Abstract
The purpose of our study was to accurately visualize and measure the normal anatomy and size of the pterygoid canal with thin-section (0.5 mm), high-resolution computed tomography (HRCT) as well as multiplanar reconstruction (MPR) and curved planar reconstruction (CPR) technologies to obtain credible and comprehensive information for clinical management. Both axial HRCT and MPR images of the pterygopalatine fossa were obtained in 167 normal adult subjects, who exhibited variable positions of pterygoid canal relative to the sphenoid sinus floor and cavity. The morphology and size of the pterygoid canal was observed and measured, respectively. All pterygoid canals (100%, 334/334) were well delineated on HRCT images. Statistical analyses showed no significant difference between the mean length of the left (12.6 ± 2.3 mm) and right pterygoid canals (12.5 ± 2.9 mm) (P = 0.405). The mean diameter of anterior, median and posterior opening of the left and right pterygoid canals exhibited no significant differences (all P > 0.05); the bilateral median opening possessed the smallest diameter (P < 0.001). Submillimeter, thin-section HRCT scan and appropriate postprocessing reconstruction technologies could clearly visualize the morphologic features of the pterygoid canal and adjacent structures, which may be helpful for making diagnostic and therapeutic decisions.
Keywords: Pterygoid canal, anatomy, HRCT
Introduction
The pterygoid canal connects pterygopalatine fossa and foramen lacerum with arteries, veins and nerves running through it [1]. Vidian neurectomy is widely considered to be highly effective in treating allergic rhinitis, vasomotor rhinitis, Sluder’s neuralgia, crocodile tears syndrome, nasal polyps and other diseases. In addition, the pterygoid canal and its contents are often subject to iatrogenic injury when surgery is performed near the sphenoid and its surrounding structures. Therefore, an accurate understanding of the pterygoid canal and its adjacent structures is helpful for developing surgical plans and reducing risk [2-5]. However, the pterygoid canal is a small structure in a relatively deep anatomical location. Due to the poor resolution of conventional computed tomography (CT), anatomical imaging studies of the pterygoid canal are rarely reported. Specifically, data regarding the length of pterygoid canal obtained from in vivo anatomical imaging are extremely rare in the literature [6-11]. With the wide application of high-resolution CT (HRCT) technology, the visualization of pterygoid canal structure has improved significantly. On basis of this perspective, we applied submillimeter (0.5 mm), thin-section HRCT and multidetector CT (MDCT) post-reconstruction technology to provide a more comprehensive description of pterygoid canal morphology and diameter measurement in the Chinese population, thereby providing additional decision-making criteria for basic research and clinical practice.
Materials and methods
Study subjects
HRCT spiral scans were performed on 420 subjects who were seen in our hospital for head and neck exams. All subjects recruited for this study met the research requirements. The inclusion criteria were the following: 1) normal healthy subjects older than 18 years old; and 2) no disease or surgical history of pterygopalatine fossa, connection structure or nasal sinus. The exclusion criteria were the following: 1) participants who could not cooperate with the medical exam; 2) imaging with artifacts; 3) poor image quality that did not meet the observation requirements. A total of 167 subjects met the above study requirements; their age ranged from 18 to 78 years with a mean age of 41.9 ± 14.5 years. There were 83 men (mean age, 41 years ± 10 (standard deviation); median age, 41 years; age range, 18-74 years) and 84 women (mean age, 42 years ± 8; median age, 42 years; age range, 19-68 years). There was no significant difference in age between men and women (P = 0.76, independent samples t-test). This study was approved by an institutional review board, and written informed consent was obtained from each subject.
CT imaging assessment
A Sensation 16 spiral CT scanner (Sensation 16; Siemens Medical Solutions, Erlangen, Germany) was utilized for volume scanning. The scan parameters were as follows: 120 Kv; 100 mAs; pixels, 512 × 512; and thickness, 0.5 mm. For the scan range, the plane of the hard palate was set as baseline, and continuous parallel scanning was performed from the lower edge of the hard palate plane upward to the level of the posterior clinoid plane. Post-processing of the raw scan data was carried out on a Leonardo workstation. The reconstruction slice thickness was also 0.5 mm. First, standard axial, coronal and sagittal MPR reconstructions were performed followed by oblique sagittal MPR reconstruction along the long axis of pterygoid canal and curved planar reconstruction (CPR) at axial plane tracking along the pterygoid canal. The window width was 4000 HU, and the window level was 700 HU.
Observation and measurement
(1) Pterygopalatine fossa: pterygoid canal morphology was observed in cross-section, coronal and sagittal planes, and the opening of pterygoid canal was measured. (2) Pterygoid canal: the morphology and the track of the pterygoid canal were observed in cross-section, coronal and oblique sagittal planes. The average diameter of the anterior opening was measured in the coronal plane. The measurement of the anterior opening was taken when we observed a complete circular shape at the wall of the pterygoid canal that was successively observed in coronal planes. The length of the pterygoid canal and the diameters of the median and posterior openings were measured in the oblique sagittal plane using CPR along the track of the pterygoid canal. The posterior opening was determined as the presence of the posterior end of the pterygoid canal. The diameter of the median opening was measured at the median section between the anterior and posterior openings. All measurements were performed in triplicate, and the average of the three measurements was taken as the final result. (3) The relationship between the pterygoid canal and sphenoid sinus was based on the anatomical positions of both structures, the relationship was divided into the following types: Type A, pterygoid canal lies completely within the floor of the sphenoid sinus or is embedded in the body of adjacent sphenoid bones; Type B, the pterygoid canal partially protrudes into the sphenoid sinus floor, and less than two-thirds of the canal wall is surrounded by sphenoid sinus air cells; Type C, at least two-thirds of the pterygoid canal is embedded inside the sphenoid sinus and surrounded by air cells of sphenoid sinus.
Statistical analysis
All numeric variables are presented as the mean ± standard deviation (X ± SD) and 95% confidence interval (CI) and were assessed for normal distribution. Statistical analysis was performed in accordance with the left and right sides, gender and the diameters of the ipsilateral anterior, median and posterior openings. Differences between left and right sides were assessed with paired two-sample t-tests. The gender difference for the ipsilateral pterygoid canal was tested with an independent t-test. One-way analysis of variance (ANOVA) and the Bonferroni method were applied to compare the ipsilateral anterior, median and posterior opening diameters among groups. SPSS statistical software (version 13.0, Chicago, IL, USA) was used for all statistical analyses, with P < 0.05 considered as statistical significance.
Results
The morphology of pterygoid canal
The detection rate of 334 pterygoid canals on HRCT was 100% among 167 participants. We found that pterygoid canals were bilaterally symmetric in 76.6% of participants (128/167) (Figure 1A), with the pterygoid canal observed as a slightly curved, thin tube in cross-section and the oblique sagittal plane and connecting the foramen lacerum from anterior to posterior (Figure 1B). In the coronal plane, 114 pterygoid canals were round (34.1%) (Figure 1C) and 220 were oval (65.9%) (Figure 1D). Among the 334 pterygoid canals, 318 (95.2%) showed a slightly curved track from the internal-anterior to external-posterior axis with an arc shape; 14 (4.2%) showed a horizontal track from the anterior to posterior axis; and the other 2 (0.6%) showed a slightly curved track from the external-anterior to internal-posterior axis.
Figure 1.
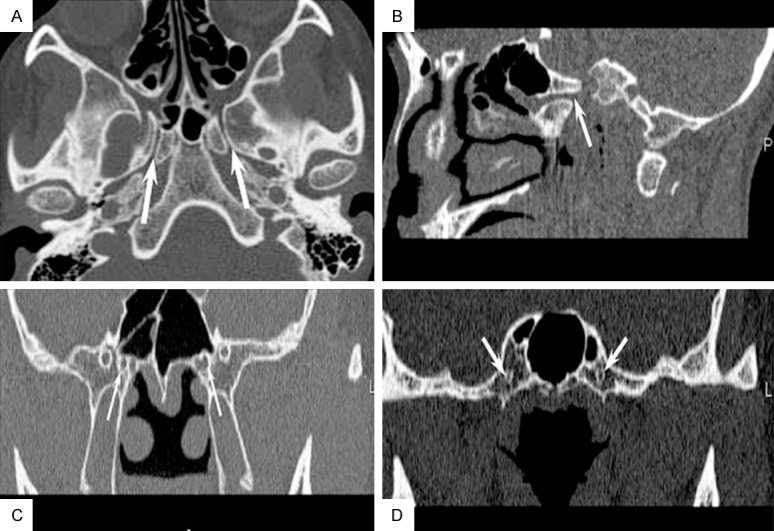
On high resolution CT, axial-section (A) and oblique sagittal reconstruction (B) images show symmetric bilateral pterygoid canals (white arrows) with a narrow middle and relatively wider anterior and posterior openings connecting the pterygopalatine fossa and foramen lacerum shows; coronal section images detect oval-shaped anterior (C) and median openings (D) of pterygoid canals (white arrows).
Pterygoid canal diameter
No significant difference was found between the length of the left (12.6 ± 2.3 mm; 95% CI: 10.2-14 .6) and right pterygoid canals (12.5 ± 2.9 mm; 95% CI: 10.4-14.4) among all subjects (t = 0.835, P = 0.405). The mean diameters of the anterior, median and posterior openings of the left pterygoid canal were 2.7 ± 0.7 mm (95% CI: 2.5-2.8), 1.9 ± 0.5 mm (95% CI: 1.8-2.0) and 1.4 ± 0.6 mm (95% CI: 1.2-1.5), respectively. The mean diameters of the anterior, median and posterior openings of the right pterygoid canal were 2.7 ± 0.6 mm (95% CI: 2.6-2.8), 1.9 ± 0.6 mm (95% CI: 1.8-1.9) and 1.3 ± 0.5 mm (95% CI: 1.2-1.4), respectively. The bilateral pterygoid canals gradually widened from the middle portion to both ends to exhibit a funnel shape. The anterior and median openings had the widest and the smallest diameters, respectively. The difference was statistically significant (left side: F = 217.603, P < 0.001; right side: F = 247.336, P < 0.001). However, there was no gender difference or diameter difference in anterior, median and posterior openings between the left and right pterygoid canals (all P > 0.05) (Table 1).
Table 1.
The measurement of pterygoid canals in 167 normal adults (mm)
| Length | Anterior opening | Median opening | Posterior opening | ||
|---|---|---|---|---|---|
| Left | Male | 12.9 ± 2.5 | 2.6 ± 0.8 | 1.4 ± 0.5 | 1.9 ± 0.5 |
| Female | 12.3 ± 2.0 | 2.7 ± 0.6 | 1.4 ± 0.5 | 1.9 ± 0.5 | |
| Right | Male | 13.0 ± 2.6 | 2.6 ± 0.7 | 1.3 ± 0.5 | 1.8 ± 0.5 |
| Female | 11.9 ± 3.1 | 2.8 ± 0.6 | 1.4 ± 0.5 | 1.9 ± 0.5 | |
The relationship between pterygoid canal and sphenoid sinus
We divided the participants into different types depending on the relationship between the pterygoid canal and sphenoid sinus. Type A, the majority of subjects had pterygoid canals within the sphenoid sinus floor, including 130 left (77.8%) and 126 right pterygoid canals (75.4%) (Figure 2A); Type B, a smaller percentage was completely inside the sphenoid sinus, including 19 left (11.4%) and 24 right pterygoid canals (14.4%) (Figure 2B); and Type C, a similar number of canals were partially inside the sphenoid sinus, including 18 left (10.8%) and 17 right pterygoid canals (10.2%) (Figure 2C). Additionally, approximately 0.6% of the cases exhibited incomplete pterygoid canal bone structure (Figure 2D).
Figure 2.
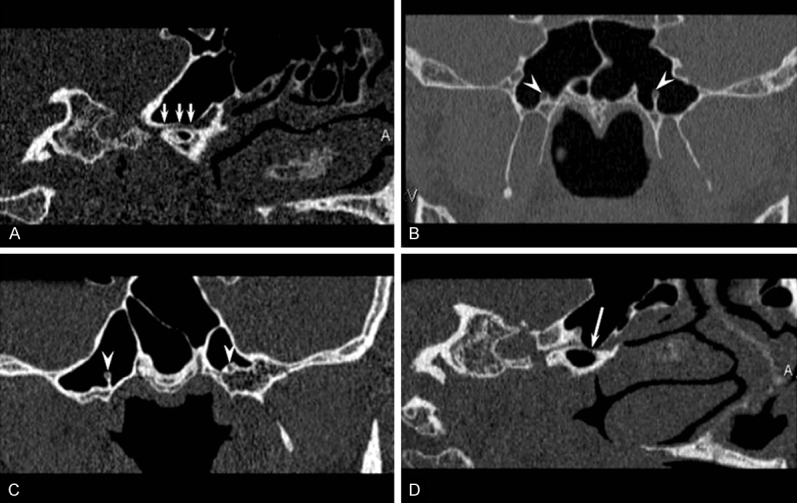
Thin-section CT reconstruction images show bilateral pterygoid canals within the sphenoid sinus floor (white arrows) (A), inside the sphenoid sinus (arrowheads) (B), the right pterygoid canal inside the sphenoid sinus and the left pterygoid canal partially inside the sphenoid sinus (arrowheads) (C), and the superior wall of the pterygoid canal is missing (white arrow) (D).
Discussion
This study demonstrates that submillimeter, thin-section HRCT scanning and post-processing reconstruction techniques can successfully visualize pterygoid canal morphological features and connection status. For the first time, we applied HRCT to measure canal length and the diameters of the anterior, median and posterior openings, and we described the relationship between the pterygoid canal and sphenoid sinus floor.
The pterygoid canal is one of the important passageways of the pterygopalatine fossa. It lies between the pterygoid and sphenoid sinuses, passing through the foramen lacerum posteriorly [1]. HRCT can clearly visualize the entire pterygoid canal and its adjacent structures. Pandolfo et al. [8], Rumboldt et al. [9] and Kim et al. [10] reported 95%, 98% and 100% pterygoid canal detection rates, respectively. Because we applied submillimeter, thin-section HRCT scan, all subjects’ pterygoid canals were clearly visualized (100%) in considerable detail. Cross-section HRCT revealed that most pterygoid canals were aligned along an interior-anterior to external-posterior axis. The pterygoid canal was a slightly curved bony structure that narrowed in the middle and widened at the anterior and posterior openings. Kim et al. [10] reported that just 19.5% of pterygoid canals were aligned in external-anterior to internal-posterior axis. The anterior opening of pterygoid canal was on the posterior wall of pterygopalatine fossa and was usually round or oval in shape. The posterior opening was slightly superior to the anterior wall of the foramen lacerum and was also round or oval shaped [6,7]. Coronal HRCT revealed that the round- or oval-shaped pterygoid canal sat on the floor of the sphenoid sinus. Overall, we observed that the morphological features of the pterygoid canal were superiorly visualized with MPR reconstruction along the structure’s track.
Pterygoid canal diameters have always exhibited relatively large variability due to different study subjects and measurement standards. Autopsy results revealed that pterygoid canal length was 14.74 ± 1.64 mm, and the diameters of the anterior and posterior openings were 3.53 ± 0.64 and 1.72 ± 0.50 mm, respectively. Pandolfo et al. [8] reported that the average anterior and posterior opening diameters were 2.5 and 1.0 mm, respectively. The HRCT results in this study showed that the mean pterygoid canal length was 12.5 ± 3.0 mm, and the diameters of the anterior and posterior openings were 2.7 ± 0.7 and 1.8 ± 0.5 mm, respectively. Studies that collected data from around the world reported that the pterygoid canal was funnel-shaped with a relatively narrow middle section [1,6-8,11-13]. However, there were previously no specific measurement values for the median opening, which we measured as 1.3 ± 0.5 mm, confirming that it was significantly smaller than the anterior and posterior openings.
The pterygoid canal is closely related to sphenoid sinus. Pandolfo and colleagues [8] reported that the bony wall between the pterygoid canal and sphenoid sinus was relatively thin, not exceeding 5 mm, and was incomplete in places. Therefore, special attention should be paid to the location of pterygoid canal relative to sphenoid sinus during surgery to avoid damaging nerves and blood vessels in the pterygoid canal [4,14,15]. According to previous studies [8,10], the majority of pterygoid canals (approximately 55%) lie under the sphenoid sinus floor with intact bony walls separating them from the sphenoid sinus. Some pterygoid canals (approximately 31%) partially protrude into the sphenoid sinus but have intact walls separating the two structures. Approximately 6% of pterygoid canals protrude into the sphenoid sinus and lack entire superior walls. This study indicated that coronal CT scans or coronal MPR can clearly reveal the relationship between the pterygoid canal and sphenoid sinus. Therefore, sphenoid sinus diseases or surgery can easily damage the nerves and blood vessels inside the pterygoid canal, especially when the structure is completely or partially inside the sphenoid sinus.
The vidian artery and corresponding nerves pass through the pterygoid canal and is a branch of maxillary artery [1]. The vidian artery joints parasympathetic fibers to the sphenopalatine ganglion in the upper pterygopalatine fossa [16]. The vidian nerve is formed by the great petrosal nerve, the deep petrosal nerve and the sympathetic fibers along the internal carotid artery. HRCT revealed that the pterygoid canal is a straight or slightly curved thin bony tube in alignment with the external-posterior to internal-anterior axis. The diameter gradually widens in the anterior direction. Previously published studies [6-10] reported that the diameters of the anterior and posterior openings were 2.5 and 1.0 mm, respectively. The results measured by HRCT in this study showed that the average diameters of the anterior and posterior openings were 2.3 and 1.0 mm, respectively. The pterygoid canal is closely related to the sphenoid sinus. Pandolfo et al. [8] reported that the distance between the pterygoid canal and the sphenoid floor ranged from 0 to 5 mm. We found that 55% of pterygoid canals were located under the sphenoid sinus floor with intact bony wall separating them from the sphenoid sinus; 31% of pterygoid canals were completely inside the sphenoid sinus; 8% of pterygoid canals showed asymmetric separation or no bone separating from sphenoid sinus; and 6% of pterygoid canals showed no superior wall and thereby passed directly through the sphenoid sinus. Therefore, special attention should be paid to the location of the pterygoid canal relative to the sphenoid sinus during surgery to avoid damaging the nerves and blood vessels in the pterygoid canal. HRCT of the pterygoid canal should include both cross-sectional and coronal plane images. The former reveal the entire morphology of the pterygoid canal, as well as its relationship to the pterygopalatine fossa and foramen lacerum, while coronal images demonstrate the relationship between the pterygoid canal and sphenoid sinus. The combination of both scan angles can accurately reveal the relationship between the pterygoid canal and surrounding structures.
The anterior opening is the optimal position for vidian nerve occlusion or nerve resection procedure. Approximately 81% of surgical procedures can successfully enter the pterygoid canal through the sphenopalatine foramen [4,10,15]. HRCT scan can accurately reveal the anterior opening of the pterygoid canal, as well as possible pathological changes, which is helpful for preoperative evaluation. Some craniofacial tumors (e.g., nasopharyngealcarcinoma) can have perineural invasion along the pterygoid canal, resulting in canal expansion and bony wall destruction [17-19]. HRCT scanning has a relatively higher sensitivity for revealing pterygoid canal injuries due to these diseases. Knowledge of the normal opening diameter of the pterygoid canal is helpful in developing clinical treatment plans and evaluating prognosis.
In summary, the application of submillimeter, thin-section HRCT scanning and MDC reconstruction can clearly reveal the morphology, size and adjacent structures of the pterygoid canal. In addition, it can provide comprehensive and accurate imaging information for the diagnosis of related diseases and guide the development of surgical plans for skull base surgery and endoscopic surgery.
Disclosure of conflict of interest
None.
References
- 1.Daniels DL, Mark LP, Ulmer JL, Mafee MF, McDaniel J, Shah NC, Erickson S, Sether LA, Jaradeh SS. Osseous anatomy of the pterygopalatine fossa. AJNR. 1998;19:1423–1432. [PMC free article] [PubMed] [Google Scholar]
- 2.Chong VF, Fan YF. Pterygopalatine fossa and maxillary nerve infiltration in nasopharyngeal carcinoma. Head Neck. 1997;19:121–125. doi: 10.1002/(sici)1097-0347(199703)19:2<121::aid-hed6>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 3.Blandino A, Gaeta M, Minutoli F, Pandolfo I. CT and MR findings in neoplastic perineural spread along the vidian nerve. Eur Radiol. 2000;10:521–526. doi: 10.1007/s003300050089. [DOI] [PubMed] [Google Scholar]
- 4.Wormald PJ, Athanasiadis T, Rees G, Robinson S. An evaluation of effect of pterygopalatine fossa injection with local anesthetic and adrenalin in the control of nasal bleeding during endoscopic sinus surgery. Am J Rhinol. 2005;19:288–292. [PubMed] [Google Scholar]
- 5.Chung NN, Ting LL, Hsu WC, Lui LT, Wang PM. Impact of magnetic resonance imaging versus CT on nasopharyngeal carcinoma: primary tumor target delineation for radiotherapy. Head Neck. 2004;26:241–246. doi: 10.1002/hed.10378. [DOI] [PubMed] [Google Scholar]
- 6.Sepahdari AR, Mong S. Skull base CT: normative values for size and symmetry of the facial nerve canal, foramen ovale, pterygoid canal, and foramen rotundum. Surg Radiol Anat. 2013;35:19–24. doi: 10.1007/s00276-012-1001-4. [DOI] [PubMed] [Google Scholar]
- 7.Omami G, Hewaidi G, Mathew R. The neglected anatomical and clinical aspects of pterygoid canal: CT scan study. Surg Radiol Anat. 2011;33:697–702. doi: 10.1007/s00276-011-0808-8. [DOI] [PubMed] [Google Scholar]
- 8.Pandolfo I, Gaeta M, Blandino A, Longo M. The radiology the pterygoid canal: normal and pathologic findings. AJNR. 1987;8:479–483. [PMC free article] [PubMed] [Google Scholar]
- 9.Rumboldt Z, Castillo M, Smith JK. The palatovaginal canal: can it be identified on routine CT and MR imaging? AJR. 2002;179:267–272. doi: 10.2214/ajr.179.1.1790267. [DOI] [PubMed] [Google Scholar]
- 10.Kim HS, Kim DI, Chung IH. High-resolution CT of the pterygopalatine fossa and its communications. Neuroradiology. 1996;38(Suppl 1):S120–126. doi: 10.1007/BF02278138. [DOI] [PubMed] [Google Scholar]
- 11.Erdogan N, Unur E, Baykara M. CT anatomy of pterygopalatine fossa and its communications: a pictorial review. Comput Med Imaging Graph. 2003;27:481–487. doi: 10.1016/s0895-6111(03)00038-7. [DOI] [PubMed] [Google Scholar]
- 12.Daniels DL, Rauschning W, Lovas J, Williams AL, Haughton VM. Pterygopalatine fossa: computed tomography studies. Radiology. 1983;149:511–516. doi: 10.1148/radiology.149.2.6622697. [DOI] [PubMed] [Google Scholar]
- 13.Ginsberg LE, Pruett SW, Chen MY, Elster AD. Skull-base foramina of the middle cranial fossa: reassessment of normal variation with high-resolution CT. AJNR. 1994;14:283–291. [PMC free article] [PubMed] [Google Scholar]
- 14.Cavallo LM, Messina A, Gardner P, Esposito F, Kassam AB, Cappabianca P, de Divitiis E, Tschabitscher M. Extended endoscopic endonasal approach to the pterygopalatine fossa: anatomical study and clinical considerations. Neurosurg Focus. 2005;19:E5. [PubMed] [Google Scholar]
- 15.Alfieri A, Jho HD, Schettino R, Tschabitscher M. Endoscopic endonasal approach to the pterygopalatine fossa: anatomic study. Neurosurgery. 2003;52:374–378. doi: 10.1227/01.neu.0000044562.73763.00. [DOI] [PubMed] [Google Scholar]
- 16.Osborn AG. The vidian artery: normal and pathologic anatomy. Radiology. 1980;136:373–378. doi: 10.1148/radiology.136.2.7403513. [DOI] [PubMed] [Google Scholar]
- 17.Rypens R, Lemort M, Dor P, Baleriaux D. Vidian metastasis of adenoid cystic carcinoma. J Neuroradiol. 1991;18:286–289. [PubMed] [Google Scholar]
- 18.Pandolfo I, Gaeta M, Blandino A, Longo M, Faranda C. Perineural spread of nasopharyngeal carcinoma: radiological and CT demonstration. Eur J Radiol. 1988;8:231–235. [PubMed] [Google Scholar]
- 19.Hirano H, Kato K, Takahashi S, Sashi R, Tate E, Watanabe O, Okane K, Watarai J. Comparison of MR imaging with CT in depiction of tumour extension into the pterygopalatine fossa. Clin Radiol. 1999;54:361–366. doi: 10.1053/crad.1999.0179. [DOI] [PubMed] [Google Scholar]


