Update to: European Journal of Human Genetics (2012) 20; doi:10.1038/ejhg.2011.237; published online 14 December 2011
1. Disease characteristics
1.1 Name of the Disease (Synonyms)
Alport syndrome.
1.2 OMIM# of the Disease
301050 (X-linked form), 203780 (autosomal recessive form), 104200 (autosomal dominant form).
1.3 Name of the Analysed Genes or DNA/Chromosome Segments
COL4A5, COL4A4, COL4A3.
1.4 OMIM# of the Gene(s)
303630 (COL4A5), 120131 (COL4A4), 120070 (COL4A3).
1.5 Mutational Spectrum
COL4A5: Missense variants (~45% of the variants, 85% of which are glycine substitutions in the conserved Gly-Xaa-Yaa repeat sequence in the collagenous domain of the alpha5(IV)-chain); splice site variants (~20%); frame shifts (small deletions, small insertions/duplications) (~20%); nonsense variants (~7%); large deletions and insertions/duplications (~12%) and other larger structural rearrangements (inversions and translocations). More than 1168 unique variants are known.
COL4A4: Missense variants (~50% of the variants, 75% of which are glycine substitutions in the conserved Gly-Xaa-Yaa repeat sequence in the collagenous domain of the alpha4(IV)-chain); frame shifts (small deletions, small insertions/duplications) (~27%); splice site variants (~13%); nonsense variants (~9%) and larger deletions. More than 268 unique variants are known.
COL4A3: Missense variants (~45% of the variants, 85% of which are glycine substitutions in the conserved Gly-Xaa-Yaa repeat sequence in the collagenous domain of the alpha3(IV)-chain); frame shifts (small deletions, small insertions/duplications) (~20%); nonsense variants (~15%); splice site variants (~15%) and larger deletions. More than 266 unique variants are known.
See:
HGMD (http://www.hgmd.org)
Alport LOVD databases (COL4A5, COL4A4, COL4A3)
(https://grenada.lumc.nl/LOVD2/COL4A/home.php?action=switch_db)
ARUP Alport (COL4A5) database (www.arup.utah.edu/database/ALPORT/ALPORT_welcome.php)
1.6 Analytical Methods
Targeted next generation sequencing. Direct sequencing of genomic exonic DNA, including flanking intronic sequences. Reverse transcriptase PCR analysis of mRNA extracted from cultured skin fibroblasts or hair roots for deep intronic variants causing RNA splicing aberrations (X-linked form). Multiplex ligation-dependent probe amplification (MLPA) for the detection of submicroscopic deletions and duplications. Conventional cytogenetic analysis for the detection of structural chromosome rearrangements.
1.7 Analytical Validation
Confirmation in an independent biological sample from the index case or an affected relative. Single exon deletions and duplications detected by MLPA should be confirmed with another technique.
1.8 Estimated Frequency of the Disease
(Incidence at birth (‘birth prevalence') or population prevalence)
The most widely used estimate of the prevalence of Alport syndrome is 1:5 000 based on the finding of about 300 cases in Utah and southern Idaho in a population of 1 500 000 people.1 The incidence of Alport syndrome was found to be 1:53 000 in Finland2 and 1:17 000 in southern Sweden.3 The inheritance is X-linked in ~85% of the families, autosomal recessive in ~15% and autosomal dominant in very few families.
1.9 If applicable, prevalence in the ethnic group of investigated person
Not applicable.
1.10 Diagnostic Setting

Comment: Genetic analysis is the diagnostic method of choice because it enables screening of symptomatic or at-risk family members, and may obviate the need for a kidney biopsy or in case electron microscopy of glomeruli is not available.
Genetic analysis is mainly used for confirmation of a clinical diagnosis and in relation to genetic counselling.
Prenatal diagnosis and pre-implantation genetic diagnosis are available for families with a known sequence variant.
2. Test characteristics
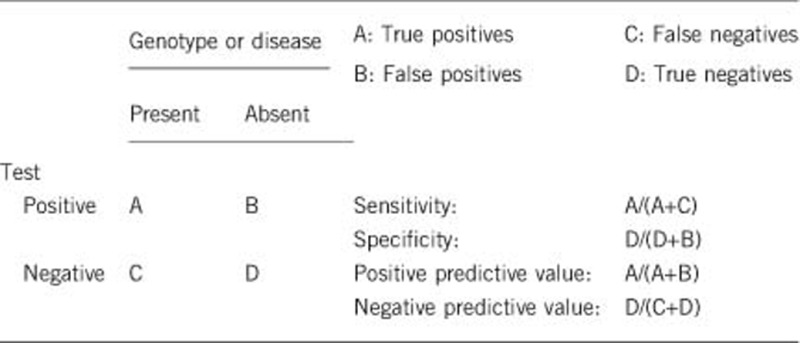
2.1 Analytical Sensitivity
(proportion of positive tests if the genotype is present)
COL4A5: Sanger sequencing of genomic DNA and MLPA: Above 99%.
COL4A3 and COL4A4: Sanger sequencing of genomic DNA and MLPA: Probably above 99%.
Targeted next generation sequencing of all the three genes (COL4A5, COL4A4 and COL4A3): Probably above 99%.
2.2 Analytical Specificity
(proportion of negative tests if the genotype is not present)
Sanger sequencing and MLPA of COL4A5: Above 99%.
Sanger sequencing and MLPA of COL4A3 and COL4A4: Probably above 99%.
Targeted next generation sequencing of all the three genes (COL4A5, COL4A4 and COL4A3): Probably above 99%.
2.3 Clinical Sensitivity
(proportion of positive tests if the disease is present)
The clinical sensitivity can be dependent on variable factors such as age or family history. In such cases a general statement should be given, even if a quantification can only be made case by case.
X-linked form: Highly dependent on fulfilment of the clinical criteria for Alport syndrome4 and may be supported by immunohistochemical findings in a kidney or skin biopsy. Above 80% in families fulfilling three or more diagnostic criteria. Higher in families with obvious X-linked inheritance, and higher in males than in females.5
Autosomal recessive form: Highly dependent on fulfilment of the clinical criteria for Alport syndrome4 and may be supported by immunohistochemical findings in a kidney or skin biopsy. Above 80% in families fulfilling three or more diagnostic criteria. Higher in families with consanguinity.
2.4 Clinical Specificity
(proportion of negative tests if the disease is not present) The clinical specificity can be dependent on variable factors such as age or family history. In such cases a general statement should be given, even if a quantification can only be made case by case.
X-linked form: Almost 100% in males by the age of 20 years.
Autosomal recessive form: Approaches 100% in males and females by the age of 20 years.
2.5 Positive clinical predictive value
(life time risk to develop the disease if the test is positive).
X-linked form: Almost 100% with respect to end-stage renal disease (ESRD) in males, and 30–40% in females. The risk for high-tone sensorineural hearing loss is 80–90% in males and 30% in females. The risk for ophthalmological manifestations is 30–50% for retinopathy and 15–30% for lenticonus in males, and lower in females.
Autosomal recessive form: Almost 100%. Heterozygotes may develop thin basement membrane disease/familial haematuria±proteinuria and sometimes renal impairment (OMIM #141200). The frequency of high-tone sensorineural hearing loss and ophthalmological manifestations are about the same as seen for males with X-linked form.
2.6 Negative clinical predictive value
(Probability of not developing the disease if the test is negative). Assume an increased risk based on family history for a non-affected person. Allelic and locus heterogeneity may need to be considered.
Index case in that family had been tested:
X-linked: Almost 100%.
Autosomal recessive: Almost 100%. Heterozygotes may develop thin basement membrane disease/benign familial haematuria (OMIM #141200)
Index case in that family had not been tested:
X-linked: Unknown, but probably high.
Autosomal recessive: Unknown, but probably high.
3. Clinical Utility
3.1 (Differential) diagnostics: The tested person is clinically affected
(To be answered if in 1.10 ‘A' was marked)
3.1.1 Can a diagnosis be made other than through a genetic test?
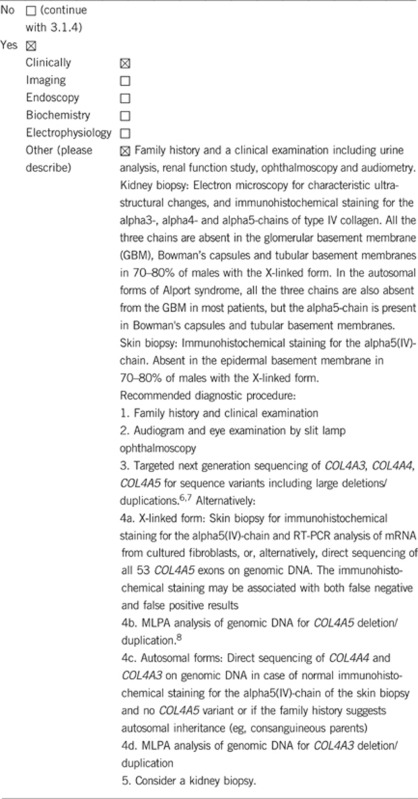
3.1.2 Describe the burden of alternative diagnostic methods to the patient
Kidney biopsy confers a risk to the patient (bleeding, infection and pain) and a skin biopsy leaves a tiny scar.
3.1.3 How is the cost effectiveness of alternative diagnostic methods to be judged?
Genetic testing is useful for confirming a clinical diagnosis, informing genetic counselling and facilitating prenatal diagnosis and pre-implantation genetic diagnosis. The three type IV collagen genes, COL4A5, COL4A3 and COL4A4, are very large genes with 48–53 exons and a coding sequence of more than 5000 bp. Targeted next generation sequencing will lower the costs and turn-around time, and will identify some large COL4A3 and COL4A4 rearrangements that are not detected by Sanger sequencing.
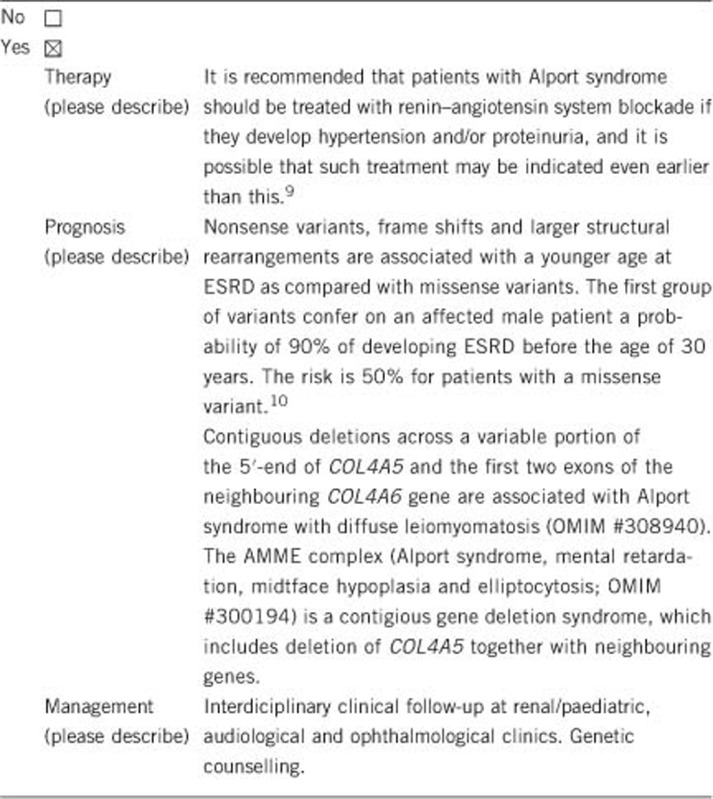
3.1.4 Will disease management be influenced by the result of a genetic test?
3.2 Predictive Setting: The tested person is clinically unaffected but carries an increased risk based on family history (To be answered if in 1.10 ‘B' was marked)
3.2.1 Will the result of a genetic test influence lifestyle and prevention?
If the test result is positive (please describe). If the test is positive, clinical follow-up and genetic counselling should be recommended. Careful management of blood pressure in a patient with a positive predictive test significantly prolongs the functioning life of a patient's native kidneys and postpones the need for renal replacement therapy. In addition, children should be referred for audiological examination to assess the need for a hearing aid.
Some patients may elect to have prenatal diagnosis or pre-implantation genetic diagnosis if they wish to avoid having an affected child.
If the test result is negative (please describe). This is not relevant if the test is negative for a known familial variant.
3.2.2 Which options in view of lifestyle and prevention does a person at risk have if no genetic test has been done (please describe)?
The same interdisciplinary surveillance programme comprising nephrological/paediatric, ophthalmological and audiological examination as for those with a positive genetic test. The frequency depends on the clinical findings.
3.3 Genetic risk assessment in family members of a diseased person
(To be answered if in 1.10 ‘C' was marked)
3.3.1 Does the result of a genetic test resolve the genetic situation in that family?
Yes. The risk assessment depends on the mode of inheritance; X-linked, autosomal recessive or dominant.
3.3.2 Can a genetic test in the index patient save genetic or other tests in family members?
Yes. If a pathogenic variant has been identified in the index patient, genetic counselling and testing for the familial variant could be offered to relatives at risk. If a relative tests negative, then none of their offspring are at risk and they will not need to be tested.
3.3.3 Does a positive genetic test result in the index patient enable a predictive test in a family member?
Yes. Carrier testing and presymptomatic testing in relatives will be possible.
3.4 Prenatal diagnosis
(To be answered if in 1.10 ‘D' was marked)
3.4.1 Does a positive genetic test result in the index patient enable a prenatal diagnosis?
Yes, prenatal and pre-implantation diagnostics can be performed in the family, if requested.
4. If applicable, further consequences of testing
Please assume that the result of a genetic test has no immediate medical consequences. Is there any evidence that a genetic test is nevertheless useful for the patient or his/her relatives? (Please describe)
Genetic testing can be useful for the patient/family in relation to genetic counselling. Genetic testing of relatives can also be relevant in relation to the selection of potential family donors for kidney transplantation. The affected mothers of males with X-linked Alport syndrome are usually advised not to donate a kidney because of their own risk of kidney failure.
Acknowledgments
This work was supported by EuroGentest2 (Unit 2:‘Genetic testing as part of health care'), a Coordination Action under FP7 (Grant Agreement Number 261469) and the European Society of Human Genetics.
The authors declare no conflict of interest.
References
- Hasstedt SJ, Atkin CL: X-linked inheritance of Alport syndrome: Family P revisited. Am J Hum Genet 1983; 35: 1241–1251. [PMC free article] [PubMed] [Google Scholar]
- Pajari H, Kaariainen H, Muhonen T, Koskimies O: Alport's syndrome in 78 patients: epidemiological and clinical study. Acta Paediatr 1996; 85: 1300–1306. [DOI] [PubMed] [Google Scholar]
- Persson U, Hertz JM, Wieslander J, Segelmark M: Alport syndrome in southern Sweden. Clin Nephrol 2005; 64: 85–90. [DOI] [PubMed] [Google Scholar]
- Flinter FA, Cameron JS, Chantler C, Houston I, Bobrow M: Genetics of classic Alport's syndrome. Lancet 1988; 2: 1005–1007. [DOI] [PubMed] [Google Scholar]
- Hanson H, Storey H, Pagan J, Flinter F: The value of clinical criteria in identifying patients with X-linked Alport syndrome. Clin J Am Soc Nephrol 2011; 6: 198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artuso R, Fallerini C, Dosa L et al: Advances in Alport syndrome diagnosis using next-generation sequencing. Eur J Hum Genet 2012; 20: 50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morinière V, Dahan K, Hilbert P et al: Improving Mutation Screening in Familial Hematuric Nephropathies through Next Generation Sequencing. J Am Soc Nephrol 2014, e-pub ahead of print 22 May 2014. [DOI] [PMC free article] [PubMed]
- Hertz JM, Juncker I, Marcussen N: MLPA and cDNA analysis improves COL4A4 mutation detection in X-linked Alport syndrome. Clin Genet 2008; 74: 522–530. [DOI] [PubMed] [Google Scholar]
- Savige J, Gregory M, Gross O, Kashtan C, Ding J, Flinter F: Expert guidelines for the management of Alport syndrome and thin basement membrane nephropathy. J Am Soc Nephrol 2013; 24: 364–375. [DOI] [PubMed] [Google Scholar]
- Jais JP, Knebelmann B, Giatras I et al: X-linked Alport syndrome: natural history in 195 families and genotype- phenotype correlations in males. J Am Soc Nephrol 2000; 11: 649–657. [DOI] [PubMed] [Google Scholar]


