Abstract
Background:
Anterior shoulder dislocation (ASD) is one of the most common reasons for referrals to emergency departments (ED). Usually, a combination of an intravenous narcotic and a benzodiazepine is used for procedural sedation and analgesia (PSA) in such cases.
Objectives:
This study compares the efficacy of two combinations to reduce ASD.
Patients and Methods:
The subjects in this clinical trial consisted of 48 patients with ASD who were randomly assigned to midazolam/fentanyl and propofol/fentanyl groups for PSA. The two groups were compared to the time interval between injection and induction of sedation (T1), duration of time from sedation to awakening (T2), the duration of time between sedation and full awareness to time, location and individuals (T3), and possible side effects.
Results:
Twenty-nine subjects (60.4%) were sedated with midazolam and 19 (39.6%) were sedated with propofol. During the procedure, one patient in the propofol group experienced apnea (P = 0.39) and three patients (one in the midazolam group and two in the propofol group) experienced bradycardia (P = 0.34). The mean T1, T2, and T3 were significantly shorter in the propofol group (P < 0.001).
Conclusions:
It seems that propofol and fentanyl can be used as a safe and fast combination for PSA in the reduction of ASD.
Keywords: Propofol, Midazolam, Shoulder Dislocation, Sedation, Analgesic
1. Background
Anterior shoulder dislocation (ASD) is one of the most common reasons for referrals to emergency departments (EDs) (1). Dislocations not associated with fractures or neurovascular injuries are reduced under sedation in the ED by emergency medicine specialists or orthopedic surgeons. Various medications and techniques are used for sedation, each with advantages and disadvantages (2, 3). Several studies have evaluated the properties of various combinations of medications used for this purpose (4-6). Usually, a combination of an intravenous narcotic and a benzodiazepine, for example fentanyl/midazolam, is used for PSA in such cases. Propofol is an effective sedative with a rapid effect and very short duration of sedation (7). These properties result in a decrease in the duration of time necessary to reduce the dislocated joint, to monitor the patient, to precisely titrate the medication, and the length of stay. On the other hand, the antiemetic property of propofol is of clinical significance in relation to the risk of apnea and aspiration during the procedure (8). Also, it can be used in liver and kidney insufficiency (7). Therefore, propofol is an appropriate medication for PSA in EDs.
2. Objectives
In the present study, the efficacy of a combination of propofol and fentanyl (propofol/fentanyl) was compared with that of midazolam and fentanyl (fentanyl/midazolam) to induce sedation for reduction of ASD in ED.
3. Patients and Methods
3.1. Subject and Study Design
This study was a prospective, randomized, and clinical trial (Registration ID in IRCT IRCT201501236238N2) of patients with ASD in an age range of 18 - 60. The study was undertaken at the ED of Imam Hossein Hospital (Tehran, Iran) between April and August 2011. Approximately 6,000 patients are admitted per month. The inclusion criteria include anterior dislocation of the shoulder and over 18 years of age. The exclusion criteria include hypersensitivity to midazolam, propofol, or fentanyl; other injury (fracture around shoulder or other limb); intake of food or fluid during last 4 hours; presence of airway difficulty; sensory problems; motor problems, vascular problems, and consumption of alcohol or other recreational drug during past 6 hours. The protocol of present study was reviewed and approved by Shahid Beheshti University of Medical Sciences. The study was conducted based on the principles of the Declaration of Helsinki. There were no gender limitations in the present study. All the study’s procedures in relation to various sedation and anesthetic procedures were thoroughly explained to each patient verbally and in written form before the study began and informed written consent was obtained. All patients were in a fasting state for at least 4 hours before the study procedures were instituted. Patients who were allergic to eggs and/or certain medications were excluded from the study. For double blind purposes, drug packs were prepared before commencement of the study by a pharmacist. Packs were sealed off and any other did not have knowledge as to the nature of the drugs. Since, propofol is white and midazolam is colorless, prescriptions for the drugs were performed by an emergency physician and data was collected by another emergency physician who was unaware of the medication groups of patients.
3.2. Study Protocol
Patients were randomly sedated with intravenous midazolam or propofol for reduction of dislocated joints. A simple randomization sequence was used based on a random number table. The physician carrying out the reduction procedure was unaware of the medications used for the purpose. For two groups, fentanyl was initially administered at a dose of 1 µg/kg. Then, a bolus of propofol titrated (slow IV during 30 seconds) until the spontaneous eyelid close. In addition, midazolam (slow IV during 30 seconds) titrated to the sedation end point (spontaneous eyelid close). Propofol (0.5 mg/kg = 0.5 mg/kg) and midazolam (initial doses = 2 mg) were both administered at, of, and followed two minutes after fentanyl administration, and depending on the patient needs subsequent doses were titrated using the same doses. Injections were carried out by an emergency physician under supervision of an expert in ED. Then, a questionnaire that consisted of demographic data the time interval between injection and induction of sedation (T1), duration of time from sedation to awakening (T2), the duration of time between sedation and full awareness to time, location and individuals (T3) was filled out for each group by an emergency physician who was unaware of the medication group of patients.
Adduction, external rotation, and flexion techniques were used to reduce the shoulder joint in all patients. The operator was an expert emergency physician with at least three years postgraduate experience and blind to the study drug. The subjects were under deep sedation and monitored during the whole procedure in relation to cardiac and respiratory functions, blood pressure, and pulse oximetry. Awakening was defined as the time of the first reaction in the form of opening the eyes after tapping on the area between the eyebrows. In the event of apnea, a facemask with a reserve bag with 100% oxygen was placed. If needed, intubation was used. Bradycardia was defined as a heart rate less than 60 pulses per minute, which is inadequate for clinical conditions. In this situation, the American Heart Association guidelines were used.
3.3. Data Analysis
Data were entered into SPSS statistic software (ver 17.5). The Fisher exact test was used for comparison of drugs side effect disparity between the two groups. For evaluation of age and time point (T1, T2, and T3) differences, a Mann-Whitney U test was used. P < 0.05 was considered significant. In the present study, the mean ± SD of T2 were 11.7 ± 6.35 vs. 4.7 ± 2.59 in the propofol and midazolam group, respectively. Therefore, with considering 95% confidence interval (α = 0.05) and power of 90% (β = 0.1) 19 patients required in each group to show a statistically significant difference between the groups. (The level of significance is 0.05, power of 0.99).
4. Results
A total of 48 patients with ASD were enrolled in this study (100% male). The mean age of patients was 31.9 ± 8.8 years (20 - 56) and the mean body weight was 82.4 ± 11.5 kg. Twenty-nine (60.4%) patients were sedated with midazolam and 19 (39.6%) with propofol. During the procedure, one patient in the propofol group experienced apnea (P = 0.39) and three patients (one in the midazolam group and two in the propofol group) experienced bradycardia (P = 0.34). All patients were followed up until there was successful shoulder reduction. A Mean ± SD shoulder reduction attempts in the propofol and midazolam groups were 1.55 (0.6) and 1.3 (0.4), respectively (P = 0.21). The mean total dose of propofol and midazolam were 1.7 mg/kg (0.7) and 1.0 mg/kg.
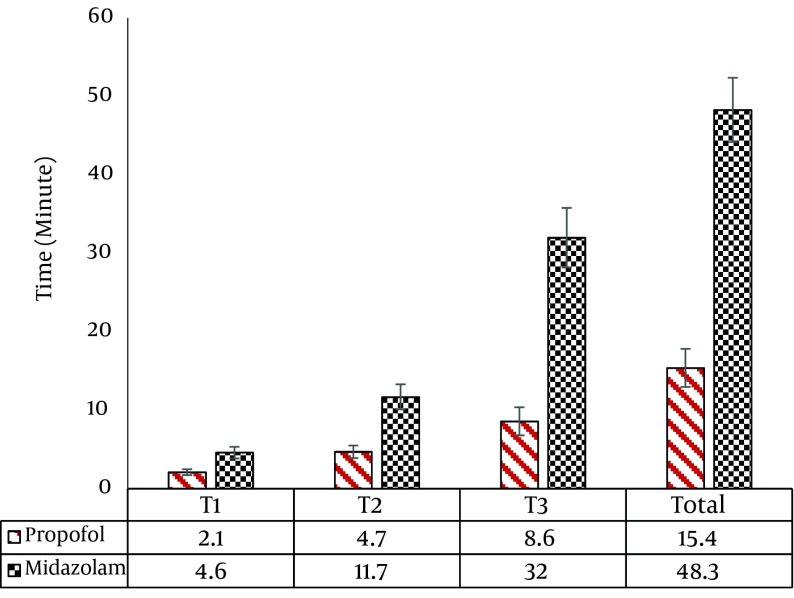
Figure 1 shows the mean T1, T2, and T3 and total time of PSA in the two groups. The mean T1 were 4.63 ± 2.35 and 2.14 ± 1.03 minutes in the midazolam and propofol groups, respectively (P < 0.001). In addition, the mean T2 and T3 in the midazolam versus propofol groups were 11.7 ± 6.35 vs. 4.7 ± 2.59 minutes and 32.07 ± 20.80 vs. 8.6 ± 3.5 minutes, respectively (P < 0.001).
Figure 1. The Time Interval between Injection and Induction of Sedation (T1); Duration of Time from Sedation to Awakening (T2); and the Duration of Time between Sedation, Full Awareness to Time, Location, and Individuals (T3).
5. Discussion
The results of this present study showed that propofol yields significantly better results when compared to midazolam in relation to the rate of sedation induction and the rate of recovery to full awareness. This study carried out suggestions that propofol is as effective as midazolam for reduction of an ASD. Propofol also causes a shorter procedural sedation and analgesia time. These findings are consistent with the results of a study carried out by Dunn et al. that showed that propofol and remifentanil shorten the recovery time, but the other results were similar to the use of morphine and midazolam during PSA to reduce ASD (9, 10). In addition, Taylor demonstrated that propofol seems to be better midazolam/fentanyl for reduction of ASD using the modified Kocher’s maneuver (11).
No significant differences were observed between the two groups in relation to the side effects of the drugs such as apnea and bradycardia. The determination of the most appropriate and safest medication or a combination of medications with a rapid anesthetic effect and the least side effects for PSA has been a concern of emergency medicine specialists. Various studies have evaluated different combinations of drugs but there is still controversy over the best modality and choices are predominantly made based on hospital protocols and policies (12). Propofol has a great appeal for emergency medicine specialists due to its shorter sedation induction time, rapid recovery to full consciousness, less side effects, and low cost (13, 14). The results of this study showed that patients sedated with propofol were in a better situation compared to those sedated with midazolam in relation to the variables mentioned above. Due to a lack of access to cerebral state index (CSI) for evaluation of the sedation level, the effects were observed and evaluated based on the subjective assessment of the physician carrying out the procedure, which might have influenced the results. The practitioner responsible to put the patient to sleep should be aware of the medications necessary, the doses involved, the side effects, and the necessary procedures to treat the complications. As a result, it was not feasible to keep the practitioner unaware of the medications used. However, to avoid a bias, the physician carrying out the reduction procedure was unaware of the medications used for the purpose.
Because propofol (an opaque, milky liquid) is easily distinguishable from midazolam and fentanyl (clear liquids), true blinding as to the nature of the study drugs was not possible. However, since the prescription of drugs and data gathering were performed by two independent physicians, blindness was performed effectively. In addition, assessing the adequacy of sedation was not done. But in similar studies the time intervals sedation, sedation to awakening, and sedation to full awareness of patients were the most important factors for the evaluation of effectiveness of the sedative effect of propofol and midazolam (9-11).
It appears that the combined use of propofol and fentanyl can be used as a safe and rapid combination to induce sedation for reduction of ASD. It is suggested to consider a patient's satisfaction in future research and comparison of costs of drugs and stay in emergency department as well as medical equipment used in an economic study.
Acknowledgments
The authors would like to gratefully thank the Imam Hossein Hospital personnel and ED nurses, without their help this work would not be possible. We would also like to thank the emergency medicine faculties and residents of Shahid Beheshti University of Medical Sciences at the aforementioned hospital for their participation and useful hints that made this research a fruitful experience. This article was based on a postgraduate thesis by Dr. Ghaffari Shad, Which was successfully completed under the supervision of Dr. Hatamabadi.
Footnotes
Authors’ Contributions:Hamid Reza Hatamabadi developed the original research idea, data analysis, and the preparation of the manuscript. Ali Arhami Dolatabadi contributed to data collection and analysis. Hojjat Derakhshanfar contributed to preparation of the manuscript. Somaye Younesian contributed to data collection and preparation of the manuscript. Ensieh Ghaffari shad contributed to the original research concept and participation in data collection.
Funding/Support:The research was conducted through a research grant from Shahid Beheshti University of Medical Sciences.
References
- 1.Jamali S. Anterior shoulder dislocation - seated versus traditional reduction technique. Aust Fam Physician. 2011;40(3):133–7. [PubMed] [Google Scholar]
- 2.Alimohammadi H, Azizi M-R, Safari S, Amini A, Kariman H, Hatamabadi HR. Axillary Nerve Block in Comparison with Intravenous Midazolam/Fentanyl for Painless Reduction of Upper Extremity Fractures. Acta Med Iranica. 2014;52(2):122–4. [PubMed] [Google Scholar]
- 3.Dolatabadi AA, Hatamabadi HR, Shahrami A. Femoral nerve block in patients with femoral shaft fractures in emergency depart ment. J Basic Appl Sci Res. 2013;3(11):15–9. [Google Scholar]
- 4.Blaivas M, Adhikari S, Lander L. A prospective comparison of procedural sedation and ultrasound-guided interscalene nerve block for shoulder reduction in the emergency department. Acad Emerg Med. 2011;18(9):922–7. doi: 10.1111/j.1553-2712.2011.01140.x. [DOI] [PubMed] [Google Scholar]
- 5.Cheok CY, Mohamad JA, Ahmad TS. A Prospective Comparison of Procedural Sedation and Ultrasound-guided Interscalene Nerve Block for Shoulder Reduction in the Emergency Department. J Orthopaedic Trauma. 2011;25(1):5–10. [Google Scholar]
- 6.Havel CJ, Strait RT, Hennes H. A clinical trial of propofol vs midazolam for procedural sedation in a pediatric emergency department. Acad Emerg Med. 1999;6(10):989–97. doi: 10.1111/j.1553-2712.1999.tb01180.x. [DOI] [PubMed] [Google Scholar]
- 7.Weaver CS, Hauter WE, Brizendine EJ, Cordell WH. Emergency department procedural sedation with propofol: is it safe? J Emerg Med. 2007;33(4):355–61. doi: 10.1016/j.jemermed.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 8.Borgeat A, Wilder-Smith OH, Saiah M, Rifat K. Subhypnotic doses of propofol possess direct antiemetic properties. Anesth Analg. 1992;74(4):539–41. doi: 10.1213/00000539-199204000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Dunn MJ, Mitchell R, Souza CD, Drummond G. Evaluation of propofol and remifentanil for intravenous sedation for reducing shoulder dislocations in the emergency department. Emerg Med J. 2006;23(1):57–8. doi: 10.1136/emj.2004.021410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dunn MJ, Mitchell R, DeSouza CI, Drummond GB, Waite A. Recovery from sedation with remifentanil and propofol, compared with morphine and midazolam, for reduction in anterior shoulder dislocation. Emerg Med J. 2011;28(1):6–10. doi: 10.1136/emj.2008.067652. [DOI] [PubMed] [Google Scholar]
- 11.Taylor DM, O'Brien D, Ritchie P, Pasco J, Cameron PA. Propofol versus midazolam/fentanyl for reduction of anterior shoulder dislocation. Acad Emerg Med. 2005;12(1):13–9. doi: 10.1197/j.aem.2004.08.039. [DOI] [PubMed] [Google Scholar]
- 12.Kariman H, Majidi A, Amini A, Dolatabadi AA, Derakhshanfar H, Hatamabadi H, et al. Nitrous oxide/oxygen compared with fentanyl in reducing pain among adults with isolated extremity trauma: a randomized trial. Emerg Med Australas. 2011;23(6):761–8. doi: 10.1111/j.1742-6723.2011.01447.x. [DOI] [PubMed] [Google Scholar]
- 13.Hohl CM, Sadatsafavi M, Nosyk B, Anis AH. Safety and clinical effectiveness of midazolam versus propofol for procedural sedation in the emergency department: a systematic review. Acad Emerg Med. 2008;15(1):1–8. doi: 10.1111/j.1553-2712.2007.00022.x. [DOI] [PubMed] [Google Scholar]
- 14.Burton JH, Miner JR, Shipley ER, Strout TD, Becker C, Thode HJ. Propofol for emergency department procedural sedation and analgesia: a tale of three centers. Acad Emerg Med. 2006;13(1):24–30. doi: 10.1197/j.aem.2005.08.011. [DOI] [PubMed] [Google Scholar]