Abstract
The gut microbiota has been linked to metabolic diseases. However, information on the microbiome of young adults at risk for type 2 diabetes (T2D) is lacking. The aim of this cross-sectional analysis was to investigate whether insulin resistant women with previous gestational diabetes (pGDM), a high risk group for T2D, differ in their stool microbiota from women after a normoglycemic pregnancy (controls). Bacterial communities were analyzed by high-throughput 16S rRNA gene sequencing using fecal samples from 42 pGDM and 35 control subjects 3–16 months after delivery. Clinical characterization included a 5-point OGTT, anthropometrics, clinical chemistry markers and a food frequency questionnaire. Women with a Prevotellaceae-dominated intestinal microbiome were overrepresented in the pGDM group (p < 0.0001). Additionally, the relative abundance of the phylum Firmicutes was significantly lower in women pGDM (median 48.5 vs. 56.8%; p = 0.013). Taxa richness (alpha diversity) was similar between the two groups and with correction for multiple testing we observed no significant differences on lower taxonomic levels. These results suggest that distinctive features of the intestinal microbiota are already present in young adults at risk for T2D and that further investigations of a potential pathophysiological role of gut bacteria in early T2D development are warranted.
Data from human and animal studies suggest that the gut microbiota influences metabolic health1,2. The microbiota itself can be markedly affected by dietary habits and medications as well as probably by other until now not fully defined factors3,4.
Several studies examined stool microbiota changes associated with metabolic diseases in human subjects. A lower bacterial diversity has been described in association with obesity and insulin resistance5,6. On the level of bacterial phyla, a decreased ratio of Bacteroidetes to Firmicutes (B/F ratio) has been shown to be associated with obesity7,8 but these findings are controversial9,10,11. Finucane et al. concluded in a recent review that there are no simple taxonomic compositions, consistent over different studies, which differentiate between obese and lean individuals12. Reduced relative abundance of Firmicutes and of the class Clostridia was found in individuals with type 2 diabetes (T2D)13,14,15. On a functional level, several groups reported a reduction of butyrate-producing bacteria in diabetic individuals14,15,16. A causal role of the gut microbiota in the development of T2D and also metabolic syndrome is supported by transplantation studies, both in animal models and in humans17,18.
Previous human studies concerning associations of the intestinal microbiota with T2D focused on individuals above 50 years of age14,15,16 and no information is available on the microbiome composition of younger subjects at risk for T2D. In this study, we therefore wanted to test if the composition of the stool microbiota already varied with T2D risk in young adults. Since no biomarkers exist to reliably identify at-risk subjects at this age we chose insulin resistant women with a recent history of gestational diabetes (GDM) as our high risk cohort and compared these to a suitable control group. Women post-GDM have a substantially increased risk for T2D, particularly if they remain insulin resistant after the pregnancy19,20,21.
Results
Baseline characteristics
We selected two diametrically opposed groups of women from a prospective post-gestation study: Insulin resistant women with a recent history of GDM (post-GDM/pGDM; n = 42) and women after a normoglycemic pregnancy as controls (n = 35). All data and samples were collected 3 to 16 months after delivery. The clinical baseline characteristics of the study cohort are shown in Table 1. A proportion of 50% of the women pGDM had impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT), whereas all controls were normoglycemic. Data from the EPIC food-frequency questionnaire22 (n = 64) showed no significant differences in dietary intake of macronutritients and fiber between the pGDM and the control group (Table S1).
Table 1. Clinical and biochemical characteristics of pGDM and controls.
| pGDM n = 42 | controls n = 35 | p-value | |
|---|---|---|---|
| clinical characteristics during previous pregnancy | |||
| GDM with/without insulin | 27/15 64.3%/35.7% | — | |
| clinical characteristics at postpartum study visit | |||
| NGT/PGT(IFG/IGT/IFG + IGT) | 21/21(7/10/4) 50%/50% (16.7%/23.8%/9.5%) | 35 100% | |
| age (years) | 37 [34–39] | 36 [32–38] | 0.242 |
| months post delivery | 8.8 [6.6–10.6] | 8.8 [6.9–10.2] | 0.914 |
| breast feeding at time of visit (full/partial/no) | 3/12/27 (7.1%/28.6%/64.3%) | 0/15/20 (0%/42.9%/57.1%) | 0.194# |
| primipara (yes/no) | 19/23 (45.2%/54.8%) | 19/16 (54.3%/45.7%) | 0.429## |
| hormonal contraception (yes/no) | 12/30 (28.6%/71.4%) | 5/29 (14.3%/82.9%) | 0.149## |
| regular menstrual cycle without hormonal contraception (yes/no) | 19/10 (63.3%/33.3%) | 12/17 (41.4%/58.6%) | 0.065## |
| bmi (kg/m2) | 27.0 [23.9–31.6] | 22.6 [21.3–26.2] | <0.001 |
| waist circumference (cm) | 86.0 [77.0–99.0] | 74.0 [70.0–86.0] | <0.001 |
| whr | 0.81 [0.77–0.87] | 0.79 [0.74–0.83] | 0.029 |
| body fatBIA (%) (n = 42/34) | 36.4 [29.9–42.5] | 30.3 [25.2–36.0] | 0.002 |
| systolic blood pressure (mmHg) | 120 [111–130] | 112 [105–123] | 0.006 |
| diastolic blood pressure (mmHg) | 74 [67–81] | 70 [64–79] | 0.060 |
| biochemical characteristics at postpartum study visit | |||
| Matsuda Index | 3.19 [2.27–4.35] | 7.31 [4.84–9.21] | <0.001 |
| HOMA-IR | 2.65 [1.91–3.63] | 1.22 [0.81–1.91] | <0.001 |
| Disposition Index | 176.04 [126.54–233.28] | 309.52 [230.54–388.33] | <0.001 |
| triglycerides (mg/dl) | 89 [70–110] | 63 [52–87] | 0.001 |
| hdl cholesterol (mg/dl) | 55 [44–64] | 64 [56–75] | <0.001 |
| ldl cholesterol (mg/dl) | 107 [91–124] | 115 [97–133] | 0.346 |
| hsCRP (mg/dl) | 0.13 [0.03–0.40] | 0.06 [0.01–0.12] | 0.003 |
| gamma-glutamyl transferase (U/l) | 18 [13–22] | 13 [11–16] | 0.003 |
| hba1c (%) (n = 42/34) | 5.4 [5.3–5.6] | 5.3 [5.1–5.5] | 0.060 |
| leptin (ng/ml) | 13.50 [9.36–19.73] | 7.01 [2.48–12.28] | <0.001 |
Values are represented as median [Q1–Q3] or as n and %. Mann-Whitney U tests were used except for #Fisher Exact test and ##χ-square test. NGT = normal glucose tolerance. PGT = pathologic glucose tolerance. IFG = impaired fasting glucose. IGT = impaired glucose tolerance.
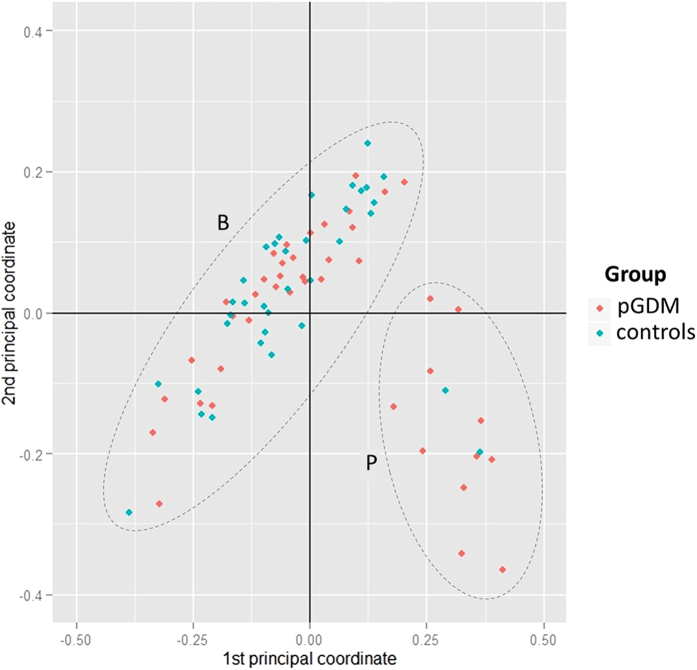
Bacterial community structure (beta diversity) in the two study groups
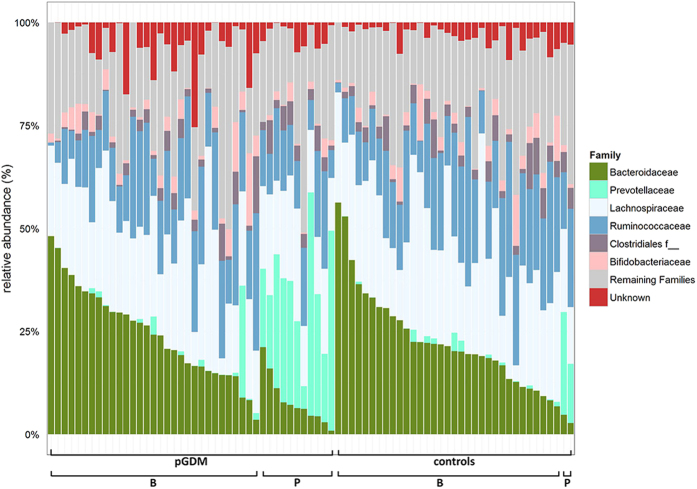
A total number of 307 Operational Taxonomic Units (OTUs) were quantified in this study. To examine the bacterial community structure in the stool samples, we analyzed the dataset by a principal coordinate analysis (PCoA) on the basis of Bray-Curtis distances and a permutational MANOVA (pMANOVA)23. We found no significant clustering of the predefined post-GDM and control group (p = 0.1). However, the samples from 13 women (cluster P) showed a bacterial composition distinct from the rest of the study cohort (cluster B) (Fig. 1, p = 0.001 in pMANOVA). The relative abundance of 35 OTUs was significantly different between these two groups after correction for multiple testing (Table S2). In particular, members of the family Prevotellaceae were more abundant in samples within cluster P (24.9 [17.8–30.2] vs. 0.08 [0.02–1.01] %, p < 0.0001), whereas the sequence proportion of the family Bacteroidaceae was decreased (6.2 [4.4–7.7] vs. 21.9 [15.9–30.8] %, p < 0.0001; Fig. 2). OTU2, which could be assigned down to the species level as Prevotella copri, was highly enriched in the subpopulation of cluster P (23.3 [13.1–28.5] vs. 0.01 [0.00–0.02] %, p < 0.001). Cluster P was significantly associated with belonging to the post-GDM group (11 out of 13 individuals in cluster P; p < 0.0001). EPIC-FFQ data revealed no differences in consumption of macronutrients and of different food groups (meat, fat, vegetables, fruits and cereals) between the women in cluster P and those in cluster B. A canonical correspondence analysis (CCA) and permutation tests showed no significant influence of age (p = 0.664), bmi (p = 0.806), time since delivery (p = 0.309) and plasma leptin levels (p = 0.294) on the beta diversity data.
Figure 1. PCoA of the bacterial community composition based on Bray Curtis analysis.
One dot represents one individual (post-GDM = red, controls = blue). pMANOVA revealed no significant differences between the prespecified groups (p = 0.1). However, two other clusters were identified in an analysis without prespecifications (designated clusters B and P; p = 0.001).
Figure 2. Top 6 bacterial families in the fecal microbiota.
One bar represents one study participant. Subjects were first sorted by group (pGDM vs. control), then by cluster (Fig. 1) and then by the relative abundance of Bacteroidaceae. The category ‘remaining families’ includes all families except for the top 6. f__ = unknown family.
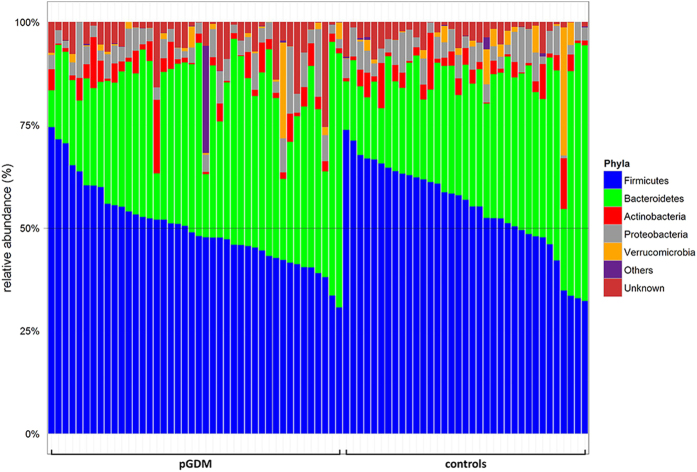
Phylum-level differences between the post-GDM and the control group
At the phylum level, Actinobacteria, Bacteroidetes, Firmicutes, Proteobacteria and Verrucomicrobia accounted on average for 95.4% of total sequences in all study participants, whereas 4.2% were unknown bacterial phyla. A minor fraction of sequences (0.4%) was assigned to the phyla Euryarchaeota, Elusimicrobia, Fusobacteria and Lentisphaerae (referred to as “others” in this manuscript).
Group comparisons for phyla abundances are shown in Fig. 3 and Table S3. Firmicutes was less abundant in women post-GDM than in controls (48.5 [43.2–55.1] vs. 56.8 [48.5–63.2] %, p = 0.013). This finding remained unchanged by the variable ‘time since delivery’ in a bivariate regression analysis (data not shown). We also saw a reduced proportion of the phylum Firmicutes when we compared only the normoglycemic women post-GDM (n = 21) with the control group (n = 35; all normoglycemic) (50.5 [45.6–55.5] vs. 56.8 [48.–63.2] %, p = 0.045). The proportion of Firmicutes also remained lower in the pGDM group when we removed all women in cluster P from the analysis (p = 0.049).
Figure 3. Relative abundances of bacterial phyla.
Each bar represents one individual. Subjects were first sorted by group (pGDM vs. control), then by the relative abundance of Firmicutes, the most common phylum.
Bacterial richness (alpha diversity) and results on lower taxonomic levels
We found no differences in the alpha diversity between pGDM and control subjects (Fig. S1). Similarly, we observed no significant differences in the taxonomic ranks class, order, family and OTU between the two study groups when we applied corrections for multiple testing. These data and the exploratory (uncorrected) p-values are shown in (Table S4).
Discussion
In this study, we compared the stool microbiota of a group of young adults at high risk for subsequent T2D, namely of insulin resistant women after recent GDM with those of a control group - women after a normoglycemic pregnancy. The main findings of this study were that the analysis of beta diversity separated the study participants into two clusters with distinct microbiome compositions and that the less common, Prevotellaceae-rich type of microbiome associated strongly with the post-GDM group. Additionally, at the phylum level, the proportion of Firmicutes was lower in the women post-GDM.
Identifying young adults at risk for T2D is difficult because of a lack of suitable biomarkers or highly predictive clinical parameters. Family history or a prediabetic glucose tolerance status have been used for this purpose but these approaches have significant limitations (discussed in20). We therefore used an alternative method to define a young adult at risk cohort and studied women with recent GDM, who remained insulin resistant after delivery. Women with GDM have an about 10-fold increased risk for T2D within 10 years compared to women normoglycemic during pregnancy21. Among those post GDM, this risk is further increased if insulin resistance persists after giving birth19,20.
Our analysis of beta diversity revealed that a subgroup of 13 women (17% of the study cohort) had a distinct microbiota composition characterized by a high proportion of the family Prevotellaceae, while Bacteroidaceae dominated in the other study participants. This finding was not explained by differences in dietary habits and is in line with a model of two enterotypes proposed recently24,25. This model remains controversial26 and our study lacks the sample size to settle the issue. Nevertheless, a Prevotellaceae-rich microbiome was associated with belonging to the high risk group for T2D in our study. Our finding adds to previous reports of an inverse association between the Bacteroides/Prevotella ratio and obesity27, non-alcoholic steatohepatitis28 and elevated total plasma cholesterol25. Potential causative links remain speculative. Prevotella are mucin degrading bacteria, which may be associated with increased gut permeability29 and P. copri, the most dominant molecular species within the taxa Prevotella in our study, has recently been associated with new-onset rheumatoid arthritis30. It could therefore be related to low-grade inflammation, which is also detrimental with respect to metabolism.
We further observed a lower relative abundance of Firmicutes in the post-GDM group, a finding previously reported for individuals with already established T2D13,14,15. This observation was also true for the normoglycemic women in our study and remained significant in an analysis restricted to women with a Bacteroidaceae-rich microbiome. The difference was small (median 49 vs. 57%) and a relevant overlap existed between the post-GDM and the control group (Fig. 3). Hence, the cause-effect relationships remain unknown. Higher resolution analyses on lower taxonomic levels, requiring large sample sizes, may nevertheless reveal specific underlying differences in microbial composition or function.
The main limitations of our present study are the limited sample size and the fact that only one stool sample per study participant was available. Additionally, the observational, cross-sectional study design precludes examining causality. Strengths of our work are the young adult, uniform cohorts of individuals with little concomitant medication and comorbidities and the detailed clinical phenotyping available.
In conclusion, this study suggests that distinctive features of the intestinal microbiota are already present in young adults at risk for T2D. In particular, it supports a link between a Prevotellaceae-dominated microbiome and T2D risk. Our results warrant further investigation in larger human cohorts and other clinical settings, as well as examination of the underlying molecular mechanisms.
Subjects and Methods
Study population
Subjects included in the present analysis were participants of the prospective, mono-center observational study PPS-Diab (prediction, prevention and subclassification of type 2 diabetes) enrolled between November 2011 and December 2013 as described previously20. Women with GDM during their last pregnancy and women following a normoglycemic pregnancy, treated at the Diabetes Center and the obstetrics department of the University Hospital (Klinikum der Universität München) in Munich, Germany, were consecutively recruited for this study in a 2:1 ratio. The diagnosis of GDM was based on a standardized oral glucose tolerance test (OGTT) after the 23rd week of the preceding pregnancy. Exclusion criteria for this study were alcohol or substance abuse, positivity for islet-autoantibodies and chronic diseases requiring medication except for hypothyroidism (n = 13). The study participants were not taking any antibiotic therapy for at least 14 days prior to clinical assessment and stool collection. The study was performed in accordance with relevant guidelines and regulations. Written informed consent was obtained from all study participants and the protocol was approved by the ethical review committee of the Ludwig-Maximilians-Universität München.
All data used in the present analysis were collected at the baseline visit of the PPS-Diab study, 3 to 16 months after the index pregnancy. For this analysis we selected two groups of women from the first 147 eligible study participants (thereof 96 post-GDM women with Matsuda Index = 4.2 [2.9–6.9]): the 45 most insulin resistant women with recent GDM (Matsuda Index = 3.3 [2.4–4.4]) and no diabetes at the time of the baseline visit (high risk subjects) and all 35 controls after a normoglycemic pregnancy (low risk subjects), from whom a stool sample was available. The samples of three individuals failed quality control after sequencing. The final study cohort therefore consisted of 42 high risk and 35 low risk women.
Anthropometric and clinical assessments
All subjects underwent a 5-point OGTT and anthropometric measurements. To quantify insulin sensitivity the Matsuda Index was calculated from the OGTT plasma glucose and insulin measurements as described previously31 and the HOMA-IR was calculated as the product of fasting glucose and fasting insulin concentrations32. The disposition index was calculated from the OGTT to describe the relationship between insulin sensitivity and first-phase insulin secretion33. Thereby, the rise in serum insulin during the first 30 minutes of the OGTT was used as a measure of the first-phase insulin secretion. Prediabetes was defined as IFG, IGT or a combination of both following the definition of the American Diabetes Association34.
Systolic and diastolic blood pressure was measured twice in a sitting position. Weight and body fat mass was assessed by a bioelectrical impedance analysis (BIA) scale (Tanita BC-418, Tanita Corporation, Tokyo, Japan). The bmi was calculated as weight in kilograms divided by height squared in meters. Waist and hip circumference were measured with a tape measurement. A food frequency questionnaire (EPIC-FFQ) for the assessment of dietary nutritional intake was completed online (n = 64)22.
Blood samples
Blood samples were processed immediately after collection and analyzed directly or stored in aliquots at −80 °C. Standard methods were used to measure glucose (glucose oxidase method, Glucose HK Gen.3, Roche Diagnostics, Mannheim, Germany), hba1c (VARIANT™ II TURBO HbA1c Kit - 2.0, Bio-Rad Laboratories, Hercules, USA), gamma-GT (enzymatic caloric test, Roche Diagnostics), triglycerides and HDL (enzymatic caloric test, Roche Diagnostics). LDL was calculated by the Friedewald equation (all triglyceride levels were below 400 mg/dl). Stored serum samples were used to measure insulin by chemiluminescence technology (CLIA, DiaSorin LIAISON systems, Saluggia, Italy). High-sensitive CRP (hsCRP) and leptin were measured from stored plasma samples by ELISAs (hsCRP by wide-range CRP, Siemens AG, Erlangen, Germany and leptin by ELISA “Dual Range”, Merck Millipore, Darmstadt, Germany).
Stool sample collection
Each study participant collected one stool sample at home using a paper stool collector and tubes pre-filled with 8 ml of stool DNA stabilizer and including a measuring spoon for the sample (PSP Spin Stool DNA Plus Kit, STRATEC Molecular, Berlin, Germany). Samples were mailed to the study center within one day after collection and then immediately stored at −80 °C until DNA extraction.
Microbiota sequencing
Bacterial DNA was obtained from fecal samples according to the manufacturer’s instructions (PSP Spin Stool DNA Plus Kit, STRATEC Molecular). The V4 region of 16S rRNA genes was amplified (25 cycles) as described previously35 following a 2-step procedure to limit artifacts36. Amplicons were purified using the AMPure XP system (Beckman Coulter GmbH, Krefeld, Germany) and sequenced in paired-end modus (PE200) using the MiSeq system (Illumina Inc., San Diego, USA). The raw read files were demultiplexed (allowing a maximum of 2 errors in barcodes) and each sample was processed using usearch37 following the UPARSE approach38. First, all reads were trimmed to the position of the first base with quality score <3 and then paired. The resulted sequences were size filtered, excluding those with assembled size <200 and >260. Paired reads with a number of expected error >3 were further filtered out and the remaining sequences were trimmed by 10 nucleotides on each side to avoid GC bias and non-random base composition. For each sample, sequences were de-replicated and checked for chimeras with UCHIME39. Sequences from all samples were merged, sorted by abundance and OTUs representatives were picked at a threshold of 97% similarity. Finally, all sequences were mapped back to the representative sequences resulting in the OTU table for all samples. The RDP classifier40 was used to assign taxonomic classification to the OTUs representative sequences (80% confidence). OTUs of particular interest were identified more precisely using the EzTaxon server: http://www.ezbiocloud.net/eztaxon41. A phylogenetic tree was constructed using fasttree42. Only OTUs with a relative abundance above 0.5% total sequences in at least one sample were kept. The OTU table was rarefied to the minimum count of sequences observed. After processing (quality- and chimera-check as well as OTU filtering) a total of 2,655,517 16S rRNA reads were used for analysis. We obtained a median of 33,807 sequences per sample with a range of 21,812–51,777 and used 20,000 sequences per sample for rarefaction.
Statistical analysis
Statistical analyses were performed using R version 3.1.043 and SPSS version 22.0 (SPSS Inc., Chicago, IL, USA). Clinical baseline characteristics are presented as median with interquartile ranges (Q1-Q3). Alpha diversity was measured by the Chao1 Index, which primary calculates the number of taxa44 and by the Shannon and Simpson Indices, which represent richness and distribution of taxa45. Differences in beta diversity were calculated by pMANOVA46 and illustrated by a PCoA of Bray Curtis distances23. The Chi-square test was used for comparing the two subtypes of microbiota composition identified by pMANOVA. A canonical correspondence analysis (CCA) and permutation tests were done using the R package phyloseq. The relative abundances of the taxonomic ranks phylum, class, order, family and of the molecular species are shown as median, interquartile ranges and minimum (min) and maximum (max). The Mann-Whitney U test, the Fisher Exact test or the χ-square test were used for comparisons between groups. The phylum Firmicutes was further analyzed together with the variable ‘time since delivery’ as independent variables by a binary logistic regression model for the dependent variable pGDM status. P-values <0.05 were considered statistically significant. Correction for multiple testing by false discovery rate control with the Benjamini–Hochberg procedure was done where indicated in the text.
Additional Information
How to cite this article: Fugmann, M. et al. The stool microbiota of insulin resistant women with recent gestational diabetes, a high risk group for type 2 diabetes. Sci. Rep. 5, 13212; doi: 10.1038/srep13212 (2015).
Supplementary Material
Acknowledgments
We thank all women who participated in the PPS-Diab study for their invaluable contribution to this project. This work is part of the Ph.D. thesis of Marina Fugmann at the Medical Faculty of the Ludwig-Maximilians-Universität München in Munich, Germany. Funding: This work was funded by Helmholtz Zentrum München, Klinikum der Universität München and the German Center for Diabetes Research.
Footnotes
The authors declare no competing financial interests.
Author Contributions M.F., F.B., U.F., V.S., K.G.P., J.S. and A.L. designed the study. M.F., M.B., M.R., H.G. and T.C. acquired and analyzed the data. M.F., M.R., T.C. and A.L. interpreted the data. All authors contributed to the drafting and revising of the article and approved the final version to be published.
References
- Musso G., Gambino R. & Cassader M. Interactions between gut microbiota and host metabolism predisposing to obesity and diabetes. Annual review of medicine 62, 361–380, 10.1146/annurev-med-012510-175505 (2011). [DOI] [PubMed] [Google Scholar]
- Vrieze A. et al. The environment within: how gut microbiota may influence metabolism and body composition. Diabetologia 53, 606–613, 10.1007/s00125-010-1662-7 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muegge B. D. et al. Diet drives convergence in gut microbiome functions across mammalian phylogeny and within humans. Science 332, 970–974, 10.1126/science.1198719 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delzenne N. M. & Cani P. D. Interaction between obesity and the gut microbiota: relevance in nutrition. Annual review of nutrition 31, 15–31, 10.1146/annurev-nutr-072610-145146 (2011). [DOI] [PubMed] [Google Scholar]
- Le Chatelier E. et al. Richness of human gut microbiome correlates with metabolic markers. Nature 500, 541–546, 10.1038/nature12506 (2013). [DOI] [PubMed] [Google Scholar]
- Turnbaugh P. J. et al. A core gut microbiome in obese and lean twins. Nature 457, 480–484, 10.1038/nature07540 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ley R. E., Turnbaugh P. J., Klein S. & Gordon J. I. Microbial ecology: human gut microbes associated with obesity. Nature 444, 1022–1023, 10.1038/4441022a (2006). [DOI] [PubMed] [Google Scholar]
- Verdam F. J. et al. Human intestinal microbiota composition is associated with local and systemic inflammation in obesity. Obesity 21, E607–615, 10.1002/oby.20466 (2013). [DOI] [PubMed] [Google Scholar]
- Duncan S. H. et al. Human colonic microbiota associated with diet, obesity and weight loss. International journal of obesity 32, 1720–1724, 10.1038/ijo.2008.155 (2008). [DOI] [PubMed] [Google Scholar]
- Fernandes J., Su W., Rahat-Rozenbloom S., Wolever T. M. & Comelli E. M. Adiposity, gut microbiota and faecal short chain fatty acids are linked in adult humans. Nutrition & diabetes 4, e121, 10.1038/nutd.2014.23 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwiertz A. et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity 18, 190–195, 10.1038/oby.2009.167 (2010). [DOI] [PubMed] [Google Scholar]
- Finucane M. M., Sharpton T. J., Laurent T. J. & Pollard K. S. A taxonomic signature of obesity in the microbiome? Getting to the guts of the matter. PloS one 9, e84689, 10.1371/journal.pone.0084689 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen N. et al. Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults. PloS one 5, e9085, 10.1371/journal.pone.0009085 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson F. H. et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature 498, 99–103, 10.1038/nature12198 (2013). [DOI] [PubMed] [Google Scholar]
- Qin J. et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490, 55–60, 10.1038/nature11450 (2012). [DOI] [PubMed] [Google Scholar]
- Zhang X. et al. Human gut microbiota changes reveal the progression of glucose intolerance. PloS one 8, e71108, 10.1371/journal.pone.0071108 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koren O. et al. Host remodeling of the gut microbiome and metabolic changes during pregnancy. Cell 150, 470–480, 10.1016/j.cell.2012.07.008 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrieze A. et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology 143, 913–916 e917, 10.1053/j.gastro.2012.06.031 (2012). [DOI] [PubMed] [Google Scholar]
- Tura A. et al. Progression to type 2 diabetes in women with former gestational diabetes: time trajectories of metabolic parameters. PloS one 7, e50419, 10.1371/journal.pone.0050419 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rottenkolber M. et al. The diabetes risk phenotype of young women with recent gestational diabetes. The Journal of clinical endocrinology and metabolism jc20143898, 10.1210/jc.2014-3898 (2015). [DOI] [PubMed] [Google Scholar]
- Feig D. S., Zinman B., Wang X. & Hux J. E. Risk of development of diabetes mellitus after diagnosis of gestational diabetes. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne 179, 229–234, 10.1503/cmaj.080012 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroke A. et al. Validation of a self-administered food-frequency questionnaire administered in the European Prospective Investigation into Cancer and Nutrition (EPIC) Study: comparison of energy, protein, and macronutrient intakes estimated with the doubly labeled water, urinary nitrogen, and repeated 24-h dietary recall methods. The American journal of clinical nutrition 70, 439–447 (1999). [DOI] [PubMed] [Google Scholar]
- Bray, J. R. & Curtis J. T. An ordination of upland forest communities of southern Westconsin. Ecological monographs. 27, 325–349 (1957). [Google Scholar]
- Bergstrom A. et al. Establishment of intestinal microbiota during early life: a longitudinal, explorative study of a large cohort of Danish infants. Applied and environmental microbiology 80, 2889–2900, 10.1128/AEM.00342-14 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roager H. M., Licht T. R., Poulsen S. K., Larsen T. M. & Bahl M. I. Microbial enterotypes, inferred by the prevotella-to-bacteroides ratio, remained stable during a 6-month randomized controlled diet intervention with the new nordic diet. Applied and environmental microbiology 80, 1142–1149, 10.1128/AEM.03549-13 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koren O. et al. A guide to enterotypes across the human body: meta-analysis of microbial community structures in human microbiome datasets. PLoS computational biology 9, e1002863, 10.1371/journal.pcbi.1002863 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furet J. P. et al. Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes 59, 3049–3057, 10.2337/db10-0253 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouzaki M. et al. Intestinal microbiota in patients with nonalcoholic fatty liver disease. Hepatology 58, 120–127, 10.1002/hep.26319 (2013). [DOI] [PubMed] [Google Scholar]
- Brown C. T. et al. Gut microbiome metagenomics analysis suggests a functional model for the development of autoimmunity for type 1 diabetes. PloS one 6, e25792, 10.1371/journal.pone.0025792 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scher J. U. et al. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. eLife 2, e01202, 10.7554/eLife.01202 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuda M. & DeFronzo R. A. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes care 22, 1462–1470 (1999). [DOI] [PubMed] [Google Scholar]
- Matthews D. R. et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985). [DOI] [PubMed] [Google Scholar]
- Kahn S. E. et al. Quantification of the relationship between insulin sensitivity and beta-cell function in human subjects. Evidence for a hyperbolic function. Diabetes 42, 1663–1672 (1993). [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes care 37 Suppl 1, S14–80 (2014). [DOI] [PubMed] [Google Scholar]
- Caporaso J. G. et al. Ultra-high-throughput microbial community analysis on the Illumina HiSeq and MiSeq platforms. The ISME journal 6, 1621–1624, 10.1038/ismej.2012.8 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry D., Ben Mahfoudh K., Wagner M. & Loy A. Barcoded primers used in multiplex amplicon pyrosequencing bias amplification. Applied and environmental microbiology 77, 7846–7849, 10.1128/AEM.05220-11 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgar R. C. Search and clustering orders of magnitude faster than BLAST. Bioinformatics 26, 2460–2461, 10.1093/bioinformatics/btq461 (2010). [DOI] [PubMed] [Google Scholar]
- Edgar R. C. UPARSE: highly accurate OTU sequences from microbial amplicon reads. Nature methods 10, 996–998, 10.1038/nmeth.2604 (2013). [DOI] [PubMed] [Google Scholar]
- Edgar R. C., Haas B. J., Clemente J. C., Quince C. & Knight R. UCHIME improves sensitivity and speed of chimera detection. Bioinformatics 27, 2194–2200, 10.1093/bioinformatics/btr381 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Garrity G. M., Tiedje J. M. & Cole J. R. Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Applied and environmental microbiology 73, 5261–5267, 10.1128/AEM.00062-07 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim O. S. et al. Introducing EzTaxon-e: a prokaryotic 16S rRNA gene sequence database with phylotypes that represent uncultured species. International journal of systematic and evolutionary microbiology 62, 716–721, 10.1099/ijs.0.038075-0 (2012). [DOI] [PubMed] [Google Scholar]
- Price M. N., Dehal P. S. & Arkin A. P. FastTree 2—approximately maximum-likelihood trees for large alignments. PloS one 5, e9490, 10.1371/journal.pone.0009490 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. (2008) Available at: http://www.R-project.org (date of access 01.04.2014).
- Chao A. Estimating the population size for capture-recapture data with unequal catchability. Biometrics 43, 783–791 (1987). [PubMed] [Google Scholar]
- Hill M. O. Diversity and evenness: a unifying notation and its consequences. Ecology 54, 427–432 (1973). [Google Scholar]
- Oksanen J. et al. vegan: Community Ecology Package. R package version 2.0-10. (2013) Available at: http://CRAN.R-project.org/package=vegan (date of access 01.04.2014).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.