Abstract
During the last decade, a significant diffusion of CTX-M-type extended-spectrum β-lactamases (ESBLs) was observed in commensal Escherichia coli from healthy children in the Bolivian Chaco region, with initial dissemination of CTX-M-2, which was then replaced by CTX-M-15 and CTX-M-65. In this work, we demonstrate that the widespread dissemination of CTX-M-65 observed in this context was related to the polyclonal spreading of an IncI1 sequence type 71 (ST71) epidemic plasmid lineage. The structure of the epidemic plasmid population was characterized by complete sequencing of four representatives and PCR mapping of the remainder (n = 16). Sequence analysis showed identical plasmid backbones (similar to that of the reference IncI1 plasmid, R64) and a multiresistance region (MRR), which underwent local microevolution. The MRR harbored genes responsible for resistance to β-lactams, aminoglycosides, florfenicol, and fosfomycin (with microevolution mainly consisting of deletion events of resistance modules). The blaCTX-M-65 module harbored by the IncI1 ST71 epidemic plasmid was apparently derived from IncN-type plasmids, likely via IS26-mediated mobilization. The plasmid could be transferred by conjugation to several different enterobacterial species (Escherichia coli, Cronobacter sakazakii, Enterobacter cloacae, Klebsiella oxytoca, Klebsiella pneumoniae, and Salmonella enterica) and was stably maintained without selective pressure in these species, with the exception of K. oxytoca and S. enterica. Fitness assays performed in E. coli recipients demonstrated that the presence of the epidemic plasmid was apparently not associated with a significant biological cost.
INTRODUCTION
CTX-M-type β-lactamases, first described in the late 1980s, have become the most common extended-spectrum β-lactamases (ESBLs) among Enterobacteriaceae worldwide (1, 2). Multiple sublineages (groups) of CTX-M-type ESBLs exist, and their dissemination has followed complex trajectories, depending on the spreading ability of the epidemic plasmids and bacterial clones with which blaCTX-M genes have become associated (1). Paradigmatic examples are the dissemination of blaCTX-M-15, mediated by IncFII and IncX plasmids associated with the Escherichia coli sequence type 131 (ST131) clone (3, 4); the dissemination of blaCTX-M-14 in Spain and the United Kingdom, mediated by IncK plasmids (5–8); and the dissemination of blaCTX-M-65 in China, mediated by F33:A-:B- plasmids (9).
In South America, members of the CTX-M-2 group emerged first and underwent wide dissemination during the 1990s (1, 10–12). Subsequently, members of the CTX-M-1 group (mostly CTX-M-15) and of the CTX-M-9 group have also disseminated in the area, outnumbering and replacing CTX-M-2 (13–18).
A similar epidemiological evolution was also observed in the Bolivian Chaco region, where we have been monitoring the evolution of antibiotic resistance among commensal E. coli isolates during the past 2 decades (from 1992 to 2011) (19–21). In that area, CTX-M-type ESBLs were first detected in 2002 and thereafter underwent a remarkable dissemination. Population analysis of CTX-M producers revealed that the early dissemination of these enzymes in the Bolivian Chaco region was mostly due to the dissemination of closely related IncA/C plasmids encoding CTX-M-2 group enzymes (CTX-M-2 and CTX-M-56) among different clones, with a minor contribution from clonal expansion of some CTX-M-15-producing strains (19, 20). In the most recent survey, carried out in 2011, almost complete disappearance of CTX-M-2 group variants was observed, along with further dissemination of CTX-M-15 and the emergence and remarkable spreading of CTX-M-9 group enzymes (CTX-M-65 and CTX-M-14), which were absent in the previous surveys. In particular, CTX-M-15 and CTX-M-65 were found to be largely dominant among CTX-M-producing E. coli isolates (21).
In this work, we found that the dissemination of CTX-M-65 observed in the area was entirely due to the polyclonal spreading of an IncI1 ST71 epidemic plasmid lineage. The plasmid structure was characterized, and transferability to other enterobacterial species and the plasmid-associated biological burden were also investigated.
(These results were presented in part at the 52nd Interscience Conference on Antimicrobial Agents and Chemotherapy, 9 to 12 September 2012, San Francisco, CA.)
MATERIALS AND METHODS
Bacterial isolates.
All the CTX-M-65-encoding E. coli isolates (n = 20) collected during the 2011 survey were included in this study (21). They were collected from three different urban areas and belonged to diverse phylogroups and randomly amplified polymorphic DNA (RAPD) types (Table 1). E. coli DH5α was used as the recipient in transformation experiments (20). Conjugation experiments were performed with 11 reference enterobacterial strains (E. coli MKD-135 [22], E. coli MG1655, Citrobacter freundii CCUG 418T, Cronobacter sakazakii ATCC 29544T, Enterobacter cloacae CIP 6085T, Klebsiella oxytoca CCUG 15717T, Klebsiella pneumoniae ATCC 13883T, Proteus mirabilis CCUG 26767T, Providencia stuartii ATCC 29914T, Serratia marcescens CCUG 1647T, and Salmonella enterica serovar Typhimurium LT2) and with three wild-type pansusceptible E. coli strains collected from the intestinal microbiota of healthy individuals and belonging to phylogenetic groups A (E. coli ER-A), B1 (E. coli ER-B1), and D (E. coli ER-D) (see Table S1 in the supplemental material).
TABLE 1.
Features of the 20 IncI1 CTX-M-65-encoding E. coli isolates
| Isolate | Origin | Phylogenetic groupb | RAPD typeb | Plasmid features |
||
|---|---|---|---|---|---|---|
| Resistance traits cotransferred with blaCTX-M-65 | pMLSTc | MRR profile | ||||
| C271a | Camiri | D | 27 | CHL/GEN/FOS | ST71 | a |
| C175 | Camiri | A | 15 | CHL/GEN/FOS | ND | a |
| V341 | Villa Montes | A | 17 | CHL/GEN/FOS | ND | a |
| V428 | Villa Montes | B1 | 22 | CHL/GEN/FOS | ND | a |
| C187 | Camiri | D | 27 | CHL/GEN/FOS | ND | a |
| M105a | Monteagudo | B1 | 23 | CHL/GEN | ST71 | b |
| V439 | Villa Montes | A | 19 | CHL/GEN | ST71 | b |
| M57 | Monteagudo | A | 20 | CHL/GEN | ST71 | b |
| C203 | Camiri | A | 16 | CHL/GEN | ST71 | b |
| M5 | Monteagudo | B1 | 26 | CHL/GEN | ND | b |
| M64 | Monteagudo | A | 21 | CHL/GEN/FOS | ND | c |
| V470 | Villa Montes | B1 | 22 | CHL/GEN/FOS | ST71 | c |
| C318 | Camiri | D | 28 | CHL/GEN/FOS | ND | c |
| V407 | Villa Montes | A | 18 | CHL/GEN/FOS | ST71 | d |
| C220 | Camiri | B1 | 24 | CHL/GEN/FOS | ST71 | e |
| C320 | Camiri | B1 | 24 | CHL/GEN/FOS | ND | e |
| M120 | Monteagudo | B1 | 22 | CHL/GEN | ST71 | f |
| V408a | Villa Montes | B1 | 22 | FOS | ST71 | g |
| C193a | Camiri | B1 | 23 | CHL/GEN/FOS | ST71 | h |
| V472 | Villa Montes | B1 | 25 | ST71 | i | |
Preliminary plasmid characterization.
CTX-M-65-encoding plasmids were transferred by electroporation into E. coli DH5α, using Mueller-Hinton agar (MHA) (Difco Laboratories, Detroit, MI) plates containing cefotaxime (2 μg/ml; Sigma-Aldrich, St. Louis, MO) for selection of transformants. The presence of blaCTX-M-65 in the transformants was always confirmed by PCR, as previously described (21). After being transferred, CTX-M-65-encoding plasmids were characterized by PCR-based replicon typing (23), followed by plasmid multilocus sequence typing (pMLST) (24; http://pubmlst.org/plasmid/).
In vitro susceptibility testing.
The antimicrobial susceptibility of E. coli transformants with CTX-M-65-encoding plasmids was determined by the disk diffusion method according to Clinical and Laboratory Standards Institute (CLSI) guidelines (25, 26). The antibiotic disks were from Oxoid (Milan, Italy). The following antibiotics were tested: tetracycline (TET), chloramphenicol (CHL), amikacin (AMK), gentamicin (GEN), kanamycin (KAN), streptomycin (STR), trimethoprim-sulfamethoxazole (SXT), and fosfomycin (FOS). E. coli ATCC 25922 was used for quality control purposes.
Plasmid characterization by sequencing and PCR mapping.
Complete sequences of four plasmids were obtained by pyrosequencing using the Roche 454 GS Junior System (Roche 454⃥Life Sciences, Basel, Switzerland) (plasmids pC271, pC193, and pV408) or a MiSeq Illumina platform (Illumina Inc., San Diego, CA, USA) (plasmid pM105). The Newbler software 2.5 (Roche) and ABySS 1.5 (27), respectively, were used to assemble the raw sequence data obtained with the two systems. Gaps were closed by a PCR-based strategy, and annotation was manually performed using the IncI1 plasmid R64 (AP005147) as a reference (28). The assembly of the shufflon regions was verified by PCR to exclude assembly artifacts and to verify the presence or absence of specific segments. The most prevalent orientation of the shufflon segments, determined by read coverage, was reported in the deposited sequences. Physical maps were generated using EasyFig software (29).
PCR mapping of the multiresistance region (MRR) of the IncI1 plasmids was carried out using the scheme and primers reported in Table S2 and Fig. S1 in the supplemental material.
Conjugation and stability experiments.
Conjugal transfer of pC193 (a representative of the IncI1 CTX-M-65-encoding plasmids) into E. coli MKD-135 (argH rpoB18 rpoB19 recA rpsL) (22) was assayed on MHA plates at 37°C, using cefotaxime (2 μg/ml) and rifampin (400 μg/ml) (Sigma-Aldrich) for selection of transconjugants, as previously described (20). Conjugal transfer of pC193 into the other enterobacterial hosts was investigated under the same experimental conditions, using E. coli MKD-135(pC193) as the donor and MacConkey agar (Oxoid) plus cefotaxime (10 μg/ml) and chloramphenicol (50 μg/ml) (Sigma-Aldrich) for selection of transconjugants. This donor was used because it is not able to grow on MacConkey medium, a feature not previously reported that we have noted while working with the strain and likely due to a defective bile salts efflux system (30). Chloramphenicol was used as an additional selective agent for pC193 to facilitate identification of transconjugants obtained with recipients of AmpC-producing species. Transconjugants were always investigated by PCR to confirm the presence of blaCTX-M-65. The detection sensitivity of the mating assay was ≥1 × 10−8 transconjugant/recipient.
For investigating plasmid stability, all transconjugants were maintained for 4 days (about 40 generations) in daily refreshed (100-fold dilution) Luria-Bertani (LB) broth without antibiotic selection, and the rate of pC193-positive cells was determined every 24 h by replica plating of at least 100 colonies onto LB agar plates plus cefotaxime (10 μg/ml) and chloramphenicol (50 μg/ml).
Growth curves and competition experiments.
The growth kinetics of E. coli MG1655 and E. coli ER-B1, with or without plasmid pC193 or pV38-8 (an epidemic IncA/C CTX-M-2-encoding plasmid previously disseminated in the study setting [19]), were determined in triplicate, using Mueller-Hinton broth (MHB) (Becton Dickinson, Sparks, MD, USA) inoculated with 5 × 107 CFU/ml (30 ml in 250-ml flasks), at 37°C and 200 rpm. Competition experiments were carried out with E. coli MG1655 harboring pC193 and E. coli MG1655 harboring pV38-8 under three different conditions: absence of antibiotic selection and cefotaxime at 0.5 μg/ml (a concentration half of the susceptibility breakpoint) and at 8 μg/ml (a concentration 2 times the resistance breakpoint). The competition mixtures were made of 5 ml of prewarmed MHB (with or without antibiotic) inoculated with 1 × 107 CFU/ml of each strain. The cultures were incubated at 37°C and 200 rpm and diluted daily 1:100 in fresh prewarmed broth for up to 16 days. The ratio of cells harboring pC193, pV38-8, or both plasmids was determined at different times (time zero and days 1, 3, 8, and 16) by plating appropriate dilutions onto MHA plus 50 μg/ml chloramphenicol (a selection marker for pC193), 50 μg/ml kanamycin (a selection marker for pV38-8), or both antibiotics. Colonies grown on MHA containing chloramphenicol and kanamycin were confirmed to carry both plasmids by analysis of E. coli DH5α transformants, obtained using plasmid DNA preparations from representative colonies selected at day 16. All experiments were performed in triplicate.
Nucleotide sequence accession numbers.
The complete nucleotide sequences of pC271, pC193, pV408, and pM105 and partial sequences of pC320 and pV470 have been deposited under GenBank\EMBL accession no. LN735561, LN735558, LN735560, LN735559, LN864415, and LN864416, respectively.
RESULTS
Identification of an IncI1 ST71 plasmid lineage responsible for CTX-M-65 dissemination in the study area.
All (n = 20) the CTX-M-65-positive E. coli isolates collected in the Bolivian Chaco region during the survey carried out in 2011 (21) were investigated for the genetic context of blaCTX-M-65. The isolates were from different urban areas and belonged to diverse phylogroups (A, B1, and D) and RAPD types (n = 14), representing a polyclonal population (Table 1).
Transfer of blaCTX-M-65 into E. coli DH5α by electrotransformation was successful with all isolates, and replicon typing assigned all the transferred CTX-M-65-encoding plasmids to the IncI1 family. MLST analysis, performed with selected plasmids representative of CTX-M-65-encoding plasmids from diverse phylogroups from each urban area (C203, V439, M57, V408, M105, C193, and C271), assigned all of them to ST71 (Table 1). Altogether, these results suggested that the dissemination of blaCTX-M-65 observed in the study area had been mediated by the dissemination of an IncI1 ST71 epidemic plasmid lineage.
Analysis of antimicrobial susceptibility profiles of DH5α transformants carrying the CTX-M-65-encoding plasmids revealed cotransfer of resistance determinants to chloramphenicol, gentamicin, and fosfomycin in a variable number of cases (90%, 90%, and 65%, respectively) (Table 1), suggesting some heterogeneity of the resistance determinants carried by the circulating plasmids of the lineage.
Characterization of the IncI1 plasmid lineage encoding CTX-M-65.
Comparative analysis of the 20 CTX-M-65-encoding IncI1 plasmids was performed by complete sequencing of four representatives and by a PCR-mapping approach targeting the MRR for characterization of the remainder.
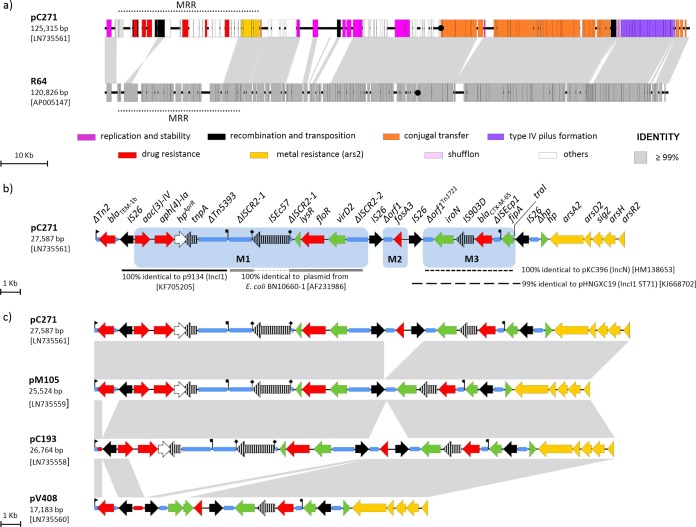
Complete sequencing was performed with three plasmids identified in E. coli isolates belonging to phylogroup B1 (i.e., the dominant phylogroup among CTX-M producers in the study setting) and collected from the three different urban areas (V408, M105, and C193) and with a fourth plasmid from an E. coli isolate of a different phylogroup (C271) (Table 1). The four plasmids ranged in size from 114,911 bp to 125,315 bp and consisted of (i) identical IncI1 scaffolds (100% nucleotide identity, considering shufflon segments in the same orientation), and (ii) an MRR that was conserved overall but also showed some differences among the four plasmids (Fig. 1).
FIG 1.
(a) Sequence comparison of plasmids pC271 and R64. Homologous segments generated by a BLASTn comparison (≥99% identity) are shown as gray blocks. Genes are represented by bars and in pC271 are classified by function into different groups, as detailed below the diagram. The location of oriT is represented by a black dot. The MRRs of pC271 and of R64 are indicated by dotted lines. (b) Structure of the MRR of pC271 (27,587 bp). Open reading frames (ORFs) are represented by thick arrows, with arrowheads showing the direction of transcription. Genes encoding resistance to antibiotics and metals are represented in red and yellow, respectively; nonfunctional ORFs (deleted or disrupted) and mobile elements are represented by pale-blue thin arrows; ORFs with known and unknown functions are drawn in green and white, respectively; insertion sequences and transposases are hatched, with the exception of IS26, shown in solid black. Triangular and square flags show inverted repeats (IRs) of Tn2 and Tn5393, respectively; the semicircular flag shows a partial IR of a Tn1721-like transposon; ISEc57 direct repeats (CACA) are indicated by diamond flags. A more detailed description of the MRR of pC271 can be found in Fig. S1 in the supplemental material. (c) Comparison of the MRRs of the four sequenced plasmids. Homologous regions (≥99% identity) are shown as gray blocks connected across lanes. The other features are as in panel b.
The scaffold region was similar to that of the IncI1 reference plasmid, R64 (28) (GenBank⃥EMBL accession no. AP005147). Gene synteny was retained over 85% of the scaffold, with nucleotide sequence divergence of 1% due to several scattered single nucleotide polymorphisms. The other differences were related to the presence or absence of some genes involved in partitioning, conjugal transfer (e.g., the shufflon segments C and D of R64 were not present in the scaffold of the Bolivian IncI1 plasmids), or encoding of hypothetical proteins (Fig. 1a). Regarding addiction systems, the scaffold of the IncI1 ST71 plasmids harbored both VagC-VagD and PndA-PndC, similar to R64.
The MRR was located between the IncI1 replicon and the rfsF-resD system, a known hot spot for the insertion of accessory modules in IncI1 plasmids (31).
The MRR of pC271 was the largest and consisted of (i) a partially deleted Tn2 transposon (ΔTn2) carrying the blaTEM-1b gene; (ii) three resistance modules bounded by IS26 elements, labeled M1, M2, and M3; and (iii) an ars2 operon encoding arsenic resistance and identical to that found in the MRR of R64 (Fig. 1b). The M1 module carried resistance determinants to aminoglycosides [aac(3)-IV, aph(4)-Ia, and a putative gene for apramycin resistance] and florfenicol (floR), the M2 module carried the fosfomycin resistance gene fosA3 in an original arrangement (i.e., IS26-fosA3-504bp-IS26) compared to those previously described (32, 33), and the M3 module carried blaCTX-M-65 in its typical genetic context (ΔISEcp1-blaCTX-M-65-IS903D) (34–36). Although the assembly was original, each of these modules, or parts thereof, was identical to those found in other plasmids (Fig. 1b). Interestingly, sequence analysis suggested that the 4.7-kb region bounded by two IS26 elements and carrying blaCTX-M-65 (M3 module) could be derived from IncN plasmids related to pKC396 (34, 35), likely by IS26-mediated mobilization (37). The presence of a remnant of the traI gene with the highest identity to several IncN plasmids and no homology with the IncI1 traI gene further supported this hypothesis (Fig. 1b). In addition, an identical module with IS26 flanking elements was recently described in a partially sequenced ST71 IncI1 CTX-M-65-encoding plasmid (pHNGXC19) from an E. coli strain of animal origin isolated in China (Fig. 1b) (36).
Compared to that of pC271, the MRRs of the other three sequenced plasmids differed by deletions involving blaTEM-1b (in pC193); the IS26-fosA3-504bp-IS26 module (in pM105); or a large fragment comprising aac(3)-IV, aph(4)-Ia, and floR (in pV408). In addition, the last plasmid harbored fosA3 in a module 1,254 bp longer than that of pC271 (labeled as IS26-fosA3-1758bp-IS26, according to the fosA3 gene orientation) and identical to that found in plasmid p06607 (Fig. 1c) (32).
PCR mapping of the MRRs of the remaining 16 plasmids confirmed their location between the IncI1 replicon and the ars2 operon, with the exception of one case (pV407) for which anchoring to the ars2 operon was not successful (suggesting the occurrence of either deletions or insertions at that level) (see Fig. S1 in the supplemental material). It also revealed a notable heterogeneity of the MRR (Table 1; see Fig. S1 in the supplemental material). Interestingly, the fosA3 module accounted for most of the observed heterogeneity, with three different arrangements represented by those found in pC271 (IS26-fosA3-504bp-IS26; n = 6), pM105 (absence of the module; n = 7), and pV408 (IS26-fosA3-1758bp-IS26; n = 7) (Fig. 1c; see Fig. S1 in the supplemental material).
MLST analysis, performed with five additional plasmids (pC220, pM120, pV407, pV470, and pV472), with the aim of typing at least one representative for each MRR profile, confirmed they belonged to the ST71 lineage (Table 1).
No specific association was found between MRR profiles and host strain features (e.g., phylogenetic group or RAPD type) (Table 1).
Transferability and stability of the CTX-M-65-encoding plasmid.
Plasmid pC193 was selected as the representative of the IncI1 ST71 CTX-M-65-encoding epidemic plasmid lineage for transferability and stability experiments, since it was completely sequenced and derived from an E. coli strain (C193) belonging to phylogroup B1.
Conjugal transfer of pC193 from E. coli C193 to E. coli MKD-135 was observed, although the conjugation frequency could not be calculated because of the recipient susceptibility to colicins produced by the donor (data not shown).
To further investigate the conjugation features of pC193, E. coli MKD-135(pC193) was used as the donor in mating experiments with a panel of 13 enterobacterial hosts, including 3 wild-type E. coli isolates belonging to phylogroups A, B1, and D and 10 reference strains of various species. Plasmid transfer was achieved at high frequency with all E. coli recipients and with C. sakazakii, E. cloacae, and S. Typhimurium (1 × 10−2 to 1 × 10−5 transconjugant/recipient) and at a lower frequency with Klebsiella spp. No transconjugants were obtained with C. freundii, S. marcescens, P. stuartii, and P. mirabilis (Table 2).
TABLE 2.
Conjugation and stability features of the IncI1 ST71 CTX-M-65-encoding plasmid pC193 in Enterobacteriaceae
| Recipient strain | Conjugation frequencya | % stabilityb |
|---|---|---|
| E. coli | ||
| MG1655 | 1 × 10−2 | 100 |
| ER-A | 1 × 10−2 | 100 |
| ER-B1 | 1.3 × 10−4 | 100 |
| ER-D | 1.1 × 10−5 | 100 |
| E. cloacae CIP 6085 | 1.3 × 10−4 | 100 |
| K. pneumoniae ATCC 13833 | 6 × 10−7 | 100 |
| K. oxytoca CCUG 15717 | 1.7 × 10−6 | 93 |
| C. freundii CCUG 418 | ||
| C. sakazaki ATCC 29544 | 7.7 × 10−3 | 100 |
| S. marcescens CCUG 1647 | ||
| P. stuartii ATCC 29914 | ||
| P. mirabilis CCUG 26726 | ||
| S. Typhimurium LT2 | 2.5 × 10−5 | 67 |
Calculated as the ratio of transconjugants to recipients.
Calculated as the ratio of IncI1 ST71 CTX-M-65-positive colonies to the total number of screened colonies at the end of the experiment.
Stability experiments, carried out by culturing transconjugants in the absence of antibiotic selective pressure for approximately 40 generations, demonstrated that pC193 was stably maintained in all tested recipients, with the exception of K. oxytoca and S. Typhimurium (Table 2).
Biological cost associated with CTX-M-encoding plasmids.
The biological cost associated with acquisition of plasmid pC193 was investigated using plasmid pV38-8 as a comparator. The latter was a representative of the CTX-M-2-encoding IncA/C epidemic plasmids responsible for the early emergence of CTX-M enzymes in the study setting but no longer present in 2011 (i.e., no IncA/C plasmids were detected in the only two CTX-M-2-encoding isolates from the 2011 survey [data not shown]) (21).
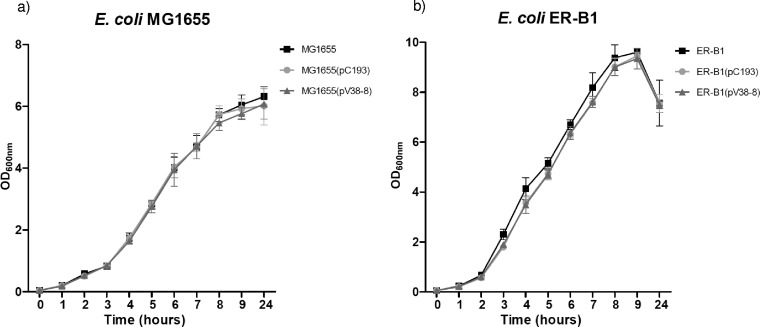
Growth of E. coli MG1655 and E. coli ER-B1 strains was substantially unaffected by the presence of either pC193 or pV38-8, demonstrating the lack of a major biological cost associated with acquisition of both plasmids (Fig. 2).
FIG 2.
Growth kinetics of E. coli recipients harboring pC193 (IncI1 CTX-M-65-encoding plasmid), pV38-8 (IncA/C CTX-M-2-encoding plasmid), or both plasmids. (a) E. coli MG1655. (b) E. coli ER-B1 (a wild-type isolate of phylogroup B1). The data are representative of three independent experiments. The error bars represent standard deviations.
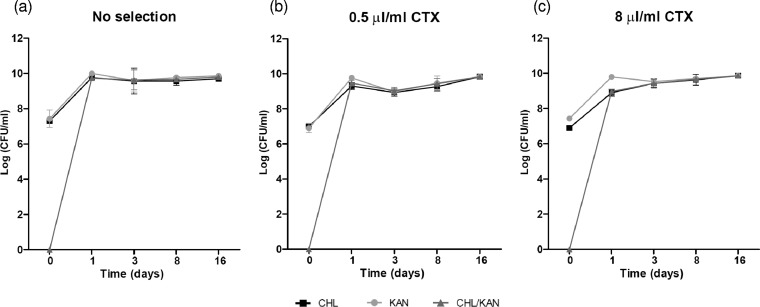
Consistent results were obtained in competition experiments performed with E. coli MG1655(pC193) versus E. coli MG1655(pV38-8), with no relative fitness cost observed under any of the three tested experimental conditions (absence of antibiotic, 0.5 μg/ml cefotaxime, and 8 μg/ml cefotaxime) (Fig. 3). In these competition experiments, conjugative plasmid transfer occurred efficiently and, after 3 days, almost all the E. coli cells were found to harbor both plasmids, which could then be stably maintained until the end of the experiment (16 days).
FIG 3.
Growth competition between E. coli MG1655(pC193) and E. coli MG1655(pV38-8) in the absence of antibiotic selective pressure (a), in the presence of 0.5 μg/ml cefotaxime (CTX) (b), and in the presence of 8 μg/ml cefotaxime (c). The data are representative of three independent experiments. The error bars represent standard deviations.
DISCUSSION
Since the early 2000s, CTX-M enzymes have emerged and disseminated worldwide, becoming the dominant ESBLs in Enterobacteriaceae in both hospital and community settings (1, 2). Dissemination of these resistance determinants has been sustained by different mechanisms, including the horizontal epidemic dissemination of transferable plasmids and the expansion of highly successful clones (1, 2).
In the present study, we found that the emergence and dissemination of CTX-M-65 recently observed in the intestinal microbiota of healthy children living in the Bolivian Chaco was due to the polyclonal spreading of an epidemic IncI1 plasmid belonging to ST71. Comparative analysis of the plasmid population, however, revealed several rearrangements in the MRR, suggesting that microevolution of these plasmids occurred during their dissemination. Interestingly, the blaCTX-M-65 module harbored by the IncI1 ST71 -type plasmids related to pKC396 (34, 35), most likely via IS26-mediated mobilization. The presence of a similar CTX-M-harboring module (IS903D-CTX-M-14-IS26) in the IncHI2 plasmid pSDB58 described in S. enterica serovar Indiana may further support this hypothesis (38). Altogether, these findings confirm the role of recombination events in the exchange of large modules containing clinically relevant resistance genes among different plasmid backbones (34, 39, 40).
Apart from the Bolivian region investigated in our work, consistent dissemination of CTX-M-65 has so far been limited to China and other Asiatic countries (i.e., Japan and Korea), where it is among the dominant CTX-M variants in enterobacteria of animal origin (36, 41–44). The reasons accounting for the peculiar CTX-M-65 epidemiology, characterized by the distribution in two distant geographical areas, remain unknown. Although the dissemination of blaCTX-M-65 in the Far East has mostly been associated with epidemic IncFII plasmids (33, 43), with no epidemic IncI1 CTX-M-65-encoding plasmids reported so far, some features might suggest that the epidemic IncI1 ST71 plasmids circulating in Bolivia could be linked to Asian countries through trade in animal-associated products (e.g., imported foods, feeds, or organic fertilizers). This hypothesis is supported by (i) the presence, in the epidemic IncI1 ST71 plasmid, of resistance determinants that are increasingly reported in enterobacterial isolates of animal origin in China (i.e., fosA3 and floR) (36, 45); (ii) the observation that a partially sequenced IncI1 ST71 CTX-M-65-encoding plasmid, harboring fosA3 (although in a different genetic environment), has been recently described in an E. coli isolate from poultry in China (36); (iii) the fact that China is one of Bolivia's largest sources of imports. However, further studies will be necessary to confirm this hypothesis.
A representative of the epidemic IncI1 ST71 CTX-M-65-encoding plasmid was able to be transferred by conjugation at high frequency between E. coli strains, and it could also be transferred to other enterobacterial species, including Klebsiella spp., E. cloacae, C. sakazakii and S. enterica. Once acquired, this epidemic plasmid could be stably maintained in the absence of antibiotic selection in most cases, and its presence was apparently not associated with any significant biological cost. Plasmid instability potentially leading to the loss of antibiotic resistance determinants other than those responsible for resistance to expanded-spectrum cephalosporins or chloramphenicol, was not specifically evaluated at this stage and represents a topic for future investigation. These findings were overall consistent with the epidemiological success of the CTX-M-65-encoding plasmid. On the other hand, competition experiments, carried out in an isogenic host background with the epidemic IncA/C CTX-M-2-encoding plasmid (previously disseminated in the same area), did not provide evidence explaining the change in the epidemiology of those plasmids (IncA/C CTX-M-2-encoding plasmid versus IncI1 CTX-M-65-encoding plasmid) observed in recent years in the study setting, and further investigations are therefore required.
Supplementary Material
ACKNOWLEDGMENTS
We thank Ana Liz Villagran, Yunni Lara, and Claudia Saavedra for their valuable support in laboratory activities.
The study was supported by the European Union Seventh Framework Programme (EvoTAR; HEALTH-F3-2011-2011-282004) and by grants from the Italian Ministry for Foreign Affairs (Fortalecimiento de la red de salud del Chaco Boliviano: una perspectiva comunitaria), the Ente Cassa di Risparmio di Firenze (Florence, Italy), and the Regione Toscana (Italy) (Toscana e Chaco, 25 anni di cooperazione sanitaria: un passo decisivo verso il contenimento della diffusione delle resistenze batteriche agli antibiotici).
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/AAC.00589-15.
REFERENCES
- 1.D'Andrea MM, Arena F, Pallecchi L, Rossolini GM. 2013. CTX-M-type β-lactamases: a successful story of antibiotic resistance. Int J Med Microbiol 303:305–317. doi: 10.1016/j.ijmm.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 2.Cantón R, González-Alba JM, Galán JC. 2012. CTX-M enzymes: origin and diffusion. Front Microbiol 3:110. doi: 10.3389/fmicb.2012.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coque TM, Novais A, Carattoli A, Poirel L, Pitout J, Peixe L, Baquero F, Cantón R, Nordmann P. 2008. Dissemination of clonally related Escherichia coli strains expressing extended-spectrum β-lactamase CTX-M-15. Emerg Infect Dis 14:195–200. doi: 10.3201/eid1402.070350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Partridge SR, Ellem JA, Tetu SG, Zong Z, Paulsen IT, Iredell JR. 2011. Complete sequence of pJIE143, a pir-type plasmid carrying ISEcp1-blaCTX-M-15 from an Escherichia coli ST131 isolate. Antimicrob Agents Chemother 55:5933–5935. doi: 10.1128/AAC.00639-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Valverde A, Cantón R, Garcillán-Barcia MP, Novais A, Galán JC, Alvarado A, de la Cruz F, Baquero F, Coque TM. 2009. Spread of blaCTX-M-14 is driven mainly by IncK plasmids disseminated among Escherichia coli phylogroups A, B1, and D in Spain. Antimicrob Agents Chemother 53:5204–5212. doi: 10.1128/AAC.01706-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cottell JL, Webber MA, Coldham NG, Taylor DL, Cerdeño-Tárraga AM, Hauser H, Thomson NR, Woodward MJ, Piddock LJ. 2011. Complete sequence and molecular epidemiology of IncK epidemic plasmid encoding blaCTX-M-14. Emerg Infect Dis 17:645–652. doi: 10.3201/eid1704.101009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dhanji H, Khan P, Cottell JL, Piddock LJ, Zhang J, Livermore DM, Woodford N. 2012. Dissemination of pCT-like IncK plasmids harboring CTX-M-14 extended-spectrum β-lactamase among clinical Escherichia coli isolates in the United Kingdom. Antimicrob Agents Chemother 56:3376–3377. doi: 10.1128/AAC.00313-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stokes MO, Cottell JL, Piddock LJ, Wu G, Wootton M, Mevius DJ, Randall LP, Teale CJ, Fielder MD, Coldham NG. 2012. Detection and characterization of pCT-like plasmid vectors for blaCTX-M-14 in Escherichia coli isolates from humans, turkeys and cattle in England and Wales. J Antimicrob Chemother 67:1639–1644. doi: 10.1093/jac/dks126. [DOI] [PubMed] [Google Scholar]
- 9.He L, Partridge SR, Yang X, Hou J, Deng Y, Yao Q, Zeng Z, Chen Z, Liu JH. 2013. Complete nucleotide sequence of pHN7A8, an F33:A-:B- type epidemic plasmid carrying blaCTX-M-65, fosA3 and rmtB from China. J Antimicrob Chemother 68:46–50. doi: 10.1093/jac/dks369. [DOI] [PubMed] [Google Scholar]
- 10.Radice M, Power P, Di Conza J, Gutkind G. 2002. Early dissemination of CTX-M-derived enzymes in South America. Antimicrob Agents Chemother 46:602–604. doi: 10.1128/AAC.46.2.602-604.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quinteros M, Radice M, Gardella N, Rodriguez MM, Costa N, Korbenfeld D, Couto E, Gutkind G, Microbiology Study Group. 2003. Extended-spectrum β-lactamases in Enterobacteriaceae in Buenos Aires, Argentina, public hospitals. Antimicrob Agents Chemother 47:2864–2867. doi: 10.1128/AAC.47.9.2864-2867.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Villegas MV, Kattan JN, Quinteros MG, Casellas JM. 2008. Prevalence of extended-spectrum β-lactamases in South America. Clin Microbiol Infect 14(Suppl 1):154–158. doi: 10.1111/j.1469-0691.2007.01869.x. [DOI] [PubMed] [Google Scholar]
- 13.Cergole-Novella MC, Guth BE, Castanheira M, Carmo MS, Pignatari AC. 2010. First description of blaCTX-M-14- and blaCTX-M-15-producing Escherichia coli isolates in Brazil. Microb Drug Resist 16:177–184. doi: 10.1089/mdr.2010.0008. [DOI] [PubMed] [Google Scholar]
- 14.Peirano G, Asensi MD, Pitondo-Silva A, Pitout JD. 2011. Molecular characteristics of extended-spectrum β-lactamase-producing Escherichia coli from Rio de Janeiro, Brazil. Clin Microbiol Infect 17:1039–1043. doi: 10.1111/j.1469-0691.2010.03440.x. [DOI] [PubMed] [Google Scholar]
- 15.Ruiz SJ, Montealegre MC, Ruiz-Garbajosa P, Correa A, Briceño DF, Martinez E, Rosso F, Muñoz M, Quinn JP, Cantón R, Villegas MV. 2011. First characterization of CTX-M-15-producing Escherichia coli ST131 and ST405 clones causing community-onset infections in South America. J Clin Microbiol 49:1993–1996. doi: 10.1128/JCM.00045-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tollentino FM, Polotto M, Nogueira ML, Lincopan N, Neves P, Mamizuka EM, Remeli GA, De Almeida MT, Rúbio FG, Nogueira MC. 2011. High prevalence of blaCTX-M extended spectrum β-lactamase genes in Klebsiella pneumoniae isolates from a tertiary care hospital: first report of blaSHV-12, blaSHV-31, blaSHV-38, and blaCTX-M-15 in Brazil. Microb Drug Resist 17:7–16. doi: 10.1089/mdr.2010.0055. [DOI] [PubMed] [Google Scholar]
- 17.Redondo C, Chalbaud A, Alonso G. 2013. Frequency and diversity of CTX-M enzymes among extended-spectrum β-lactamase-producing Enterobacteriaceae isolates from Caracas, Venezuela. Microb Drug Resist 19:42–47. doi: 10.1089/mdr.2012.0079. [DOI] [PubMed] [Google Scholar]
- 18.Sennati S, Santella G, Di Conza J, Pallecchi L, Pino M, Ghiglione B, Rossolini GM, Radice M, Gutkind G. 2012. Changing epidemiology of extended-spectrum β-lactamases in Argentina: emergence of CTX-M-15. Antimicrob Agents Chemother 56:6003–6005. doi: 10.1128/AAC.00745-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pallecchi L, Bartoloni A, Fiorelli C, Mantella A, Di Maggio T, Gamboa H, Gotuzzo E, Kronvall G, Paradisi F, Rossolini GM. 2007. Rapid dissemination and diversity of CTX-M extended-spectrum β-lactamase genes in commensal Escherichia coli isolates from healthy children from low-resource settings in Latin America. Antimicrob Agents Chemother 51:2720–2725. doi: 10.1128/AAC.00026-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pallecchi L, Malossi M, Mantella A, Gotuzzo E, Trigoso C, Bartoloni A, Paradisi F, Kronvall G, Rossolini GM. 2004. Detection of CTX-M-type β-lactamase genes in fecal Escherichia coli isolates from healthy children in Bolivia and Peru. Antimicrob Agents Chemother 48:4556–4561. doi: 10.1128/AAC.48.12.4556-4561.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bartoloni A, Pallecchi L, Riccobono E, Mantella A, Magnelli D, Di Maggio T, Villagran AL, Lara Y, Saavedra C, Strohmeyer M, Bartalesi F, Trigoso C, Rossolini GM. 2013. Relentless increase of resistance to fluoroquinolones and expanded-spectrum cephalosporins in Escherichia coli: 20 years of surveillance in resource-limited settings from Latin America. Clin Microbiol Infect 19:356–361. doi: 10.1111/j.1469-0691.2012.03807.x. [DOI] [PubMed] [Google Scholar]
- 22.Kholodii GY, Mindlin SZ, Bass IA, Yurieva OV, Minakhina SV, Nikiforov VG. 1995. Four genes, two ends, and a res region are involved in transposition of Tn5053: a paradigm for a novel family of transposons carrying either a mer operon or an integron. Mol Microbiol 17:1189–1200. doi: 10.1111/j.1365-2958.1995.mmi_17061189.x. [DOI] [PubMed] [Google Scholar]
- 23.Carattoli A, Bertini A, Villa L, Falbo V, Hopkins KL, Threlfall EJ. 2005. Identification of plasmids by PCR-based replicon typing. J Microbiol Methods 63:219–228. doi: 10.1016/j.mimet.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 24.García-Fernández A, Chiaretto G, Bertini A, Villa L, Fortini D, Ricci A, Carattoli A. 2008. Multilocus sequence typing of IncI1 plasmids carrying extended-spectrum β-lactamases in Escherichia coli and Salmonella of human and animal origin. J Antimicrob Chemother 61:1229–1233. doi: 10.1093/jac/dkn131. [DOI] [PubMed] [Google Scholar]
- 25.Clinical and Laboratory Standards Institute. 2015. Methods for dilution antimicrobial susceptibility. Tests for bacteria that grow aerobically; approved standards, 10th ed CLSI document M07-A10. CLSI, Wayne, PA. [Google Scholar]
- 26.Clinical and Laboratory Standards Institute. 2015. Performance standards for antimicrobial susceptibility testing. CLSI supplement M100-S25. CLSI, Wayne, PA. [Google Scholar]
- 27.Simpson JT, Wong K, Jackman SD, Schein JE, Jones SJ, Birol I. 2009. ABySS: a parallel assembler for short read sequence data. Genome Res 19:1117–1123. doi: 10.1101/gr.089532.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sampei G, Furuya N, Tachibana K, Saitou Y, Suzuki T, Mizobuchi K, Komano T. 2010. Complete genome sequence of the incompatibility group I1 plasmid R64. Plasmid 64:92–103. doi: 10.1016/j.plasmid.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 29.Sullivan MJ, Petty NK, Beatson SA. 2011. Easyfig: a genome comparison visualizer. Bioinformatics 27:1009–1010. doi: 10.1093/bioinformatics/btr039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thanassi DG, Cheng LW, Nikaido H. 1997. Active efflux of bile salts by Escherichia coli. J Bacteriol 179:2512–2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson TJ, Shepard SM, Rivet B, Danzeisen JL, Carattoli A. 2011. Comparative genomics and phylogeny of the IncI1 plasmids: a common plasmid type among porcine enterotoxigenic Escherichia coli. Plasmid 66:144–151. doi: 10.1016/j.plasmid.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 32.Wachino J, Yamane K, Suzuki S, Kimura K, Arakawa Y. 2010. Prevalence of fosfomycin resistance among CTX-M-producing Escherichia coli clinical isolates in Japan and identification of novel plasmid-mediated fosfomycin-modifying enzymes. Antimicrob Agents Chemother 54:3061–3064. doi: 10.1128/AAC.01834-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hou J, Huang X, Deng Y, He L, Yang T, Zeng Z, Chen Z, Liu JH. 2012. Dissemination of the fosfomycin resistance gene fosA3 with CTX-M β-lactamase genes and rmtB carried on IncFII plasmids among Escherichia coli isolates from pets in China. Antimicrob Agents Chemother 56:2135–2138. doi: 10.1128/AAC.05104-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cullik A, Pfeifer Y, Prager R, von Baum H, Witte W. 2010. A novel IS26 structure surrounds blaCTX-M genes in different plasmids from German clinical Escherichia coli isolates. J Med Microbiol 59:580–587. doi: 10.1099/jmm.0.016188-0. [DOI] [PubMed] [Google Scholar]
- 35.Zong Z, Yu R, Wang X, Lü X. 2011. blaCTX-M-65 is carried by a Tn1722-like element on an IncN conjugative plasmid of ST131 Escherichia coli. J Med Microbiol 60:435–441. doi: 10.1099/jmm.0.026997-0. [DOI] [PubMed] [Google Scholar]
- 36.Yang X, Liu W, Liu Y, Wang J, Lv L, Chen X, He D, Yang T, Hou J, Tan Y, Xing L, Zeng Z, Liu J. 2014. F33: A-: B-, IncHI2/ST3, and IncI1/ST71 plasmids drive the dissemination of fosA3 and blaCTX-M-55/-14/-65 in Escherichia coli from chickens in China. Front Microbiol 5:688. doi: 10.3389/fmicb.2014.00688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harmer CJ, Moran RA, Hall RM. 2014. Movement of IS26-associated antibiotic resistance genes occurs via a translocatable unit that includes a single IS26 and preferentially inserts adjacent to another IS26. mBio 5:e01801–1814. doi: 10.1128/mBio.01801-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li L, Liao XP, Liu ZZ, Huang T, Li X, Sun J, Liu BT, Zhang Q, Liu YH. 2014. Co-spread of oqxAB and blaCTX-M-9G in non-Typhi Salmonella enterica isolates mediated by ST2-IncHI2 plasmids. Int J Antimicrob Agents 44:263–268. doi: 10.1016/j.ijantimicag.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 39.Miriagou V, Carattoli A, Fanning S. 2006. Antimicrobial resistance islands: resistance gene clusters in Salmonella chromosome and plasmids. Microbes Infect 8:1923–1930. doi: 10.1016/j.micinf.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 40.Partridge SR, Zong Z, Iredell JR. 2011. Recombination in IS26 and Tn2 in the evolution of multiresistance regions carrying blaCTX-M-15 on conjugative IncF plasmids from Escherichia coli. Antimicrob Agents Chemother 55:4971–4978. doi: 10.1128/AAC.00025-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zheng H, Zeng Z, Chen S, Liu Y, Yao Q, Deng Y, Chen X, Lv L, Zhuo C, Chen Z, Liu JH. 2012. Prevalence and characterisation of CTX-M β-lactamases amongst Escherichia coli isolates from healthy food animals in China. Int J Antimicrob Agents 39:305–310. doi: 10.1016/j.ijantimicag.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 42.Yao Q, Zeng Z, Hou J, Deng Y, He L, Tian W, Zheng H, Chen Z, Liu JH. 2011. Dissemination of the rmtB gene carried on IncF and IncN plasmids among Enterobacteriaceae in a pig farm and its environment. J Antimicrob Chemother 66:2475–2479. doi: 10.1093/jac/dkr328. [DOI] [PubMed] [Google Scholar]
- 43.Hou J, Yang X, Zeng Z, Lv L, Yang T, Lin D, Liu JH. 2013. Detection of the plasmid-encoded fosfomycin resistance gene fosA3 in Escherichia coli of food-animal origin. J Antimicrob Chemother 68:766–770. doi: 10.1093/jac/dks465. [DOI] [PubMed] [Google Scholar]
- 44.Yuan L, Liu JH, Hu GZ, Pan YS, Liu ZM, Mo J, Wei YJ. 2009. Molecular characterization of extended-spectrum β-lactamase-producing Escherichia coli isolates from chickens in Henan Province, China. J Med Microbiol 58:1449–1453. doi: 10.1099/jmm.0.012229-0. [DOI] [PubMed] [Google Scholar]
- 45.Lu Y, Zhao H, Sun J, Liu Y, Zhou X, Beier RC, Wu G, Hou X. 2014. Characterization of multidrug-resistant Salmonella enterica serovars Indiana and Enteritidis from chickens in Eastern China. PLoS One 9:e96050. doi: 10.1371/journal.pone.0096050. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.