Abstract
Objectives: To describe a case of extramedullary-intradural metastases causing cauda equina syndrome (CES) as the primary syndrome of lung cancer, and to review the pertinent medical literature. Summary of Background Data: Intradural spinal metastasis is rare, accounting for 6% of all spinal metastases. Of all primary lesion types, lung carcinoma is about 40-85%. Extramedullary-intradural metastases of lung cancer causing CES is unusual. Methods: A 55-year-old patient with symptoms of low back pain that radiated to bilateral lower legs with painful paresthesias and piecemeal sphincter disturbances and lead to urinary incontinence, and constipation at last for three months. The MRI showed that there was an isolated, well-demarcated, intradural extramedullary mass at the L3, 4 levels. Results: The patient was admitted to the hospital as the severe cauda equina syndrome (CES) and considering the possibility of nerve system neoplasms for surgery. After a series of examinations, the X-ray and computed tomography (CT) detected a tumor in the left upper lobe with hilar and mediastinal lymph node metastases. The concluded diagnosis through histopathologic examination with immunohistochemistry after the patient received an L3-L4 laminectomy and tumor excision and biopsy was extramedullary-intradural spinal metastasis of the small cell lung cancer (SCLC). The patient had a rapid improvement of the CES. Conclusion: Although the majority of cauda equina tumors are primary tumors, extramedullary-intradural metastasis should be considered before surgery in patients with rapid developed CES.
Keywords: Cauda equina syndrome, small cell lung cancer, extramedullary intradural spinal metastasis
Introduction
Metastasis at intradural-extramedullary cauda equine caused by lung cancer was very rare [1]. Once the neoplasm metastasize to the cauda equina, symptoms such as low back pain, bilateral sciatica, motor weakness of the lower extremities, and rectal and bladder sphincter dysfunction may occur and is therefore clinically diagnosed as cauda equina syndrome (CES) [1-3]. To our knowledge, the isolated metastasis cases at intradural-extramedullary cauda equine caused by SCLC were not found before the detection and therapy of SCLC [3]. This report describes the case of a 55-year-old man who developed rapid cauda equina syndrome then was confirmed as the small cell lung cancer by radiologic check and histopathologic examination with immunohistochemistry.
Case report
A 55-year-old man with symptoms and signs of low back pain that radiated to bilateral lower legs with painful paresthesias and piecemeal sphincter disturbances for three months was admitted to our hospital in September 2011. The patient had a smoking history of about 30 years and had quit smoking for about 5 years. The patient presented with low back pain when fasciitis was initially considered. Conservative therapy such as rest and massage is preformed. They could work a little. Eight weeks later, painful paresthesias and dysesthesias spread to the posterior area of thighs, buttocks and the perianal area with progressively worsened conditions. In clinics, the patient’s lumbosacral magnetic resonance imaging (MRI) revealed an extramedullary intradural mass measuring 2.6 cm craniocaudally, 1.2 cm coronally by 1.1 cm anteroposteriorly in the horizontal plane at the L3, 4 level (Figure 1A and 1B). He was admitted to the hospital considering the possibility of nerve system neoplasms for surgery in September 2011. During this time, the constipation sustained in conjunction with urinary incontinence. The contrast enhanced MRI showed the mild homogeneous enhancement and a clear boundary for the mass (Figure 2). The neurologic examination showed no decreased muscle tone and strength in the legs. Hamstring and quadriceps abductor and adductor strength of his legs were 4/5. Ankle flexor and extensor strengths were measured to be 5 bilateral. Bilateral Babinski signs were not elicited. Bilateral deep tendon reflexes decreased. Sensation of vibration, joint position, pinprick, and temperature was impaired in both legs. Bilateral elevation test of straight leg were positive at 45°. There were tenderness percussion pain at spinous processes of L3-5. Radiating pain was obvious while doing that. The thoracic cord, cervical cord and brain MRI scans showed no evidence of tumor.
Figure 1.
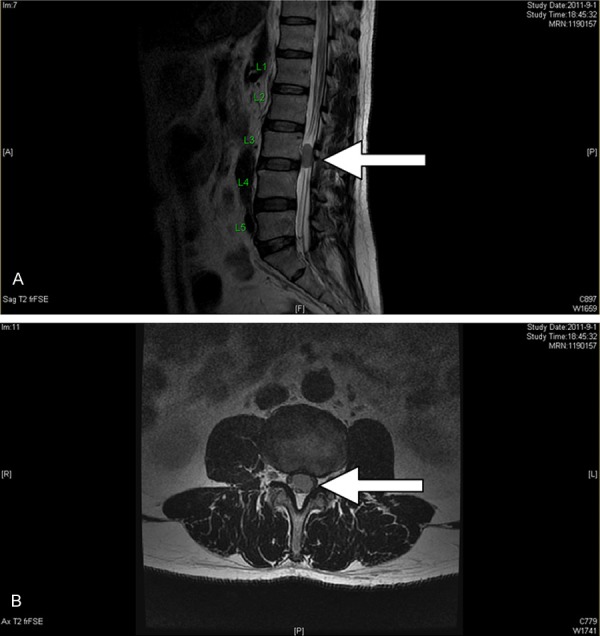
The lumbosacral magnetic resonance imaging showing an extramedullary-intradural mass (white arrows) measuring 2.6 cm craniocaudally by 1.2 cm coronally (A) and 1.1 cm anteroposteriorly in horizontal plane (B) at the L3-L4 level. The mass demonstrated relatively low signal intensity on T2-weightedimage in the sagittal (A) and axial (B) plane.
Figure 2.

The contrast enhanced lumbosacral magnetic resonance imaging showing an extramedullary intradural mass (white arrow) demonstrated the mild homogeneous enhancement, a clear boundary and relatively intermediate signal intensity on T1-weighted image in the sagittal plane.
The preoperative routine chest radiograph showed an abnormal mass in the left lung. A chest computed tomography (CT) scan revealed a tumor in the left upper lobe with ipsilateral hilar and mediastinal lymph node metastases (Figure 3). There is no evidence of other metastasis according to bone scan. The patient was radiographically and clinically diagnosed as lung cancer (clinical stage IV) by the supporting findings.
Figure 3.
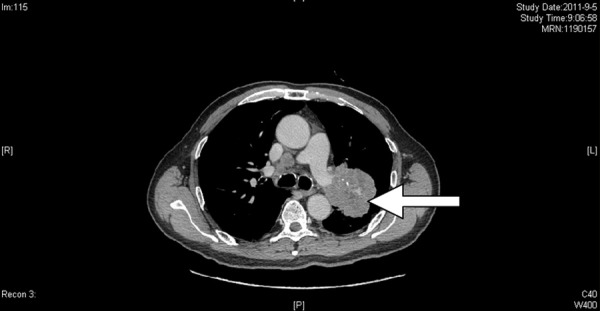
A chest computed tomography (CT) scan revealed a mass (white arrows) in the left upper lobe with ipsilateral hilar and mediastinal lymph node metastases.
The patient underwent an L3-L4 laminectomy and internal fixation because of the serious pain and CES (constipation and urinary incontinence) firstly. After opening dural, we found a pale pink fragile mass, which infiltrated and surrounded the majority of the caudal rootlets. There is no obvious erosion to nerve (Figure 4), so we resected the tumor as most as we could. The pathologic section of extramedullary-intradural spinal metastasis showed the tumor cells arranged like nest and flakes and were beam shaped and adenoid structured. There were hemorrhage and necrosis partly. It’s obvious that there were small round and oval cells with nuclear molding. The cells were characterized by hyperchromatic nuclei with scanty cytoplasm, ill-defined cell borders. The SCLC was diagnosed by histopathologic examination with HE and immunohistochemistry staining (CK7(partly+), CK20(-), TTF-1(+++), SyN(++), CgA(partly+), Vimentin(-), CK(focus+), EMA(partly+), S-100(-), GFAP(-), Ki-67(70%+)) (Figure 5A-C).
Figure 4.
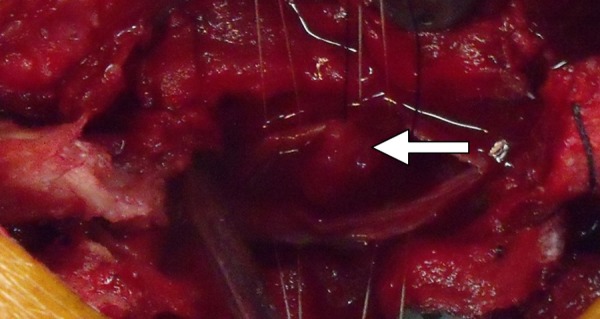
The picture showed a pale pink fragile mass, which infiltrated and surrounded the majority of the caudal rootlets. There is no obvious erosion to nerve.
Figure 5.
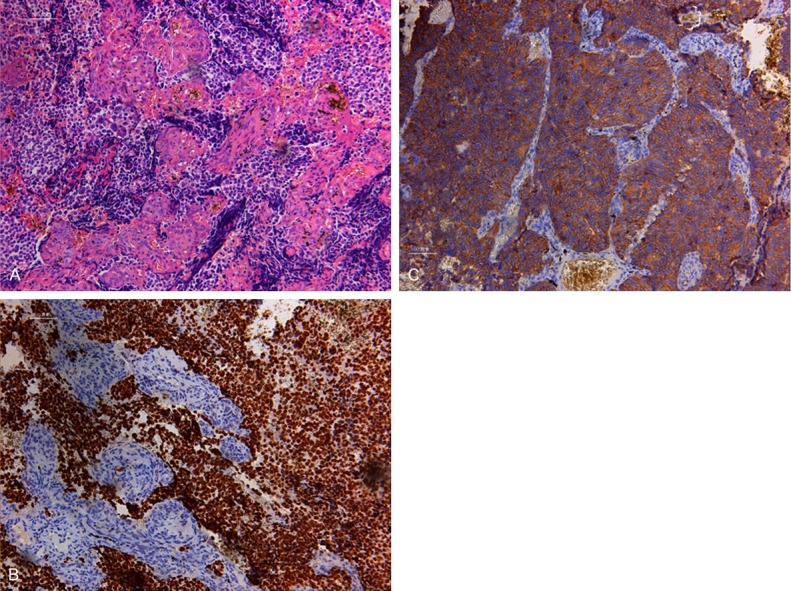
A hematoxylin and eosin-stained tissue section showed lots of small round and oval cells with nuclear molding. The cells had hyperchromatic nuclei with scanty cytoplasm. (A) Immunohistochemical staining was strong positive for thyroid transcription factor-1 (TTF-1) (B) and synaptophysin(SyN) (C) stain. Scale bars =20 µm? Magnified Zoom 100 times.
Two weeks after the surgery, treatments of combination chemotherapy with cisplatin and etoposide were performed. The wound healed and there was no pain any more. He could urinate himself after removing the catheter. After the first couse of chemotherapy, the patient was discharged from our hospital in September 2011. And the patient was followed up regularly and died after one year.
Discussion
CES is the clinical diagnosis of polyradicular symptomatology caused by the compression of the lumbosacral nerve roots located in the dural sac [1-3]. Spinal neoplasms were the main causes of the CES. Different spinal neoplasm causing the CES have different locations, such as epidural, intramedullary, and extramedullary intradural [4-6]. Most of patients were affected by epidural spinal cord compression. The majority of isolated cauda equina tumors causing CES are primary neurologic tumors such as glioma and meningioma [7]. Extramedullary-intradural cauda equina metastatic tumors from outside the central nervous system are very rare [1-8]. Up to now, there are 8 cases, including our current case, being reported as the cauda equine metastases caused by lung cancer. (see Table 1) 20 cases, including this case, have been reported in the literature. Renal cell carcinoma was the most common source of cauda equine metastasis in all the reported cases [9-32].
Table 1.
[3] Patient profiles in some reported cases of intradural extramedullary cauda equine spinal metastasis of lung cancer
| Author | Age/sex | level | interval | Num (Sol./Mul.) | Clincal syndrome | Brain Invol. | Pathology of lung cancer | Therapy | Outcome | Fellow-up time |
|---|---|---|---|---|---|---|---|---|---|---|
| Coutinho LM [1] | 60/M | Cauda equina | 3 ms | Sol | pain | unknown | undifferenciated carcinoma | Surg | unknown | unknown |
| Lin CL [3] | 79/M | L2-3 | 1 m | Sol | CES+pain+ | no | SCLC | Surg | Death | 1 m |
| Kotil K [10] | 50/M | L4/5 | 2 ws | Sol | CES | no | adenocarcinoma | Surg | Resolved | 1 ys |
| ERIC BLONDET [11] | 23/M | L3-4 | 6 ms | Sol | Pain | no | atypical lung carcinoid | Surg | Improved | 2 ys death |
| Cansever T [12] | 79/M | L2-3 | 1y | Sol | CES+pain | no | pulmonary squamous cell | Surg | Improved | unknown |
| Chow TS [13] | 61/M | L3-4 | Average 3.6 ms | Unknown | sensory changes | unknown | adenocarcinoma | Surg | Improved | 6 ms death |
| Tsimpas A [14] | 62/M | L2 | 4 ms | Sol | Pain+weakness | unknown | Large cell neuroendocrine carcinoma | Surg | Pain release | 12 ms |
| Present case | 55/M | L3-4 | 3 ms | Sol | CES+Pain | no | SCLC | Surg | Death | 12 ms |
All patients had the diagnosis with previous cancer history to differentiate spinal cauda equina metastasis from primary neoplastic lesions. Our reported case here has no cancer history until the detection of CES. CES is the primary syndrome. He also has no proof of other metastasis. In this case, we should make the diagnosis with clinical history, MRI and the exploration of surgery. The syndrome had a quick clinical progression within 3 months. MRI showed that there was a isolated mass in cauda equine with clear edge. However, because of the rapid progress in CES, a diagnostic surgery of decompression and biopsy of the mass lesion was preformed firstly. This released the CES. At the same time, we got the clear diagnosis of the mass. Our case is a rare case with metastasis at intradural-extramedullary spinal cord caused by small cell lung cancer. SCLC is very aggressive in clinical progression, with the inclination of frequent widespread metastases. But to the best of our knowledge, this is the first reported case of isolated extramedullary intradural spinal metastasis of SCLC causing CES which was the the primary syndrome of lung cancer.
A decompression surgery mostly of laminectomy is necessary when a patient develops cauda equine syndrome with the injury of sphincter function. As what was said in the literature (Table 1), most of the surgeries could give the patients a obvious improve in the syndromes even if possibly it couldn’t help to improve the survival time and avoid the complications of spinal fluid leak, hematoma, postoperative infections, failure to resect the tumor completely et al. [4]. Specially to SCLC patient with extramedullary intradural spinal metastasis, the tumor is aggressive. The immediate surgery is still recommended following the rapid developed CES [4,5].
Up to now, there were 5 possible routes for metastatic intradural spinal tumor from outside the central nervous system [1-9]. They are the rich venous plexus route; perineural lymphatics route; seeding route from involved osseous structures to the cerebrospinal fluid through the dura; spreading route via subarachnoid space; and hematogenous via the arterial system route [3,9-32]. We tried to find the possible route through which our reported case metastasized. Because all the auxiliary examination revealed no evidence of bony, abdominal and cerebral metastasis in our case, hematogenous metastasis seem to be the most possible way to spread. Small cell lung cancer is predisposed to hematogenous spreading. All of the reported cases had had metastasis or treatments of lung cancer before the unusual metastasis to the cauda equine. But our case is a case of extramedullary intradural metastases causing cauda equine syndrome (CES) as the primary symptom of lung cancer. Maybe that means this small cell lung cancer is more aggressive. We must watch out the unusual metastasis to the cauda equina in lung cancer cases especially in SCLC cases. At the same time, we should find the possible evidence of metastasis in extramedullary-intradural tumor cases when we make the diagnosis. The extramedullary-intradural metastases causing cauda equine syndrome (CES) maybe is the sign of deterioration of SCLC.
Acknowledgements
This work was funded by the Chinese National Natural Science Fund (31271284, 31171150, 81171146, 30971526, 31100860, 31040043, 31371210 81372044), The Chinese Educational Ministry New Century Excellent Talents Support Project (BMU20110270), Chinese National Ministry of Science and Technology 973 Project (No. 2014CB542200) and 863 Project (No. SS2015AA020501). The ministry of education innovation team (IRT1201).
Disclosure of conflict of interest
None.
References
- 1.Coutinho LM, Teixeira JL. Metastatic carcinoma involving the cauda equine. Arq Neuropsiquiatr. 1976;34:288–92. doi: 10.1590/s0004-282x1976000300010. [DOI] [PubMed] [Google Scholar]
- 2.Hargraves RW, Cotelingam JD, Harris RD, Pulliam MW. Unusual metastasis to the cauda equina: case report. Neurosurgery. 1986;19:828–30. doi: 10.1227/00006123-198611000-00020. [DOI] [PubMed] [Google Scholar]
- 3.Lin CL, Chang JL, Lo HC, Wu KA. Extramedullary-intradural spinal metastasis of small cell lung cancer causing cauda equina syndrome. Am J Med Sci. 2010;339:192–4. doi: 10.1097/MAJ.0b013e3181bedd1f. [DOI] [PubMed] [Google Scholar]
- 4.Frey I, Le Breton C, Lefkopoulos A, Perrot N, Khalil A, Chopier J, Le Blanche A, Bigot JM. Intradural extramedullary spinal canal secondary neoplasms: MR findings in 30 patients. Eur Radiol. 1998;8:1187–92. doi: 10.1007/s003300050532. [DOI] [PubMed] [Google Scholar]
- 5.Schaller B, Merlo A, Kirsch E, Lehmann K, Huber PR, Lyrer P, Steck AJ, Gratzl O. Prostate-specific antigen in the cerebrospinal fluid leads to diagnosis of solitary cauda equina metastasis: a unique case report and review of the literature. Br J Cancer. 1998;77:2386–9. doi: 10.1038/bjc.1998.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wippold FJ 2nd, Smirniotopoulos JG, Pilgram TK. Lesions of the cauda equina: a clinical and pathology review from the Armed Forces Institute of Pathology. Clin Neurol Neurosurg. 1997;99:229–34. doi: 10.1016/s0303-8467(97)00095-4. [DOI] [PubMed] [Google Scholar]
- 7.Kim DY, Lee JK, Moon SJ, Kim SC, Kim CS. Intradural spinal metastasis to the cauda equina in renal cell carcinoma: a case report and review of the literature. Spine (Phila Pa 1976) 2009;34:E892–5. doi: 10.1097/BRS.0b013e3181b34e6c. [DOI] [PubMed] [Google Scholar]
- 8.Jallo GI, Kothbauer KF, Silvera VM, Epstein FJ. Intraspinal clear cell meningioma: diagnosis and management: report of two cases. Neurosurgery. 2001;48:218–21. doi: 10.1097/00006123-200101000-00042. discussion 221-2. [DOI] [PubMed] [Google Scholar]
- 9.Okamoto H, Shinkai T, Matsuno Y, Saijo N. Intradural parenchymal involvement in the spinal subarachnoid space associated with primary lung cancer. Cancer. 1993;72:2583–8. doi: 10.1002/1097-0142(19931101)72:9<2583::aid-cncr2820720912>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 10.Kotil K, Kilinc BM, Bilge T. Spinal metastasis of occult lung carcinoma causing cauda equina syndrome. J Clin Neurosci. 2007;14:372–5. doi: 10.1016/j.jocn.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Blondet E, Dulou R, Camparo P, Pernot P. Lumbar intradural metastasis of a primary carcinoid tumor of the lung. Case illustration. J Neurosurg Spine. 2005;2:231. doi: 10.3171/spi.2005.2.2.0231. [DOI] [PubMed] [Google Scholar]
- 12.Cansever T, Kabatas S, Civelek E, Yilmaz C, Caner H. Spinal metastasis of occult lung carcinoma causing cauda equine syndrome with lumbar spinal stenosis. Turk Neurosurg. 2011;21:408–12. doi: 10.5137/1019-5149.JTN.2711-09.2. [DOI] [PubMed] [Google Scholar]
- 13.Chow TS, McCutcheon IE. The surgical treatment of metastatic spinal tumors within the intradural extramedullary compartment. J Neurosurg. 1996;85:225–30. doi: 10.3171/jns.1996.85.2.0225. [DOI] [PubMed] [Google Scholar]
- 14.Tsimpas A, Post NH, Moshel Y, Frempong-Boadu AK. Large cell neuroendocrine carcinoma of the lung metastatic to the cauda equina. Spine J. 2010;10:e1–5. doi: 10.1016/j.spinee.2010.03.031. [DOI] [PubMed] [Google Scholar]
- 15.Kubota M, Saeki N, Yamaura A, Iuchi T, Ohga M, Osato K. A rare case of metastatic renal cell carcinoma resembling a nerve sheath tumor of the cauda equina. J Clin Neurosci. 2004;11:530–2. doi: 10.1016/j.jocn.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 16.Lin TK, Chen SM, Jung SM. Solitary intradural extramedullary metastasis of renal cell carcinoma to the conus medullaris. Kaohsiung J Med Sci. 2011;27:45–8. doi: 10.1016/j.kjms.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Maxwell M, Borges LF, Zervas NT. Renal cell carcinoma: a rare source of cauda equina metastasis. Case report. J Neurosurg. 1999;90:129–32. doi: 10.3171/spi.1999.90.1.0129. [DOI] [PubMed] [Google Scholar]
- 18.Mak KH, Kwok JC. Intradural spinal metastasis from renal cell carcinoma: a case report. J Orthop Surg (Hong Kong) 2001;9:57–61. doi: 10.1177/230949900100900212. [DOI] [PubMed] [Google Scholar]
- 19.Gaetani P, Di Ieva A, Colombo P, Tancioni F, Aimar E, Debernardi A, Rodriguez Y Baena R. Intradural spinal metastasis of renal clear cell carcinoma causing cauda equina syndrome. Acta Neurochir (Wien) 2004;146:857–61. doi: 10.1007/s00701-004-0299-z. [DOI] [PubMed] [Google Scholar]
- 20.Takada T, Doita M, Nishida K, Miura J, Yoshiya S, Kurosaka M. Unusual metastasis to the cauda equina from renal cell carcinoma. Spine (Phila Pa 1976) 2003;28:E1114–7. doi: 10.1097/01.BRS.0000049910.72881.A0. [DOI] [PubMed] [Google Scholar]
- 21.Sountoulides P, Metaxa L, Cindolo L. Atypical presentations and rare metastatic sites of renal cell carcinoma: a review of case reports. J Med Case Rep. 2011;5:429. doi: 10.1186/1752-1947-5-429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alfieri A, Mazzoleni G, Schwarz A, Campello M, Broger M, Vitale M, Vigl EE. Renal cell carcinoma and intradural spinal metastasis with cauda equina infiltration: case report. Spine (Phila Pa 1976) 2005;30:161–3. [PubMed] [Google Scholar]
- 23.Amin MB, Amin MB, Tamboli P, Javidan J, Stricker H, de-Peralta Venturina M, Deshpande A, Menon M. Prognostic impact of histologic subtyping o adult renal epithelial neoplasms: an experience of 405 cases. Am J Surg Pathol. 2002;26:281–91. doi: 10.1097/00000478-200203000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Delahunt B, Eble JN. Papillary renal cell carcinoma: a clinicopathologic and immunohistochemical study of 105 tumors. Mod Pathol. 1997;10:537–44. [PubMed] [Google Scholar]
- 25.Mullins GM, Eggleston JC, Santos GW, Udvarhelyi GB. Infiltration of the cauda equina in lymphosarcoma. Johns Hopkins Med J. 1971;129:170–6. [PubMed] [Google Scholar]
- 26.Karp SJ, Souhami RL, Hoffbrand BI. Cauda equina compression--an uncommon presentation of diffuse lymphocytic lymphoma. J Neurol Neurosurg Psychiatry. 1984;47:653. doi: 10.1136/jnnp.47.6.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Simpson RK Jr, Goodman JC, Ehni G. Nasopharyngeal carcinoma metastatic to the cauda equina. Surg Neurol. 1986;26:306–10. doi: 10.1016/0090-3019(86)90168-0. [DOI] [PubMed] [Google Scholar]
- 28.Takahashi I, Isu T, Iwasaki Y, Akino M, Takahashi A, Abe H, Kitagawa M, Kojima H, Inoue K, Saitoh H. [Metastatic Grawitz’s tumor to the cauda equina: case report] . No Shinkei Geka. 1990;18:1157–60. [PubMed] [Google Scholar]
- 29.Cho DY, Wang YC, Chen JT. Intradural metastasis to the cauda equina from carcinoma of the anus. Spine. 1995;20:2341–4. doi: 10.1097/00007632-199511000-00014. [DOI] [PubMed] [Google Scholar]
- 30.Rivano C, Borzone M, Pesce C, Pisani R. Cauda equina metastasis from ovarian malignancy. Eur J Gynaecol Oncol. 1996;17:397–9. [PubMed] [Google Scholar]
- 31.Ito K, Miyahara T, Goto T, Horiuchi T, Sakai K, Hongo K. Solitary metastatic cauda equina tumor from breast cancer -case report- Neurol Med Chir (Tokyo) 2010;50:417–20. doi: 10.2176/nmc.50.417. [DOI] [PubMed] [Google Scholar]
- 32.Rao KC, Jhaveri HS, Gellad FE. Carcinoid tumor with intradural metastases. J Comput Tomogr. 1988;12:258–260. doi: 10.1016/0149-936x(88)90080-x. [DOI] [PubMed] [Google Scholar]


