Abstract
The aim of this study is to investigate the effect of ECG criteria which are used for the distinction between AVNRT and AVRT for the choice of treatment in patients with Supraventricular Tachycardia (SVT). The 77 patients with narrow QRS complex SVT which was treated with Adenosine or Diltiazem in the Emergency Department were evaluated retrospectively. All 12-lead ECG during tachycardia were blindly reviewed according to ECG criteria (Pseudo-r` in V1, Pseudo-S-wave in the inferior leads, Visible P-wave, aVL notch) by a cardiologist and an emergency physician. In this study, while 59.6% of the patients returned to normal sinus rhythm (NSR) after the first dose 6 mg, 64.91% of them after the first dose 12 mg and 71.92% of them after the second dose of 12 mg adenosine, 95% of the patients returned to NSR after the 0.25 mg/kg diltiazem. The most visible ECG findings were visible P waves and the least visible ECG findings were Pseudo-S waves in the inferior leads. It was statistically significant between converted by adenosine to NSR and converted by diltiazem to NSR to the presence of visible P-wave and the aVL lead notch in their ECG findings. Conclusion: The rate of return to NSR through diltiazem was found higher than that of adenosine in narrow complex SVT patients. Also, diltiazem may be the first medication to be preferred in the presence of retrograt P wave and aVL notch in the ECG of the patients with narrow QRS complex stable SVT.
Keywords: AVNRT, AVRT, supraventricular tachycardia, SVT, adenosine, diltiazem, emergency medicine
Introduction
Narrow QRS complex supraventricular tachycardia (SVT) are common (23 to 47/100,000) cardiac emergency cases in Emergency Department (ED) [1]. Atrioventricular nodal reentrant tachycardia (AVNRT) are seen most common atrioventricular tachycardia in emergency department (ED) [2]. AVNRT is caused by a re-entran circuit involving the posterior and anterior inputs into the compact atrioventricular node [3-5]. AVNRT types are classified as typical (slow-fast) and atypical (fast-slow and slow-slow), according to the ratio of atrial-His/His-atrial intervals [2]. Atrioventricular reciprocating tachycardia (AVRT) is also a re-entran tachycardia; it requires the presence of an accessory pathway, a small strand of myocardium that bridges the normal insulation berween atria and ventricules [3-5].
ECGs are used to discriminate between these two mechanisms on patients with narrow QRS complex SVT. The presence of a pseudo-R’-wave in lead V1 or pseudo-S-wave in the inferior, visible P-wave, aVL notch has been used for the differential diagnosis between AVNRT and AVRT [6-8]. The findings that presence of a pseudo r` wave or pseudo S wave, or both, had an accuracy of 100% in predicting anterior-type AVNRT confirmed the previous report [9]. This ECG criteria are especially used in the selection of ablation therapy [2,6,8]. But, this criterias have been not used for evaluation of medical treatment in ED up to now.
Vagal maneuvers and adenosine are recommended to terminate stable narrow QRS complex SVTs, as an initial therapeutic choices in ACC/AHA/ESC guidelines [8]. It was showed that adenosine is able to convert narrow QRS complex SVT to Normal Sinus Rythm (NSR) at the rate of 86, 5-89% in studies [10,11]. Long-acting AV nodal blocking agents such as nondihy dropyridine calcium channel blockers (verapamil and diltiazem), flecainide or β blockers are used in case of adenosine or vagal maneuvers fail to convert rhythms of patients from narrow QRS complex SVT to NSR [8]. Diltiazem convertion rates were determined at 96-98.1% in studies [10,12].
AVNRT and AVRT are typically terminated by adenosine [13]. It was determined that convertion rate to NSR is at 72% in patients with AVRT and at 83% in patients with AVNRT by flecainide in a study in ED [14].
Also, ECG criterias have been not used to choose medical treatment in ED up to now.
The aim of this study is to determine the worthiness of ECG criterias in decision making for treatment of patients with stable narrow QRS complex SVT, which are used for the distinction between AVNRT and AVRT in patients with stable narrow QRS complex SVT in ED.
Materials and methods
After approval of Research Ethics Committee, the seventy-seven cases with narrow QRS complex (< 0.12 s) SVT were evaluated retrospectively between June 15, 2011 and June 20, 2013 at the Istanbul Bakırköy Dr. Sadi Konuk Training and Research Hospital Emergency Department. Data regarding the age, sex, past medical history, chief complaint, characteristics of stable narrow QRS complex SVT, on admission mean systolic and diastolic blood pressure, heart rate were evaluated from the patient files as retrospectively.
The evaluation of ECG criterias
All of patients diagnosed on 12 lead ECG were documented in this study. The 12-lead ECGs were recorded at a speed of 25 mm/s, set to 10 mm/mV, and filter set to 0.5 and 1000 Hz. All 12-lead ECG during tachycardia in patients which was treated in ED were blindly reviewed according to ECG criteria [6,7] as follow by a cardiologist and an emergency physician.
Pseudo-r` in V1
Presence of a positive deflection at the end of the QRS in lead V1, mimicking an incomplete right bundle branch block during tachycardia, and the absence of this deflection during sinus rhythm.
Pseudo-S-wave in the inferior leads (II, III, aVF)
Presence of a negative deflection at the end of the QRS in the inferior leads during tachycardia and the absence of this sign during sinus rhythm.
Visible P-wave
Presence of deflection in the ST-segment was interpreted as a retrograde P-wave in at least one of the 12 leads.
aVL notch
Any positive deflection at the end of the QRS during tachycardia and its absence during normal sinus rhythm.
If there was pseudo-S-wave in the leads II, III, aVF or pseudo-r` in V1 of any patient’s ECG it was evaluated as AVNRT [9].
Administration of diltiazem and adenosine
Diltiazem was administrated to patients with stable narrow QRS complex SVT at a dose of 0.25 mg/kg IV over 2 minutes, when rhythm was not converted to NSR, diltiazem was given an additional IV dose of 0.35 mg/kg in ED [8].
Adenosine was administrated to the patients with narrow QRS complex SVT at a dose of 6 mg IV bolus on antecubital region, following that preformed 20 ml salin infusion was given. When rhythm was not converted to NSR in 2 minutes, adenosine was given an additional IV 12 mg bolus. When rhythm was not converted to NSR in 2 minutes, adenosine was given an additional IV 12 mg bolus again [8,10].
Patient selection and exclusion criterias
Patients with other tachicardas without SVT (like sinus tachycardia, atrial flutter, atrial fibrillation, ventricular tachycardia) were excluded from study.
One hundred forty five patients with stable narrow QRS complex SVT were admitted to ED, over a 24-months period. But, 68 patients (27 patients who could not be reached their ECGs and treatment process, 30 patinets could be converted by vagal maneuvers and 11 patients not consensus by a cardiologist and an EP on their ECG criterias) were excluded in this study.
Statistical analysis
Data were analyzed with Number Cruncher Statistical System (NCSS) 2007 Statistical Software (Utah, USA). Continuous datas are expressed as mean ± SD. Proportions are expressed as percentages with 95% confidence intervals. Fisher’s exact and Pearson’s Chi-Square test were used the evaluation of treatment responses according to electrocardiographic criterias. Values of P < 0.05 were accepted statistically significant.
Results
Forty six point eight percent male and 53.2% female of 77 narrow QRS complex SVT patients. The mean age of cases was 57.86 ± 20.351 years (minimum 16, maximum 113).
The complaints and past medical histories of patients were shown on Table 1. Narrow QRS complex SVT was found on 35.1% of patients. Palpitation was found to be the most common complaint. Diabetes Mellitus was found to be the most common disease in past medical histories.
Table 1.
Demographic and pre-treatment characteristics of narrow QRS complex SVT patients
| Variables | Frequency |
|---|---|
| Mean Age (years) | 57.86 ± 20.351 years |
| Sex (M/F) | 36/41 |
| Mean Systolic Blood Pressure (mmHg) | 120.66 ± 26.120 |
| Mean Diastolic Blood Pressure (mmHg) | 73.45 ± 15.281 |
| Mean Heart Rate (bpm ) | 172.29 ± 16.502 |
| Complaints | |
| Palpitation | 58 (75.3%) |
| Resting Dyspnea | 7 (9.1%) |
| Chest Discomfort And Pain | 6 (7.8%) |
| Faintness | 5 (6.5%) |
| Syncope | 1 (1.3%) |
| Past Medical Histories | |
| Hypertension | 21 (27.3%) |
| Diabetes Mellitus | 30 (39%) |
| Myocardial Infarction | 23 (29.9%) |
| Narrow QRS complex SVT | 27 (35.1%) |
On admission, the mean systolic blood pressure was 120.66 ± 26.120 mmHg (minimum: 80-maximum: 217 mmHg) and the mean diastolic blood pressure was 73.45 ± 15.281 mmHg (minimum: 50-maximum: 144 mmHg). Mean heart rate was 172.29 ± 16.502 bpm (minimum: 140- maximum: 210 bpm) (Table 1).
Seventy seven patients affected by SVT who were unresponsive to carotid sinus massage were treated with an IV adenosine and IV diltiazem in our ED. The study design and results in patients with SVT was showen in Figure 1.
Figure 1.
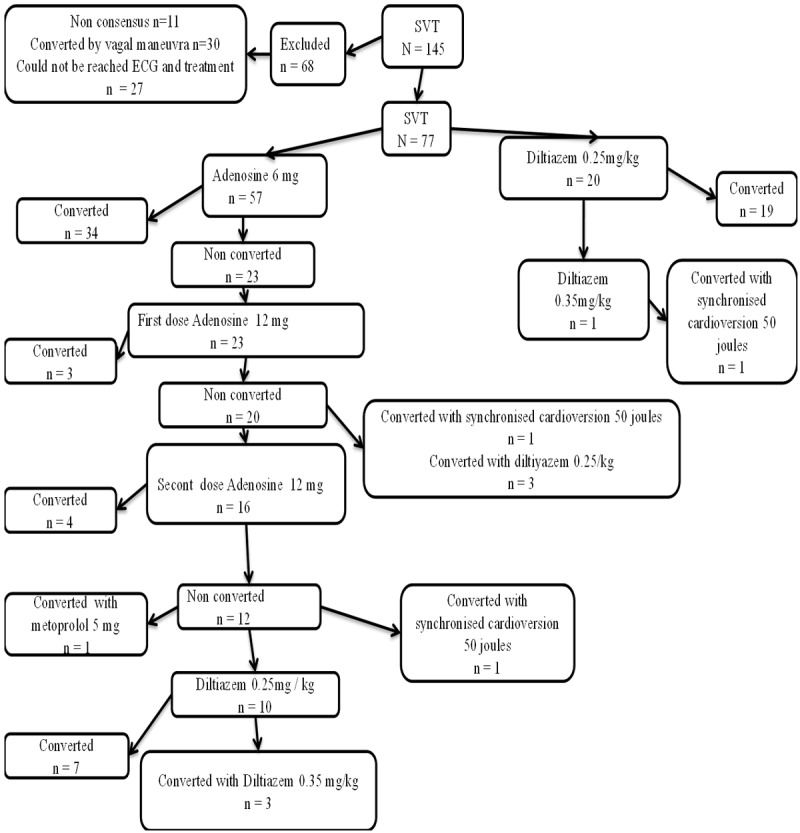
The study design and results in patients with SVT.
The study design and treatment results in patients with SVT were showen in Figure 1.
Seventy four percent of 77 patients were given adenosine as a first medication. Fifty nine point six percent of 57 patients with SVT by first dose of 6 mg adenosine, 0.5 percent of them by first dose of 12 mg adenosine and 0.7 percent of them by second dose of 12 mg adenosine were converted to sinus rhythm.
Ninety five percent of 20 patients with SVT were converted by 0.25 mg/kg diltiazem and the remaining one patient (5%) could not be converted to sinus rhythm by 0.35 mg/kg diltiazem.
One patient who was unresponsive to the second 12 mg dose adenosine was converted to sinus rhythm by 5 mg metoprolol. Three patients who were unresponsive to the first 12 mg dose of adenosine and 7 patients who were unresponsive to the second 12 mg dose of adenosine were converted to sinus rhythm by 0.25 mg diltiazem. Three patients who were unresponsive to 0.25 mg/kg diltiazem were converted to sinus rhythm by 0.35 mg/kg diltiazem. Because hipotansion occured in three patients that were unresponsive to the second and third dose diltiazem, they were converted to sinus rhythm by treatment with synchronised electrical cardioversion by 50 joules.
Conversion with the first dose of 6mg adenosine in 59.6% (34/57), conversion with the first dose of 0.25 mg/kg diltiazem in 95% (19/20) were found (P = 0.000).
The total conversion rate for adenosine (6 mg + 12 mg + 12 mg) was 71.92% (41/57) compared with 96.9% for total diltiazem (0.25 mg/kg + 0.35 mg/kg) (32/33), the difference between the two agents was statistically significant (P = 0.000) (Table 2).
Table 2.
Conversion rates of adenosine and diltiazem
| Drugs | Converted patients | p | |
|---|---|---|---|
|
| |||
| n | % | ||
| Adenosine (6 mg) | 34 | 59.6 | 0.000 |
| Diltiazem (0.25 mg/kg dose) | 19 | 95.0 | |
| Adenosine (total dose)* | 41 | 71.92 | 0.000 |
| Diltiazem (total dose)** | 32 | 96.9 | |
Adenosine total dose: 6 mg + 12 mg + 12 mg;
Diltiazem total dose: 0.25 mg/kg + 0.35 mg/kg.
The most visible ECG findings were visible P waves (21 versus 24) among the ones which were converted with both adenosine and diltiazem and the least visible ECG findings were Pseudo-S waves in the inferior leads (10 versus 4).
It was statistically significant between converted by adenosine 6 mg (first dose) to sinus rhythm and converted by diltiazem (first dose) to sinus rhythm to the presence of visible P-wave and the aVL lead notch in their ECG findings (P = 0.006, P = 0.024 respectively).
It was not statistical significant to the presence of pseudo-s-wave in inferior leads and psudo-r’-wave in lead V1 (P = 0.215, P = 0.331 respectively).
Also, it was statistically significant between converted by adenosine (total dose) to sinus rhythm and converted by diltiazem (total dose) to sinus rhythm to the presence of visible P-wave and the aVL lead notch in their ECG findings (P = 0.038, P = 0.005 respectively).
It was not statistical significant to the presence of pseudo-s-wave in inferior leads and psudo-r’-wave in lead V1 (P = 0.200, P = 0.475 respectively).
In this study, AVNRT (the presence of pseudo-s-wave in inferior leads and psudo-r’-wave in lead V1) was found on 26% of patients’ ECGs. It was not statistically significant between converted by adenosine to sinus rhythm and converted by diltiazem to sinus rhythm to the presence of AVNRT in their ECG findings (Table 3).
Table 3.
Treatment and electrocardiographic characteristics of the study population
| Electrocardiographic Characteristics | Converted drugs | ||
|
|
|||
| total adenosine n (%) | total diltiazem n (%) | p | |
|
| |||
| Visible P-wave | 21 (46.7) | 24 (53.3) | 0.038 |
| aVL notch | 16 (41) | 23 (59) | 0.005 |
| Pseudo-S-wave in leads II, III, and aVF | 10 (71.4) | 4 (28.6) | 0.200 |
| Pseudo-R’-wave in lead V1 | 12 (63.2) | 7 (36.8) | 0.475 |
| AVNRT | 13 (65) | 7 (35) | 0.168 |
| Total | 41 (56.2) | 32 (43.8) | |
|
| |||
| 6 mg adenosine n (%) | 0.25 mg/kg diltiazem n (%) | P | |
|
| |||
| Visible P-wave | 14 (38.9) | 22 (61.1) | 0.006 |
| aVL notch | 15 (41.7) | 21 (58.3) | 0.024 |
| Pseudo-S-wave in leads II, III, and aVF | 9 (69.2) | 4 (30.8) | 0.215 |
| Pseudo-R’-wave in lead V1 | 11 (61.1) | 7 (38.9) | 0.331 |
| AVNRT | 12 (63.2) | 7 (36.8) | 0.221 |
| Total | 34 (100) | 29 (100) | |
|
| |||
| 12 mg adenosine n (%) | 0.35 mg/kg diltiazem n (%) | p | |
|
| |||
| Visible P-wave | 3 (60.0) | 2 (40.0) | 0.800 |
| aVL notch | 1 (33.3) | 2 (66.7) | 0.200 |
| Pseudo-S-wave in leads II, III, and aVF | 0 (0) | 0 (0) | |
| Pseudo-R’-wave in lead V1 | 0 (0) | 0 (0) | |
| AVNRT | 0 (0) | 0 (0) | |
| Total | 4 (100) | 4 (100) | |
It was found that medium of sistolic blood pressure was 120.38 mmHg and the medium of diastolic blood pressure was 72.73 mmHg in patients with administration of Adenosine, and that the medium of sistolic blood pressure was 122.38 mmHg while the medium of diastolic blood pressure was 76.91 mmHg in patients with administration of Diltiazem. Hipotension rate for adenosine was compared with diltiazem, the difference between the two agents was not statistically significant (P > 0.05). In hospital mortality was not observed in any patient treated due to SVT.
Discussion
This study was to distinguish between AVRT and AVNRT is the first study showing that ECG criterias used in the selection of patients with narrow QRS complex SVT treated in the ED.
For the preference of the ablation treatment in narrow QRS complex stable SVT patients, some ECG criterias are used to distinguish between AVNRT and AVRT [6,7,9,15,16]. But up until now they have not been used for the preference of treatment in ED. In this study, we investigate whether it is possible to use these ECG criteria for treatment preference planning in ED.
Adenosine is recommended as the first treatment option for stable narrow QRS complex SVT in the studies [8,10-13,15,17]. With a 6 mg beginning dose of adenosine, 60% of return to sinus rhythm was observed while with the following administration of a 12 mg dose of bolus adenosine, the rate rose to 90% [18]. According to the studies, the successful return to sinus rhythm through diltiazem in SVT patients was found to be 96-98% [10,12,19]. In two randomized clinical study by Brandy W.J. Jr et al. and Cheng, K.A. et al., it was found that in stable SVT patients, adenosine and diltiazem had similar rates of return to sinus rhythm [20,21].
In our study, 59.6% of the patients returned to sinus rhythm after the first dose of adenosine while with the first following dose of 12 mg, this rate increased to 64.91% and with the second dose of 12 mg adenosine, this rate further increased to 71.92%. In this study, 95% of the diltiazem-administered returned to sinus rhythm after the first dose. The rate increased to 96.9% when diltiazem was administered to patients who did not respond to adenosine.
These ECG criteria used for distinguishing between AVNRT and AVRT for the preference of ablation treatment in narrow QRS complex stable SVT patients have not been used for the emergent treatment of stable narrow QRS complex SVT patients [5,6,13-15].
In a retrospective study by Glatter K.A. et al. [11], 85% of the AVRT patients and 86% of AVNRT patients returned to normal sinus rhythm. Electrophysiological criteria used for planning of this study. In these two groups, no statistical difference was observed in terms of terminating tachycardia through adenosine [11].
In acute episodes of AVNRT that do not respond to valsalva maneuvers, adenosine is the treatment of choice. Continuous administration of antiarrhythmic drugs maybe ineffective in up to 70% of cases [22].
In our study show that both in the first 6 mg dose of adenosine and first 0.25 mg/kg dose of diltiazem, and in total doses, the rate of return to sinus rhythm through diltiazem was found to be statistically significantly higher than that of adenosine in narrow complex SVT patients. In our study similar to literature, repeated administration of adenosine was ineffective in 70% of cases.
The studies of González-Torrecilla E. et al. [6] and Di Toro D. et al. [7] assessed the rates of these ECG criterias in SVT patients. In these studies, the rate of retrograde P wave was 40.4-44.5% in SVT patients while it was 25-36.5% in AVNRT patients and 66.7-72% in AVRT patients. And aVL lead notch was observed in 39.6% of SVT patients while it was detected in 51.3% of AVNRT patients and in 7.4% of AVRT patients. In these studies, the rate of pseudo-s-wave in inferior was 0.8-35.6% while the rate of pseudo-R’-wave in lead V1 was 25.7-32.6% [6,7].
P-wave activity in AVNRT may be only partially hidden within the QRS complex and may deform the QRS to give a pseudo-R wave in lead V1/or a pseudo- S wave in inferior leads [15]. The finding that presence of a pseudo R’ wave or pseudo S wave, or both, had an accuracy of 100% in predicting anterior-type AVNRT confirmed the previous report [9].
In our study, the rate of visible retrograde P wave (58.4%) in SVT patients was higher than those of both of these studies while the rate of pseudo-R’-wave in lead V1 (24.6%) was lower than those of both of these studies. And the rate of pseudo-S-wave in inferior (18.2%) was higher than that of González-Torrecilla E. et al. [5] study and was lower than that of Di Toro et al. [7]; and the rate of aVL lead notch (50.6%) was found to be higher than that of Di Toro et al.
In the studies retrograde P wave was observed to be higher in AVRT patients while aVL lead notch was observed to be higher in AVNRT patients [6,7].
In our study, the difference was not statistically significant between adenosine and diltiazem in the treatment of acute episodes of AVNRT. But, we report that the first treatment option may be diltiazem instead of adenosine in the presence of aVL notch and retrograde P wave in ECG of stable narrow QRS complex SVT patients.
Conclusion
Diltiazem may be the first medication (compared to adenosine) to be preferred in the presence of retrograt P wave and aVL notch in the ECG of the patients with narrow QRS complex stable SVT.
Study limitations
We used ECG criteria in the definitive diagnosis of AVRT and AVNRT which have not been used for SVT treatment in the ED up until now. However, electrophysiological studies to show which patients with these criteria we detected are AVRT or AVNRT have not been conducted.
In our next study, we supported these ECG criteria, which we think affect the emergent treatment option, by electrophysiological studies and we planned that the treatment option shall be preferred according to ECG criteria and electrophysiological study results.
Acknowledgements
We would like to thank to all the physicians, nurses and research coordinators who contributed to this study and made it possible. Special thanks to Rana Konyalioglu that contributed to statistical analysis of this study.
Disclosure of conflict of interest
None.
References
- 1.Orejarena LA, Vidaillet H Jr, DeStefano F, Nordstrom DL, Vierkant RA, Smith PN, Hayes JJ. Paroxysmal supraventricular tachycardia in the general population. J Am Col Cardiol. 1998;31:150–157. doi: 10.1016/s0735-1097(97)00422-1. [DOI] [PubMed] [Google Scholar]
- 2.Katritsis DG, Camm AJ. Classification and differential diagnosis of atrioventricular nodal re-entrant tachycardia. Europace. 2006;8:29–36. doi: 10.1093/europace/euj010. [DOI] [PubMed] [Google Scholar]
- 3.Elvas L, Gursoy S, Brugada J, Andries E, Brugada P. Atrioventricular nodal reentrant tachycardia: a review. Can J Cardiol. 1994;10:342–8. [PubMed] [Google Scholar]
- 4.McGuire MA, Bourke JP, Robotin MC, Johnson DC, Meldrum-Hanna W, Nunn GR, Uther JB, Ross DL. High resolution mapping of Koch’s triangle using sixty electrodes in humans with atrioventricularjunctional (AVnodal) reentrant tachycardia. Circulation. 1993;88:2315–28. doi: 10.1161/01.cir.88.5.2315. [DOI] [PubMed] [Google Scholar]
- 5.Whinnett ZI, Sohaib SM, Davies DW. Diagnosis and management of supraventricular tachycardia. BMJ. 2012;345:e7769. doi: 10.1136/bmj.e7769. [DOI] [PubMed] [Google Scholar]
- 6.González-Torrecilla E, Almendral J, Arenal A, Atienza F, del Castillo S, Fernández-Avilés F. Independent predictive accuracy of classicalelectrocardiographic criteria in the diagnosis of paroxysmal atrioventricular reciprocating tachycardias in patients without pre-excitation. Europace. 2008;10:624–8. doi: 10.1093/europace/eun084. [DOI] [PubMed] [Google Scholar]
- 7.Di Toro D, Hadid C, López C, Fuselli J, Luis V, Labadet C. Utility of the aVL lead in the electrocardiographic diagnosis of atrioventricular node re-entrant tachycardia. Europace. 2009;11:944–948. doi: 10.1093/europace/eup130. [DOI] [PubMed] [Google Scholar]
- 8.Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW Kudenchuk PJ, Ornato JP, McNally B, Silvers SM, Passman RS, White RD, Hess EP, Tang W, Davis D, Sinz E, Morrison LJ. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Cardiovascular Care. Circulation. 2010;122(Suppl 3):S729–67. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]
- 9.Tai CT, Chen SA, Chiang CE, Lee SH, Wen ZC, Chiou CW Ueng KC, Chen YJ, Yu WC, Chang MS. A new electrocardiographic algorithm using retrograde p waves for differentiating atrioventricular node reentrant tachycardia from atrioventricular reciprocating tachycardia mediated by concealed accessory pathway. J Am Coll Cardiol. 1997;29:394–402. doi: 10.1016/s0735-1097(96)00490-1. [DOI] [PubMed] [Google Scholar]
- 10.Lim SH, Anantharaman V, Teo WS, Chan YH. Slow infusion of calcium channel blockers compared with intravenous adenosine in the emergency treatment of supraventricular tachycardia. Resuscitation. 2009;80:523–528. doi: 10.1016/j.resuscitation.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 11.Riccardi A, Arboscello E, Ghinatti M, Minuto P, Lerza R. Adenosine in the treatment of supraventricular tachycardia: 5 years of experience (2002-2006) Am J Emerg Med. 2008;26:879–82. doi: 10.1016/j.ajem.2007.11.029. [DOI] [PubMed] [Google Scholar]
- 12.Lim SH, Anantharaman V, Teo WS. Slow-infusion of calcium channel blockers in the emergency management of supraventricular tachycardia. Resuscitation. 2002;52:167–74. doi: 10.1016/s0300-9572(01)00459-2. [DOI] [PubMed] [Google Scholar]
- 13.Glatter KA, Cheng J, Dorostkar P, Modin G, Talwar S, Al-Nimri M Lee RJ, Saxon LA, Lesh MD, Scheinman MM. Electrophysiologic effects of adenosine in patients with supraventricular tachycardia. Circulation. 1999;99:1034–1040. doi: 10.1161/01.cir.99.8.1034. [DOI] [PubMed] [Google Scholar]
- 14.Hohnloser SH, Zabel M. Short- and long-term efficacy and safety of flecainide acetate for supraventricular arrhythmias. Am J Cardiol. 1992;70:3A–9A. doi: 10.1016/0002-9149(92)91071-b. [DOI] [PubMed] [Google Scholar]
- 15.Blomström-Lundqvist C, Scheinman MM, Aliot EM, Alpert JS, Calkins H, Camm AJ, Campbell WB, Haines DE, Kuck KH, Lerman BB, Miller DD, Shaeffer CW, Stevenson WG, Tomaselli GF, Antman EM, Smith SC Jr, Alpert JS, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Hiratzka LF, Hunt SA, Jacobs AK, Russell RO Jr, Priori SG, Blanc JJ, Budaj A, Burgos EF, Cowie M, Deckers JW, Garcia MA, Klein WW, Lekakis J, Lindahl B, Mazzotta G, Morais JC, Oto A, Smiseth O, Trappe HJ. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the European Society of Cardiology committee for practice guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42:1493–1531. doi: 10.1016/j.jacc.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 16.Letsas KP, Weber R, Siklody CH, Mihas CC, Stockinger J, Blum T Kalusche D, Arentz T. Electrocardiographic differentiation of common type atrioventricular nodal reentrant tachycardia from atrioventricular reciprocating tachycardia via a concealed accessory pathway. Acta Cardiol. 2010;65:171–6. doi: 10.2143/AC.65.2.2047050. [DOI] [PubMed] [Google Scholar]
- 17.Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, Kudenchuk PJ, Ornato JP, McNally B, Silvers SM, Passman RS, White RD, Hess EP, Tang W, Davis D, Sinz E, Morrison LJ. Part 8: Adult Advanced Cardiovascular Life Support 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:729–767. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]
- 18.DiMarco JP, Miles W, Akhtar M, Milstein S, Sharma AD, Platia E, McGovern B, Scheinman MM, Govier WC. Adenosine for paroxysmal supraventricular tachycardia: dose ranging and comparison with verapamil. Assessment in placebo-controlled, multicenter trials. The Adenosine for PSVT Study Group. Ann Intern Med. 1990;113:104–110. doi: 10.7326/0003-4819-113-2-104. [DOI] [PubMed] [Google Scholar]
- 19.Dougherty AH, Jackman WM, Naccarelli GV, Friday KJ, Dias VC. Acute conversion of paroxysmal supraventricular tachycardia with intravenous diltiazem. Am J Cardiol. 1992;70:587–592. doi: 10.1016/0002-9149(92)90196-6. [DOI] [PubMed] [Google Scholar]
- 20.Brady WJ Jr, DeBehnke DJ, Wickman LL, Lindbeck G. Treatment of Out-of-hospital Supraventricular Tachycardia: Adenosine vs Verapamil. Acad Emerg Med. 1996;3:574–85. doi: 10.1111/j.1553-2712.1996.tb03467.x. [DOI] [PubMed] [Google Scholar]
- 21.Cheng KA Intravenous Adenosine versus Verapamil in Terminating Episodes of Paroxysmal Supraventricular Tachycardia Study Group. [A randomized, multicenter trial to compare the safety and efficacy of adenosine versus verapamil for termination of paroxysmal supraventricular tachycardia] . Zhonghua Nei Ke Za Zhi. 2003;42:773–6. [PubMed] [Google Scholar]
- 22.Katritsis DG, Camm AJ. Atrioventricular nodal reentrant tachycardia. Circulation. 2010;122:831–840. doi: 10.1161/CIRCULATIONAHA.110.936591. [DOI] [PubMed] [Google Scholar]


