Abstract
Objective: To describe a personalised lamellar keratoplasty (LK) associated with the keratopigmentation (KTP) technique for corneal leucoma among Asian patients. Methods: This report was a non-randomised, retrospective clinical study performed in 32 consecutive eyes of 32 patients to improve cosmetic appearance. Twenty-two patients underwent LK combined with KTP, either by intralamellar or superficial route. Ten patients underwent the single personalised keratopigmentation method. The subjective and objective cosmetic results, ocular irritation, colour fading, neovascularisation formation and incidence of immune rejection were evaluated until three years after surgery. Results: No complications occurred, and the corneal leucoma was successfully stained with India ink in all 32 patients. Most of the patients showed good cosmetic appearance. Pain, conjunctival congestion, corneal edema and foreign body sensation disappeared gradually within two to three weeks after surgery in all patients. Graft swelling, non-healing, or detaching was not observed during follow-up. However, two patients had slight opacity three years after LK. Colour fading was observed in one patient who underwent intralamellar corneal staining 10 months after surgery. Re-staining was performed. Conclusion: KTP combined with personalised LK is an effective personalised technique that presents long-standing colour staining and good cosmetic efficacy.
Keywords: Lamellar keratoplasty, keratopigmentation, corneal leucoma, partial lamellar keratoplasty
Introduction
Corneal leucoma frequently occurs in keratitis and corneal wound because of multiple factors, such as physical, chemical and congenital [1]. Corneal opacity tends to result in cosmetic problems. If the scar is located in the visual axis area, it can cause visual loss and even functional blindness. The treatments for this condition include functional and cosmetic approaches [2]. Corneal transplantation, such as penetrating keratoplasty (PK) and lamellar keratoplasty (LK), is an excellent treatment for corneal macula or for leucoma patients who want to rehabilitate their visual acuity. However, after corneal transplantation, many people encounter graft rejection and chronic endothelial cell loss [3]. Keratopigmentation (KTP) has been used for centuries for cosmetic purposes when visual reconstruction is ineffective or is not chosen as an option. Galen (131-201 A.D.) first used copper sulphate to colour the corneal leucoma [4-6]. Later on, more chemical substances, such as India ink, have been used by surgeons to shade the scars in corneal leucoma patients. Cosmetic contact lenses are known to be the most commonly used method to improve aesthetic appearance [7-9]. However, people may be intolerant to wearing contact lenses, refuse to have the prosthesis for psychological reasons, or develop chronic inflammation and infection [10].
Using KTP for cosmetic purposes is a good choice for patients who are intolerant to wearing or are unwilling to try contact lenses. Several cases using KTP for cosmetic purposes among leucoma patients have been reported [11,12]. However, for patients whose corneal surface is unstable, such as corneal surfaces with angiogenesis, epithelial recurrent erosion and irregular surface, this method is not appropriate because of the surgical challenge it presents and the many complications it can cause, including pigment fading and recurrent erosion, among others. Thus, we introduced a new method that combines KTP with LK that is likely to obtain better cosmetic efficacy. We developed a personalised, safe, durable and cosmetic surgical LK technique combined with KTP especially suitable for Asians. We used India ink as the pigment for the KTP surgery either through the intralamellar corneal staining (ICS) or superficial corneal staining (SCS) route [13]. We studied the cosmetic effect of KTP with and without the LK technique in treating cornea leucoma patients. We evaluated the postoperative ocular discomfort and/or pain, medium-term durability, patients’ subjective satisfaction and objective cosmetic results.
Materials and methods
Patients
The Institutional Review Board of Tongji Eye Institute and the Research Ethics Committee of the University approved of this retrospective, non-randomised, non-comparative clinical case series. The tenets of the Declaration of Helsinki were followed in the investigation. Corneal leucoma was diagnosed on the basis of the slit-lamp microscope findings. Before the surgery, visual quality, intraocular pressure, corneal topography, anterior segment optic coherence tomography (AS-OCT) and ocular B scan were conducted to estimate the overall corneal topography, which could help to safely prepare the lamellar pocket. The surgical indications of the study were patients who have no light perception or low vision with no possibility of visual recovery, those who have a functional eye with corneal opacity located in the non-optical axis area, and those who are intolerant to wearing coloured contact lenses and refuse corneal prosthesis implantation. Patients with persistent corneal edema secondary to the corneal endothelial failure, neurotrophic corneal erosions and intractable glaucoma were excluded from the study. Thirty-two patients (32 eyes) were included in this study conducted from January 1, 2010 to April 30, 2011 (Table 1). Thirty patients were men (93.75%) and two were women (6.25%). The mean age was 21.6±8.4 years (range, 10-40 years old).
Table 1.
Summary of clinical data of 32 patients
| Patient | Sex | Age | Clinical diagnosis | Number of years | Visual acuity (pre/post) | Method of corneal tattooings | Complications |
|---|---|---|---|---|---|---|---|
| 1 | M | 27 | Penetrating injury, Strabismus | 19 | NLP/NLP | LK+ICS, Squint surgery | none |
| 2 | M | 30 | Injured by a stick, Iridodialysis, Cataract | 20 | LP/LP | LK+ICS, Cataract extraction and Coreoplasty | none |
| 3 | M | 34 | Perforating injury, Aphakia, Disuse exotropia | 29 | 0.01/LP | SCS, Squint surgery | none |
| 4 | M | 27 | Perforating injury, Atretopsia, Anterior synechia | 16 | LP/LP | ICS | none |
| 5 | M | 26 | Perforating injury, LK state | 10 | 0.2/0.2 | ICS | none |
| 6 | M | 44 | Perforating injury | 22 | NLP/NLP | ICS | none |
| 7 | F | 57 | corneal ulcer in childhood | 20 | FC/0.01 | LK+ICS | none |
| 8 | M | 45 | Perforating injury | 40 | 0.1/0.1 | SCS | none |
| 9 | M | 36 | Perforating injury, Iridodialysis, Cataract | 18 | NLP/LP | LK+SCS, Coreoplasty, Phaco+IOL | none |
| 10 | M | 25 | Alkali burn, Cataract | 12 | NLP/NLP | LK+ICS, Phaco+IOL | none |
| 11 | M | 44 | Penetrating injury | 23 | NLP/LP | LK+ICS | none |
| 12 | M | 47 | Perforating injury | 11 | LP/0.02 | LK+SCS | none |
| 13 | M | 53 | Perforating injury, Cataract | 20 | 0.1/0.2 | LK+ICS, Phaco+IOL | none |
| 14 | M | 39 | Herpes simplex keratitis | 10 | 0.2/0.2 | SCS | none |
| 15 | M | 52 | Penetrating injury | 32 | NLP/LP | LK+ICS | none |
| 16 | M | 28 | Congenital corneal leucoma | 28 | 0.01/0.02 | LK+ICS | none |
| 17 | M | 31 | Perforating injury | 16 | 0.01/0.01 | ICS | none |
| 18 | F | 44 | Herpes simplex keratitis | 10 | NLP/NLP | LK+ICS | none |
| 19 | M | 46 | Perforating injury | 23 | 0.01/0.01 | ICS | none |
| 20 | M | 50 | Injured by a stick, Strabismus | 40 | NLP/NLP | LK+SCS, Squint surgery | none |
| 21 | M | 53 | Corneal ulcer | 12 | LP/LP | LK+ICS | none |
| 22 | M | 62 | Perforating injury, Cataract | 32 | NLP/LP | ICS, Phaco+IOL | none |
| 23 | M | 41 | Perforating injury | 20 | NLP/NLP | LK+SCS | none |
| 24 | M | 50 | Perforating injury | 15 | NLP/NLP | LK+ICS | none |
| 25 | M | 28 | Perforating injury | 16 | NLP/NLP | LK+SCS | none |
| 26 | M | 45 | Herpes simplex keratitis | 27 | LP/0.02 | LK+ICS | none |
| 27 | M | 37 | corneal ulcer | 23 | 0.01/0.01 | LK+SCS | none |
| 28 | M | 36 | Perforating injury | 14 | LP/0.02 | LK+ICS | none |
| 29 | M | 55 | Perforating injury, Cataract | 28 | 0.02/0.04 | SCS, Phaco+IOL | none |
| 30 | M | 45 | Fungal corneal ulcer | 24 | HM/0.02 | LK+SCS | none |
| 31 | M | 33 | Congenital corneal leucoma | 33 | LP/LP | LK+ICS | none |
| 32 | M | 45 | Keratitis | 28 | 0.01/0.01 | LK+SCS | none |
*M, Male; F, Female; NLP, No light perception; LP, light perception; FC, finger count; HM, hand motion.
Surgical technique
The surgery was performed by a single surgeon (Dr Yanlong Bi). After retrobulbar anaesthesia (5 mL 2% lidocaine and 0.5% L-bupivacaine combined with one drop of 0.1% epinephrine), the lamellar pocket and the LK were performed manually. The diameter and depth of each individual’s lamellar dissection were evaluated by slit-lamp microscope and AS-OCT (Carl ZeissMeditec, Germany) before the surgery. For the LK patients, donor tissue (we used glycerin-20°C cryopreserved corneas) was thawed and rehydrated in normal saline solution for 30 min. A personalised outline of the corneal leucoma area was carved first, and then a 1/3-4/5 thickness of the anterior corneal lamellar stroma was excised depending on the location of the neovascularisation if present. The corresponding thickness of the donor tissue was moulded to match the size and shape of the recipient bed. Interrupted 10-0 nylon sutures were applied, and the knots were buried.
KTP was performed using one of the two approaches described below (Figure 1). We used India ink (Intenze Products, USA) as the dyeing pigment. The ink was sterilised at 121°C for 15 min in a sterile glass bottle before use. We used two colours, nigger-brown and gloss black, to match the corresponding eyes. In the ICS route, an angled crescent iris restorer was used to make a dissection into the corneal stroma. The dissection was created at 1/5-1/2 depth of the cornea, depending on the plane of the opacity. India ink was smeared on the pocket by the same iris restorer. For LK patients, after the graft was sutured, the ink was smeared directly under the graft using the iris restorer. In the SCS route, micropunctures were made with a 23-gauge needle, which reached the stromal bed through the superficial layers. This manoeuvre was repeated until the staining achieved a satisfactory appearance. Unlike LK, the two KTP approaches generally do not need suturing. However, when the pocket is not closed sufficiently, suture is needed to prevent the ink from leaking. For the patients already suffering from corneal perforation, we made two unconnected pockets separately by using the central perforating banding to prevent the ink from leaking into the anterior chamber during or after the surgery. The central perforating band could be managed either by LK combined with ICS or by LK combined with SCS. Additional surgery, such as strabismus (two patients, 6.3%), cataract extraction (five patients, 15.6%) and coreoplasty (two patients, 6.3%), was performed when needed. In case of strabismus, adequate resection or recession of muscles was performed to correct the deviation of the angle. In case of white cataract, lens extraction or iridodialysis repair was performed to minimise the area of the corneal KTP. Patients wore bandage contact lenses immediately after surgery. The patients were given tobramycin dexamethasone eye drops (TobraDex, Alcon) for one week.
Figure 1.
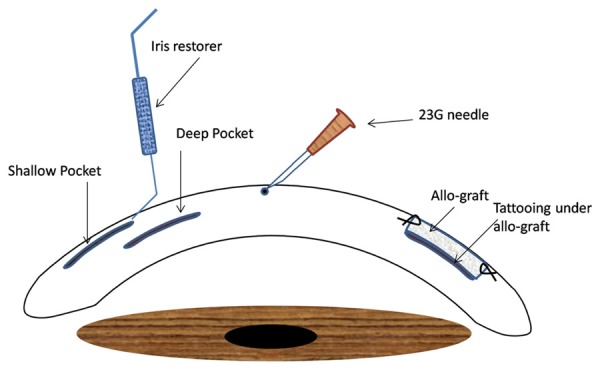
Schematic drawing of LK combined with KTP method.
Postoperative evaluation
Postoperatively, slip-lamp microscope examination was conducted to measure the changes in the graft, sutures, pigmentation fading and neovascularisation, among others. The satisfaction of the patients and observers was recorded using the protocol of Alio [12] at the time point of 36 months. The ocular situations of patients were quantified at the time point of one month: measuring pain (0-5), conjunctival congestion (0-5), foreign body sensation (0-5), corneal edema (0-5), colour fading (0-5) and intraocular irritation (0-5). The follow-up examinations were scheduled one to three days, one to three weeks and one to three months after surgery. The patients were followed-up every year until 36 months, postoperatively.
Results
No technical complications were encountered during surgery. No ink was found to leak during surgery or infiltrate into the anterior chamber after surgery. No anterior chamber inflammation occurred, and re-epithelisation was completed 5-14 days after surgery. Fourteen patients underwent LK combined with ICS (43.75%). Eight patients underwent LK combined with SCS (25%). Six patients underwent ICS only (18.75%), and four received SCS only (12.5%). Five patients used nigger-brown and 27 patients used gloss black to match their eyes.
Data on the 32 patients are shown in Table 1. Satisfaction evaluation is presented in Table 2. Patients’ ocular conditions one week after surgery are given in Table 3. No obvious colour fading and migration of the staining were observed for most patients, and all patients accepted the corneal appearance within 36 months after surgery (Figure 2). In one patient who underwent ICS, fading of colour was observed 38 months after surgery, and re-staining was easily performed by separating the original pocket. In two patients who underwent LK and KTP, partial graft opacification occurred 10 months after surgery, and they received re-staining after changing the graft. Graft-related complications were not observed within the next two years’ follow-up. As analysed in Table 2, the cosmetic results showed that 28 patients were given excellent assessment, and four patients were given cosmetically acceptable assessment. From the observers’ assessment, 6 patients were rated excellent, 26 good and 0 poor. All patients stated that they would repeat the surgery if needed.
Table 2.
Patients and observers’ evaluation of the cosmetic results
| Evaluation | Number of patients | |
|---|---|---|
| Poor: unacceptable esthetic aspect or very different to the fellow eye | 0 | |
| Observer | Good: symmetric aspect compared to the fellow eye and very cosmetically acceptable | 26 |
| Excellent: excellent cosmetically aspect and excellent symmetry compared to the fellow eye | 6 | |
| Unhappy or poor | 0 | |
| Patient | Happy or very good | 4 |
| Very happy or excellent | 28 |
Table 3.
Patients’ ocular situation one month after surgery
| Pain | Conjunctival congestion | Foreign body sensation | Corneal edema | Color fading | Intraocular irritation | |
|---|---|---|---|---|---|---|
| SCS | 4 | 3 | 4 | 4 | 4 | 4 |
| ICS | 1 | 1 | 1 | 1 | 1 | 1 |
| LK+KTP | 2 | 4 | 3 | 2 | 2 | 2 |
(*much to less: 5-0).
Figure 2.
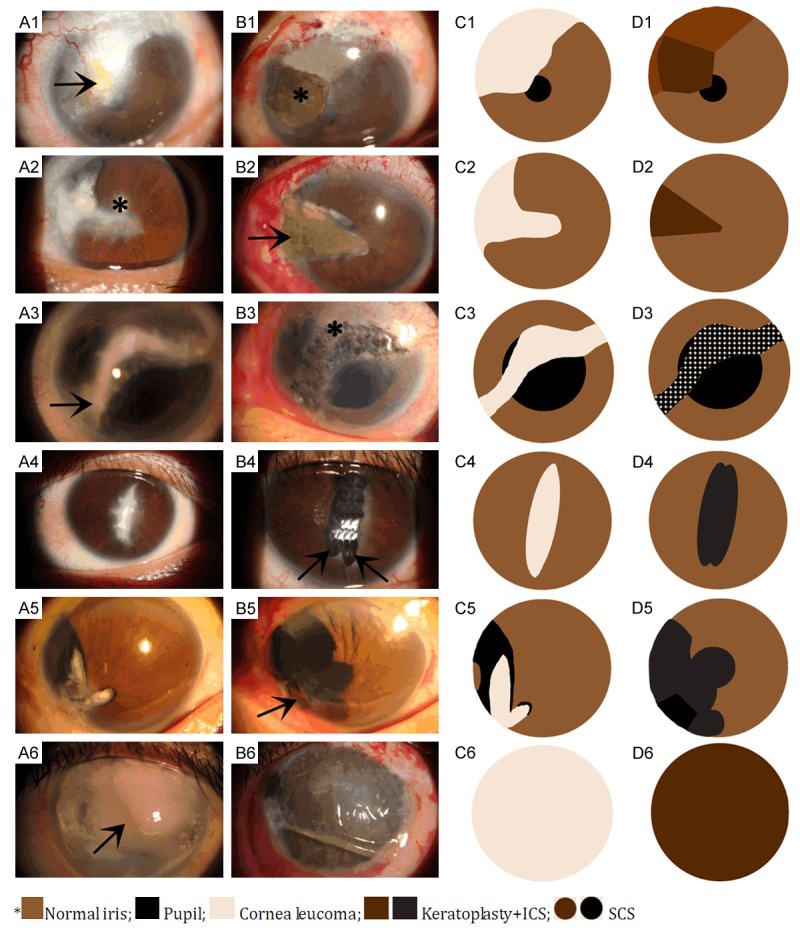
A 27-year-old man whose left eye suffered from penetrating injury 19 years ago and has no light perception. A1, C1. A full-thickness corneal amyloidosis (arrow) with a rough surface before surgery. B1, D1. Partial LK combined with ICS (asterisk) was performed. 3 years later, the graft was smooth and flat, and the pigmentation was homogeneous. A 30-year-old man whose left eye was injured by a stick for 20 years ago and has light perception only. A2, C2. A full-thickness old scar in the 9 o’clock position with superior iridodialysis and traumatic white cataract (asterisk). B2, D2. Partial LK with ICS (arrow), cataract extraction and iridodialysis repair were performed simultaneously. A 34-year-old man whose left cornea was perforated by fireworks 20 years ago and has no light Perception. A3, C3. In the weak junction of the penetrating scar site and the irregular leucoma (arrow). B3, D3. only SCS was performed (asterisk). Disuse exotropia was also corrected. A 27-year-old man whose left cornea was perforated by a pair of scissors 21 years ago and has light perception only. A4, C4. Corneal leucoma, atretopsia and anterior synechia were diagnosed. B4, D4. To obtain good resistance to the tension at the scar junction and to prevent the dye from infiltrating into the eye, we separated the scar into two parts along the centre of the scar and used ICS (arrow), respectively. The two parts were connected but not cut through. A 46-year-old man whose right cornea was perforated by a broken glass10 years ago and has light perception only. A5, C5. Cornea leucoma, traumatic cataract and iridodialysis were diagnosed. B5, D5. Local LK (arrow), two-pocket ICS, cataract extraction, IO L implantation and coreoplasty were performed simultaneously. Visual acuity at the end of follow-up was 0.5. A 44-year-old man whose right eye was injured by fireworks 22 years ago and has no light perception. A6, C6. Whole cornea leucoma and central band keratopathy (arrow) were diagnosed. B6, D6. We performed calcified plaque scraping, EDTA chelation and a single whole corneal pocket ICS with no sutures. A therapeutic contact lens was worn for two weeks.
Discussion
Patients with a sightless and cosmetically impaired eye usually require a safe, stable and effective cosmetic method to improve their appearance. However, because of the high risk factors and limitations of PK [3,14], ocular surface irritation of the cosmetic contact lenses [10] and psychological unwillingness to replace one’s own eyeball with an ocular prosthesis, the use of KTP with or without LK for cosmetic purposes is a good choice [15]. In this report, we presented an alternative personalised method to reconstruct the appearance of patients’ cornea. To the best of our knowledge, this report is the first to combine LK and KTP at the same time and to emphasise applying different staining methods in the same cornea.
In the past, the two popular staining techniques used were transepithelial intrastromal micropuncture and staining the anterior stroma after epithelial debridement [16,17]. Afterwards, a new technique called intrastromal lamellar pocket was used and proved to have a good outcome [11,12,18]. Alio described two different KTP approaches: ICS and SCS [12]. According to recent studies, the advantages of SCS are simple manipulation by surgeons and low risk of perforation. Its side effect is its ability to damage the corneal surface caused by the multiple iatrogenic punctures, which may cause persistent corneal surface instability, especially in cases with primary ocular surfaces or corneal diseases. ICS has more advantages than SCS in the terms of homogeneous pigmentation, faster surgery, faster postoperative recovery, less stimulating sensations and long-term pigmentation [19-22]. However, ICS is not suitable for patients whose scars are located superficially, are irregular, or located at the junction of an old corneal penetrating area. SCS may be more suitable for these patients [14]. For those who have a stable and transparent superficial corneal surface, both methods are suitable. However, both methods are not suitable for those with conditions of recurrent erosion and inflammation of the corneal epithelium, band keratopathy and corneal amyloidosis, among others, because they could cause further damage. In these cases, we recommend LK combined with ICS [14-16].
In some cases, such as a full-thickness scar occurring as a result of corneal perforation, we can make two pockets along the bilateral sides of the scar band, but the two pockets should not be connected to prevent the ink from infiltrating into the anterior chamber. Then, SCS can be performed but only on the middle scar band if this joint is thin and weak. Preoperatively, AS-OCT and the whole cornea thickness evaluation can help to ensure the safety of this procedure. If this scar joint is thick and has good resistance to tension, LK combined with ICS may be considered.
Concerning the pigment leakage or the colour changes, SCS is located superficially, and thus the mouth of the puncture cannot self-close during the early days after surgery. Tearing caused by the stimulating sensations on the corneal surface after surgery usually leads to early colour fading. For ICS, pigment diffusion usually occurs in the open mouth of the pocket. For patients treated by LK combined with ICS, pigment leakage could occur in the graft margin [12,23]. Fortunately, no obvious pigment fading occurred during our follow-up, and only one patient observed colour fading 38 months after surgery. Re-staining was easily performed through the original pocket.
Concerning the selection of colour dye, our cases are all Asian patients, and their irises are nigger-brown. We initially chose the dark-brown dye similar to the iris. However, the colour appeared slightly whitish under naked eye observation. Thus, we choose the pure black dye for the rest of the patients. Although the black colour could appear improperly under the slit-lamp microscope observation, all patients acquired a satisfactory cosmetic appearance under naked eye observation.
In sum, our study showed that the personalised LK combined with KTP provided an alternative treatment method for corneal leucoma patients. The method is safe, stable and reasonable, and it achieves satisfactory cosmetic results. Further studies are needed to determine the stability and toxicity of the pigment and its long-term effects on the graft.
Acknowledgements
Supported by the Natural Science Foundation of China (NSFC: 81470028, to Yanlong Bi) and the Program for New Century Excellent Talents in University, (NCET: 13-0420, to Yanlong Bi).
Disclosure of conflict of interest
None.
References
- 1.Glassy CM, Glassy MS, Aldasouqi S. Tattooing: medical uses and problems. Cleve Clin J Med. 2012;79:761–70. doi: 10.3949/ccjm.79a.12016. [DOI] [PubMed] [Google Scholar]
- 2.Chang KC, Kwon JW, Han YK, Wee WR, Lee JH. The epidemiology of cosmetic treatments for corneal opacities in a Korean population. Korean J Ophthalmol. 2010;24:148–54. doi: 10.3341/kjo.2010.24.3.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu SQ, Zhou P, Zhang B, Qiu WY, Yao YF. Long-term comparison of full-bed deep lamellar keratoplasty with penetrating keratoplasty in treating corneal leucoma caused by herpes simplex keratitis. Am J Ophthalmol. 2012;153:291–99. doi: 10.1016/j.ajo.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 4.Van der Velden, Samderubun EM, Kok JH. Dermatography as a modern treatment for coloring leucoma cornea. Cornea. 1994;13:349–353. doi: 10.1097/00003226-199407000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Holth S. Revival of Galen’s corneal staining with copper sulfate and tannine should be abandoned. Am J Ophthalmol. 1931;14:378–379. [Google Scholar]
- 6.Ziegler SL. Multicolor Tattooing of the Cornea. Trans Am Ophthalmol Soc. 1922;20:71–87. [PMC free article] [PubMed] [Google Scholar]
- 7.Hallock GG. Cosmetic trauma surgery. Plast Reconstr Surg. 1995;95:380–381. [PubMed] [Google Scholar]
- 8.Kuzan WM Jr. Plastic Surgery. J Am Coll Surg. 1999;188:171–77. doi: 10.1016/s1072-7515(98)00310-x. [DOI] [PubMed] [Google Scholar]
- 9.Hoeyberhs JL. Fortnightly review: Cosmetic surgery. BMJ. 1999;318:512–16. doi: 10.1136/bmj.318.7182.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Custer PL, Kennedy RH, Woog JJ, Kaltreider SA, Meyer DR. Orbital implants in enucleation surgery. A report by the American Academy of Ophthalmology. Ophthalmology. 2003;110:2054–61. doi: 10.1016/S0161-6420(03)00857-1. [DOI] [PubMed] [Google Scholar]
- 11.Fogla R, Gupta A, Indumathy TR. Microkeratome-assisted corneal tattooing: a case report. Cornea. 2010;29:446–8. doi: 10.1097/ICO.0b013e3181ae2560. [DOI] [PubMed] [Google Scholar]
- 12.Kim C, Kim KH, Han YK, Wee WR, Lee JH, Kwon JW. Five-year results of corneal tattooing for cosmetic repair in disfigured eyes. Cornea. 2011;30:1135–9. doi: 10.1097/ICO.0b013e3181f2391a. [DOI] [PubMed] [Google Scholar]
- 13.Alio JL, Sirerol B, Walewska-Szafran A, Miranda M. Corneal tattooing (keratopigmentation) with new mineral micronised pigments to restore cosmetic appearance in severely impaired eyes. Br J Ophthalmol. 2010;94:245–9. doi: 10.1136/bjo.2008.149435. [DOI] [PubMed] [Google Scholar]
- 14.Amesty MA, Alio JL, Rodriguez AE. Corneal tolerance to micronised mineral pigments for keratopigmentation. Br J Ophthalmol. 2014;98:1756–60. doi: 10.1136/bjophthalmol-2014-305611. [DOI] [PubMed] [Google Scholar]
- 15.Alio JL, Rodriguez AE, Toffaha BT. Keratopigmentation (corneal tattooing) for the management of visual disabilities of the eye related to iris defects. Br J Ophthalmol. 2011;95:1397–401. doi: 10.1136/bjophthalmol-2011-300170. [DOI] [PubMed] [Google Scholar]
- 16.Pitz S, Jahn R, Frisch L, Duis A, Pfeiffer N. Corneal tattooing: an alternative treatment for disfiguring corneal scars. Br J Ophthalmol. 2002;86:397–99. doi: 10.1136/bjo.86.4.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mannis MJ, Eghbali K, Schwab IR. Keratopigmentation: a review of corneal tattooing. Cornea. 1999;18:633–37. [PubMed] [Google Scholar]
- 18.Panda A, Mohan M, Chawdhary S. Corneal tattooing-experiences with “lamellar pocket procedure”. Indian J Ophthalmol. 1984;32:408–11. [PubMed] [Google Scholar]
- 19.Duggan JN, Nanavati BP. Tattooing of corneal opacity with gold and platinum chloride. Br J Ophthalmol. 1936;20:419–25. doi: 10.1136/bjo.20.7.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burris TE, Holmes-Higgin DK, Silvestrini TA. Lamellar intrastromal corneal tattoo for treating iris defects (artificial iris) Cornea. 1998;17:169–73. doi: 10.1097/00003226-199803000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Remky A, Redbrake C, Wenzel M. Intrastromal corneal tattooing for iris defects [letter] . J Cataract Refract Surg. 1998;24:1285–7. doi: 10.1016/s0886-3350(98)80215-0. [DOI] [PubMed] [Google Scholar]
- 22.Anastas CN, McGhee CN, Webber SK, Bryce IG. Corneal tattooing revisited: excimer laser in the treatment of unsightly leucomata. Aust N Z J Ophthalmol. 1995;23:227–30. doi: 10.1111/j.1442-9071.1995.tb00163.x. [DOI] [PubMed] [Google Scholar]
- 23.Hos D, Heindl LM, Bucher F, Cursiefen C. Novel lamellar, flap-based tattooing techniques for corneal opacities in scarred and vascularized blind eyes. Cornea. 2015;34:82–6. doi: 10.1097/ICO.0000000000000259. [DOI] [PubMed] [Google Scholar]


