Abstract
Objective: To analyze the outcomes of total elbow arthroplasty in the treatment of elderly type C distal humeral fractures and discuss the clinic efficacy. Methods: 8 cases of elderly type C distal humeral fractures, Male was in one case, female in seven cases, and the average age was 66.5 years (60-81). All cases were closed fractures because of falling and none had associated injuries. According to AO classification, type C1 were in one cases, C2 in four cases and C3 in three cases. The average time from injury to operation was 5.5 days (3-9), and the type of prosthesis which all cases replaced was Coonrad-Marrey. The postoperative follow-up was obtained regularly which the contents included Mayo elbow score, pain evaluation, the motion range and the stability of the elbow, muscle strength, examination of related complications such as heterotopic ossification, prosthesis loosening and nerve damage. Results: The incision infection was in one case, ulnar nerve symptom in two cases, weakness of musculus triceps brachii in one case and mild pain of elbow in two cases. The average motion rage of elbow was 103.5±3.2 degree (78-118) in flexion-extension and 126.4±4.1 degree (94-148) in rotation. All elbow joints were stable postoperatively, no prosthesis loosening and apparent wear was found. The heterotopic ossification was found in 1 case. The average Mayo elbow score was 85.2±3.4 (75-95), four cases of excellent and four cases of good. Conclusion: The total elbow arthroplasty was recommended in clinic to treat elderly type C distal humeral fractures because the clinic outcomes are satisfied.
Keywords: Humerus, fractures, elbow, arthroplasty, replacement
Introduction
Distal humerus fracture, approximately accounting for 2% of total fractures [1,2], is commonly seen in elderly females [3,4]. For total intra-articular fracture, i.e. intercondylar fracture (Type C of AO), the anatomical structure of joint must be recovered through operation, and early functional exercise shall be performed. Elderly patients, however, due to their osteoporosis and poor bone quality, usually go through severe fracture; for traditional internal fixation, anatomical reduction is difficult to proceed and the braking time is too long, which influence the functional recovery after operation, and lead to invalidation of fixation and nonunion and other severe complications with higher possibilities. The occurrence reported by literatures varies from 5% to 25% [5]. Hence, some scholars recommend one-staged elbow joint replacement [6-11] for distal humerus fracture of type C (total intra-articular fracture, AO type) in elderly patients, which achieves a satisfactory effect [12,13]. However, the sample size of reported cases is relatively small, and the follow-up time is comparatively short, the long-term therapeutic effect remains to be assessed further.
In this paper, elderly patients with distal humerus fracture of type C who had gone through elbow joint replacement in recent years were studied, and postoperative pain, function and complication were analyzed. A comprehensively judgment of the curative effect of this method, will offer reference to clinical practice.
Materials and methods
General information
From March 2007 to March 2011, elbow joint replacement were performed in eight elderly patients with distal humerus fracture of type C who aged from 60 to 81 years old with a mean of 66.5, including one male and seven females, in our hospital. These patients had no past history of disease in elbow. Of these patients, three suffered from left fracture and five from right ones. All fractures were closed fracture, which were caused by falling without combined injuries and of which one was C1 type, four were C2 and three were C3. Bone mineral density examination were performed before operation and the result showed that five patients had osteoporosis and the other three got close to the lower limit of the normal range. Of the patients, one was experiencing diabetes, two coronary heart disease, four hypertension and one cerebral embolism (affected limbs at non-fracture side). The operation was not carried out until pre-operative assessment and medical symptoms were adjusted to the satisfactory conditions. All joint prostheses were semi-restricted Coonrad-Morrey ones (Zimmer, America).
Operation
When brachial plexus block or general anesthesia was satisfying, make the patient be at supine position; inflate air and pressurize after blood was driven by tourniquet. The interior posterior median approach olecranon appeared and protected the ulnar nerve. Bryan-Morrey triceps can be used to pull out the approach; release triceps attachment points from the back of olecranon; peel the anconeus and open the exposed fracture outside and the proximal ulna. If the bilateral condylus humeri were damaged, the medial epicondyle can be exposed first and protect the ulnar nerve; peel the soft tissue from fracture fragments. Pull out the subcutaneous tissue towards side. Make the lateral epicondyle exposed, peel the soft tissue and remove all fractured fragment. Expose the humerus at outside of triceps; treat humerus medullary cavity; afterwards, insert prosthesis at humerus side or tested model, making its convex wing at forehead place at the top of coronoid fossa and the rear plane consistent with that of malleolus medialis and lateral condyle of humerus. If fracture has already extended to the proximal side of coronoid fossa, give an axial load to the forearm at elbow flexion position after inserting the tested model, so as to estimate the depth that the humerus prosthesis has inserted. Perform osteotomy for distal humerus with osteotomy template; one may peel and pull out partial triceps from interior olecranon, rotate forearm, and expose olecranon tip and coronoid process fundus. Remove the olecranon tip; conduct high-speed drill and file humerus medullary cavity from coronoid process fundus and use pointed drill to open it; bone file gradually extend humerus medullary cavity. Pay special attention to ensure that medullary space file perpendicular to distal plane of ulna to ensure that alignment of prosthesis inside the medullary space is normal. Place the tested model of prosthesis; try restoration and examine the activity of elbow joint. The standard to judge whether the depth of prosthesis is appropriate is that the center of the prosthesis should be at the center of olecranon meniscus incisura. Adjust the axial rotation of prosthesis, to make its curvature movement axis perpendicular to the plane at the back of olecranon. Bone cement is to be injected first into humerus medullary cavity and then into ulna medullary cavity. Insert the prosthesis at the side of ulna, and then trim the taken broken bone blocks into appropriate shape and then transplant them to forehead of distal humerus, and afterwards, insert prosthesis at the side of humerus and knock on it, to make the bone block tightly close to the wing of prosthesis. Insert connection set for fixation; the intra-operative test and imaging examination are to used for confirmation of firmness of joint; after being fixed firmly, wash it; distal ulna drills hole to musculus triceps brachii and suture the musculus flexor and common extensor tendon with the triceps (Figure 1). Suture the incision layer by layer, and place drainage tube; sterility accessories are used for pressure dressing; conduct external fixation for elbow joint, making it place at mild flexed position.
Figure 1.
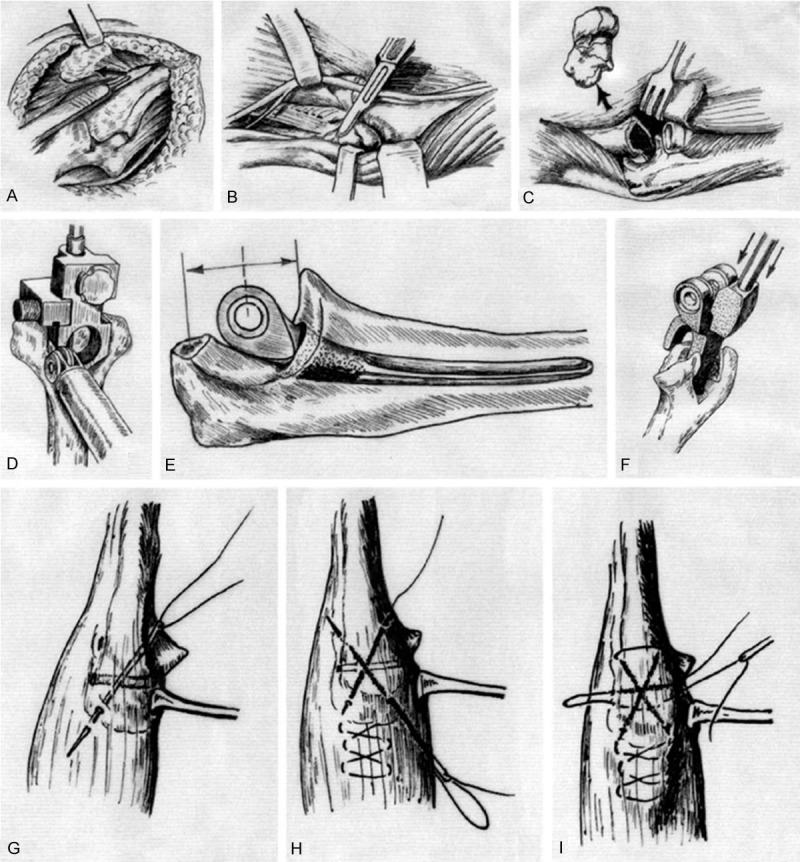
Schematic Diagram for Operation Procedure. (A) Use Bryan-Money approach (triceps-reflecting approach); through releasing the Sharpey fiber on olecranon, pull out the musculus triceps brachii from inside to outside; remain the continuity of muscle and the expanded part of its facies lateralis anconeus. Rotate the ulna to expose and use ulnar bone cavity (C). (B, C) For patients with bicondylar comminuted fracture, the approach and the attachment points of triceps can be reserved by using musculus triceps brachii: make the ulnar nerve exposed and move it forwards; excise the broken bone blocks (B) from inside first; then make the lateral epicondyle exposed and peel the whole soft tissues and remove the whole fractured pieces. Rotate the ulna so that ulna medullary cavity (C) can be exposed. (D) Make preparations of synostosis for Coonrad-Morrey typed semi-restricted prosthesis. Install osteotomy template through medullary space alignment positioning system; incise the trochlea humeri of appropriate size. (E) One should notice that the appropriate depth for insertion of prosthesis at ulna side should be that the center of the prosthesis at ulna side be consistent with that of olecranon meniscus incisura. (F) Implantation of Coonrad-Morrey prosthesis. Perform bone grafting at the back of anterior convex wing, and the prosthesis at the side of humerus should be close to the distal end enough so that it can be connected with the prosthesis at the side of ulna. Connect the joint prosthesis by adopting needle-by-needle locking system. After connecting the prosthesis at the side of humerus with the prosthesis at the side of ulna, throw the prosthesis at the side of humerus into the medullary space until its anterior convex wing repains to the top of coronoid process. (G-I) Anastomose and repair of muscle tendon of triceps: use a bone drill to drill crisscrossing and transverse bony tunnelat the distal ulna; use a No. 5 non-absorbable suture to go across the bone tunnel and muscle tendon (G); the suture crossed the muscle tendom and then return to the another bone tunnel (H); j is used for the second transerve suture: strengthen repair (I).
Raise the bolster for elbow on day when the operation is performed. Perform unloaded active and passive elbow activity after two to three days of the operation. Conduct functional exercise under the principle of controlled pain and extend the ROM (Range of motion) as much as possible. However, the ill limb can only lift object less than 5 kg for once, and object less than 1 kg for repeated motion [14]. The external fixation can be protectively used for two to three months. Four patients performed systematic training treatment under the guidance of rehabilitation physician and four patients performed functional exercise by themselves, instead of the rehabilitation due to economic factors.
Follow-up
Regular follow-up visit were performed after one, two, three and six months of the operation, as well as the intervals of six months afterwards, which included: evaluation on pain and the severity of elbow joint, examination on activity, stability of joint and elbow myodynamia, shoot of X-ray film to see the existence of heterotopic ossification, fracture, loosening and wearing of periprosthetic fracture and the conditions of knitting of anterior prosthesis, record on other complications, like wound infection, nonunion, nerve injury, etc., as well as Mayo Elbow Performance Score (MEPS) performed on patients at last follow-up visit, including pain (45), activity (20), stability (10) and function (25) of joint (the full mark is 100, wherein, the scores which are greater than 90 refer to “excellent”, 75~89 refers to “good”, 60~74 is within acceptable limit and scores which are less than 60 refer to “poor”.
Statistical analysis
The statistical software, SPSS 15.0 was employed for the management and analysis of the data.
Results
The average of time from being injured to operation was 5.5 days (3-9 days), and the average of operation time was 85 min. All patients were continuously followed up. Of these patients, one experienced wound infection after operation, for whom, the infection disappeared and the wound was cured after debridement & washing and the treatment of sensitive antibiotics. Two experienced ulnar nerve symptoms, both of whom got better after symptomatic treatment, and felt only sense abnormity 12 months after operation and one of whom totally recovered at the last follow-up. One had triceps brachii muscle level IV. Two had mild pain in elbow, which only happened at active movement but not at rest. The average of elbow flexion and extension range was 103.5±3.2 degrees (78-118), the average of flexion limitation was 28.5 degrees and that of extension limitation was 15.7 degrees. The average rotating range of forearm was 126.4±4.1 degrees (94-148). During follow-up, all elbow joints were stable; no prosthesis loosening, abrasion, or periprosthetic fracture was observed; and anterior grafted bone totally recovered (Figure 2). One patient was found with heterotopic ossification 6 months after operation, which did not progress after oral administration of indometacin, and then hardly influence the activity of elbow. At the last follow-up, the average of MEPS score was 85.2±3.4 (75-95). Four patients showed excellent and four good.
Figure 2.
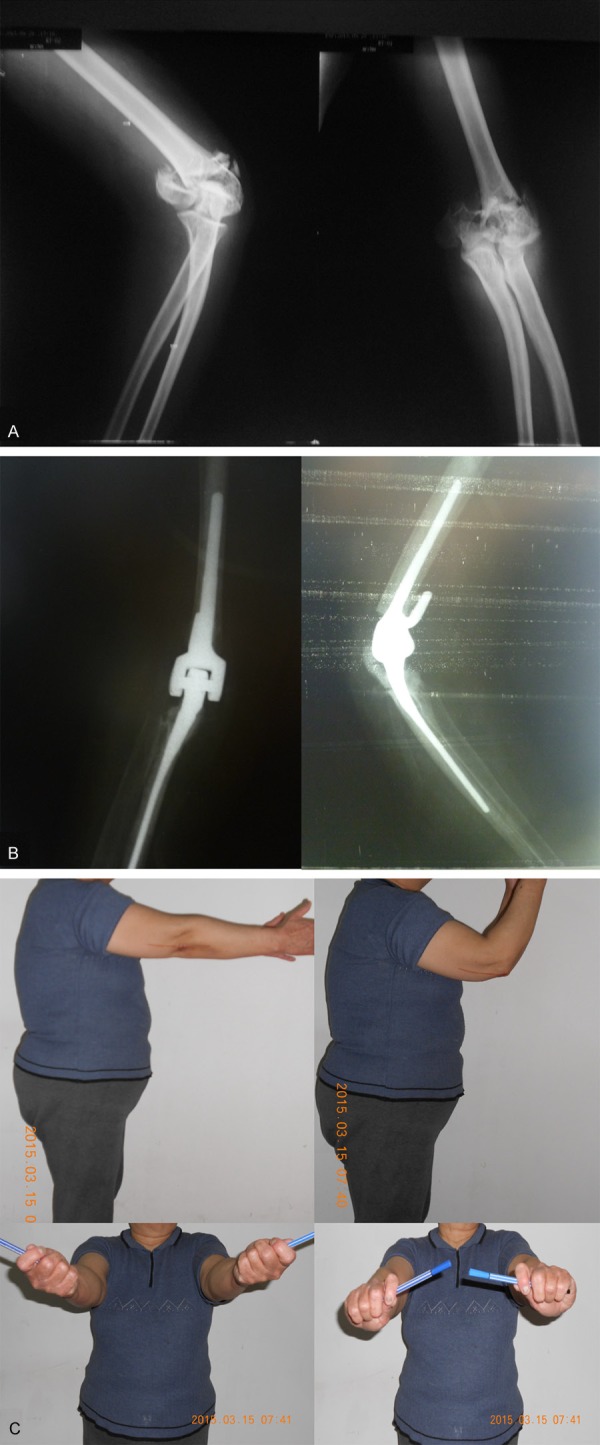
A. A 74 year-old female patient experiencing distal right humerus fracture of type C3 of AO due to falling. B. Coonrad-Morrey elbow joint prosthesis replacement was performed four days after being injured. C. The activity of affected elbow joint basically recovered to normal one year after operation.
Discussion
The distal humerus fracture can be treated with open reduction and internal fixation for most young patients [15-17]. In elderly patients, however, internal fixation usually fails to reach to the expected fixation strength, and the risk of non-healing obviously increases, due to the case that most patients are complicated with osteoporosis, and then complicated and comminuted fractures often occur, restoration is difficult and the dissection and reestablishment of joints cannot be ensured. In the past, researchers held the view that joint replacement can only be adopted as the remedial measure for obvious decrease of patients’ life quality [18,19]. Nevertheless, more and more scholars thought that one-stage elbow joint replacement for the treatment of intercondylar fracture of distal humerus in elderly patients can lead to more satisfied prognosis and superior elbow activity [6-13,20,21]. The advantages of this method include that: (1) The complicated technical problems of anatomical reduction and strong fixation for articular comminuted fracture are passed; technical difficulty of the operation is reduced; technical operation is simplified; operation time is shortened, so that hemorrhage during operation is reduced, the occurrence of complications like postoperative infection is reduced, and then prognosis is improved. (2) Instant stability of joint is achieved to guarantee early functional rehabilitation. Coonrad-Morrey prosthesis has seven degrees of interior and exterior loosening range, which can guarantee the stability of prosthesis even in the case of deficient medial and lateral malleolus so that rehabilitation exercise of elbow can be started immediately after operation and that delayed functional training for elbow caused by unstable fracture or invalid fixation for internal fixation are avoided, making joint functional rehabilitation obviously improved. (3) The complications caused by non-healing and joint cartilage injury after internal fixation operation, such as pain and severe traumatic arthritis, as well as the corresponding treatments (including second operation) are avoided, thus sorrow and economical burden can be reduced for patients.
The view above has been generally acknowledged overseas. There still exists dispute over it in China, though it tends to be admitted [6,22]. Baoguo Jiang et al. [6] believed that the indications of operation for one-staged elbow joint replacement include (1) Severe osteoporosis; (2) Severe comminuted fracture happens while the internal fixation fails to offer stable fixation; (3) Articular surface is badly damaged; (4) It is expected that the happening of traumatic arthritis is unavoidable. Basically, one or more of the above-mentioned points happen in elderly patients with fracture of type C. Several literatures on comparison of treatment outcome in the treatment of intercondylar fracture by steel plate and prosthesis came to arrive at the same conclusions - prosthesis possesses the advantages of shorter operation time, lower infection rate, superior curative effect, etc. [22-24]. Infection, poorer coverage of soft tissues and insufficient bending elbow myodynamia are the absolute contraindications, while primary degenerative osteoarthritis, higher requirements for elbow function and existence of hand dysfunction are relative contraindications, which must be strictly mastered by clinical physicians.
The most widely used prostheses so far are semi-restricted Coonrad-Morrey ones, the superiority of which lies in that the looseness of coronal plane has made its movement curve within the tolerated limit; it has duplicated kinesiology and biomechanical characteristics of normal elbow; it has reduced the stress between bone and cement interface and the wearing of joint; it can still guarantee the stability of joint on the condition that sclerotic is deficient or potential injury existing in ligament [14,25].
At present, Kamineni and Morrey [26] have held the associated study with the largest sample size and the longest follow-up. From 1982 to 2001, they had investigated forty-three patients with distal humerus fracture who had received total elbow replacement; the duration of follow-up had lasted for seven years. The average of MEPS score was 93 (75-100), and “excellent” accounted for 93%; the average of flexion and extension degree of elbow joint was 131 degrees; euphotic zone emerged in nine prostheses, but of which six always kept stable. In the report, the occurrence of postoperative complications was higher; eleven patients experienced infection, and three loosened prostheses and three periprosthetic fracture. In this group, the function of elbow was relatively lower than that reported above, the cause of which may be that, professional and systematic rehabilitation training can effectively extend the activity range of elbow joint, especially can obviously improve the extending function [27] compared with training by oneself. In this study, four patients refused rehabilitation due to personal reason, leading to poorer satisfaction to the curative effects. The occurrence of complications in this study, however, compared to that reported by Kamineni and Morrey, was relatively decreased. Thus, it is considered to be associated with the improvements in operation techniques and performances of prosthesis.
In this study, all the prostheses were stable after operation without loosening, obvious wearing or periprosthetic fracture. However, the sample size of this study was small and the duration of follow-up remained to be prolonged so as to gain the long-term conditions of prosthesis. Literature reported that, compared with fully restricted or non-restricted prosthesis, the occurrence of complications, like loosening, instability and fracture of prosthesis for Coonrad-Morrey semi-restricted prosthesis was decreased to a large extent. In this study, one patient who was complicated with diabetes suffered from wound infection after operation, and he went through a longer therapy (for six weeks), adhesive soft tissues at the back of elbow, partial cicatrization, and delayed joint activity. The curative effect was influenced seriously (MEPS score was 75). There were two ulnar neurological symptoms, of which one was considered to suffer from excessive pulling during operation and the other one showed horizontal heterotopic ossification in medial epicondyle of humerus by X-ray examination, which was considered to be caused by stimulating nerve due to hyper-osteogenic. One patient performed excessive exercise by oneself after operation, and he told that he felt sudden pain in the muscle at the back of his elbow; even though the pain disappeared through braking, the myodynamia of musculus triceps brachii was examined as level IV. It was considered as muscle laceration.
Summing up the experience through the treatment, the following key points should be noticed: (1) Inquire disease history carefully before operation and perform physical and imaging examinations; confirm whether there is contraindications for operation or disease history which may influence the effect after operation; strictly control the indications for operation. (2) On osteotomy during operation, the template should be tightly attained to outside of the caput humeral and the rear of distal humerus, to guarantee that the depth of osteotomy and rotating alignment are accurate. (3) Fully clean the broken bone blocks and bone residues after osteotomy, especially the lining range of interior ulnar nerve, to avoid damaging and stimulating nerve. (4) Fully press the anterior grafted bone of prosthesis at the side of humerus. (5) Antibacterial and absorbable suture is recommended for layer-by-layer strict suture and subcutaneous continuous suture is adopted for skin, since the old people are with poor skin union ability, and accurate folding is difficult as a result of loose skin, and that the soft tissues suffer from injuries with severity of different level due to fracture. (6) Perform rehabilitation training for postoperative system.
In conclusion, total elbow joint replacement can offer superior effects in the treatment of distal humerus fracture of type C in elderly patients. Meanwhile, it can be easily operated, take less operation time and have less complications. Since the sample size of this study is small and the duration of follow-up remains to be prolonged, the long-term efficacy needs to be observed further.
Disclosure of conflict of interest
None.
References
- 1.Court-Brown C, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Robinson CM, Hill RM, Jacobs N, Dall G, Court-Brown CM. Adult distal humeral metaphyseal fractures: epidemiology and results of treatment. J Orthop Trauma. 2003;17:38–47. doi: 10.1097/00005131-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Desimone LJ, Sanchez-Sotelo J. Total elbow arthroplasty for distal humerus fractures. Orthop Clin North Am. 2013;44:381–387. doi: 10.1016/j.ocl.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 4.Charissoux JL, Mabit C, Fourastier J, Beccari R, Emily S, Cappelli M, Malingue E, Mansat P, Hubert L, Proust J, Bratu D, Veillard D, Grandmaison FL, Apard T, Martinel V, Bonnevialle N. Complex intra-articular fractures of the distal humerus in elderly patients. Rev Chir Orthop. 2008;94:536–562. doi: 10.1016/j.rco.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 5.Diederichs G, Issever AS, Greiner S, Linke B, Korner J. Three-dimensional distribution of trabecular bone density and cortical thickness in the distal humerus. J Shoulder Elbow Surg. 2009;18:399–407. doi: 10.1016/j.jse.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Jiang BG, Chen JH, Zhang PX, Zhang DY, Fu ZG. Clinical outcomes of total elbow replacement in the treatment of complex distal humeral fractures. Zhonghua Wai Ke Za Zhi. 2010;48:213–216. [PubMed] [Google Scholar]
- 7.Kaźmierczak M, Pyszel KS, Surdziel PH. Total elbow arthroplasty in complicated distal humerus fracture-a case report. Pol Orthop Traumatol. 2013;78:91–96. [PubMed] [Google Scholar]
- 8.Argintar E, Berry M, Narvy SJ, Kramer J, Omid R, Itamura JM. Hemiarthroplasty for the treatment of distal humerus fractures: short-term clinical results. Orthopedics. 2012;35:1042–1045. doi: 10.3928/01477447-20121120-06. [DOI] [PubMed] [Google Scholar]
- 9.Antuña SA, Laakso RB, Barrera JL, Espiga X, Ferreres A. Linked total elbow arthroplasty as treatment of distal humerus fractures. Acta Orthop Belg. 2012;78:465–472. [PubMed] [Google Scholar]
- 10.Choo A, Ramsey ML. Total elbow arthroplasty: current options. J Am Acad Orthop Surg. 2013;21:427–437. doi: 10.5435/JAAOS-21-07-427. [DOI] [PubMed] [Google Scholar]
- 11.Ducrot G, Ehlinger M, Adam P, Di Marco A, Clavert P, Bonnomet F. Complex fractures of the distal humerus in the elderly: is primary total elbow arthroplasty a valid treatment alternative? A series of 20 cases. Orthop Traumatol Surg Res. 2013;99:10–20. doi: 10.1016/j.otsr.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Adolfsson L, Hammer R. Elbow hemiarthroplasty for acute reconstruction of intraarticular distal humerus fractures. A preliminary report involving 4 patients. Acta Orthop. 2006;77:785–787. doi: 10.1080/17453670610012999. [DOI] [PubMed] [Google Scholar]
- 13.Burkhart KJ, Nijs S, Mattyasovszky SG, Wouters R, Gruszka D, Nowak TE, Rommens PM, Müller LP. Distal humerus hemiarthroplasty of the elbow for comminuted distal humeral fractures in the elderly patient. J Trauma. 2011;71:635–642. doi: 10.1097/TA.0b013e318216936e. [DOI] [PubMed] [Google Scholar]
- 14.Jiang XY, Gong MQ, Liu XH, He L, Zhang LD, Wang MY, Rong GW, Zhang H. Semi-constrained total elbow arthroplasty for the treatment of the elbow disorders. Zhonghua Wai Ke Za Zhi. 2009;47:884–887. [PubMed] [Google Scholar]
- 15.Greiner S, Haas NP, Bail HJ. Outcome after open reduction and angular stable internal fixation for supra-intercondylar fractures of the distal humerus: preliminary results with the LCP Distal Humerus System. Arch Orthop Trauma Surg. 2008;128:723–729. doi: 10.1007/s00402-007-0428-2. [DOI] [PubMed] [Google Scholar]
- 16.Kaiser T, Brunner A, Hohendorff B, Ulmar B, Babst R. Treatment of supra and intra-articular fractures of the distal humerus with LCP Distal Humerus Plate. A 2-year follow-up. J Shoulder Elbow Surg. 2011;20:206–212. doi: 10.1016/j.jse.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 17.Proust J, Oksman A, Charissoux JL, Mabit C, Arnaud JP. Results of internal fixation for intra-articular distal humerus fractures in elderly patients. Rev Chir Orthop. 2007;93:798–806. doi: 10.1016/s0035-1040(07)78463-5. [DOI] [PubMed] [Google Scholar]
- 18.Prasad N, Dent C. Outcome of total elbow replacement for distal humeral fractures in the elderly. A comparison of primary surgery and surgery after failed internal fixation or conservative treatment. J Bone Joint Surg Br. 2008;90:343–348. doi: 10.1302/0301-620X.90B3.18971. [DOI] [PubMed] [Google Scholar]
- 19.Augereau B, Mansat P. Total elbow replacement implants. Rev Chir Orthop. 2005;91:31–96. [Google Scholar]
- 20.Frankle M, Virani N, Fischer D, et al. Immediate total elbow arthroplasty for distal humerus fracture. Tech Orthop. 2006;21:363–373. [Google Scholar]
- 21.Chalidis B, Dimitriou C, Papadopoulos P, Petsatodis G, Giannoudis PV. Total elbow arthroplasty for the treatment of insufficient distal humeral fractures. A retrospective clinical study and review of the literature. Injury. 2009;40:582–590. doi: 10.1016/j.injury.2009.01.123. [DOI] [PubMed] [Google Scholar]
- 22.Jiang XY. Treatment progress of fractures and dislocation of elbow joint. Zhongguo Gu Shang. 2010;23:645–647. [PubMed] [Google Scholar]
- 23.Sanchez-Sotelo J. Distal humeral fractures: role of internal fixation and elbow arthroplasty. J Bone Joint Surg Am. 2012;94:555–568. doi: 10.2106/JBJS.946icl. [DOI] [PubMed] [Google Scholar]
- 24.McKee MD, Veillette CJ, Hall JA, Schemitsch EH, Wild LM, McCormack R, Perey B, Goetz T, Zomar M, Moon K, Mandel S, Petit S, Guy P, Leung I. A multicenter, prospective, randomized, controlled trial of open reduction-internal fixation versus total elbow arthroplasty for displaced intra-articular distal humeral fractures in elderly patients. J Shoulder Elbow Surg. 2009;18:3–12. doi: 10.1016/j.jse.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 25.Maheshwari R, Vaziri S, Helm RH. Total elbow replacement with the Coonrad-Morrey prosthesis: our medium to long-term results. Ann R Coll Surg Engl. 2012;94:189–192. doi: 10.1308/003588412X13171221589775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamineni S, Morrey BF. Distal humeral fractures treated with non-custom total elbow replacement. J Bone Joint Surg Am. 2004;86:940–947. doi: 10.2106/00004623-200405000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Barlow JD, Morrey BF, O’Driscoll SW, Steinmann SP, Sanchez-Sotelo J. Activities after total elbow arthroplasty. J Shoulder Elbow Surg. 2013;22:787–791. doi: 10.1016/j.jse.2013.01.023. [DOI] [PubMed] [Google Scholar]


