01.ccm.0000280434.33451.87. [Comparative Study]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parsons PE, Eisner MD, Thompson BT, Matthay MA, Ancukiewicz M, Bernard GR, et al. Lower tidal volume ventilation and plasma cytokine markers of inflammation in patients with acute lung injury. Crit Care Med. 2005 Jan;33(1):1–6. doi: 10.1097/01.ccm.0000149854.61192.dc. [Clinical Trial Comparative Study Multicenter Study Randomized Controlled Trial Research Support, U.S. Gov't, P.H.S.]. discussion 230–2. [DOI] [PubMed] [Google Scholar]
- 29.Parsons PE, Matthay MA, Ware LB, Eisner MD. Elevated plasma levels of soluble TNF receptors are associated with morbidity and mortality in patients with acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2005 Mar;288(3):L426–L431. doi: 10.1152/ajplung.00302.2004. [Evaluation Studies Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 30.Parsons PE, Moore FA, Moore EE, Ikle DN, Henson PM, Worthen GS. Studies on the role of tumor necrosis factor in adult respiratory distress syndrome. Am Rev Respir Dis. 1992 Sep;146(3):694–700. doi: 10.1164/ajrccm/146.3.694. [Comparative Study Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 31.Marks JD, Marks CB, Luce JM, Montgomery AB, Turner J, Metz CA, et al. Plasma tumor necrosis factor in patients with septic shock. Mortality rate, incidence of adult respiratory distress syndrome, and effects of methylprednisolone administration. Am Rev Respir Dis. 1990 Jan;141(1):94–97. doi: 10.1164/ajrccm/141.1.94. [Clinical Trial Randomized Controlled Trial Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 32.Roten R, Markert M, Feihl F, Schaller MD, Tagan MC, Perret C. Plasma levels of tumor necrosis factor in the adult respiratory distress syndrome. Am Rev Respir Dis. 1991 Mar;143(3):590–592. doi: 10.1164/ajrccm/143.3.590. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 33.Hyers TM, Tricomi SM, Dettenmeier PA, Fowler AA. Tumor necrosis factor levels in serum and bronchoalveolar lavage fluid of patients with the adult respiratory distress syndrome. Am Rev Respir Dis. 1991 Aug;144(2):268–271. doi: 10.1164/ajrccm/144.2.268. [Comparative Study Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 34.O'Grady NP, Preas HL, Pugin J, Fiuza C, Tropea M, Reda D, et al. Local inflammatory responses following bronchial endotoxin instillation in humans. Am J Respir Crit Care Med. 2001 Jun;163(7):1591–1598. doi: 10.1164/ajrccm.163.7.2009111. [Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 35.Bouros D, Alexandrakis MG, Antoniou KM, Agouridakis P, Pneumatikos I, Anevlavis S, et al. The clinical significance of serum and bronchoalveolar lavage inflammatory cytokines in patients at risk for Acute Respiratory Distress Syndrome. BMC Pulm Med. 2004 Aug 17;4:6. doi: 10.1186/1471-2466-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Takala A, Jousela I, Takkunen O, Kautiainen H, Jansson SE, Orpana A, et al. A prospective study of inflammation markers in patients at risk of indirect acute lung injury. Shock. 2002 Apr;17(4):252–257. doi: 10.1097/00024382-200204000-00002. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 37.Meduri GU, Headley S, Kohler G, Stentz F, Tolley E, Umberger R, et al. Persistent elevation of inflammatory cytokines predicts a poor outcome in ARDS. Plasma IL-1 beta and IL-6 levels are consistent and efficient predictors of outcome over time. Chest. 1995 Apr;107(4):1062–1073. doi: 10.1378/chest.107.4.1062. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 38.Donnelly SC, Strieter RM, Kunkel SL, Walz A, Robertson CR, Carter DC, et al. Interleukin-8 and development of adult respiratory distress syndrome in at-risk patient groups. Lancet. 1993 Mar 13;341(8846):643–647. doi: 10.1016/0140-6736(93)90416-e. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 39.Jorens PG, Van Damme J, De Backer W, Bossaert L, De Jongh RF, Herman AG, et al. Interleukin 8 (IL-8) in the bronchoalveolar lavage fluid from patients with the adult respiratory distress syndrome (ARDS) and patients at risk for ARDS. Cytokine. 1992 Nov;4(6):592–597. doi: 10.1016/1043-4666(92)90025-m. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 40.Schutte H, Lohmeyer J, Rosseau S, Ziegler S, Siebert C, Kielisch H, et al. Bronchoalveolar and systemic cytokine profiles in patients with ARDS, severe pneumonia and cardiogenic pulmonary oedema. Eur Respir J. 1996 Sep;9(9):1858–1867. doi: 10.1183/09031936.96.09091858. [Comparative Study]. [DOI] [PubMed] [Google Scholar]
- 41.Jacobs RF, Tabor DR, Burks AW, Campbell GD. Elevated interleukin-1 release by human alveolar macrophages during the adult respiratory distress syndrome. Am Rev Respir Dis. 1989 Dec;140(6):1686–1692. doi: 10.1164/ajrccm/140.6.1686. [DOI] [PubMed] [Google Scholar]
- 42.Pugin J, Verghese G, Widmer MC, Matthay MA. The alveolar space is the site of intense inflammatory and profibrotic reactions in the early phase of acute respiratory distress syndrome. Crit Care Med. 1999 Feb;27(2):304–312. doi: 10.1097/00003246-199902000-00036. [Comparative Study Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 43.Pugin J, Ricou B, Steinberg KP, Suter PM, Martin TR. Proinflammatory activity in bronchoalveolar lavage fluids from patients with ARDS, a prominent role for interleukin-1. Am J Respir Crit Care Med. 1996 Jun;153(6 Pt 1):1850–1856. doi: 10.1164/ajrccm.153.6.8665045. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S. Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 44.Suter PM, Suter S, Girardin E, Roux-Lombard P, Grau GE, Dayer JM. High bronchoalveolar levels of tumor necrosis factor and its inhibitors, interleukin-1, interferon, and elastase, in patients with adult respiratory distress syndrome after trauma, shock, or sepsis. Am Rev Respir Dis. 1992 May;145(5):1016–1022. doi: 10.1164/ajrccm/145.5.1016. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 45.Park WY, Goodman RB, Steinberg KP, Ruzinski JT, Radella F, 2nd, Park DR, et al. Cytokine balance in the lungs of patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2001 Nov 15;164(10 Pt 1):1896–1903. doi: 10.1164/ajrccm.164.10.2104013. [Research Support, U.S. Gov't, Non-P.H.S. Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 46.Cohen MJ, Brohi K, Calfee CS, Rahn P, Chesebro BB, Christiaans SC, et al. Early release of high mobility group box nuclear protein 1 after severe trauma in humans: role of injury severity and tissue hypoperfusion. Crit Care. 2009;13(6):R174. doi: 10.1186/cc8152. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Villar J, Perez-Mendez L, Espinosa E, Flores C, Blanco J, Muriel A, et al. Serum lipopolysaccharide binding protein levels predict severity of lung injury and mortality in patients with severe sepsis. PLoS One. 2009;4(8):e6818. doi: 10.1371/journal.pone.0006818. [Research Support, Non-U.S. Gov't]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bajwa EK, Khan UA, Januzzi JL, Gong MN, Thompson BT, Christiani DC. Plasma C-reactive protein levels are associated with improved outcome in ARDS. Chest. 2009 Aug;136(2):471–480. doi: 10.1378/chest.08-2413. [Comparative Study Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Greene KE, Wright JR, Steinberg KP, Ruzinski JT, Caldwell E, Wong WB, et al. Serial changes in surfactant-associated proteins in lung and serum before and after onset of ARDS. Am J Respir Crit Care Med. 1999 Dec;160(6):1843–1850. doi: 10.1164/ajrccm.160.6.9901117. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S. Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 50.Greene KE, Ye S, Mason RJ, Parsons PE. Serum surfactant protein-A levels predict development of ARDS in at-risk patients. Chest. 1999 Jul;116(1 Suppl):90S–91S. [PubMed] [Google Scholar]
- 51.Bersten AD, Hunt T, Nicholas TE, Doyle IR. Elevated plasma surfactant protein-B predicts development of acute respiratory distress syndrome in patients with acute respiratory failure. Am J Respir Crit Care Med. 2001 Aug 15;164(4):648–652. doi: 10.1164/ajrccm.164.4.2010111. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 52.Eisner MD, Parsons P, Matthay MA, Ware L, Greene K. Plasma surfactant protein levels and clinical outcomes in patients with acute lung injury. Thorax. 2003 Nov;58(11):983–988. doi: 10.1136/thorax.58.11.983. [Multicenter Study Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gong MN, Wei Z, Xu LL, Miller DP, Thompson BT, Christiani DC. Polymorphism in the surfactant protein-B gene, gender, and the risk of direct pulmonary injury and ARDS. Chest. 2004 Jan;125(1):203–211. doi: 10.1378/chest.125.1.203. [Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 54.Kobayashi J, Kitamura S. KL-6: a serum marker for interstitial pneumonia. Chest. 1995 Aug;108(2):311–315. doi: 10.1378/chest.108.2.311. [Comparative Study]. [DOI] [PubMed] [Google Scholar]
- 55.Ishizaka A, Matsuda T, Albertine KH, Koh H, Tasaka S, Hasegawa N, et al. Elevation of KL-6, a lung epithelial cell marker, in plasma and epithelial lining fluid in acute respiratory distress syndrome. Am J Physiol Lung Cell Mol Physiol. 2004 Jun;286(6):L1088–L1094. doi: 10.1152/ajplung.00420.2002. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 56.Bierhaus A, Humpert PM, Morcos M, Wendt T, Chavakis T, Arnold B, et al. Understanding RAGE, the receptor for advanced glycation end products. J Mol Med (Berl) 2005 Nov;83(11):876–886. doi: 10.1007/s00109-005-0688-7. [Research Support, Non-U.S. Gov't Review]. [DOI] [PubMed] [Google Scholar]
- 57.Uchida T, Shirasawa M, Ware LB, Kojima K, Hata Y, Makita K, et al. Receptor for advanced glycation end-products is a marker of type I cell injury in acute lung injury. Am J Respir Crit Care Med. 2006 May 1;173(9):1008–1015. doi: 10.1164/rccm.200509-1477OC. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Calfee CS, Ware LB, Eisner MD, Parsons PE, Thompson BT, Wickersham N, et al. Plasma receptor for advanced glycation end products and clinical outcomes in acute lung injury. Thorax. 2008 Dec;63(12):1083–1089. doi: 10.1136/thx.2008.095588. [Randomized Controlled Trial Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fremont RD, Koyama T, Calfee CS, Wu W, Dossett LA, Bossert FR, et al. Acute lung injury in patients with traumatic injuries: utility of a panel of biomarkers for diagnosis and pathogenesis. J Trauma. 2010 May;68(5):1121–1127. doi: 10.1097/TA.0b013e3181c40728. [Evaluation Studies Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dierynck I, Bernard A, Roels H, De Ley M. The human Clara cell protein: biochemical and biological characterisation of a natural immunosuppressor. Mult Scler. 1996 Jul;1(6):385–387. doi: 10.1177/135245859600100621. [DOI] [PubMed] [Google Scholar]
- 61.Lesur O, Langevin S, Berthiaume Y, Legare M, Skrobik Y, Bellemare JF, et al. Outcome value of Clara cell protein in serum of patients with acute respiratory distress syndrome. Intensive Care Med. 2006 Aug;32(8):1167–1174. doi: 10.1007/s00134-006-0235-1. [Multicenter Study Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 62.Determann RM, Millo JL, Waddy S, Lutter R, Garrard CS, Schultz MJ. Plasma CC16 levels are associated with development of ALI/ARDS in patients with ventilator-associated pneumonia: a retrospective observational study. BMC Pulm Med. 2009;9:49. doi: 10.1186/1471-2466-9-49. [Research Support, Non-U.S. Gov't]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Katayama M, Ishizaka A, Sakamoto M, Fujishima S, Sekiguchi K, Asano K, et al. Laminin gamma2 fragments are increased in the circulation of patients with early phase acute lung injury. Intensive Care Med. 2010 Mar;36(3):479–486. doi: 10.1007/s00134-009-1719-6. [Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Carvalho AC, Bellman SM, Saullo VJ, Quinn D, Zapol WM. Altered factor VIII in acute respiratory failure. N Engl J Med. 1982 Oct 28;307(18):1113–1119. doi: 10.1056/NEJM198210283071803. [DOI] [PubMed] [Google Scholar]
- 65.Rubin DB, Wiener-Kronish JP, Murray JF, Green DR, Turner J, Luce JM, et al. Elevated von Willebrand factor antigen is an early plasma predictor of acute lung injury in nonpulmonary sepsis syndrome. J Clin Invest. 1990 Aug;86(2):474–480. doi: 10.1172/JCI114733. [Research Support, U.S. Gov't, P.H.S.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bajaj MS, Tricomi SM. Plasma levels of the three endothelial-specific proteins von Willebrand factor, tissue factor pathway inhibitor, and thrombomodulin do not predict the development of acute respiratory distress syndrome. Intensive Care Med. 1999 Nov;25(11):1259–1266. doi: 10.1007/s001340051054. [Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 67.Moss M, Ackerson L, Gillespie MK, Moore FA, Moore EE, Parsons PE. von Willebrand factor antigen levels are not predictive for the adult respiratory distress syndrome. Am J Respir Crit Care Med. 1995 Jan;151(1):15–20. doi: 10.1164/ajrccm.151.1.7812545. [Comparative Study Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 68.Ware LB, Eisner MD, Thompson BT, Parsons PE, Matthay MA. Significance of von Willebrand factor in septic and nonseptic patients with acute lung injury. Am J Respir Crit Care Med. 2004 Oct 1;170(7):766–772. doi: 10.1164/rccm.200310-1434OC. [DOI] [PubMed] [Google Scholar]
- 69.Calfee CS, Eisner MD, Parsons PE, Thompson BT, Conner ER, Jr, Matthay MA, et al. Soluble intercellular adhesion molecule-1 and clinical outcomes in patients with acute lung injury. Intensive Care Med. 2009 Feb;35(2):248–257. doi: 10.1007/s00134-008-1235-0. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Review]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Agouridakis P, Kyriakou D, Alexandrakis MG, Prekates A, Perisinakis K, Karkavitsas N, et al. The predictive role of serum and bronchoalveolar lavage cytokines and adhesion molecules for acute respiratory distress syndrome development and outcome. Respir Res. 2002;3:25. doi: 10.1186/rr193. [Comparative Study]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Flori HR, Ware LB, Glidden D, Matthay MA. Early elevation of plasma soluble intercellular adhesion molecule-1 in pediatric acute lung injury identifies patients at increased risk of death and prolonged mechanical ventilation. Pediatr Crit Care Med. 2003 Jul;4(3):315–321. doi: 10.1097/01.PCC.0000074583.27727.8E. [Comparative Study Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 72.Gallagher DC, Parikh SM, Balonov K, Miller A, Gautam S, Talmor D, et al. Circulating angiopoietin 2 correlates with mortality in a surgical population with acute lung injury/adult respiratory distress syndrome. Shock. 2008 Jun;29(6):656–661. doi: 10.1097/shk.0b013e31815dd92f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Meyer NJ, Li M, Feng R, Bradfield J, Gallop R, Bellamy S, et al. ANGPT2 genetic variant is associated with trauma-associated acute lung injury and altered plasma angiopoietin-2 isoform ratio. Am J Respir Crit Care Med. 2011 May 15;183(10):1344–1353. doi: 10.1164/rccm.201005-0701OC. [Multicenter Study Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ong T, McClintock DE, Kallet RH, Ware LB, Matthay MA, Liu KD. Ratio of angiopoietin-2 to angiopoietin-1 as a predictor of mortality in acute lung injury patients. Crit Care Med. 2010 Sep;38(9):1845–1851. doi: 10.1097/CCM.0b013e3181eaa5bf. [Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boldt J, Wollbruck M, Kuhn D, Linke LC, Hempelmann G. Do plasma levels of circulating soluble adhesion molecules differ between surviving and nonsurviving critically ill patients? Chest. 1995 Mar;107(3):787–792. doi: 10.1378/chest.107.3.787. [DOI] [PubMed] [Google Scholar]
- 76.Okajima K, Harada N, Sakurai G, Soga Y, Suga H, Terada T, et al. Rapid assay for plasma soluble E-selectin predicts the development of acute respiratory distress syndrome in patients with systemic inflammatory response syndrome. Transl Res. 2006 Dec;148(6):295–300. doi: 10.1016/j.trsl.2006.07.009. [Comparative Study]. [DOI] [PubMed] [Google Scholar]
- 77.Idell S, James KK, Levin EG, Schwartz BS, Manchanda N, Maunder RJ, et al. Local abnormalities in coagulation and fibrinolytic pathways predispose to alveolar fibrin deposition in the adult respiratory distress syndrome. J Clin Invest. 1989 Aug;84(2):695–705. doi: 10.1172/JCI114217. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Idell S, Koenig KB, Fair DS, Martin TR, McLarty J, Maunder RJ. Serial abnormalities of fibrin turnover in evolving adult respiratory distress syndrome. Am J Physiol. 1991 Oct;261(4 Pt 1):L240–L248. doi: 10.1152/ajplung.1991.261.4.L240. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 79.Bitterman PB, Rennard SI, Adelberg S, Crystal RG. Role of fibronectin as a growth factor for fibroblasts. J Cell Biol. 1983 Dec;97(6):1925–1932. doi: 10.1083/jcb.97.6.1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Grinnell F, Feld M, Minter D. Fibroblast adhesion to fibrinogen and fibrin substrata: requirement for cold-insoluble globulin (plasma fibronectin) Cell. 1980 Feb;19(2):517–525. doi: 10.1016/0092-8674(80)90526-7. [DOI] [PubMed] [Google Scholar]
- 81.Seeger W, Hubel J, Klapettek K, Pison U, Obertacke U, Joka T, et al. Procoagulant activity in bronchoalveolar lavage of severely traumatized patients--relation to the development of acute respiratory distress. Thromb Res. 1991 Jan 1;61(1):53–64. doi: 10.1016/0049-3848(91)90168-v. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 82.Bertozzi P, Astedt B, Zenzius L, Lynch K, LeMaire F, Zapol W, et al. Depressed bronchoalveolar urokinase activity in patients with adult respiratory distress syndrome. N Engl J Med. 1990 Mar 29;322(13):890–897. doi: 10.1056/NEJM199003293221304. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 83.Senior RM, Skogen WF, Griffin GL, Wilner GD. Effects of fibrinogen derivatives upon the inflammatory response. Studies with human fibrinopeptide B. J Clin Invest. 1986 Mar;77(3):1014–1019. doi: 10.1172/JCI112353. [Research Support, U.S. Gov't, P.H.S.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Leavell KJ, Peterson MW, Gross TJ. The role of fibrin degradation products in neutrophil recruitment to the lung. Am J Respir Cell Mol Biol. 1996 Jan;14(1):53–60. doi: 10.1165/ajrcmb.14.1.8534486. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 85.Seeger W, Elssner A, Gunther A, Kramer HJ, Kalinowski HO. Lung surfactant phospholipids associate with polymerizing fibrin: loss of surface activity. Am J Respir Cell Mol Biol. 1993 Aug;9(2):213–220. doi: 10.1165/ajrcmb/9.2.213. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 86.Gunther A, Mosavi P, Heinemann S, Ruppert C, Muth H, Markart P, et al. Alveolar fibrin formation caused by enhanced procoagulant and depressed fibrinolytic capacities in severe pneumonia. Comparison with the acute respiratory distress syndrome. Am J Respir Crit Care Med. 2000 Feb;161(2 Pt 1):454–462. doi: 10.1164/ajrccm.161.2.9712038. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 87.Ware LB, Fang X, Matthay MA. Protein C and thrombomodulin in human acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2003 Sep;285(3):L514–L521. doi: 10.1152/ajplung.00442.2002. [Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 88.McClintock D, Zhuo H, Wickersham N, Matthay MA, Ware LB. Biomarkers of inflammation, coagulation and fibrinolysis predict mortality in acute lung injury. Crit Care. 2008;12(2):R41. doi: 10.1186/cc6846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tomashefski JF., Jr Pulmonary pathology of acute respiratory distress syndrome. Clin Chest Med. 2000 Sep;21(3):435–466. doi: 10.1016/s0272-5231(05)70158-1. [Review]. [DOI] [PubMed] [Google Scholar]
- 90.Chelly N, Mouhieddine-Gueddiche OB, Barlier-Mur AM, Chailley-Heu B, Bourbon JR. Keratinocyte growth factor enhances maturation of fetal rat lung type II cells. Am J Respir Cell Mol Biol. 1999 Mar;20(3):423–432. doi: 10.1165/ajrcmb.20.3.3201. [Comparative Study Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 91.Danilenko DM. Preclinical and early clinical development of keratinocyte growth factor, an epithelial-specific tissue growth factor. Toxicol Pathol. 1999 Jan-Feb;27(1):64–71. doi: 10.1177/019262339902700113. [Review]. [DOI] [PubMed] [Google Scholar]
- 92.Deterding RR, Jacoby CR, Shannon JM. Acidic fibroblast growth factor and keratinocyte growth factor stimulate fetal rat pulmonary epithelial growth. Am J Physiol. 1996 Oct;271(4 Pt 1):L495–L505. doi: 10.1152/ajplung.1996.271.4.L495. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 93.Ware LB, Matthay MA. Keratinocyte and hepatocyte growth factors in the lung: roles in lung development, inflammation, and repair. Am J Physiol Lung Cell Mol Physiol. 2002 May;282(5):L924–L940. doi: 10.1152/ajplung.00439.2001. [Research Support, U.S. Gov't, P.H.S. Review]. [DOI] [PubMed] [Google Scholar]
- 94.Stern JB, Fierobe L, Paugam C, Rolland C, Dehoux M, Petiet A, et al. Keratinocyte growth factor and hepatocyte growth factor in bronchoalveolar lavage fluid in acute respiratory distress syndrome patients. Crit Care Med. 2000 Jul;28(7):2326–2333. doi: 10.1097/00003246-200007000-00024. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 95.Verghese GM, McCormick-Shannon K, Mason RJ, Matthay MA. Hepatocyte growth factor and keratinocyte growth factor in the pulmonary edema fluid of patients with acute lung injury. Biologic and clinical significance. Am J Respir Crit Care Med. 1998 Aug;158(2):386–394. doi: 10.1164/ajrccm.158.2.9711111. [Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 96.Thickett DR, Armstrong L, Christie SJ, Millar AB. Vascular endothelial growth factor may contribute to increased vascular permeability in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2001 Nov 1;164(9):1601–1605. doi: 10.1164/ajrccm.164.9.2011071. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 97.Thickett DR, Armstrong L, Millar AB. A role for vascular endothelial growth factor in acute and resolving lung injury. Am J Respir Crit Care Med. 2002 Nov 15;166(10):1332–1337. doi: 10.1164/rccm.2105057. [Comparative Study Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 98.Maitre B, Boussat S, Jean D, Gouge M, Brochard L, Housset B, et al. Vascular endothelial growth factor synthesis in the acute phase of experimental and clinical lung injury. Eur Respir J. 2001 Jul;18(1):100–106. doi: 10.1183/09031936.01.00074701. [DOI] [PubMed] [Google Scholar]
- 99.Ware LB, Kaner RJ, Crystal RG, Schane R, Trivedi NN, McAuley D, et al. VEGF levels in the alveolar compartment do not distinguish between ARDS and hydrostatic pulmonary oedema. Eur Respir J. 2005 Jul;26(1):101–105. doi: 10.1183/09031936.05.00106604. [Comparative Study Research Support, N.I.H., Extramural Research Support, U.S. Gov't, P.H.S.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chesnutt AN, Matthay MA, Tibayan FA, Clark JG. Early detection of type III procollagen peptide in acute lung injury. Pathogenetic and prognostic significance. Am J Respir Crit Care Med. 1997 Sep;156(3 Pt 1):840–845. doi: 10.1164/ajrccm.156.3.9701124. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 101.Clark JG, Milberg JA, Steinberg KP, Hudson LD. Type III procollagen peptide in the adult respiratory distress syndrome. Association of increased peptide levels in bronchoalveolar lavage fluid with increased risk for death. Ann Intern Med. 1995 Jan 1;122(1):17–23. doi: 10.7326/0003-4819-122-1-199501010-00003. [Clinical Trial Controlled Clinical Trial Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 102.Meduri GU, Tolley EA, Chinn A, Stentz F, Postlethwaite A. Procollagen types I and III aminoterminal propeptide levels during acute respiratory distress syndrome and in response to methylprednisolone treatment. Am J Respir Crit Care Med. 1998 Nov;158(5 Pt 1):1432–1441. doi: 10.1164/ajrccm.158.5.9801107. [Clinical Trial Randomized Controlled Trial Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 103.Marshall RP, Bellingan G, Webb S, Puddicombe A, Goldsack N, McAnulty RJ, et al. Fibroproliferation occurs early in the acute respiratory distress syndrome and impacts on outcome. Am J Respir Crit Care Med. 2000 Nov;162(5):1783–1788. doi: 10.1164/ajrccm.162.5.2001061. [Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 104.Gajic O, Afessa B, Thompson BT, Frutos-Vivar F, Malinchoc M, Rubenfeld GD, et al. Prediction of death and prolonged mechanical ventilation in acute lung injury. Crit Care. 2007;11(3):R53. doi: 10.1186/cc5909. [Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gajic O, Dabbagh O, Park PK, Adesanya A, Chang SY, Hou P, et al. Early identification of patients at risk of acute lung injury: evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med. 2011 Feb 15;183(4):462–470. doi: 10.1164/rccm.201004-0549OC. [Evaluation Studies Multicenter Study Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Trillo-Alvarez C, Cartin-Ceba R, Kor DJ, Kojicic M, Kashyap R, Thakur S, et al. Acute lung injury prediction score: derivation and validation in a population-based sample. Eur Respir J. 2011 Mar;37(3):604–609. doi: 10.1183/09031936.00036810. [DOI] [PubMed] [Google Scholar]
- 107.Ware LB, Koyama T, Billheimer DD, Wu W, Bernard GR, Thompson BT, et al. Prognostic and pathogenetic value of combining clinical and biochemical indices in patients with acute lung injury. Chest. 2010 Feb;137(2):288–296. doi: 10.1378/chest.09-1484. [Comparative Study Multicenter Study Randomized Controlled Trial Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wang Z, Beach D, Su L, Zhai R, Christiani DC. A genome-wide expression analysis in blood identifies pre-elafin as a biomarker in ARDS. Am J Respir Cell Mol Biol. 2008 Jun;38(6):724–732. doi: 10.1165/rcmb.2007-0354OC. [Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Gong MN, Zhou W, Williams PL, Thompson BT, Pothier L, Boyce P, et al. -308GA and TNFB polymorphisms in acute respiratory distress syndrome. Eur Respir J. 2005 Sep;26(3):382–389. doi: 10.1183/09031936.05.00000505. [DOI] [PubMed] [Google Scholar]
- 110.Sutherland AM, Walley KR, Manocha S, Russell JA. The association of interleukin 6 haplotype clades with mortality in critically ill adults. Arch Intern Med. 2005 Jan 10;165(1):75–82. doi: 10.1001/archinte.165.1.75. [Comparative Study Research Support, Non-U.S. Gov't]. [DOI] [PubMed] [Google Scholar]
- 111.Gong MN, Thompson BT, Williams PL, Zhou W, Wang MZ, Pothier L, et al. Interleukin-10 polymorphism in position -1082 and acute respiratory distress syndrome. Eur Respir J. 2006 Apr;27(4):674–681. doi: 10.1183/09031936.06.00046405. [Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chang DW, Hayashi S, Gharib SA, Vaisar T, King ST, Tsuchiya M, et al. Proteomic and computational analysis of bronchoalveolar proteins during the course of the acute respiratory distress syndrome. Am J Respir Crit Care Med. 2008 Oct 1;178(7):701–709. doi: 10.1164/rccm.200712-1895OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Schnapp LM, Donohoe S, Chen J, Sunde DA, Kelly PM, Ruzinski J, et al. Mining the acute respiratory distress syndrome proteome: identification of the insulin-like growth factor (IGF)/IGF-binding protein-3 pathway in acute lung injury. Am J Pathol. 2006 Jul;169(1):86–95. doi: 10.2353/ajpath.2006.050612. [Research Support, N.I.H., Extramural]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Stringer KA, Serkova NJ, Karnovsky A, Guire K, Paine R, 3rd, Standiford TJ. Metabolic consequences of sepsis-induced acute lung injury revealed by plasma (1)H-nuclear magnetic resonance quantitative metabolomics and computational analysis. Am J Physiol Lung Cell Mol Physiol. 2011 Jan;300(1):L4–L11. doi: 10.1152/ajplung.00231.2010. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. [DOI] [PMC free article] [PubMed] [Google Scholar]