Abstract
A patient with dilated cardiomyopathy with poor ejection fraction posted for laparoscopic surgery for rectal cancer which was successfully performed under general anesthesia with endotracheal intubation and mechanical ventilation was reported. Our observations strongly indicate that detailed preoperative assessment, watchful intraoperative monitoring, and skillful optimization of fluid status and hemodynamic play important role in the high risk patient under general anesthesia with endotracheal intubation and mechanical ventilation.
Keywords: Anaesthetic management, laparoscopic surgery, dilated cardiomyopathy
Introduction
Dilated cardiomyopathy (DCM) that is characterized by ventricular dilation and impaired myocardial dilation is recognized as an important disorder that threatens human health and life [1-3]. DCM is well known to be defined by the presence of (a) fractional myocardial shortening <25% and/or ejection fraction <45% and (b) left ventricular end diastolic diameter >117% excluding any known cause of myocardial disease [4-6]. DCM and resulting comorbidity, such as heart failure or atrial fibrillation, significantly increase the risk for perioperative adverse events [7]. It is widely acknowledged that management of patients with severe cardiomyopathies and left ventricular dysfunction is associated with a high morbidity and mortality in the preoperative period [8,9]. Left ventricular ejection fraction (LVEF) of ≤35% is considered to be an optimal predictor of postoperative cardiac events [6,10]. Because of the increased risks of perioperative complications, anesthetic management of DCM requires the application of a specific technique. It has been shown that appropriate preoperative assessment, adequate perioperative monitoring, and early intervention to hemodynamic disturbances, may help prevent adverse events and improve patient outcome [11]. Herein we provide a patient with dilated cardiomyopathy with poor ejection fraction posted for laparoscopic surgery for rectal cancer which was successfully performed under general anesthesia with endotracheal intubation and mechanical ventilation.
Case presentation
The patient was a 63-year-old man with a medical history notable for diabetes mellitus, benign prostatic hypertrophy, and a dilated cardiomyopathy characterized by severe left ventricular dysfunction without a history of congestive heart failure (CHF), in Huanggan Central Hospital, Hubei, PR China. Ten days ago, he was admitted to another hospital with heart palpitation, chest discomfort, weight loss, abdominal pain, changes in bowel habit, or bleeding, and had no history of abdominal surgery or trauma. On examination, there was rectal neoplasm. He was referred to our institution with a curative intent.
On admission, he had a temperature of 36.4°C, blood pressure of 140/90 mm Hg, heart rate of 110 bpm, respiratory rate of 19 bpm, weight of 67.5 kg, and O2 saturation of 96% on room air. Initial laboratory studies of electrolytes, complete blood count and cardiac enzymes were within normal limits. EKG showed sinus tachycardia and incomplete left bundle branch block. Chest radiograph showed biventricular enlargement (Figure 1A). He had undergone a cardiac ultrasound imaging study, which revealed a left ventricle of 62 mm, left atrium of 48 mm, right ventricle of 36 mm, right atrium of 43 mm, a left-ventricular shortening <18%, and a left-ventricular ejection fraction of 31% (Figure 1B-D). He appeared comfortable seated in a supine position and denied dyspnea. On examination, auscultation revealed low breath sounds, a little moist rale over the left lung base, and a grade 2/6 systolic murmur at the apex. At the time of his cardiac evaluation, he was mildly symptomatic, and didn’t experience edema of lower limbs. The patient understood and accepted the risks and benefits of surgery and anesthesia by a frank discussion, and wished very much to proceed with elective laparoscopic surgery for rectal cancer. Written informed consent was obtained from the patient and his family.
Figure 1.
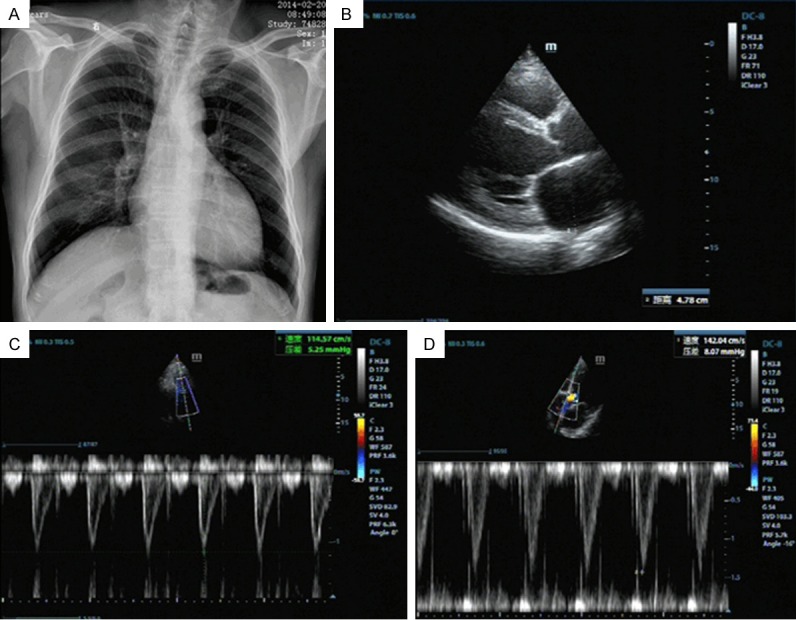
Imaging data. A. Chest radiograph showed biventricular enlargement. B-D. Cardiac ultrasound imaging study revealed a left ventricle of 62 mm, left atrium of 48 mm, right ventricle of 36 mm, right atrium of 43 mm, a left-ventricular shortening <18%, and a left-ventricular ejection fraction of 31%.
In the operating room, the patient was lightly sedated with 2 mg intravenous midazolam, and left radial artery cannulation and right internal jugular vein cannulation were performed under local anesthesia. After preoxygenation, intravenous induction of general anesthesia was accomplished with 50 µg sufentanil, 10 mg etomidate, and 50 mg rocuronium. The trachea was easily intubated with a tracheal tube under direct laryngoscopy. After intubation, heart rate of 140 bpm was treated by intravenous cedilanid 0.4 mg. Mild hypotension was initially treated by infusion of epinephrine at 3 to 6 µg/min. Additional support was achieved by intravenous infusion of nitroglycerin 0.3 to 0.8 µg/kg/min to promote right ventricular afterload reduction. General anesthesia was maintained with 1.0% to 1.5% sevoflurane, 0.3-0.6 µg/kg/min remifentanil and 0.1-0.2 mg/kg/min propofol (so as to maintain PaCO2 between 35-45 mmHg). Intermittent doses of rocuronium were administered to maintain skeletal muscle paralysis [12,13]. The depth of anesthesia was monitored by recording entropy (Datex-Ohmeda, GE Healthcare)/bispectral index (BIS). Figure 2 showed intraoperative parameters in response to laparoscopic surgery and anesthetic management. The overall anesthetic goal is to maintain adequate volume expansion by maintaining central venous pressure (CVP) of 10-15 mmHg and avoid decreased perfusion by maintaining mean arterial pressure (MAP).
Figure 2.
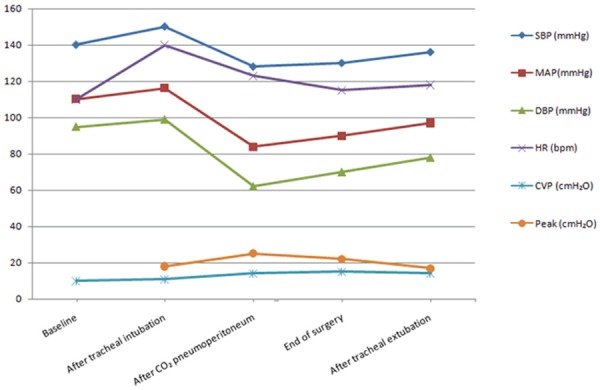
Intraoperative haemodynamics. SBP: systolic blood pressure, MAP: mean arterial pressure, DBP: diastolic blood pressure, CVP: central venous pressure, and Peak: Peak of airway resistance.
The laparoscopic operation for rectal cancer lasted 5 h. After confirmation of neuromuscular recovery, the patient was extubated. After stabilization in the operate room, he was transported to an intensive care unit dedicated to the care of surgical patients after surgery. On postoperative day 2, he was transferred to a step-down unit and was discharged home on postoperative day 6. At last follow-up on postoperative day 30, he had walked independently and made a near full recovery in terms of his motor function.
Discussion
The present case described successful anesthetic management of the patient with dilated cardiomyopathy with poor ejection fraction posted for laparoscopic surgery for rectal cancer. Based on our knowledge, this is the first study in a patient with dilated cardiomyopathy with poor ejection fraction posted for laparoscopic surgery under general anesthesia with endotracheal intubation and mechanical ventilation.
Several clinical studies have demonstrated cardiovascular stability in the patient with dilated cardiomyopathy or low myocardial ejection fraction [14] undergoing non-cardiac surgery. Sumler et al reported general anesthetic management of the patient with dilated cardiomyopathy undergoing pulmonary resection surgery, and indicated that in patients presenting for pulmonary resection, additional effects resulting from positioning, one-lung ventilation, surgical procedures, and contraction of the pulmonary vascular bed imposed physiological effects on cardiovascular function [11]. Sanatkar et al observed the hemodynamic effects of spinal block with low dose of bupivacaine and sufentanil in patients with low myocardial ejection fraction, and reported thedecrease of blood pressure after a low dose of subarachnoid block [14]. Srivastava et al reported anesthetic management of renal transplant surgery in patients of dilated cardiomyopathy with ejection fraction less than 40% using combined spinal epidural technique, and indicated that meticulous preoperative optimization, close intraoperative monitoring, tailoring the anesthetic plan to patient’s specific needs, optimization of fluid status and hemodynamic, and watchful postoperative care are the key to a successful renal transplant in these high risk patients [15]. Pradeep et al reported the successful anesthetic management of a patient with severe dilated cardiomyopathy for fractured femur surgical repair under graded epidural anaesthesia [16]. Kaya et al demonstrated the application of successful anesthetic management of hysterosalpingooophorectomy in a patient who had been diagnosed with severe idiopathic dilated cardiomyopathy by using regional anesthetic management (thoracic epidural anesthesia) [17].
General anesthesia, muscle relaxation, and positive-pressure ventilation all impose cardiovascular burden [18,19]. For most patients with adequate cardiovascular reserve, these effects are well tolerated. However, this case was asked to provide anesthetic care for the patient with significantly reduced cardiac function who required laparoscopic surgery for rectal cancer. Anesthetic management of a patient having dual problems of DCM and laparoscopic surgery is a challenge for the anesthesiologist. Preoperative assessment in the patient with DCM often includes the following factors: Patient with DCM is on the verge of developing cardiac failure, so preoperative volume assessment must be taken care of. Arrhythmias like ventricular tachyarrhythmias and atrial fibrillation are commonly associated with DCM [20-22], so preoperative assessment and correction of electrolytes particularly are very important. Intraoperative monitoring is essential and the following factors must be taken care of: (1) avoidance of drug induced myocardial depression, (2) maintenance of myocardial contractility, (3) hypotension should be avoided to prevent myocardial hypoperfusion, (4) maintenance of adequate preload while preventing fluid overload.
In conclusion, data presented here provide successful anesthetic management of the patient with dilated cardiomyopathy with poor ejection fraction posted for laparoscopic surgery for rectal cancer. Our observations strongly indicate that detailed preoperative assessment, watchful intraoperative monitoring, and skillful optimization of fluid status and hemodynamic play important role in the high risk patient under general anesthesia with endotracheal intubation and mechanical ventilation.
Disclosure of conflict of interest
None.
References
- 1.Strecker T, Rosch J, Weyand M, Agaimy A. Pathological findings in cardiac apex removed during implantation of left ventricular assist devices (LVAD) are non-specific: 13-year-experience at a German Heart Center. Int J Clin Exp Pathol. 2014;7:5549–5556. [PMC free article] [PubMed] [Google Scholar]
- 2.Everitt MD, Sleeper LA, Lu M, Canter CE, Pahl E, Wilkinson JD, Addonizio LJ, Towbin JA, Rossano J, Singh RK, Lamour J, Webber SA, Colan SD, Margossian R, Kantor PF, Jefferies JL, Lipshultz SE. Recovery of echocardiographic function in children with idiopathic dilated cardiomyopathy: results from the pediatric cardiomyopathy registry. J Am Coll Cardiol. 2014;63:1405–1413. doi: 10.1016/j.jacc.2013.11.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.George RS, Birks EJ, Cheetham A, Webb C, Smolenski RT, Khaghani A, Yacoub MH, Kelion A. The effect of long-term left ventricular assist device support on myocardial sympathetic activity in patients with non-ischaemic dilated cardiomyopathy. Eur J Heart Fail. 2013;15:1035–1043. doi: 10.1093/eurjhf/hft059. [DOI] [PubMed] [Google Scholar]
- 4.Expression of concern. ‘Guidelines: Pre-operative Cardiac Risk Assessment and Perioperative Cardiac Management in Non-Cardiac Surgery’, [Eur Heart J (2009) 30 (22), 2769-2812; doi:10.1093/eurheartj/ehp337] . Eur Heart J. 2013;34:3460. doi: 10.1093/eurheartj/eht431. [DOI] [PubMed] [Google Scholar]
- 5.Poldermans D, Bax JJ, Boersma E, De Hert S, Eeckhout E, Fowkes G, Gorenek B, Hennerici MG, Iung B, Kelm M, Kjeldsen KP, Kristensen SD, Lopez-Sendon J, Pelosi P, Philippe F, Pierard L, Ponikowski P, Schmid JP, Sellevold OF, Sicari R, Van den Berghe G, Vermassen F, Hoeks SE, Vanhorebeek I, Vahanian A, Auricchio A, Ceconi C, Dean V, Filippatos G, Funck-Brentano C, Hobbs R, Kearn P, McDonag T, McGregor K, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Vardas P, Widimsky P, De Caterina R, Agewall S, Al Attar N, Andreotti F, Anker SD, Baron-Esquivias G, Berkenboom G, Chapoutot L, Cifkova R, Faggiano P, Gibbs S, Hansen HS, Iserin L, Israel CW, Kornowski R, Eizagaechevarria NM, Pepi M, Piepoli M, Priebe HJ, Scherer M, Stepinska J, Taggart D, Tubaro M. Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery: the Task Force for Preoperative Cardiac Risk Assessment and Perioperative Cardiac Management in Non-cardiac Surgery of the European Society of Cardiology (ESC) and endorsed by the European Society of Anaesthesiology (ESA) Eur J Anaesthesiol. 2010;27:92–137. doi: 10.1097/EJA.0b013e328334c017. [DOI] [PubMed] [Google Scholar]
- 6.Poldermans D, Bax JJ, Boersma E, De Hert S, Eeckhout E, Fowkes G, Gorenek B, Hennerici MG, Iung B, Kelm M, Kjeldsen KP, Kristensen SD, Lopez-Sendon J, Pelosi P, Philippe F, Pierard L, Ponikowski P, Schmid JP, Sellevold OF, Sicari R, Van den Berghe G, Vermassen F. Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery. Eur Heart J. 2009;30:2769–2812. doi: 10.1093/eurheartj/ehp337. [DOI] [PubMed] [Google Scholar]
- 7.Mittnacht AJ, Fanshawe M, Konstadt S. Anesthetic considerations in the patient with valvular heart disease undergoing noncardiac surgery. Semin Cardiothorac Vasc Anesth. 2008;12:33–59. doi: 10.1177/1089253208316442. [DOI] [PubMed] [Google Scholar]
- 8.Mutlak H, Humpich M, Zacharowski K, Lehmann R, Meininger D. Valvular heart disease: anesthesia in non-cardiac surgery. Anaesthesist. 2011;60:799–813. doi: 10.1007/s00101-011-1939-3. [DOI] [PubMed] [Google Scholar]
- 9.Sirvinskas E. Peculiarities of anesthesia for patients with valvular heart disease during non-cardiac surgery. Medicina (Kaunas) 2003;39:730–738. [PubMed] [Google Scholar]
- 10.Ruwald MH, Solomon SD, Foster E, Kutyifa V, Ruwald AC, Sherazi S, McNitt S, Jons C, Moss AJ, Zareba W. Left Ventricular Ejection Fraction Normalization in Cardiac Resynchronization Therapy and Risk of Ventricular Arrhythmias and Clinical Outcomes: Results from the MADIT-CRT Trial. Circulation. 2014;130:2278–86. doi: 10.1161/CIRCULATIONAHA.114.011283. [DOI] [PubMed] [Google Scholar]
- 11.Sumler ML, Andritsos MJ, Blank RS. Anesthetic management of the patient with dilated cardiomyopathy undergoing pulmonary resection surgery: a case-based discussion. Semin Cardiothorac Vasc Anesth. 2013;17:9–27. doi: 10.1177/1089253212453620. [DOI] [PubMed] [Google Scholar]
- 12.Iwasaki H, Takahoko K, Otomo S, Sasakawa T, Kunisawa T. Monitoring of neuromuscular blockade in one muscle group alone may not reflect recovery of total muscle function in patients with ocular myasthenia gravis. Can J Anaesth. 2013;60:1222–1227. doi: 10.1007/s12630-013-0042-4. [DOI] [PubMed] [Google Scholar]
- 13.Eikermann M, Groeben H, Husing J, Peters J. Accelerometry of adductor pollicis muscle predicts recovery of respiratory function from neuromuscular blockade. Anesthesiology. 2003;98:1333–1337. doi: 10.1097/00000542-200306000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Sanatkar M, Sadeghi M, Esmaeili N, Sadrossadat H, Shoroughi M, Ghazizadeh S, Khoshraftar E, Pour Anvari H, Alipour N. The hemodynamic effects of spinal block with low dose of bupivacaine and sufentanil in patients with low myocardial ejection fraction. Acta Med Iran. 2013;51:438–443. [PubMed] [Google Scholar]
- 15.Srivastava D, Tiwari T, Sahu S, Chandra A, Dhiraaj S. Anaesthetic management of renal transplant surgery in patients of dilated cardiomyopathy with ejection fraction less than 40% Anesthesiol Res Pract. 2014;2014:525969. doi: 10.1155/2014/525969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pradeep Kumar K, Jagadesh G. Anaesthetic management of a patient with dilated cardiomyopathy for fracture femur surgery-a case report. J Clin Diagn Res. 2014;8:172–173. doi: 10.7860/JCDR/2014/7102.4154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaya C, Koksal E, Ustun YB, Semizoglu Y, Yilmaz N. Anesthetic management of hysterosalpingooophorectomy in a case with severe idiopathic dilated cardiomyopathy. Med Arch. 2014;68:144–146. doi: 10.5455/medarh.2014.68.144-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baumert JH, Hein M, Hecker KE, Satlow S, Neef P, Rossaint R. Xenon or propofol anaesthesia for patients at cardiovascular risk in non-cardiac surgery. Br J Anaesth. 2008;100:605–611. doi: 10.1093/bja/aen050. [DOI] [PubMed] [Google Scholar]
- 19.Larsen JR, Torp P, Norrild K, Sloth E. Propofol reduces tissue-Doppler markers of left ventricle function: a transthoracic echocardiographic study. Br J Anaesth. 2007;98:183–188. doi: 10.1093/bja/ael345. [DOI] [PubMed] [Google Scholar]
- 20.Theis JL, Zimmermann MT, Larsen BT, Rybakova IN, Long PA, Evans JM, Middha S, de Andrade M, Moss RL, Wieben ED, Michels VV, Olson TM. TNNI3K mutation in familial syndrome of conduction system disease, atrial tachyarrhythmia and dilated cardiomyopathy. Hum Mol Genet. 2014;23:5793–5804. doi: 10.1093/hmg/ddu297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han LN, Guo SL, Lin XM, Shi XM, Zang CB, Yang LM, Ding GL. Torasemide reduces dilated cardiomyopathy, complication of arrhythmia, and progression to heart failure. Genet Mol Res. 2014;13:7262–7274. doi: 10.4238/2014.September.5.11. [DOI] [PubMed] [Google Scholar]
- 22.Saito T, Asai K, Sato S, Takano H, Mizuno K, Shimizu W. Ultrastructural features of cardiomyocytes in dilated cardiomyopathy with initially decompensated heart failure as a predictor of prognosis. Eur Heart J. 2015;36:724–32. doi: 10.1093/eurheartj/ehu404. [DOI] [PubMed] [Google Scholar]


