Abstract
Background: Chronic low back and lower extremity pain is mainly caused by lumbar disc herniation (LDH) and radiculitis. Various surgery and nonsurgical modalities, including epidural injections, have been used to treat LDH or radiculitis. Therefore, we conducted this meta-analysis to assess the effects of the two interventions in managing various chronic low and lower extremity pain. Methods: A systematic literature search was conducted to identify randomized controlled trials (RCTs) which compared the effect of local anesthetic with or without steroids. The outcomes included pain relief, functional improvement, opioid intake, and therapeutic procedural characteristics. Pooled estimates were calculated using a random-effects or fixed-effects model, depending on the heterogeneity between the included studies. Results: 10 RCTs (involving 1111 patients) were included in this meta-analysis. The pooled results showed that 41.7% of patients who received local anesthetic with steroid (group 1) and 40.2% of patients who received local anesthetic alone (group 2) had significant improvement in pain relief. And the Numeric Rating Scale pain scales were significantly reduced by 4.09 scores (95% CI: -4.26, -3.91), and 4.12 (95% CI: -4.35, -3.89) scores, respectively. Similarly, 39.8% of patients in group 1 and 40.7% of patients in group 2 achieved significantly improved functional status. The Oswestry Disability Index in the two groups were reduced by 14.5 (95% CI: -15.24, -13.75) and 12.37 (95% CI: -16.13, -8.62), respectively. The average procedures per year in group 1 was 3.68 ± 1.17 and 3.68 ± 1.26 in group 2 with an average total relief per year of 31.67 ± 13.17 weeks and 32.64 ± 13.92 weeks, respectively. The opioid intake decreased from baseline by 8.81 mg (95% CI: -12.24, -5.38) and 16.92 mg (95% CI: -22.71, -11.12) in the two groups, respectively. Conclusion: This meta-analysis confirms that epidural injections of local anesthetic with or without steroids have beneficial but similar effects in the treatment of patients with chronic low back and lower extremity pain.
Keywords: Chronic low back pain, lower extremity pain, epidural injections, local anesthetic, steroids, meta-analysis
Introduction
Lumbar disc herniation (LDH), which is the main cause for radicular pain, was first reported by Mixter and Barr [1] in 1934. Since then, amounts of literature has been published to descript the epidemiology, diagnosis, pathophysiology and treatment for herniated disc pain [2-4]. According to some estimates, the prevalence of lumbar radiculopathy or sciatica approaches 9.8 per 1,000 cases [4], of which 5.1% in men and 3.7% in women [3]. Even though, the symptoms in 23% to 48% of patients would resolve spontaneously, and 5% to 15% of patients still need surgical treatment, which would lead to heavy economic burden and strain on health services [5-7]. Various conservative, surgical or nonsurgical modalities have used in the treatment of LDH or radicular pain [8-12]. However, surgery is not available for everyone who is symptomatic, and it may lead to failure in approximately 25% of patients in well-selected cases [13]. In contrast, epidural injections are one of the most commonly performed nonsurgical treatments for LDH [9-11].
Epidural injection administration routes include transforaminal, interlaminar, and caudal approaches [14-16]. Among the three approaches available to access the lumbar epidural space, the transforaminal approach requires the smallest volume to reach the primary site of pathology, and the interlaminar approach is the most commonly used [2,14,17]. However, the effectiveness of the three approaches in managing low back and lower extremity pain remains controversial in the previously published studies. In a recent systematic review conducted by Manchikanti L, et al [18], the authors assessed the short- and long-term efficacy of epidural injections in the treatment of LDH. They found that transforaminal epidural injections did not result in superior efficacy than caudal or interlaminar approaches [18]. In contrast, in several other systematic reviews that compared the efficacy of three approaches obtained controversial results, in which transforaminal and caudal epidural injections were more effective than interlaminar epidural injections [2,14,17,19,20]. However, several flaws have been found in these systematic reviews, including variable study designs, different baseline characteristics between treatment groups, small sample size, duration of follow-up, inappropriate methodology, and improper study evaluation [2,17,21].
In addition, the underlying mechanism of epidurally administered local anesthetic and steroid injections in the treatment of chronic low back pain still remains unknown [2,14,17,19,20,22-27]. According to the current evidence, there is a trend suggesting that local anesthetics might have comparable effectiveness as steroids in the treatment of low back pain without LDH and also pain of facet joint origin [28-39]. Moreover, the animal experiment also showed that, the nerve root infiltration could prevent mechanical allodynia in rats with local anesthetic with or without steroids, which indicates that corticosteroids may not be necessary for the nerve root blocks [29].
With regard to the effectiveness of local anesthetic with or without steroids, there is no meta-analysis that has been conducted to compare their effectiveness in the management of low back and lower extremity pain. And whether the local anesthetic with steroids would provide better effect than anesthetic alone remains unknown. Under this consideration, we performed this meta-analysis only based on randomized controlled trials (RCTs) to compare the efficacy of local anesthetic with steroids with anesthetic alone in the management of low back and lower extremity pain.
Material and methods
Literature search
We conducted this meta-analysis in keeping with the preferred reported items for systematic reviews and meta-analyses guidelines [40]. A comprehensive search was performed to identify eligible studies, which assessed the efficacy of epidural injection of local anesthetic with steroids in managing chronic pain of disc herniation or radiculitis. Database, including Pubmed, Embase, Web Of Science, were searched up to October 21, 2014, using (“lumbosacral region” [MeSH Terms] OR (“lumbosacral” [All Fields] AND “region” [All Fields]) OR “lumbosacral region” [All Fields] OR “lumbar” [All Fields]) AND Disc [All Fields] AND (“hernia” [MeSH Terms] OR “hernia” [All Fields] OR “herniation” [All Fields]) AND (“anesthetics” [Pharmacological Action] OR “anesthetics” [MeSH Terms] OR “anesthetics” [All Fields] OR “anesthetic” [All Fields]) AND (“steroids” [MeSH Terms] OR “steroids” [All Fields]). No language restrictions was imposed in the search strategy. We also manually searched the reference lists of published articles and reviews to identify other potential relevant studies.
Study inclusion and exclusion criteria
Studies were included in this meta-analysis if they (1) were RCTs; (2) assessed the efficacy of epidural injection of local anesthetic with or without steroids in managing chronic pain of disc herniation or radiculitis; (3) presented the effect size and its 95% confidence intervals (CIs). In contrast, those studies were excluded if they were not randomized controlled design, or did not assign patients to receive the epidural injection of local anesthetic with or without steroids, or did not provide available studies of interest. We also excluded reviews, letters, comments, and case reports.
Review strategy
Endnote bibliographic software was used to create an electronic library of citations identified in the literature searches. Database, including Pubmed, Embase and Web Of Science, were searched by using of Endnote. After the duplicate records were deleted, two independent investigators (Jinshuai Zhai and Long Zhang) were trained to perform the abstract review and thereafter full text review. Disagreements between two investigators were resolved through consensus and discussion. Two investigators (Xicheng Li and Zhi Tian) independently extracted the following information using a standardized data extraction form: the first author, patients’ age, sample size, baseline characteristics, the number of patients with significant pain relief (50%) or improvement in functional status in each group, the overall average procedures per year in each group, total relief per year in each group, opioid intake characteristics.
Quality assessment
We assessed the methodological quality of included studies by using the validated Jadad 5 point scale. The scale consists of three items describing randomization (0-2 points), blinding (0-2 points), and dropouts and withdrawals (0-1 point) in the report of randomized controlled trial [41]. A score of one is given for each of the points described. A further point is obtained where the method of randomization and/or blinding is given and is appropriate. The quality scale ranges from 0 to 5 points. Higher scores indicate better reporting. Articles with ≥3 score are said to be of high quality [42].
Statistical analysis
Dichotomous variables (pain relief, functional improvement), were expressed as risk ratio (RR) with 95% CIs, and dichotomous outcomes (average procedure per year, total relief per year, opioid intake) were expressed as weighted mean differences (WMDs) with 95% CIs. Heterogeneity between the studies was tested by using I 2 statistic, in which, an I 2 value more than 50% was considered as significant heterogeneity [43]. The pooled estimates were calculated using a fixed-effects model (Mantel-Haenszel method) [44] or random-effects mo-del (DerSimonian-Laird method) [45], according to the heterogeneity among the studies. The presence of publication bias was evaluated by using the Begg and Egger tests [46,47]. A P value less than 0.05 was considered as statistically significant. All statistical analyses were conducted by using of STATA software version 12.0 (Stata Corporation, College Station, TX, USA).
Results
Literature search
The flow chart of search strategy is shown in Figure 1. Initially, a total of 654 publications were identified from Pubmed, Embase, and Web Of Science, of which 276 were excluded because of duplicate records. Then though various means, we obtained all the full text. After reviewing the title/abstract and full texts, 312 and 56 studies were excluded respectively, because the data they provided were not available (reviews, letters, case reports, non-randomized controlled trials). Consequently, the remaining 10 studies involving 1111 patients met the inclusion criteria and were included in this meta-analysis [48-57].
Figure 1.
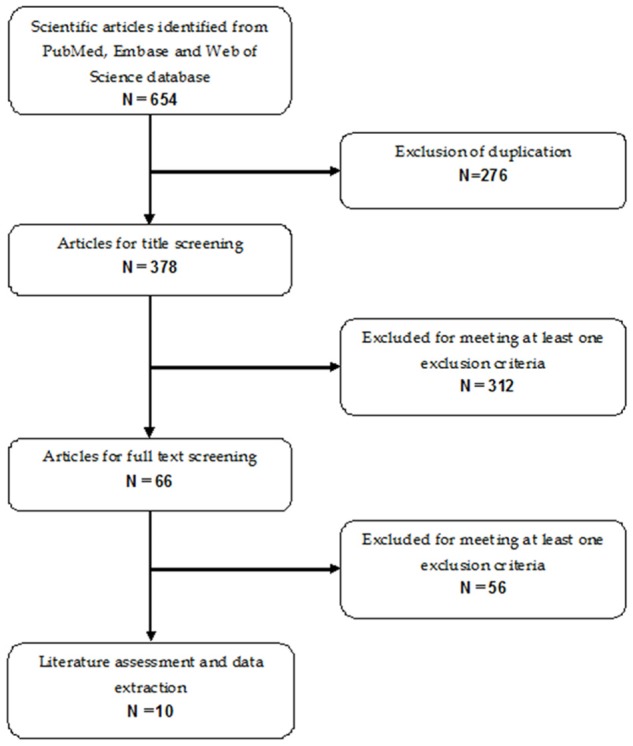
Eligibility of studies for inclusion in systematic review.
Characteristics, quality of eligible studies
The main characteristics of the 10 RCTs included in this meta-analysis are described in Table 1. Of them, nine were carried out in USA [48-54,56,57], and the remaining one was carried out in Greece [55]. The sample size of those 10 RCTs ranged from 58 to 183. All the studies were well-conducted prospectively RCTs. Four studies [50,51,53,54] included in this meta-analysis used interlaminar route to administer local anesthetic or steroids, another four studies using caudal route [52,55-57], one using transforaminal route [48], and the remaining one did not report the administration route [49]. The majority of studies used Numeric Rating Scale (NRS) to assess the pain rating scores and Oswestry Disability Index (ODI) to measure functional ability. A 50% or more improvement in pain relief and functional status was considered significant. There were no significantly differences in the demographic characteristics between the two groups (age of patients, male/female ratio, duration of pain, initial NRS and ODI) in majority of the included studies except in four studies [50-52,57], in which patients in the local anesthetic group had higher weight or larger proportion of gradual onset than those in the local anesthetic with steroids group. The average Jadad score of included studies was 4.
Table 1.
Baseline characteristics of patients in the trials included in the meta-analysis
| Study | Treatment regimen | Sample size | Age (mean ± SD, years) | Duration of pain (months) | Epidural approach | Jadad score |
|---|---|---|---|---|---|---|
| Manchikanti L [48] | 1% lidocaine + 0.5 ml betamethasone | 60 | 42.6 ± 11.2 | 103.8 ± 92.5 | transforaminal | 4 |
| 1.5 ml 1% lidocaine + 0.5 ml sodium chloride solution | 60 | 43.1 ± 11.8 | 98.4 ± 83.4 | |||
| Cohen SP [49] | Steroids + bupivacaine | 28 | 42.46 ± 12.65 | 2.61 ± 1.82 | Not report | 4 |
| Saline + bupivacaine | 30 | 42.27 ± 10.73 | 2.82 ± 1.7 | |||
| Manchikanti L [50] | Local anesthetic + non-particulate betamethasone | 35 | 42.4 ± 10.0 | 111.1 ± 79.8 | Interlaminar | 4 |
| Local anesthetic only | 35 | 41.5 ± 13.4 | 131.3 ± 102.7 | |||
| Manchikanti L [51] | Local anesthetic + non-particulate betamethasone | 30 | 53.9 ± 11.4 | 138.1 ± 89.4 | Interlaminar | 4 |
| Local anesthetic only | 30 | 49.8 ± 14.7 | 121.0 ± 81.5 | |||
| Manchikanti L [52] | 9 ml, 0.5% idocaine + 1 ml steroid | 60 | 43 ± 14.5 | 81.3 ± 81.7 | Caudal | 4 |
| 10 ml local anesthetic + 0.5% idocaine | 60 | 38.7 ± 14.1 | 93.4 ± 86.9 | |||
| Manchikanti L [53] | Local anesthetic + steroids | 60 | 41.2 ± 11.9 | 104.2 ± 106.5 | Interlaminar | 4 |
| Local anesthetic alone | 60 | 42.7 ± 11.4 | 129 ± 90.9 | |||
| Manchikanti L [54] | 5 ml, 0.5% idocaine + 1 ml non-particulate betamethasone | 60 | 40.6 ± 12.5 | 133.2 ± 108.5 | Interlaminar | 4 |
| 6 ml, 0.5% idocaine | 60 | 49 ± 14.1 | 135 ± 120.3 | |||
| Sayegh FE [55] | 12 ml, 2% xylocaine + 1 ml betamethasone | 93 | 50.75 ± 15.52 | 53.1 ± 33.5 | Caudal | 4 |
| 12 ml, 2% xylocaine + 8 ml water for injection | 90 | 47.56 ± 16.42 | 51.4 ± 30.4 | |||
| Manchikanti L [56] | 1 ml steroid + 9 ml, 0.5% idocaine | 60 | 43 ± 14.5 | 81.3 ± 81.7 | Caudal | 4 |
| local anesthetic + 10 ml, 0.5% idocaine | 60 | 48.7 ± 14.1 | 93.4 ± 86.9 | |||
| Manchikanti L [57] | 9 ml, 0.5% idocaine + 1 ml non-particulate betamethasone | 70 | 48 ± 12.3 | 160.7 ± 113.3 | Caudal | 4 |
| 10 ml 0.5% idocaine | 70 | 52.4 ± 141. | 152.1 ± 106.9 |
Pain relief
Nine studies provided the data of pain relief [48-54,56,57]. The pooled estimates indicated that patients in the local anesthetic with steroids group had a 41.7% improvement in pain relief, and patients in the local anesthetic group had a 40.2% improvement in pain relief. However, there was no significant differences between the two groups (RR = 0.93, 95% CI: 0.85, 1.01; P = 0.076) (Figure 2).
Figure 2.
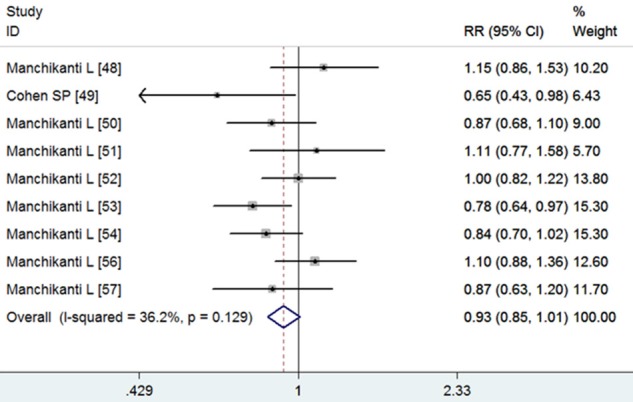
Comparison of pain relief improvement between local anesthetic with or without steroids for patientswith low back and lower extremity pain.
Data of NRS pain scores were available from eight studies [48,50-54,56,57]. The aggregated results suggest that, local anesthetic with steroids was associated with 4.09 scores reduction (WMD = -4.09, 95% CI: -4.26, -3.91; P = 0.000), and local anesthetic alone was associated with 4.12 scores reduction (WMD = -4.12, 95% CI: -4.35, -3.89; P = 0.000). However, no significant difference was observed in the NRS pain scores between the two groups (WMD = 0.20, 95% CI: -0.10, 0.50; P = 0.197) (Figure 3).
Figure 3.
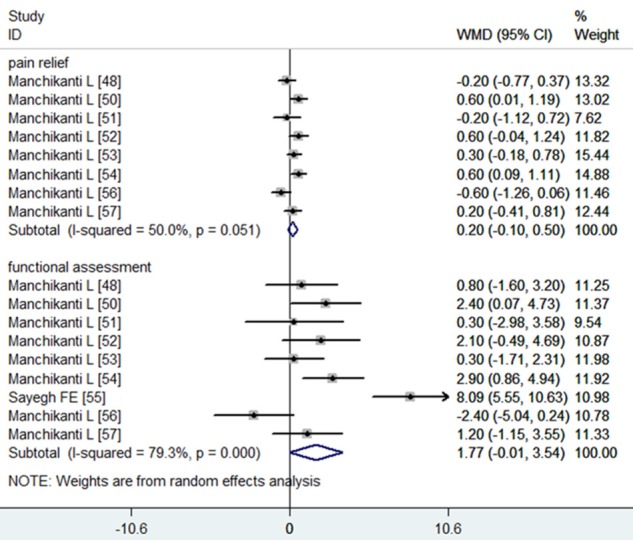
Comparison of NRS pain scores and ODI between local anesthetic with or without steroids for patients with low back and lower extremity pain.
Functional assessment
Eight studies reported the data of functional assessment [48,50-54,56,57]. Significant reduction was observed by 39.8% in the local anesthetic with steroids group and 40.7% in the local anesthetic group. However, no significant difference was found between the two groups (RR = 0.98, 95% CI: 0.86, 1.11; P = 0.729) (Figure 4).
Figure 4.
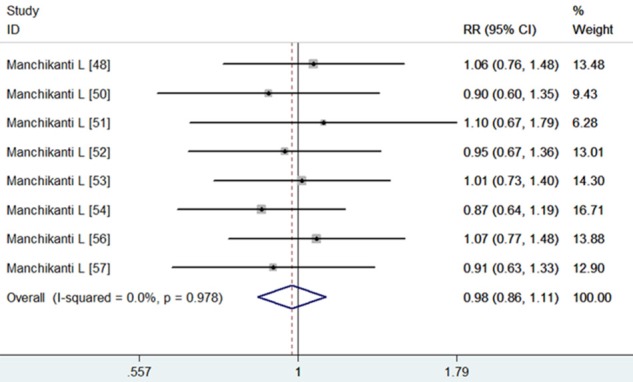
Comparison of functional improvement between local anesthetic with or without steroids for patients with low back and lower extremity pain.
Data of ODI were available from eight studies [48,50-54,56,57]. The aggregated results suggest that, local anesthetic with steroids was associated with a 14.50 reduction (WMD = -14.5, 95% CI: -15.24, -13.75; P = 0.000), and local anesthetic alone was associated with a 12.37 reduction (WMD = -12.37, 95% CI: -16.13, -8.62; P = 0.000). However, there was no significant differences in the ODI between the two groups (WMD = 1.77, 95% CI: -0.01, 3.54; P = 0.051) (Figure 3).
Opioid intake
Seven studies presented the data of opioid intake [48,50-54,56]. Significant reduction from baseline was observed by 8.81 mg (95% CI: -12.24, -5.38) in the local anesthetic with steroids group and 16.92 mg (95% CI: -22.71, -11.12) in the local anesthetic group. However, no significant difference was found between the two groups (WMD = -3.03, 95% CI: -6.55, 0.48; P = 0.091) (Figure 5).
Figure 5.
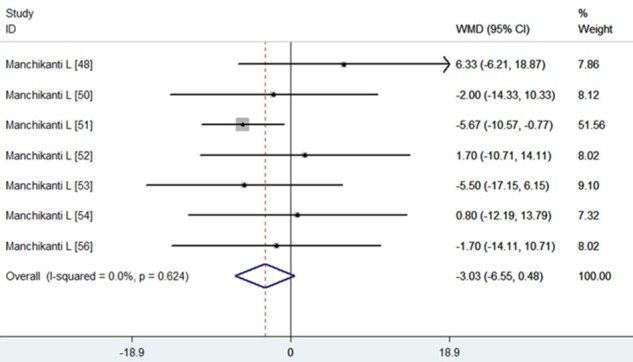
Comparison of opioid intake reduction between local anesthetic with or without steroids for patients with low back and lower extremity pain.
Therapeutic procedural characteristics
Six studies showed the data of procedures frequency [48,51-54,56]. The average procedures per year in the local anesthetic with or without steroids groups were 3.68 ± 1.17 and 3.68 ± 1.26, respectively. Pooled estimates using a fixed-model indicated that there was no significant difference in procedures frequency between the two groups (WMD = -0.03, 95% CI: -0.21, 0.16; P = 0.759) (Figure 6).
Figure 6.
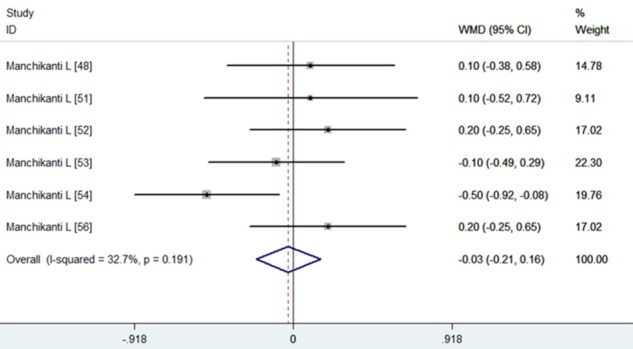
Comparison of procedures frequency between local anesthetic with or without steroids for patients with low back and lower extremity pain.
Seven studies provided the data of average total relief [48,50-54,56]. The average total relief in the local anesthetic with or without steroids groups were 31.67 ± 13.17 weeks and 32.64 ± 13.92 weeks, respectively. Pooled estimates using a fixed-model suggest that there was no significant difference in average total relief between the two groups (WMD = 0.27, 95% CI: -0.60, 1.14; P = 0.540) (Figure 7).
Figure 7.
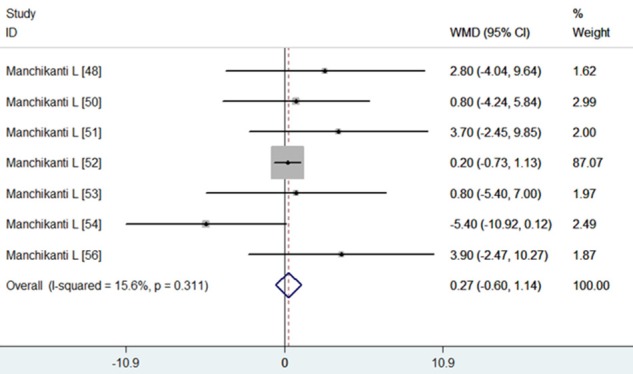
Comparison of average total relief between local anesthetic with or without steroids for patients with low back and lower extremity pain.
Publication bias
We performed the Begg’s and Egger’s test to assess the publication bias. However, no evidence of potential publication bias was found according to the Begg’s and Egger’s test (Egger’s test, P = 0.917; Begg’s test, P = 0.789) (Figure 8).
Figure 8.
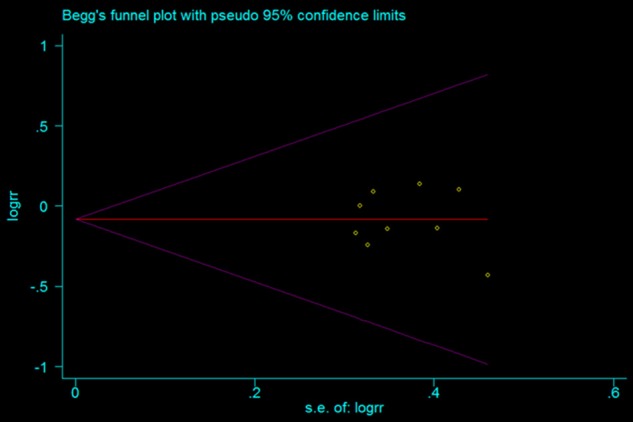
Test for publication bias for RR of pain relief improvement in patients with low back and lower extremity pain.
Discussion
This meta-analysis based on ten randomized, active control trials of patients treated with either local anesthetic with steroids or local anesthetic alone showed significant improvement in all outcomes in both groups. Our study indicated that 41.7% of patients who administered local anesthetic with steroids and 40.2% of patients who administered local anesthetic alone obtained significant improvement in pain relief. And 39.8% of patients in the local anesthetic with steroids group and 40.7% of patients in the local anesthetic group achieved improved functional status. Average total relief per year was 31.67 ± 13.17 weeks with 3.68 ± 1.17 procedures in local anesthetic with steroids group, and 32.64 ± 13.92 weeks with 3.68 ± 1.26 procedures in the local anesthetic alone group. These results demonstrated that both treatments were effective but that local anesthetic with steroids did not bring superior effect than local anesthetic alone.
The mechanisms that anesthetic and steroids have significant improvement in pain relief and functional status are not entirely known [24,27,58]. However, there are evidences suggesting that noxious peripheral stimulation, excess nociception, excess release of neurotransmitters, are involved in the pathogenesis of chronic pain [14,59]. Moreover, an increasing body of evidence suggests that both anesthetic and steroids had significant effects on the modulation of noxious stimulation by various mechanisms [28,60,61], but no significant difference in the treatment of facet joint-caused low back pain without disc herniation [62-64]. Therefore, based on the evidence above, we conclude that patients would achieve long-term relief from radicular pain when they were treated with local anesthetics with or without steroids.
Several studies or systematic reviews have been conducted in assessing the effects of epidural injections. However, their results remained debate. In a systematic review conducted by Conn et al [17], the authors evaluated the effect of caudal epidural injections with or without steroids in the management of chronic low back pain. However, only two studies with a follow up of more than six months and the use of fluoroscopy met the inclusion criteria and were included in that study [36,65]. One trial that showed positive results [66], was excluded in that systematic review because its follow up was only 24 weeks. Based on very small number of the studies included, the authors concluded that patients who were administered with caudal epidural injection with or without steroids achieved long-term relief in managing chronic low back.
In another study conducted by Iversen et al [67], the authors carried out the epidural injection under ultrasound without fluoroscopy, however, they found negative results. In that study, caudal epidural steroid or saline injection was gave to the patients with chronic lumbar radiculopathy. After the 52 week follow-up, the authors detected that no significant differences was found between the steroid and saline groups. However, this study has been criticized for its study design performance, patient enrollment, lack of fluoroscopy, and interpretation of results [68,69]. In an editorial accompanying Iversen et al [67], Cohen [70] argued that overall epidural steroid injections seem to be beneficial, but only provide modest improvement in carefully selected patients with predominantly radicular symptoms. Cohen [70] explained the failure of caudal epidural steroid injection in Iversen’ study with four potential reasons: (1) the targeting areas were far removed from the site of caudal steroids injection; (2) the effect of caudal epidural steroid injection was negated by the combination of low dose of steroid (40 mg triamcinolone) used and high volume (30 ml), which diluted the concentration of steroid bathing the nerve roots; (3) the local anaesthetic was not used to break the cycle of pain, and thus reverse the processes of central sensitization; (4) patients were not randomly assigned, in which the sham group experienced a shorter duration of pain. Patients with shorter duration of symptoms were more likely to achieve better effect than those with longer duration [71,72]. Therefore, Cohen believed that Iversen and colleagues’ study was probably underpowered. Despite these negative findings, Cohen suggested that we should not misinterpret Iversen’s study as suggesting that epidural steroid injections have no benefits in neuropathic back pain [70].
In this meta-analysis, we only included randomized active control trials to calculate the effect estimates. And we found that the majority of these included studies have been criticized for a lack of placebo group. However, it is not achievable to use placebo-controlled neural blockade as intervention in the clinical practice [73-75]. There are some arguments that a local anesthetic injection should be considered as a placebo because it reveals similar effects as the later one. However, this argument also seems inaccurate because injections of sodium chloride solution, dextrose, and local anesthetics into multiple structures have been found to produce different active outcomes in the published studies [76-78].
Our study has several strengths. First, this meta-analysis was conducted on prospectively randomized, blind, active control trials, and all of them were well-performed, high quality. The prospective trial design would minimize the recall and selection bias that always occurred in the retrospective studies. Second, most of the included ten studies have enlarged sample size, which could reduce the possibility of overestimating the treatment effect as compared with smaller samples. In addition, the enlarged sample size would enhance our statistical power to detect the effects of local anesthetic with or without steroids.
However, some limitations involved in this meta-analysis should be taken into account when interpreting our results. First, uncontrolled confounding inherited from original studies might influence the effect estimate. Although most of the included studies had comparable demographic characteristics between the two groups, unbalanced proportion of gender, weight, mode of gradual onset, and initial NRS were found in some studies [50-52,57]. Gender and weight is probably not associated with the response. However, patients with gradual onset may have an inferior response than those with onset following an injury. Moreover, higher initial NRS in the local anesthetic with steroids group would have an impact on the decreases of pain scores in the local anesthetic alone group. Therefore, we could not exclude the possibility that the uncontrolled confounding factors may bias our findings. Second, there was considerable heterogeneity among the included studies. This heterogeneity could be explained to the variation in baseline characteristics, epidural injection routes, duration of follow-up, and study design between the studies. Further, the previous studies indicated that different epidural injection routes would result in different outcomes. These factors may exaggerate or obscure the final treatment effects. Third, because of the limited number of included studies, we did not compare the effects of local anesthetic between the three epidural injection routes.
In conclusion, our meta-analysis showed effective but comparable outcomes in pain relief, functional improvement, opioid intake, average procedures per year, and average total relief between patients receiving local anesthetic with steroids and those receiving local anesthetic alone. On the basis of these findings, there is currently a lack of evidence to support that local anesthetic with steroids is superior to local anesthetic alone in managing chronic low back and lower extremity pain.
Disclosure of conflict of interest
None.
References
- 1.Barr JS, Mixter WJ. Rupture of the intervertebral disc with involvement of the spinal canal. N Eng J Med. 1934;211:201–215. [Google Scholar]
- 2.Manchikanti L, Boswell MV, Singh V, Benyamin RM, Fellows B, Abdi S, Buenaventura RM, Conn A, Datta S, Derby R, Falco FJ, Erhart S, Diwan S, Hayek SM, Helm S, Parr AT, Schultz DM, Smith HS, Wolfer LR, Hirsch JA ASIPP-IPM. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009;12:699–802. [PubMed] [Google Scholar]
- 3.Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine (Phila Pa 1976) 2008;33:2464–72. doi: 10.1097/BRS.0b013e318183a4a2. [DOI] [PubMed] [Google Scholar]
- 4.Savettieri G, Salemi G, Rocca WA, Meneghini F, D’Arpa A, Morgante L, Coraci MA, Reggio A, Grigoletto F, Di Perri R. Prevalence of lumbosacral radiculopathy in two Sicilian municipalities. Sicilian Neuro-Epidemiologic Study (SNES) Group. Acta Neurol Scand. 1996;93:464–9. doi: 10.1111/j.1600-0404.1996.tb00027.x. [DOI] [PubMed] [Google Scholar]
- 5.Hoy D, Brooks P, Blyth F, Buchbinder R. The Epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24:769–81. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Tosteson AN, Tosteson TD, Lurie JD, Abdu W, Herkowitz H, Andersson G, Albert T, Bridwell K, Zhao W, Grove MR, Weinstein MC, Weinstein JN. Comparative effectiveness evidence from the spine patient outcomes research trial: surgical versus nonoperative care for spinal stenosis, degenerative spondylolisthesis, and intervertebral disc herniation. Spine (Phila Pa 1976) 2011;36:2061–8. doi: 10.1097/BRS.0b013e318235457b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R, Verhagen A, Koes B, Peul WC. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J. 2011;20:513–22. doi: 10.1007/s00586-010-1603-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rubinstein SM, van Middelkoop M, Assendelft WJ, de Boer MR, van Tulder MW. Spinal manipulative therapy for chronic low-back pain: an update of a Cochrane review. Spine (Phila Pa 1976) 2011;36:E825–46. doi: 10.1097/BRS.0b013e3182197fe1. [DOI] [PubMed] [Google Scholar]
- 9.Manchikanti L, Helm Ii S, Singh V, Hirsch JA. Accountable interventional pain management: a collaboration among practitioners, patients, payers, and government. Pain Physician. 2013;16:E635–70. [PubMed] [Google Scholar]
- 10.Manchikanti L, Pampati V, Falco FJ, Hirsch JA. Assessment of the growth of epidural injections in the medicare population from 2000 to 2011. Pain Physician. 2013;16:E349–64. [PubMed] [Google Scholar]
- 11.Manchikanti L, Pampati V, Falco FJ, Hirsch JA. Growth of spinal interventional pain management techniques: analysis of utilization trends and Medicare expenditures 2000 to 2008. Spine (Phila Pa 1976) 2013;38:157–68. doi: 10.1097/BRS.0b013e318267f463. [DOI] [PubMed] [Google Scholar]
- 12.Manchikanti L, Falco FJ, Singh V, Pampati V, Parr AT, Benyamin RM, Fellows B, Hirsch JA. Utilization of interventional techniques in managing chronic pain in the Medicare population: analysis of growth patterns from 2000 to 2011. Pain Physician. 2012;15:E969–82. [PubMed] [Google Scholar]
- 13.Tosteson AN, Skinner JS, Tosteson TD, Lurie JD, Andersson GB, Berven S, Grove MR, Hanscom B, Blood EA, Weinstein JN. The cost effectiveness of surgical versus nonoperative treatment for lumbar disc herniation over two years: evidence from the Spine Patient Outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2008;33:2108–15. doi: 10.1097/brs.0b013e318182e390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parr AT, Diwan S, Abdi S. Lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain: a systematic review. Pain Physician. 2009;12:163–88. [PubMed] [Google Scholar]
- 15.Manchikanti L, Pampati V, Boswell MV, Smith HS, Hirsch JA. Analysis of the growth of epidural injections and costs in the Medicare population: a comparative evaluation of 1997, 2002, and 2006 data. Pain Physician. 2010;13:199–212. [PubMed] [Google Scholar]
- 16.Manchikanti L, Singh V, Pampati V, Smith HS, Hirsch JA. Analysis of growth of interventional techniques in managing chronic pain in the Medicare population: a 10-year evaluation from 1997 to 2006. Pain Physician. 2009;12:9–34. [PubMed] [Google Scholar]
- 17.Conn A, Buenaventura RM, Datta S, Abdi S, Diwan S. Systematic review of caudal epidural injections in the management of chronic low back pain. Pain Physician. 2009;12:109–35. [PubMed] [Google Scholar]
- 18.Manchikanti L, Benyamin RM, Falco FJ, Kaye AD, Hirsch JA. Do Epidural Injections Provide Short- and Long-term Relief for Lumbar Disc Herniation? A Systematic Review. Clin Orthop Relat Res. 2015;473:1940–56. doi: 10.1007/s11999-014-3490-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buenaventura RM, Datta S, Abdi S, Smith HS. Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Physician. 2009;12:233–51. [PubMed] [Google Scholar]
- 20.Manchikanti L, Boswell MV, Singh V, Derby R, Fellows B, Falco FJ, Datta S, Smith HS, Hirsch JA. Comprehensive review of therapeutic interventions in managing chronic spinal pain. Pain Physician. 2009;12:E123–98. [PubMed] [Google Scholar]
- 21.Manchikanti L, Singh V, Boswell MV. Interventional pain management at crossroads: the perfect storm brewing for a new decade of challenges. Pain Physician. 2010;13:E111–40. [PubMed] [Google Scholar]
- 22.Benyamin RM, Singh V, Parr AT, Conn A, Diwan S, Abdi S. Systematic review of the effectiveness of cervical epidurals in the management of chronic neck pain. Pain Physician. 2009;12:137–57. [PubMed] [Google Scholar]
- 23.Manchikanti L. Role of neuraxial steroids in interventional pain management. Pain Physician. 2002;5:182–99. [PubMed] [Google Scholar]
- 24.Byröd G, Otani K, Brisby H, Rydevik B, Olmarker K. Methylprednisolone reduces the early vascular permeability increase in spinal nerve roots induced by epidural nucleus pulposus application. J Orthop Res. 2000;18:983–7. doi: 10.1002/jor.1100180619. [DOI] [PubMed] [Google Scholar]
- 25.Lundin A, Magnuson A, Axelsson K, Nilsson O, Samuelsson L. Corticosteroids peroperatively diminishes damage to the C-fibers in microscopic lumbar disc surgery. Spine (Phila Pa 1976) 2005;30:2362–7. doi: 10.1097/01.brs.0000184685.93424.f0. discussion 2368. [DOI] [PubMed] [Google Scholar]
- 26.Hua SY, Chen YZ. Membrane receptor-mediated electrophysiological effects of glucocorticoid on mammalian neurons. Endocrinology. 1989;124:687–91. doi: 10.1210/endo-124-2-687. [DOI] [PubMed] [Google Scholar]
- 27.Hayashi N, Weinstein JN, Meller ST, Lee HM, Spratt KF, Gebhart GF. The effect of epidural injection of betamethasone or bupivacaine in a rat model of lumbar radiculopathy. Spine (Phila Pa 1976) 1998;23:877–85. doi: 10.1097/00007632-199804150-00008. [DOI] [PubMed] [Google Scholar]
- 28.Pasqualucci A, Varrassi G, Braschi A, Peduto VA, Brunelli A, Marinangeli F, Gori F, Colò F, Paladini A, Mojoli F. Epidural local anesthetic plus corticosteroid for the treatment of cervical brachial radicular pain: single injection versus continuous infusion. Clin J Pain. 2007;23:551–7. doi: 10.1097/AJP.0b013e318074c95c. [DOI] [PubMed] [Google Scholar]
- 29.Tachihara H, Sekiguchi M, Kikuchi S, Konno S. Do corticosteroids produce additional benefit in nerve root infiltration for lumbar disc herniation? Spine (Phila Pa 1976) 2008;33:743–7. doi: 10.1097/BRS.0b013e3181696132. [DOI] [PubMed] [Google Scholar]
- 30.Riew KD, Park JB, Cho YS, Gilula L, Patel A, Lenke LG, Bridwell KH. Nerve root blocks in the treatment of lumbar radicular pain. A minimum five-year follow-up. J Bone Joint Surg Am. 2006;88:1722–5. doi: 10.2106/JBJS.E.00278. [DOI] [PubMed] [Google Scholar]
- 31.Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Lumbar facet joint nerve blocks in managing chronic facet joint pain: one-year follow-up of a randomized, double-blind controlled trial: Clinical Trial NCT00355914. Pain Physician. 2008;11:121–32. [PubMed] [Google Scholar]
- 32.Manchikanti L, Singh V, Falco FJ, Cash KM, Fellows B. Cervical medial branch blocks for chronic cervical facet joint pain: a randomized, double-blind, controlled trial with one-year follow-up. Spine (Phila Pa 1976) 2008;33:1813–20. doi: 10.1097/BRS.0b013e31817b8f88. [DOI] [PubMed] [Google Scholar]
- 33.Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Evaluation of lumbar facet joint nerve blocks in managing chronic low back pain: a randomized, double-blind, controlled trial with a 2-year follow-up. Int J Med Sci. 2010;7:124–35. doi: 10.7150/ijms.7.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Effectiveness of thoracic medial branch blocks in managing chronic pain: a preliminary report of a randomized, double-blind controlled trial. Pain Physician. 2008;11:491–504. [PubMed] [Google Scholar]
- 35.Manchikanti L, Cash KA, McManus CD, Pampati V, Smith HS. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 1-Discogenic pain without disc herniation or radiculitis. Pain Physician. 2008;11:785–800. [PubMed] [Google Scholar]
- 36.Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 2-Disc herniation and radiculitis. Pain Physician. 2008;11:801–15. [PubMed] [Google Scholar]
- 37.Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 3--Post surgery syndrome. Pain Physician. 2008;11:817–31. [PubMed] [Google Scholar]
- 38.Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y. Cervical epidural injections in chronic discogenic neck pain without disc herniation or radiculitis: preliminary results of a randomized, double-blind, controlled trial. Pain Physician. 2010;13:E265–78. [PubMed] [Google Scholar]
- 39.Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y. The effectiveness of fluoroscopic cervical interlaminar epidural injections in managing chronic cervical disc herniation and radiculitis: preliminary results of a randomized, double-blind, controlled trial. Pain Physician. 2010;13:223–36. [PubMed] [Google Scholar]
- 40.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2010;8:336–41. [PMC free article] [PubMed] [Google Scholar]
- 41.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 42.Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta-analyses. Ann Intern Med. 2001;135:982–9. doi: 10.7326/0003-4819-135-11-200112040-00010. [DOI] [PubMed] [Google Scholar]
- 43.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48. [PubMed] [Google Scholar]
- 45.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 46.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101. [PubMed] [Google Scholar]
- 47.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Manchikanti L, Cash KA, Pampati V, Falco FJ. Transforaminal epidural injections in chronic lumbar disc herniation: a randomized, double-blind, active-control trial. Pain Physician. 2014;17:E489–501. [PubMed] [Google Scholar]
- 49.Cohen SP, White RL, Kurihara C, Larkin TM, Chang A, Griffith SR, Gilligan C, Larkin R, Morlando B, Pasquina PF, Yaksh TL, Nguyen C. Epidural steroids, etanercept, or saline in subacute sciatica: a multicenter, randomized trial. Ann Intern Med. 2012;156:551–9. doi: 10.7326/0003-4819-156-8-201204170-00397. [DOI] [PubMed] [Google Scholar]
- 50.Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Evaluation of the effectiveness of lumbar interlaminar epidural injections in managing chronic pain of lumbar disc herniation or radiculitis: a randomized, double-blind, controlled trial. Pain Physician. 2010;13:343–55. [PubMed] [Google Scholar]
- 51.Manchikanti L, Cash KA, McManus CD, Damron KS, Pampati V, Falco FJ. Lumbar interlaminar epidural injections in central spinal stenosis: preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012;15:51–63. [PubMed] [Google Scholar]
- 52.Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Effect of fluoroscopically guided caudal epidural steroid or local anesthetic injections in the treatment of lumbar disc herniation and radiculitis: a randomized, controlled, double blind trial with a two-year follow-up. Pain Physician. 2012;15:273–86. [PubMed] [Google Scholar]
- 53.Manchikanti L, Cash KA, McManus CD, Pampati V, Benyamin RM. A randomized, double-blind, active-controlled trial of fluoroscopic lumbar interlaminar epidural injections in chronic axial or discogenic low back pain: results of 2-year follow-up. Pain Physician. 2013;16:E491–504. [PubMed] [Google Scholar]
- 54.Manchikanti L, Singh V, Cash KA, Pampati V, Falco FJ. The role of fluoroscopic interlaminar epidural injections in managing chronic pain of lumbar disc herniation or radiculitis: a randomized, double-blind trial. Pain Pract. 2013;13:547–58. doi: 10.1111/papr.12023. [DOI] [PubMed] [Google Scholar]
- 55.Sayegh FE, Kenanidis EI, Papavasiliou KA, Potoupnis ME, Kirkos JM, Kapetanos GA. Efficacy of steroid and nonsteroid caudal epidural injections for low back pain and sciatica: a prospective, randomized, double-blind clinical trial. Spine (Phila Pa 1976) 2009;34:1441–7. doi: 10.1097/BRS.0b013e3181a4804a. [DOI] [PubMed] [Google Scholar]
- 56.Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. A randomized, controlled, double-blind trial of fluoroscopic caudal epidural injections in the treatment of lumbar disc herniation and radiculitis. Spine (Phila Pa 1976) 2011;36:1897–905. doi: 10.1097/BRS.0b013e31823294f2. [DOI] [PubMed] [Google Scholar]
- 57.Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Fluoroscopic caudal epidural injections in managing post lumbar surgery syndrome: two-year results of a randomized, double-blind, active-control trial. Int J Med Sci. 2012;9:582–91. doi: 10.7150/ijms.4672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee HM, Weinstein JN, Meller ST, Hayashi N, Spratt KF, Gebhart GF. The role of steroids and their effects on phospholipase A2. An animal model of radiculopathy. Spine (Phila Pa 1976) 1998;23:1191–6. doi: 10.1097/00007632-199806010-00001. [DOI] [PubMed] [Google Scholar]
- 59.Manchikanti L, Giordano J, Fellows B, Hirsch JA. Placebo and nocebo in interventional pain management: a friend or a foe-or simply foes? Pain Physician. 2011;14:E157–75. [PubMed] [Google Scholar]
- 60.Pasqualucci A. Experimental and clinical studies about the preemptive analgesia with local anesthetics. Possible reasons of the failure. Minerva Anestesiol. 1998;64:445–57. [PubMed] [Google Scholar]
- 61.Mao J, Chen LL. Systemic lidocaine for neuropathic pain relief. Pain. 2000;87:7–17. doi: 10.1016/S0304-3959(00)00229-3. [DOI] [PubMed] [Google Scholar]
- 62.Manchikanti L, Cash KA, McManus CD, Pampati V, Smith HS. One-year results of a randomized, double-blind, active controlled trial of fluoroscopic caudal epidural injections with or without steroids in managing chronic discogenic low back pain without disc herniation or radiculitis. Pain Physician. 2011;14:25–36. [PubMed] [Google Scholar]
- 63.Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Management of pain of post lumbar surgery syndrome: one-year results of a randomized, double-blind, active controlled trial of fluoroscopic caudal epidural injections. Pain Physician. 2010;13:509–21. [PubMed] [Google Scholar]
- 64.Manchikanti L, Cash KA, McManus CD, Pampati V, Benyamin RM. A preliminary report of a randomized double-blind, active controlled trial of fluoroscopic thoracic interlaminar epidural injections in managing chronic thoracic pain. Pain Physician. 2010;13:E357–69. [PubMed] [Google Scholar]
- 65.Dashfield AK, Taylor MB, Cleaver JS, Farrow D. Comparison of caudal steroid epidural with targeted steroid placement during spinal endoscopy for chronic sciatica: a prospective, randomized, double-blind trial. Br J Anaesth. 2005;94:514–9. doi: 10.1093/bja/aei084. [DOI] [PubMed] [Google Scholar]
- 66.Ackerman WE 3rd, Ahmad M. The efficacy of lumbar epidural steroid injections in patients with lumbar disc herniations. Anesth Analg. 2007;104:1217–22. doi: 10.1213/01.ane.0000260307.16555.7f. tables of contents. [DOI] [PubMed] [Google Scholar]
- 67.Iversen T, Solberg TK, Romner B, Wilsgaard T, Twisk J, Anke A, Nygaard O, Hasvold T, Ingebrigtsen T. Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: multicentre, blinded, randomised controlled trial. BMJ. 2011;343:d5278. doi: 10.1136/bmj.d5278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Iversen T, Solberg TK, Romner B, Wilsgaard T, Twisk J, Anke A, Nygaard O, Hasvold T, Ingebrigtsen T. Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: multicentre, blinded, randomised controlled trial. BMJ. 2011;343:d5278. doi: 10.1136/bmj.d5278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Iversen T, Solberg TK, Romner B, Wilsgaard T, Twisk J, Anke A, Nygaard O, Hasvold T, Ingebrigtsen T. Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: multicentre, blinded, randomised controlled trial. BMJ. 2011;343:d5278. doi: 10.1136/bmj.d5278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cohen SP. Epidural steroid injections for low back pain. BMJ. 2011;343:d5310. doi: 10.1136/bmj.d5310. [DOI] [PubMed] [Google Scholar]
- 71.Freynhagen R, Baron R, Gockel U, Tölle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006;22:1911–20. doi: 10.1185/030079906X132488. [DOI] [PubMed] [Google Scholar]
- 72.Benzon HT. Epidural steroid injections for low back pain and lumbosacral radiculopathy. Pain. 1986;24:277–95. doi: 10.1016/0304-3959(86)90115-6. [DOI] [PubMed] [Google Scholar]
- 73.Manchikanti L, Datta S, Derby R, Wolfer LR, Benyamin RM, Hirsch JA American Pain Society. A critical review of the American Pain Society clinical practice guidelines for interventional techniques: part 1. Diagnostic interventions. Pain Physician. 2010;13:E141–74. [PubMed] [Google Scholar]
- 74.Manchikanti L, Datta S, Gupta S, Munglani R, Bryce DA, Ward SP, Benyamin RM, Sharma ML, Helm S 2nd, Fellows B, Hirsch JA. A critical review of the American Pain Society clinical practice guidelines for interventional techniques: part 2. Therapeutic interventions. Pain Physician. 2010;13:E215–64. [PubMed] [Google Scholar]
- 75.Manchikanti L, Falco FJ, Boswell MV, Hirsch JA. Facts, fallacies, and politics of comparative effectiveness research: Part I. Basic considerations. Pain Physician. 2010;13:E23–54. [PubMed] [Google Scholar]
- 76.Pham Dang C, Lelong A, Guilley J, Nguyen JM, Volteau C, Venet G, Perrier C, Lejus C, Blanloeil Y. Effect on neurostimulation of injectates used for perineural space expansion before placement of a stimulating catheter: normal saline versus dextrose 5% in water. Reg Anesth Pain Med. 2009;34:398–403. doi: 10.1097/AAP.0b013e3181b48648. [DOI] [PubMed] [Google Scholar]
- 77.Tsui BC, Kropelin B, Ganapathy S, Finucane B. Dextrose 5% in water: fluid medium for maintaining electrical stimulation of peripheral nerves during stimulating catheter placement. Acta Anaesthesiol Scand. 2005;49:1562–5. doi: 10.1111/j.1399-6576.2005.00736.x. [DOI] [PubMed] [Google Scholar]
- 78.Indahl A, Kaigle AM, Reikeräs O, Holm SH. Interaction between the porcine lumbar intervertebral disc, zygapophysial joints, and paraspinal muscles. Spine (Phila Pa 1976) 1997;22:2834–40. doi: 10.1097/00007632-199712150-00006. [DOI] [PubMed] [Google Scholar]


